Abstract
Inflammatory bowel diseases (IBD), mainly including Crohn’s disease and ulcerative colitis, are characterized by chronic inflammation of the gastrointestinal tract. Despite improvements in detection, drug treatment and surgery, the pathogenesis of IBD has not been clarified. A number of miRNAs have been found to be involved in the initiation, development and progression of IBD, and they may have the potential to be used as biomarkers and therapeutic targets. Here, we have summarized the recent advances about the roles of miRNAs in IBD and analyzed the contribution of miRNAs to general diagnosis, differential diagnosis and activity judgment of IBD. Furthermore, we have also elaborated the promising role of miRNAs in IBD-related cancer prevention and prognosis prediction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inflammatory bowel diseases (IBD), mainly referring to the Crohn’s disease (CD) and ulcerative colitis (UC), are characterized by uncontrolled chronic inflammation of the gastrointestinal (GI) tract. The initiation of IBD is mainly due to the abnormal immune response against luminal antigens and microbiota. The incidence of IBD rises in parallel with rapid modernization and urbanization of a country. The highest occurrence of IBD is observed in developed countries in the West, affecting up to 0.5% of the general population [1]. And the rate of increase in its prevalence varies notably in Asia, with some countries in East Asia experiencing an over doubled increase in the past few decades [2]. The researches on the concrete mechanisms of IBD gradually focus on the genetic level, such as rs2910164, rs3024505, and MYO9B gene polymorphisms [3]. Up to now, there has been no comprehensive theory of IBD etiopathogenesis, leading to some difficulties in diagnosis, differential diagnosis, judging prognosis and therapy [4].
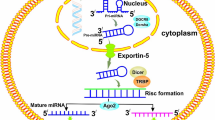
MiRNAs are evolutionarily conserved non-coding RNA molecules(20–22 nucleotides in length)that primarily function to prevent mRNA translation or initiate mRNA degradation at the posttranscriptional level via binding to the 3′ untranslated region (UTR) of their target mRNAs [5]. Besides, some animal miRNAs may also target 5′UTR and coding regions according to bioinformatics predictions and others experiments [6]. Many investigations have showed that miRNAs are associated with many diseases, such as tumors, autoimmune diseases, cardiac diseases and endocrine disorders [7–14]. In 2008, Wu et al. [15] had firstly assessed miRNA expression in UC patients. Since then, large numbers of related studies have emerged. And now there is a tendency of translating IBD-related miRNAs into clinical application. Here we reviewed the recent related studies and specifically elaborated the prospect of specific miRNAs on diagnosis and treatment in IBD.
Roles of MiRNAs in IBD Pathogenesis
There is no denying that findings of preclinical experiments can provide basic directions for clinical application. Recently, the roles of miRNAs in IBD pathogenesis are gradually recognized.
Dysregulation of Intestinal Epithelial Barrier
Large numbers of intestinal epithelial cells constitute the intestinal physical barrier. Tight junction among epithelial cells contributes to the stability of intestinal cells. These components collectively serve as a reliable barrier against commensal bacteria. However, dysregulation of intestinal epithelial cells can impair barrier function, leading to increased paracellular permeability and possibility of antigen exposure. Subsequently, acute inflammation can become chronic owing to persistent existence of harmful stimulation. The risk of IBD naturally goes up [16, 17]. Increasing numbers of scientific researchers have focused on the mechanism of dysregulation of intestinal epithelial cells. Some technological research findings have been put into clinical treatment, such as anti-TNF-α therapy [18]. Other findings enrich the established explanation for the mechanisms of classical anti-IBD drugs, such as glucocorticoids [19]. As the genetic regulators in posttranscriptional level, miRNAs have become a hot spot in development of IBD.
MiR-21 has been proved to be significantly increased in the fibroblasts of active UC [20]. It is the only miRNA that is associated with both nitric oxide synthase 2 (NOS2) and CD68 in IBD, contributing to relevant concentrations of nitric oxide (NO) and activation of macrophages. The change in NO pathway leads to senescence in adjacent epithelial cells by up-regulating HP1γ. In addition, miR-146a, miR-126, miR-223, and miR-221 have been found to be involved in the regulation of NOS2 in IBD tissues [21].
Occludin and claudin are tight junction proteins, which help to maintain impenetrability of barrier function against intestinal bacterial antigen. Loss or mutation of these genes can give an easier access to chronic inflammation [22–24]. It has been proved that miR-122 can directly target the occludin mRNA and increase the intestinal tight junction permeability in two levels, filter-grown Caco-2 monolayers (in vitro) and recycling perfusion of mouse intestine intestinal model systems (in vivo) [25]. MiR-874 can suppress occludin and claudin-1 expression, promoting the paracellular permeability in vitro through targeting 3′UTR of AQP3 [26]. MiR-233 may indirectly downregulate claudin-8 in the IL-23 pathway in mice with trinitrobenzene sulfonic acid (TNBS)-induced colitis, a specially established model to study mucosal inflammation [27]. Yang et al. had found that overexpression of miR-21 may impair the intestinal epithelial function by targeting RhoB in UC patients. The process may cause a series of alterations, such as a decrease in the transepithelial electrical resistance, an increase in barrier permeability, and even epithelial apoptosis [28, 29].
