Abstract
Background
A new device with metallic wires for scrape cytology was developed.
Aims
To compare the diagnostic performance of scrape cytology and conventional cytology during endoscopic retrograde cholangiopancreatography for biliary strictures.
Methods
A total of 420 cases with biliary stricture underwent transpapillary bile cytology. Among them, there are 79 cases with scrape cytology using the new device (scrape group) and 341 cases with conventional cytology (control group). Seventy-two and 174 cases underwent biliary biopsy at the same time as bile cytology in the scrape and control group, respectively.
Results
The sensitivity for malignancy of bile cytology in the scrape and control group was 41.2% [pancreatic cancer (PC): 23.1%, biliary cancer (BC): 52.5%] and 27.1% (PC: 16.3%, BC: 38.0%), respectively (P = 0.023). When analyzed PC and BC, respectively, there was no significant difference between the two groups. In the both groups, the sensitivity was significantly higher for BC than PC. In the scrape group, there was no difference in the sensitivity between cytology and biopsy [39.7% (PC: 17.4%, BC: 55.3%)], but in the control group, a significantly lower sensitivity was observed with cytology than biopsy (36.4% (PC: 19.7%, BC: 50.0%)) (P = 0.046). When analyzed PC and BC, respectively, there was no significant difference between cytology and biopsy. The sensitivity of combined cytology and biopsy was 55.6% (PC: 30.4%, BC: 71.1%) in the scrape group and 47.0% (PC: 24.6%, BC: 64.3%) in the control group.
Conclusion
Scrape bile cytology for biliary strictures may be superior to conventional cytology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endoscopic transpapillary bile cytology and biliary forceps biopsy with endoscopic retrograde cholangiopancreatography (ERCP) are generally performed for pathological diagnosis of biliary strictures. While these techniques have high specificity (90–100%), the sensitivity is low. The sensitivity of bile cytology for malignant biliary strictures is reported to be 6–55% with aspiration cytology [1,2,3,4,5,6,7] and 6–72% with brush cytology [1,2,3,4, 8,9,10,11,12,13,14,15,16,17,18,19]. Although the sensitivity of biliary forceps biopsy is reported to be 29–81% [4, 8,9,10,11,12,13, 20,21,22], which is slightly higher than that of bile cytology, the technical difficulty is higher. In addition, the sensitivity of bile cytology and biliary forceps biopsy significantly varies between facilities and reports.
There are several reasons why pathological diagnosis of bile cytology and biliary forceps biopsy is difficult; these reasons include insufficient amounts of specimens, poor quality of sampled specimens, and technical difficulties in approaching the stricture site. While bile cytology can be performed with relative ease, the procedure results in insufficient amounts and poor quality of specimens. Although biliary forceps biopsy can sample more specimens than bile cytology, the lesion site might not be accurately sampled under fluoroscopy. To overcome these issues, a device that enables an accurate approach to the target site and acquisition of specimens with sufficient quantity and quality for pathological evaluation is desired.
Trefle (Piolax Medical Devices, Yokohama, Japan) is a new device for scrape cytology, in which the device scrapes using the looped metallic wires. Trefle can be accurately guided to the target site over the guidewire; the stricture can then be scraped using the looped metal wire, thus providing sufficient specimens. Only one report on the diagnostic performance of the new device is currently available [23]. However, it must be noted that this report described a single-arm study, and the diagnostic ability was not compared with conventional cytology.
This study compares the pathological diagnostic performance between conventional cytology and scrape cytology using the new device for biliary strictures and is the first report to conduct such a comparison.
Methods
Patients
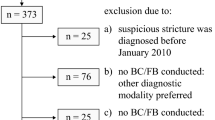
Between April 2010 and July 2017, 420 cases of transpapillary bile cytology underwent ERCP for biliary strictures at St. Marianna University School of Medicine Hospital. Cases without biliary strictures and those with postoperative reconstruction, other than Billroth-I, were excluded. Our hospital introduced the new device for scrape bile cytology in June 2015. Since then, bile cytology has been performed using the new device. The scrape group comprised 79 cases with scrape cytology using the new device [males, 52; females, 27; age, 72.2 ± 12.3 years (mean ± standard deviation (SD))]. The control group comprised 341 cases of bile cytology before introducing the new device [males, 229; females, 112; age, 68.8 ± 13.5 years (mean ± SD)]. In the control group, aspiration cytology was performed in 312 cases and brush cytology was performed in 29 cases. There were 72 cases in which biliary forceps biopsy was performed at the same time as cytology in the scrape group (mean number of biopsies, 2.3), and there were 174 cases in the control group (mean number of biopsies, 2.5).