Epithelial fibrosis is a major factor in IBD development, especially in CD. Downregulation of miR-29b may promote fibrosis by up-regulation of collagen I and III transcripts and collagen III protein, inducing the pathogenesis of intestinal fibrosis in mucosa overlying a stricture in CD patients [30]. TGF-β1, a mediator of fibrosis in many diseases, can significantly inhibit the expression of miR-200b. MiR-200b can ameliorate intestinal fibrosis through directly downregulating ZEB1 and ZEB2 in DLD-1 cells [31]. Some studies revealed that miR-200b might play a pivotal role in epithelial fibrosis and even in epithelial-mesenchymal transition (EMT) in inflamed mucosa and ulcers of both CD and UC patients [32]. MiR-155 is a relatively specific miRNA in UC. In 2012, Paraskevi et al. [33] had tested blood samples from CD, UC patients and healthy controls, in which miR-155 was the most highly expressed of the UC-associated miRNA. Min et al. [34] had proved that miR-155 was involved in UC pathogenesis in inflammatory cytokine-stimulated colonic epithelial cells (HT29 cells) by directly inhibiting FOXO3 and indirectly silencing IκBα. Pathak et al. [35] had collected biopsies from patients with UC (n = 8) or CD (n = 8) undergoing colonoscopy for their ordinary follow-up and found that miR-155 could isolate intestinal fibroblasts and myofibroblasts from UC patients but not from CD patients through directly suppressing SOCS1 expression. Wu et al. [36] had detected the miRNA profile and found that the expression of miR-192 decreased by nearly half in active UC tissues. They employed HT29 cell lines to validate that miR-192 might play roles in inhibiting the formation of UC through modulating multiple microbial response pathways and fibrosis mediators, such as MIP-2α (macrophage inflammatory peptide-2α), Toll-like receptor 6, TRAF-interacting protein, CC chemokine receptor 6, and IL-18 receptor [36]. And meanwhile, it is necessary to carry out studies to determine whether miR-192 could influence models of innate immunity, inflammation, and fibrosis via regulating these putative targets [36].
Disruption of Immune Homeostasis
IBD can essentially be regarded as chronic intestinal inflammation, and intestinal immune homeostasis keeps the balance between inflammatory and anti-inflammatory processes [37]. Dysregulation of immune cell and inflammatory responses is a hallmark of multiple diseases encompassing atherosclerosis, rheumatoid arthritis, psoriasis, and metabolic syndromes [38]. Once inflammation is overreacted in intestinal tract, the foundation of IBD pathogenesis will be established, leading to a breakdown of intestinal homeostasis and the development of aberrant inflammatory responses to the intestinal flora [39].
Innate immune system contains many immune cells, including monocytes/macrophages, dendritic cells (DCs), neutrophils, natural killer (NK) cells, NK T cells, mast cells, eosinophils, and basophils. Many miRNAs participate in IBD through influencing different innate immune cells. Chuang et al. [40] had found that miR-192, miR-495, miR-512, and miR-671 might suppress NOD2 expression in HCT116 cells. MiR-10a, whose expression decreased in inflamed mucosa of IBD, might downregulate mucosal inflammatory response through inhibiting IL-12/IL-23p40 and NOD2 expression in DCs [41, 42]. MiR-146a, a NO-responsive miRNA, was reported to target NUMB gene and alleviate the suppression of sonic hedgehog (SHH) signaling in macrophages of murine model [43]. MiR-320 could directly target NOD2 in intestinal biopsies of children with IBD [44]. MiR-23b could directly target 3′UTR of Marcksl-1 in macrophages of hPepT1 transgenic mice model [45]. The presence of microbiota downregulated miR-107 expression in DCs and macrophages in a MyD88- and NF-κB-dependent manner, inhibiting TLR ligand-stimulated IL-23p19 expression and IL-23 production [46]. Maharshak et al. [47] had demonstrated an inflammation-dependent homeostatic role for the regulation of AChE by miR-132 in IBD.
The immune cells in adaptive immune system are mainly B cells and T cells. According to accumulated evidences, T cells play a major role in IBD genesis and development. IBD-related T cells mainly contain T-helper (Th) cells (Th1, Th17) and regulatory T (Treg) cells [48]. Wu et al. [41] had tested the cytokines of CD4+ T cells from IBD and transfected the cells with pre-miR-10a. IFN-γ, TNF, and IL-17A were significantly downregulated, indicating that miR-10a preferentially suppressed Th1 and Th17 cells. Deletion of miR-21 could exacerbate CD4+ T cell-mediated models of colitis [49]. Loss of miR-155 may lead to the decrease in Th1/Th17 [50]. As a Foxp3 target, miR-155 may play a key role in controlling Treg homeostasis and function [51]. MiR-212/132 was proved in intestinal epithelial cells of mice to be an effective therapeutic target by affecting multiple kinds of T cells. Repression of miR-212/132 led to the induction of Treg1 cells and IL-10-producing CD4+ cells and led to the reduction in Th17 cells [52]. MiR-210 may function as a pivotal mediator in T cells connection. CD4+ T cells activation robustly induced miR-210 expression via HIF-1α under hypoxia conditions, and miR-210 also regulated Th17 polarization under reoxygenation by targeting HIF-1α [53].
However, there are two limit points. One is the fragmentization of study results. It is hard to weave them into a quite integrated network. This problem results from a lack of vital breakthrough in the relationship between miRNA and intestinal immunological diseases. It is in an urgent need of more critical miRNAs or mechanisms connecting with other classical and novel pathways. The other is the lack of practical value of study results. Most current researches still stay in molecular biological level. Few have been proved to own potentials to be translated into clinical use.
Dysregulation of Cellular Autophagy
Autophagy is an ancient lysosomal bulk degradative process in which the membrane-surrounded structures (autophagosomes) engulf both organelles and cytosolic macromolecules and deliver them to the lysosome for degradation. In higher eukaryotes, this pathway, mainly referring to macroautophagy, plays a crucial role in many processes, such as cell differentiation, which is the response to environmental stress and clearance of intracellular pathogenic microbes (xenophagy) [54]. Dysregulated autophagy has been linked to various human diseases including IBD. A number of studies have implicated the importance of autophagy to regulate the biological function of Paneth cells [55]. The current genome-wide association studies (GWAS) and following meta-analyses have had a great success in identifying novel IBD-associated genetic loci and in highlighting a series of autophagy-correlated molecular pathways underlying the pathogenesis of IBD. MiRNAs function as a kind of contributor to regulate some autophagy-related susceptibility genes in IBD, such as ATG5 (autophagy-related gene 5), ATG16L(autophagy-related gene 16-like 1), and IRGM (immunity-related GTPase family, M). Autophagy regulates miRNA homeostasis by degrading the miRNA-induced silencing complex (miRISC) [56, 57].
IRGM is a human protein recently highlighted for its contribution to autophagy. It has been proved that the gut mucosa of CD patients harbor an increased amount of the pathogenic adherent-invasive E. coli (AIEC), and IRGM-dependent autophagy makes a prominent contribution to fighting pathogenic AIEC [58]. Brest et al. [59] had found that miR-196 was overexpressed in the inflammatory intestinal epithelia of individuals with CD. The loss of tight regulation of IRGM expression led to a defect in autophagy-mediated controlling of intracellular replication of CD-associated AIEC by autophagy (Fig. 1). Whether miRNAs could regulate precisely autophagy-related susceptibility genes in IBD pathogenesis needs more exploration on the further mechanism in dysregulation of cellular autophagy.
MiRNA dysregulation of autophagy in IBD pathogenesis. Autophagy is an ancient cellular process in which the membrane-surrounded structures (autophagosomes) engulf both organelles and cytosolic macromolecules and deliver them to the lysosome for degradation. MiR-196 was overexpressed in the inflammatory intestinal epithelia of individuals with Crohn’s disease, downregulating the expression of IRGM. MiR-142-3p negatively regulated ATG16L1 expression and decreased autophagic activity. The miR-93 and miR-106b targeted ATG16L1, leading to a reduction in autophagosome formation. The infection of AIEC activated nuclear factor-κB and subsequently up-regulated the expression of miR-30C and miR-130a. ATG5 and ATG16L1 targeted miR-30c and miR-130a, respectively
ATG16L1 exists in three alternative splicing isoforms and is an essential adaptor protein for autophagosome formation in the process of autophagy [60, 61]. The defects of ATG16L1 function, usually observed in CD tissues, are closely associated with the elevated intestinal inflammation and aberrant Paneth cell function. And some single nucleotide polymorphisms (SNPs) linked to the pathogenesis of CD are located in ATG16L1 [62]. Interestingly, ATG16L1 expression can also be regulated by the interaction of several distinct miRNAs. Zhai et al. [63] had demonstrated that miR-142-3p might negatively regulate ATG16L1 and decrease autophagic activity on cell death and apoptosis induced by starvation in HCT116, Caco-2, and Jurkat cell lines. Meanwhile, miR-142-3p could inhibit NOD2-dependent autophagy and downregulate IL-8 mRNA expression effectively, further implying an autophagy-related role of miR-142-3p in the intestinal inflammation and CD. Enhanced by increased c-Myc, which was highly expressed in active CD, the high expression of miR-93 and miR-106b displayed a reduction in autophagosome formation by targeting ATG16L1. Nguyen et al. [64] had found that the infection of AIEC up-regulated expression of miR-30C and miR-130a by activating nuclear factor-kB (NF-κB) both in T84 cells and mouse enterocytes. Meanwhile, NF-κB p65 subunit could interact directly with the promoter elements of hsa-miR-30c and hsa-miR-130a genes. The signal pathway might effectively induce the secretion of the proinflammatory cytokine interleukin 8 (IL-8), leading to a defect in autophagy-mediated clearance of intracellular AIEC (Fig. 1).