In the scrape group, the underlying diseases that caused biliary stricture were malignant diseases (n = 68) and benign diseases (n = 11). On the other hand, in the control group, there were 280 patients with malignant diseases and 61 patients with benign diseases (Table 1).
Endoscopic Procedures
Trefle (Piolax Medical Devices, Yokohama, Japan) is a new scraping device that comprises scraping loops (three loops of 1.6-mm-diameter metal wire) and a 7-Fr outer sheath. The scraping loops and delivery sheath are both available over the guidewire (Fig. 1). There are side holes of the outer sheath, allowing bile to be aspirated by applying a negative pressure while scraping. As for technique of scrape cytology using the new device, after cannulation into the bile duct, a 0.025-inch guidewire was placed through the biliary stricture. Next, the sheath was inserted beyond the stricture over the guidewire, and the scraping loops were opened. While passing the scraping loops through the stricture under fluoroscopy, bile was aspired by applying a negative pressure to the side holes on the device. After the scraping loops passed the stricture, they were temporarily closed and stored in the sheath. This was followed by the insertion of the sheath beyond the stricture over the guidewire again, followed by opening of the scraping loops. Similarly, scraping and aspiration of bile were repeated five times. All bile specimens collected via aspiration were submitted for cytological examination.
In bile cytology of the control group, aspiration cytology was performed by inserting a cannula (ERCP catheter, MTW Endoscopie, Wesel, German) or 7-Fr tapered catheter (CX-PTCD kit [PD-EN7F (ST) 180C4], Gadelius Medical, Japan) beyond the stricture. Bile was sampled through aspiration and submitted for cytological examination. For brush cytology, we used a cytology brush (RX Cytology Brush, Boston Scientific, Natick, MA, USA). The brush part of the cytology brush is not a wire guidance. First, the outer sheath was inserted beyond the stricture, and the brush was then withdrawn to scrape the stricture. Aspired bile and cleaning solution from the brush were submitted for cytological examination.
Biliary forceps biopsy was performed after bile cytology for both the scrape and control groups with biopsy forceps (Radial Jaw 4P, Boston Scientific, Marlborough, Mass, USA) under fluoroscopy.
We did not routinely perform EST prior to sampling. The decision of with or without EST was left to the operator’s discretion. All ERCP procedures were performed under the supervision of an expert who has performed ERCP for > 1000 cases.
Diagnosis
Specimens were considered cancerous when malignant cells were clearly identified or highly atypical cells indicative of malignancy were observed. Specimens were considered to indicate a benign disease if normal cells were identified, atypical cells which cannot rule out malignancy were observed, or specimens were acellular. In cases where surgery was performed, the final diagnosis was based on the pathological diagnosis of the excised specimen. In non-resected cases, diagnosis was based on the clinical course.
Measurements
The data were retrieved from clinical and procedural records. The patient characteristics, the specimen sampling rates, sensitivity, specificity, and accuracy were retrospectively compared between the scrape and control groups. In addition, the diagnostic ability of bile cytology and biliary forceps biopsy was compared; likewise, the combined diagnostic results of bile cytology and biliary forceps biopsy were also compared. We also investigated procedural adverse events caused by scrape with a metal wire using the new device in order to evaluate the safety of scrape with a metal wire.
The specimen sampling rate was defined as the rate of obtaining of specimens in adequate quantity and quality for diagnosis. The sensitivity indicates the cancer detection rate, that is, the proportion of cases diagnosed with cancer by endoscopic sampling among all cases finally diagnosed with cancer.
This study was approved by the institutional review board of St. Marianna University School of Medicine (approval number: 3736).
Statistical Analysis
Chi-square test, Fisher’s exact test, and Welch’s t test were used for statistical analysis where appropriate. A P value of < 0.05 was regarded to be significant. Statistical analysis was performed using the StatMate IV software (ATMS Co., Ltd., Tokyo, Japan).
Results
Patient Characteristics
There was no difference in terms of gender and primary disease between the scrape and control groups (N.S.). The patients in the scrape group were significantly elder compared with those in the control group (P = 0.032) (Table 1).