Apart from the direct regulation between miRNAs and autophagy-associated genes, a growing number of evidences have proved that autophagy could regulate miRNA homeostasis via degrading the miRISC [65, 66]. Sibony et al. [67] had proposed a new mechanism in autophagy-associated CD pathogenesis that microbes, which disrupted the autophagy pathway, could induce altered AGO2 expression and subsequently influenced miRNAs to promote disease. Autophagy was involved in the regulation of the critical miRISC component AGO2 in epithelial cells, immune cells, and primary intestinal epithelial cells. AGO2 could significantly regulate 4 miRNAs: miR-148a, miR-15b, miR-23a, and let-7c. Among them, let-7c and miR-23a have been associated with active ulcerative colitis. Let-7c also played a key role in regulation of inflammation, interleukin 6, and interleukin 10 cytokine expression, and microbial infection.
Role of MiRNAs in IBD Diagnosis
Current diagnosis of IBD mainly relies on clinical manifestations, endoscopic evaluation, and imaging methods including magnetic resonance and histopathological examination [68]. However, clinical manifestations of IBD are various and approximately one quarter of patients can appear extraintestinal manifestations before IBD diagnosis [69]. Endoscopy and histopathological examination are regarded as the most common and reliable methods in diagnosis of IBD [70, 71]. Both of them greatly require clinicians’ skills and many other essential conditions [72]. Increasing numbers of researchers begin to focus on the specific biomarkers, such as C-reactive protein, calprotectin, lactoferrin, S100A12 protein, and pyruvate kinase [70, 73].
General Diagnosis of IBD
MiRNAs might have the potential to be used in CD and UC diagnosis. Guo et al. [74] had investigated the miRNA expression profiles of inflamed and non-inflamed terminal ileal mucosa in active CD patients and found that miR-192-5p was decreased in inflamed mucosa. Additionally, let-7b-5p and miR-495-5p were differentially expressed in non-inflamed mucosa compared with healthy control. The expression of miR-361-3p was higher, while that of miR-124-3p was lower in inflamed mucosa compared with that in the non-inflamed [74]. Jeremy et al. had tested miRNA profile in saliva of patients with IBD and found that miR-101 was up-regulated in patients with CD, while miR-21, miR-31, and miR-142 were up-regulated in patients with UC. MiRPlus-E1067, miRPlus-E1088, and miRPlus-E1117 were significantly reduced in the endoscopically involved UC colonic tissue as compared to those of endoscopically uninvolved [75]. Furthermore, these researches provided the possibility of a kind of noninvasive diagnostic method in IBD. Jensen et al. [76] had highlighted the function of miR-16, miR-106a, and miR-140-3p in plasma for the diagnosis of CD. Using reverse-transcription polymerase chain reaction (RT-PCR), they have measured miRNAs in a validation cohort of 102 patients with CD. Compared with patients without CD, miR-16 was significantly downregulated in patients with CD (fold change 0.83, P = 0.02). Receiver operating characteristic (ROC) analyses showed an area under the curve of 0.65 [76]. MiR-31 was reported to own the potential as a marker of genetic predisposition for CD [77]. Applying statistical simulation approaches to the high-throughput RNA-sequencing data of colonic tissue samples, Peck et al. had identified that miR-31 was aberrantly expressed in an inflammation-independent fashion in patients with CD. The tissue samples were collected from 21 CD and 14 non-IBD patients. And after the data analysis of different clinical phenotype groups (I, non-stricturing and non-penetrating; II, stricturing; III, penetrating/fistulizing), miR-215 demonstrated a potential as a predictor of a penetrating disease phenotype of the ileum in CD [77]. MiR-206 and miR-424 were also identified as biomarkers that were commonly and specifically expressed in the fresh-frozen tissue of colonic mucosa of patients with IBD [78]. Radha et al. had created a 31-miRNA biomarker panel to stratify UC patients from normal individuals (92.8% accuracy, 96.2% specificity, and 89.5% sensitivity) [79]. Zahm et al. had evaluated eleven miRNAs (miR-16, miR-20a, miR-21, miR-30e, miR-93, miR-106a, miR-140, miR-192, miR-195, miR-484, and let-7b) in CD patients. Amazingly, the combination of the eleven miRNAs showed an excellent clinical performance (sensitivity 70–83%; specificity 75–100%) [80]. MiR-29 family and miR-19-3p were significantly downregulated in mucosa overlying stricture in CD patients as compared to overlying non-strictured areas [81, 82].
Therefore, these miRNAs all have potentials to play important roles in IBD, and even some miRNA panels are showing an amazing performance. However, the samples of most studies are too small to be qualified for the clinical testing standard. Large sample analysis is eagerly needed.
Differential Diagnosis of IBD
The differential diagnosis of IBD can be divided into two aspects. One is to differentiate CD and UC, which can date back to 2010 when Magali et al. revealed that miRNAs could function as new biomarkers to distinguish UC and CD at early stages [83]. MiR-24 was detected to be differentially expressed in UC and L2 CD (Crohn’s colitis) samples from rectal biopsies by quantitative real-time PCR (qRT-PCR). Receiver operating characteristic (ROC) analysis of UC and L2 CD samples revealed that rectal miR-24 correctly classified 84.2% of patients, with a sensitivity of 83.3% and specificity of 85.7%, suggesting miR-24 might be a potential biomarker to help differentiate UC from L2 CD [84]. In addition, by using qRT-PCR and miRNA microarray analysis, Jeremy et al. had reported that a panel of miRNAs (miR-19a, miR-21, miR-31, miR-101, miR-146a, and miR-375) differentially expressed in matched colon biopsies collected from 10 CD and 7 UC patients. And these miRNAs reflected a statistical significance as potential markers to discriminate CD and UC [75]. Wu et al. [85] had demonstrated that eight miRNAs in peripheral blood (miRs-28-5p, miR-103-2, miR-149, miR-151-5p, miR-340, miR-505, miR-532-3p, and miRPlus-E1153) were able to distinguish active CD from active UC. The other aspect is the differentiation between IBD and other types of colitis. The differential expression of miR-31, in formalin-fixed, paraffin-embedded colonic mucosa collected from IBD patients, could distinguish IBD from collagenous colitis, lymphocytic colitis infectious colitis, chronic ischemic colitis, diverticular disease-associated colitis, drug-induced colitis, or colitis of unknown cause [78, 86].
Activity Judgment of IBD
The activity judgment of IBD can provide guidance for clinical treatment. Despite recent development of next-generation sequencing and bioinformatics, the current scientific knowledge of diagnostic markers to improve interventional approaches in IBD is still scarce [87]. During recent years, miRNA has gradually showed its potential of judging IBD activity, especially in UC. Mehmet et al. had detected that microarray-based miRNA profiles by colonic mucosal pinch biopsies collected from the descending part were obtained endoscopically from patients with different stages of IBD (active UC, n = 20; quiescent UC, n = 19), as well as healthy controls (n = 20) [88]. MiR-20b and miR-98 are found to be up-regulated more than a tenfold in active UC as compared to the rest. MiR-125b and let-7e were up-regulated more than fivefold in quiescent UC compared to the rest. The level of these miRNAs might serve as a promising choice to judge activity of IBD. Wu et al. [15] had investigated that miR-192 expression was significantly suppressed only in active UC by colonoscopic pinch biopsies from the sigmoid colon. Koukos et al. [89] had found that miR-4284 levels were significantly decreased in colonic tissues samples from active UC patients, with an observed sevenfold reduction, compared to the inactive UC controls. MiR-126 was only found to be overexpressed in active UC colonic tissues, directly downregulating IκBα expression [90]. The combination of circulating hsa-miR-4454, hsa-miR-223-3p, hsa-miR-23a-3p, and hsa-miR-320e in serum was correlated with UC activity and showed a higher sensitivity and specificity values than C-reactive protein [91]. The serum levels of miR-142-5p, miR-595, and miR-1246 showed a trend to distinguish active from inactive CD [92].
Role of MiRNAs in IBD Treatment
The classical treatment of IBD contains lifestyle changes, drug use, and surgery. Nowadays, an increasing number of new treatments attract clinicians’ attention, such as anti-fibrotic therapies, kinase inhibitors, barrier support, stem cell transplantation, and fecal microbiota transplantation [93].