Pathological Diagnosis
Specimen sampling rates from bile cytology in the scrape and control groups were 98.7% (78/79) and 96.5% (329/341), respectively, and did not show a significant difference (N.S.).
The sensitivity of bile cytology in the scrape and control groups was 41.2% (28/68) and 27.1% (76/280), respectively, indicating that the scrape group had a significantly higher rate (P = 0.023) (Table 2). The sensitivity of brush cytology and aspiration cytology in the control group was 11.1% (2/18) and 28.2% (74/262), respectively, with a significantly higher rate in the scrape group (P = 0.036, P = 0.040). Comparison of sensitivity between scrape cytology and aspiration cytology was shown in Table 3.
Comparison with regard to primary disease indicated that sensitivity to biliary cancer was 52.5% in the scrape group and 38.0% in the control group. Thus, in cases of biliary cancer, although the scrape group had higher sensitivity, the statistical difference was not significant (P = 0.100). On the other hand, sensitivity to pancreatic cancer was 23.1% in the scrape group and 16.3% in the control group, indicating no significant difference (P = 0.405). In the scrape and control group, the sensitivity was significantly higher for biliary cancer than pancreatic cancer (P = 0.018, < 0.001). Specificity in bile cytology was 100% in both the scrape and control groups, and accuracy was 49.4 and 40.2%, respectively. Thus, the accuracy for the scrape group was approximately 9% higher, but the difference was not significant (P = 0.136).
The sensitivity of biliary forceps biopsy in the scrape and control groups was 39.7 and 36.4%, respectively (N.S.). In the scrape group, there was no difference in the sensitivity between bile cytology and biliary forceps biopsy (41.2 vs. 39.7%) (N.S.), but in the control group, a significantly higher sensitivity was observed with biliary forceps biopsy than with bile cytology (27.1 vs. 36.4%) (P = 0.046). Regarding the sensitivity of biliary forceps biopsy for each primary disease, pancreatic cancer and biliary cancer was 17.4 and 55.3%, respectively, in the scrape group and 19.7 and 50.0%, respectively, in the control group. On the other hand, the sensitivity of bile cytology for pancreatic cancer and biliary cancer was 23.1 and 52.5%, respectively, in the scrape group and 16.3 and 38.0%, respectively, in the control group. Therefore, in the comparison between cytology and biopsy, statistically significant difference was not found in either pancreatic cancer or biliary cancer in the scrape and control group. However, for biliary cancer in the control group, although there was no statistically difference, biopsy had higher sensitivity than cytology (38.0 vs. 50.0%) (P = 0.079). Comparison between bile cytology and biliary biopsy is shown in Table 4.
In cases where bile cytology and biliary forceps biopsy were both performed, the combined sensitivity were 55.6% (25/63) in the scrape group and 47.0% (55/151) in the control group. While there was no statistically significant difference (P = 0.255), the scrape group was approximately 9% higher than the control group (Table 5). Analysis on the basis of primary diseases showed that when comparing pancreatic cancer and biliary cancer, the sensitivity was 30.4 and 71.1%, respectively, (P = 0.002) in the scrape group and 24.6 and 64.3%, respectively, (P < 0.001) in the control group. In both the groups, sensitivity was significantly higher for biliary cancer than pancreatic cancer. Among the samples determined to be malignant, 40.0% (10/25) were positive based on only cytology and 44.0% (11/25) were positive based on only biopsy in the scrape group. In contrast, 29.1% (16/55) were positive based on only cytology and 52.7% (29/55) were positive based on only biopsy in the control group. Thus, more cases were found to be positive based on only biopsy in the control group (P = 0.012).
Adverse Events Caused by Scrape with Metal Wire
The procedural adverse events caused by scrape with metal wire using the new device were one case of bleeding. When a metallic wire was used to scrape a biliary stricture caused by biliary invasion owing to gallbladder cancer (Fig. 2a), an active bleed occurred. The patient went into a state of shock (blood pressure < 60 mmHg), and there were massive hemobilia (Fig. 2b). But placement of a fully covered metallic stent and coiling with Angio made it possible to achieve hemostasis (Fig. 3).