MiRNAs as Potential Therapeutic Targets
MiR-19b was significantly downregulated in active Crohn’s disease (CD) [94]. As a direct regulator of SOCS3 (suppressor of cytokine signaling 3), miR-19b could suppress the inflammatory response by inhibiting SOCS3 from modulating chemokine production in intestinal epithelial cells (IECs) [94]. Cheng et al. [94] had demonstrated that treatment with pre-miR-19b could induce a striking improvement in histological signs of inflammation in CD, and the histological scores confirmed miR-19b’s anti-inflammatory effect. Overexpression of miR-122 could block LPS-induced caspase-3- and caspase-9-dependent apoptosis by downregulating NOD2 in intestinal epithelial cells, implying that miR-122 might be a potential therapeutic target in CD [95]. MiR-141 could directly inhibit the expression of CXCL12β in the epithelial cells of the inflamed colons from colitic mice and CD patients and block immune cell recruitment [96]. MiR-146b could improve intestinal epithelial barrier function and relieve intestinal inflammation in the dextran sodium sulfate (DSS)-induced colitis mice, through indirectly decreasing Siah2 expression and ubiquitinating TRAF proteins via activation of the NF-κB pathway [97], suggesting that miR-146b might have a therapeutic role in IBD. MiR-155 could regulate the inflammatory phenotype of intestinal myofibroblasts by targeting SOCS1 in UC, disturbing the process of intestinal inflammation [35]. Administrating miR-210 mimics might negatively regulate Hif1α and Th17 differentiation in IBD [53]. MiR-93 might improve intestinal epithelial barrier function by supporting FoxO1’s exclusion from the nucleus [16]. MiR-132 might pay an inflammation-dependent homeostatic role in IBD [47]. Furthermore, deficiency of miR-212/132 cluster led to a reduction in Th17 cells, an elevation of IL-10-producing CD4+ cells, and improved resistance to colitis [52]. Transfecting model cells with let-7e or let-7f might lead to reduced expression of IL-23R protein, regulating different T cell expression and improving intestinal inflammatory response [98]. Treatment with a synthetic mimic of miR-200c-3p in UC might decrease inflammation by counteracting the inflammatory action of IL-8 [99]. MiR-595 was significantly up-regulated in the sera of active colonic CD, UC, and RA patients [92]. It was reported that miR-595 could target the cell adhesion molecule neural cell adhesion molecule-1, and fibroblast growth factor receptor 2. It played a key role in the protection, differentiation, and repair of colonic epithelium, as well as the maintenance of tight junctions. Facilitation of NO/COX-2/miR-210 cascade might contribute to colon damage in UC patients [100]. IL-23/miR-223/CLDN8 cascade might participate in intestinal inflammation formation [27].
MiRNAs as Preventers of Colorectal Carcinogenesis
Colorectal cancer (CRC) is a well-established adverse outcome of longstanding IBDs, accounting for approximately 10–15% of all IBD deaths [101]. MiRNAs have been implicated in the regulation of IBD-related cancer processes [102]. Some miRNAs, including miR-146, miR-21, miR-200, miR-224, have been proved to be associated with senescence, DNA damage response, and epithelial-mesenchymal transition [103–106].
Preclinical studies in miRNA therapeutics with mimics or antagonists have demonstrated a great prospect, which encourages a further development of their clinical use for preventing IBD-related CRC [107]. MiR-214 may participate in a carcinogenesis-related NF-kB phosphorylation feed loop circuits [108]. MiR-214 inhibitor can significantly reduce inflammation responses and the number and size of tumors [109]. Chemically modified antisense-miR-214 has successfully provided a promising controlling approach for IBD-associated dysplasia and cancer. The miR-31-mimics-transfected colon cancer cells demonstrate significantly less hypoxia-inducible factor 1(FIH-1) 3′-UTR luciferase activity [110]. Chronic activation of HIF-1 pathway is the primary mechanism of tumor angiogenesis, leading to the production of vascular endothelial growth factor and basic fibroblast growth factor. MiR-224, the significantly overexpressed miRNA in IBD-associated cancers, has been proved to dysregulate cell cycle control by targeting tumor suppressor gene p21. MiR-224 is validated to regulate indeed release from the G1/S check-point, thereby circumventing a key cellular defense mechanism against uncontrolled proliferation [105, 111]. The advantage of miRNAs is their ability to affect multiple targets with a single hit, and the power of targeting a single miRNA far exceeds that of targeting a single gene. Future studies should be designed to explore more small molecular substances targeting specific miRNAs, such as miRNA mimics, anti-miRNAs oligonucleotides (AMOs), antagomirs, locked nucleic acid (LNA)-modified oligonucleotides, so as to develop the advanced therapeutical approach.
MiRNAs as Evaluation Tools of Drug Use
Chen et al. [112] had recruited steroid-sensitive patients, steroid-resistant patients and healthy individuals to screen miRNA expression profiles of serum and colon tissue samples. MiR-195 was found significantly decreased in the steroid-resistant patients, leading to an increased expression of Smad7 and corresponding up-regulation of p65 and the activator protein 1 pathway [112]. Thus, miR-195 might be a predictor for judging steroid resistance. Fujioka et al. had investigated nineteen CD patients who were applied to the induction therapy by infliximab, a kind of anti-TNF-α drug. Let-7d and let-7e were significantly increased in the group of patients who achieved clinical remission, indicating that they could serve as a clinical evaluation tool of infliximab [113]. Despite poor findings in relationship between miRNA biomarkers and IBD treatment evaluation, the topic has already been attracting researchers’ attention.
The specific miRNA expression needs to be detected in a large population before it can be used as a biomarker for clinical usage. More clinical trials and translational work should be performed to examine whether the miRNAs described in Table 1 can function as novel targets.
Role of MiRNAs in Predicting Risks of IBD-Related Cancer
IBD dysplasia is often difficult to diagnose because of the chronic regeneration and repair associated with chronic inflammation, as well as the difficulties in distinguishing such lesions from surrounding inflamed colonic mucosa [114]. This problem establishes an obstacle for prognosis prediction at early stage. The new molecular markers for prognosis-related judgment are urgently required. Identifying prognosis-related biomarkers of IBD patients may help to identify subgroups of patients that would benefit from more aggressive therapeutic interventions. The aberrant expression of miRNAs, which has been demonstrated in IBD-related cancer, contributes to cancer development.
MiR-26b, validated as a potential biomarker of IBD and CRC in previous reports, showed its value for predicting UC-associated neoplasms. The combination of Ki-67 and miR-26b reached a high accuracy of 93% [115, 116]. MiR-196, a family of miRNAs, was overexpressed in the inflammatory intestinal epithelia of individuals with Crohn’s disease and downregulated the IRGM protective variant [59]. The alteration of miR-196 was identified as a specific biomarker of CD-related dysplasia [59].
Ueda et al. [117] had analyzed the correlation between higher methylation levels of miR-124a genes and the higher epidemiologic risk of colitis-associated cancer (CAC) development in UC patients. Three miR-124a genes (miR-124a-1, miR-124a-2, and miR-124a-3) were methylated in all neoplastic tissues (CAC, dysplasia, and sporadic colorectal cancer). Due to a prominent association with disease extent and duration, the methylation level of miR-124a-3 was considered as a promising marker for estimating individual risk for CAC. High level of miR-155 was related to cancer cell invasion and poor survival, suggesting that miR-155 might be a potential indicator of poor prognosis [118]. Svrcek et al. [119] had found that overexpression of miR-155, targeting mismatch repair proteins, in the colonic mucosa samples was significantly associated with microsatellite-instability-related CRC.
The combinations of several miRNAs also showed potential values for predicting IBD prognosis. Kanaan et al. [111] had screened miRNA expression profiles in UC and CD patients and found that five miRNAs (miR-193b, miR-373, let-7e, miR-15b, and miR-372) were significantly downregulated in the progression from non-neoplastic tissue to dysplasia and from dysplasia to cancer, indicating that a low expression of these five miRNAs may predict a poor prognosis. Tan et al. [120] had screened miRNA expression profiles in UC and UC-related colorectal cancer patients. As a result, miR-194, miR-215, miR-93, miR-192, miR-92a, miR-29b, and miR-20a were significantly up-regulated, while miR-1231, miR-195, miR-143, and miR-145 were downregulated. Fang et al. had collected 223 patients with colorectal-related diseases and 130 healthy controls and selected three aberrantly expressed miRNAs (miR-24, miR-320a, and miR-423-5p). The sensitivity of the three miRNAs for predicting the early stage of CRC was 77.78, 90.74, and 88.89%, respectively, suggesting the promising potential of the three miRNAs to serve as novel biomarkers for IBD-related CRC early detection [7].
Because of the relatively small molecular weight and the endogenous power of targeting broad-range regulators, miRNAs are superior to protein in clinical application for predicting risks of IBD-related cancer. Following the trend of biomarker research, future studies should be performed to explore circulating miRNAs as valuable biomarkers. Meanwhile, concerning the lack of sufficient sensitivity and specificity of circulating miRNAs, it is reasonable to combine these circulating miRNAs with current tissue biomarkers so as to improve their accuracy.
Conclusion
IBD is a chronic complex disorder caused by multiple factors. Current studies about the role of miRNAs in IBD mainly focus on three aspects. The first aspect is the alteration of miRNA profiles in IBD. Many miRNAs, such as miR-10, miR-21, miR-122, and miR-155 [28, 41, 95, 121], have turned out to be significantly increased or decreased. MiRNA expression profiles in IBD can help to select the potential diagnostic biomarkers. Schaefer et al. [75] had claimed that examining the expression of miR-101, miR-21, miR-31, miR-142-3p, and miR-142-5p in saliva might be able to assist in differential diagnosis of IBD. The specific circulating miRNA expression may be valuable for the diagnosis of IBD, but it needs to be verified in a large population before clinical usage. The second aspect is the exploration of potential therapeutic miRNAs. Many miRNAs could directly intervene IBD genesis and development, such as miR-19b and miR-210 [53, 94, 100]. The third aspect is about the concrete pathways of miRNAs. MiRNA-related mechanisms in IBD mainly involve three closely linked parts: immune homeostasis disorder, dysregulation of intestinal epithelial barrier, and inhibition of autophagy. Some miRNAs can regulate multiple pathways, while some miRNAs are simultaneously regulated by several pathways, forming a complex network in IBD.
Many miRNAs, such as miR-21 and miR-146, are identified not only as new diagnostic and prognostic tools, but also as potential therapeutic targets in the future (Table 1). However, there are still many obstacles that need to be overcome before putting the basic research to clinical use. Some screening tests of IBD-related miRNA expression profiles show different results. Despite large quantities of findings on specific mechanisms, most of them are sporadic and cannot be weaved into an integral network. To our knowledge, the mechanism of NOD2/NF-κB pathway-mediated inflammatory response has received most attention (Fig. 2), but it is still difficult to be linked with other signal pathways completely. Furthermore, how to combine different miRNA molecules into one panel to reach clinical standard of IBD diagnosis? How to administrate miRNA mimics or antagonists? How to maximize miRNA therapeutic effects and minimize side effects? What combination drug regimen should we take to optimize patients’ progression? These problems still remain unknown. Despite large amounts of researches on miRNA, few of them own representativeness. Other than inevitable experimental errors, many subjective and objective reasons should be taken into consideration, such as different experimental models, different cell types, racial differences, and patients’ progression. It is necessary to execute a large-scale, population-based prospective cohort to validate the feasibility of clinical miRNA expression tests in IBD diagnosis, which may bring clinical application of miRNAs into a new stage.