Discussion
Endoscopic techniques such as transpapillary bile cytology and biliary forceps biopsy with ERCP, and endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) are generally performed for the pathological diagnosis of lesions that cause biliary strictures. Transpapillary bile cytology and biliary forceps biopsy with ERCP have an advantage that biliary drainage with endoscopic biliary stenting (EBS) or endoscopic naso-biliary drainage (ENBD) can be simultaneously performed. However, the sensitivity for these techniques is unsatisfactory.
Bile cytology is relatively technically easy if bile duct cannulation is possible. However, acquiring sufficient samples with the amount and quality required for pathological evaluation is often difficult. In this study, the specimen sampling rate of bile cytology did not differ between the scrape and control groups. However, given the fact that sensitivity was higher in the scrape group, the scrape group may have conferred a better quantity and quality of specimen collection. As the whole length of the new device comprises a looped metallic wire that is used for scraping and that acts over the guidewire, inserting into the target site and scraping the stricture can be performed accurately. Scraping with a metal wire may enabled obtaining a higher quantity of specimens compared with the traditional brush cytology.
According to several previous reports, biliary forceps biopsy can sample more specimens compared with bile cytology, and its sensitivity is slightly higher [4, 8,9,10,11, 14]. In this study, the sensitivity was significantly higher with biopsy than with cytology in the control group. However, both cytology and biopsy displayed similar sensitivities in the scrape group. Compared with cytology, biopsy is technically more difficult. Furthermore, when performed under fluoroscopy, the specimen might not be accurately sampled from the lesion site. However, because the whole length of the new device acts over a guidewire, it is easy to insert into the target site, enabling accurate scraping of the stricture.
In this study, although scrape cytology with the new device shows better sensitivity than conventional cytology, it still resulted in an unsatisfactory sensitivity of 41%. However, when combined with biopsy, the sensitivity increased to 56%. Therefore, it is desirable to combine scrape cytology and biopsy. Particularly in cases of biliary cancer, the sensitivity of combined biopsy and scrape cytology was 71.1%, which was relatively good; however, for pancreatic cancer, the sensitivity of combined scrape cytology and biopsy was low at 30%. According to the previous reports, EUS-FNA for pancreatic cancer has a good sensitivity of ≥ 85% [24,25,26,27,28]. Therefore, for the pathological diagnosis of pancreatic cancer, one must rely on other methods such as EUS-FNA. In addition, because there are reports that multiple cytology via ENBD [29, 30] and fluorescence in situ hybridization [31, 32] contribute to an increased diagnostic ability, the additional use of these techniques may be also useful. Conversely, because performing EUS-FNA for the pathological diagnosis of biliary cancer is often technically difficult, the combined use of biopsy and scrape cytology appears to be useful.
Only one report on the diagnostic performance of the new device is currently available [23]. Sakuma et al. [23] reported positive results regarding pathological diagnosis using the new device, with a specimen sampling rate of 93.5% and a sensitivity of 64.7%. However, it must be noted that this report described a single-arm study, and the diagnostic ability was not compared with conventional cytology. The sensitivity was 64.7%, which was better than our results of 41%. This inconsistency may be owing to Sakuma et al. evaluating precipitated specimens extracted from aspirated bile for histological examination not only cytological examination. We submitted all aspirated bile for cytological examination. Although this processing is cumbersome, separately evaluating precipitated specimens in the sampled bile may increase the diagnostic ability. Another reason for their results being more favorable is considered that they had more biliary cancer cases and fewer pancreatic cancer cases than those in our study.
We confirmed one case of severe bleeding that was accompanied by shock vital by scraping with the new device. Because the new device scrapes the site using a metallic wire, more tissues may be obtained and better specimens are sampled; however, there may be a risk for bleeding. If there is any resistance when pulling the metallic wire to scrape, pulling should be immediately halted. We were able to hemostasis by placement of a fully covered metallic stent and performing coiling with Angio; therefore, such procedures should be available immediately when performing scraping with the new device.
This study has several limitations. First, the study design is a single-center, retrospective study. The decision to use aspiration cytology or brush cytology in the control group was at the discretion of the endoscopist, leading to a lower number of samples being derived from brush cytology. Perhaps because of this low number of brush cytology cases, sensitivity was found to be lower than that reported in existing studies. In the future, comparison and verification of brush cytology and scrape cytology with a randomized controlled trial are desired. In addition, the fact of about 10% higher proportion of biliary cancer in the scrape group may contributes high sensitivity of the scrape group. However, even in the examination of biliary cancer cases, there was no statistically difference, but the scrape group was about 15% more sensitive. Therefore, we believe that only the difference in the proportion of the primary diseases affected the results. Moreover, sampling specimens were not re-reviewed in a blinded manner by the same pathologist. Because of the retrospective study with a relatively large number of cases, it was difficult to re-review.
In conclusion, our results of bile scrape cytology with the new device for biliary strictures were better than that of conventional cytology. Bile scrape cytology had sensitivity similar to that of biliary forceps biopsy. Combined scrape cytology and biopsy is expected to achieve a good diagnostic result, particularly for biliary cancer.
References
Foutch PG, Kerr DM, Harlan JR, Kummet TD. A prospective, controlled analysis of endoscopic cytotechniques for diagnosis of malignant biliary strictures. Am J Gastroenterol. 1991;86:577–580.
Desa LA, Akosa AB, Lazzara S, Domizio P, Krausz T, Benjamin IS. Cytodiagnosis in the management of extrahepatic biliary stricture. Gut. 1991;32:1188–1191.
Mansfield JC, Griffin SM, Wadehra V, Matthewson K. A prospective evaluation of cytology from biliary strictures. Gut. 1997;40:671–677.
Sugiyama M, Atomi Y, Wada N, Kuroda A, Muto T. Endoscopic transpapillary bile duct biopsy without sphincterotomy for diagnosing biliary strictures: a prospective comparative study with bile and brush cytology. Am J Gastroenterol. 1996;91:465–467.
Davidson B, Varsamidakis N, Dooley J, et al. Value of exfoliative cytology for investigating bile duct strictures. Gut. 1992;33:1408–1411.
Kurzawinski TR, Deery A, Dooley JS, Dick R, Hobbs KE, Davidson BR. A prospective study of biliary cytology in 100 patients with bile duct strictures. Hepatology. 1993;18:1399–1403.
Hattori M, Nagino M, Ebata T, Kato K, Okada K, Shimoyama Y. Prospective study of biliary cytology in suspected perihilar cholangiocarcinoma. Br J Surg. 2011;98:704–709.
Ponchon T, Gagnon P, Berger F, et al. Value of endobiliary brush cytology and biopsies for the diagnosis of malignant bile duct stenosis: results of a prospective study. Gastrointest Endosc. 1995;42:565–572.
Jailwala J, Fogel EL, Sherman S, et al. Triple-tissue sampling at ERCP in malignant biliary obstruction. Gastrointest Endosc. 2000;51:383–390.
Draganov PV, Chauhan S, Wagh MS, et al. Diagnostic accuracy of conventional and cholangioscopy-guided sampling of indeterminate biliary lesions at the time of ERCP: a prospective, long-term follow-up study. Gastrointest Endosc. 2012;75:347–353.
Weber A, von Weyhern C, Fend F, et al. Endoscopic transpapillary brush cytology and forceps biopsy in patients with hilar cholangiocarcinoma. World J Gastroenterol. 2008;14:1097–1101.
Pugliese V, Conio M, Nicolò G, Saccomanno S, Gatteschi B. Endoscopic retrograde forceps biopsy and brush cytology of biliary strictures: a prospective study. Gastrointest Endosc. 1995;42:520–526.
Kitajima Y, Ohara H, Nakazawa T, et al. Usefulness of transpapillary bile duct brushing cytology and forceps biopsy for improved diagnosis in patients with biliary strictures. J Gastroenterol Hepatol. 2007;22:1615–1620.
De Bellis M, Sherman S, Fogel EL, et al. Tissue sampling at ERCP in suspected malignant biliary strictures (Part 2). Gastrointest Endosc. 2002;56:720–730.
Ferrari Júnior AP, Lichtenstein DR, Slivka A, Chang C, Carr-Locke DL. Brush cytology during ERCP for the diagnosis of biliary and pancreatic malignancies. Gastrointest Endosc. 1994;40:140–145.
Glasbrenner B, Ardan M, Boeck W, Preclik G, Möller P, Adler G. Prospective evaluation of brush cytology of biliary strictures during endoscopic retrograde cholangiopancreatography. Endoscopy. 1999;31:712–717.
Harewood GC, Baron TH, Stadheim LM, Kipp BR, Sebo TJ, Salomao DR. Prospective, blinded assessment of factors influencing the accuracy of biliary cytology interpretation. Am J Gastroenterol. 2004;99:1464–1469.
Sasaki Y, Okabe Y, Ishida Y, et al. Evaluation of endoscopic transpapillary brushing cytology for the diagnosis of bile duct cancer based on the histopathologic findings. Dig Dis Sci. 2014;59:2314–2319.
Lee JG, Leung JW, Baillie J, Layfield LJ, Cotton PB. Benign, dysplastic, or malignant–making sense of endoscopic bile duct brush cytology: results in 149 consecutive patients. Am J Gastroenterol. 1995;90:722–726.
Kubota Y, Takaoka M, Tani K, et al. Endoscopic transpapillary biopsy for diagnosis of patients with pancreaticobiliary ductal strictures. Am J Gastroenterol. 1993;88:1700–1704.
Schoefl R, Haefner M, Wrba F, et al. Forceps biopsy and brush cytology during endoscopic retrograde cholangiopancreatography for the diagnosis of biliary stenoses. Scand J Gastroenterol. 1997;32:363–368.
Kawashima H, Itoh A, Ohno E, Goto H, Hirooka Y. Transpapillary biliary forceps biopsy to distinguish benign biliary stricture from malignancy: how many tissue samples should be obtained? Dig Endosc. 2012;24:22–27.
Sakuma Y, Kodama Y, Sogabe Y, et al. Diagnostic performance of a new endoscopic scraper for malignant biliary strictures: a multicenter prospective study. Gastrointest Endosc. 2017;85:371–379.
Hewitt MJ, McPhail MJ, Possamai L, Dhar A, Vlavianos P, Monahan KJ. EUS-guided FNA for diagnosis of solid pancreatic neoplasms: a meta-analysis. Gastrointest Endosc. 2012;75:319–331.
Chen J, Yang R, Lu Y, Xia Y, Zhou H. Diagnostic accuracy of endoscopic ultrasound-guided fine-needle aspiration for solid pancreatic lesion: a systematic review. J Cancer Res Clin Oncol. 2012;138:1433–1441.
Puli SR, Bechtold ML, Buxbaum JL, Eloubeidi MA. How good is endoscopic ultrasound-guided fine-needle aspiration in diagnosing the correct etiology for a solid pancreatic mass?: a meta-analysis and systematic review. Pancreas. 2013;42:20–26.
Chen G, Liu S, Zhao Y, Dai M, Zhang T. Diagnostic accuracy of endoscopic ultrasound-guided fine-needle aspiration for pancreatic cancer: a meta-analysis. Pancreatology. 2013;13:298–304.
Banafea O, Mghanga FP, Zhao J, Zhao R, Zhu L. Endoscopic ultrasonography with fine-needle aspiration for histological diagnosis of solid pancreatic masses: a meta-analysis of diagnostic accuracy studies. BMC Gastroenterol. 2016;31:108. https://doi.org/10.1186/s12876-016-0519-z.
Uchida N, Kamada H, Ono M, et al. How many cytological examinations should be performed for the diagnosis of malignant biliary stricture via an endoscopic nasobiliary drainage tube? J Gastroenterol Hepatol. 2008;23:1501–1504.
Yagioka H, Hirano K, Isayama H, et al. Clinical significance of bile cytology via an endoscopic nasobiliary drainage tube for pathological diagnosis of malignant biliary strictures. J Hepatobiliary Pancreat Sci. 2011;18:211–215.
Kipp BR, Stadheim LM, Halling SA, et al. A comparison of routine cytology and fluorescence in situ hybridization for the detection of malignant bile duct strictures. Am J Gastroenterol. 2004;99:1675–1681.
Chaiteerakij R, Barr Fritcher EG, Angsuwatcharakon P, et al. Fluorescence in situ hybridization compared with conventional cytology for the diagnosis of malignant biliary tract strictures in Asian patients. Gastrointest Endosc. 2016;83:1228–1235.
Funding
The authors report that no financial support for this study was provided.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors declare no conflict of interests for this article.
Rights and permissions
About this article
Cite this article
Nakahara, K., Michikawa, Y., Morita, R. et al. Diagnostic Ability of Endoscopic Bile Cytology Using a Newly Designed Biliary Scraper for Biliary Strictures. Dig Dis Sci 64, 241–248 (2019). https://doi.org/10.1007/s10620-018-5217-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-018-5217-y