MiRNA-regulated NOD2/NF-κB pathways in IBD. Some miRNAs, including miR-10a, miR-122, miR-192, miR-320, miR-495, miR-512, and miR-671, can bind to NOD2 mRNA and suppress the expression of intracellular receptor NOD2. Once NOD2 is combined with MDP, the downstream of NOD2 signaling activates the IκB kinase (IKK) complex, phosphorylating the NF-κB inhibitor IκB. NF-κB can be activated by miR-146b and miR-214. Free NF-κB translocates to the nucleus and stimulates the transcription of a large number of target genes
In summary, miRNAs play an important role in IBD. Many miRNAs can be considered as novel diagnostic markers and therapeutic targets. Further research should be performed to promote the clinical application of miRNAs in IBD.
References
Molodecky NA, Soon IS, Rabi DM, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012;142:46–54.
Ng WK, Wong SH, Ng SC. Changing epidemiological trends of inflammatory bowel disease in Asia. Intest Res. 2016;14:111–119.
Gazouli M, Papaconstantinou I, Stamatis K, et al. Association study of genetic variants in miRNAs in patients with inflammatory bowel disease: preliminary results. Dig Dis Sci. 2013;58:2324–2328.
Kalla R, Ventham NT, Kennedy NT. MicroRNAs: new players in IBD. Gut. 2015;64:504–517.
Bartel DP. MicroRNA target recognition and regulatory functions. Cell. 2009;136:215–233.
Da Sacco L, Masotti A. Recent insights and novel bioinformatics tools to understand the role of MicroRNAs binding to 5′ untranslated region. Int J Mol Sci. 2013;14:480–495.
Fang Z, Tang J, Bai Y, et al. Plasma levels of microRNA-24, microRNA-320a, and microRNA-423-5p are potential biomarkers for colorectal carcinoma. J Exp Clin Cancer Res. 2015;34:86.
Huang SP, Lévesque E, Guillemette C, et al. Genetic variants in microRNAs and microRNA target sites predict biochemical recurrence after radical prostatectomy in localized prostate cancer. Int J Cancer. 2014;11:2661–2667.
Shen Y, Pan Y, Xu L, et al. Identifying microRNA-mRNA regulatory network in gemcitabine-resistant cells derived from human pancreatic cancer cells. Tumour Biol. 2015;36:4525–4534.
Zhao HM, Wei W, Sun YH, Gao JH, Wang Q, Zheng JH. MicroRNA-9 promotes tumorigenesis and mediates sensitivity to cisplatin in primary epithelial ovarian cancer cells. Tumor Biol. 2015;36:6867–6873.
Honardoost MA, Naghavian R, Ahmadinejad F, Hosseini A, Ghaedi K. Integrative computational mRNA-miRNA interaction analyses of the autoimmune-deregulated miRNAs and well-known Th17 differentiation regulators: an attempt to discover new potential miRNAs involved in Th17 differentiation. Gene. 2015;572:153–162.
Zeng L, Cui J, Wu H, Lu Q. The emerging role of circulating microRNAs as biomarkers in autoimmune diseases. Autoimmunity. 2014;47:419–429.
Lee S, Lim S, Ham O, et al. ROS-mediated bidirectional regulation of miRNA results in distinct pathologic heart conditions. Biochem Biophys Res Commun. 2015;465:349–355.
Zhu J, Zhang Y, Zhang W, et al. MicroRNA-142-5p contributes to Hashimoto’s thyroiditis by targeting CLDN1. J Transl Med. 2016;1:166.
Wu F, Zikusoka M, Trindade A, et al. MicroRNAs are differentially expressed in ulcerative colitis and alter expression of macrophage inflammatory peptide-2 alpha. Gastroenterology. 2008;135:1624–1635.
Haines RJ, Beard RS, Eitner RA, Chen L, Wu MH. TNFα/IFNγ mediated intestinal epithelial barrier dysfunction is attenuated by microRNA-93 downregulation of PTK6 in mouse colonic epithelial cells. PLoS ONE. 2016;4:e0154351.
Blander JM. Death in the intestinal epithelium—basic biology and implications for inflammatory bowel disease. FEBS J. 2016;283:2720–2730.
Okamoto R, Watanabe M. Role of epithelial cells in the pathogenesis and treatment of inflammatory bowel disease. J Gastroenterol. 2016;1:11–21.
Fischer A, Gluth M, Weege F, et al. Glucocorticoids regulate barrier function and claudin expression in intestinal epithelial cells via MKP-1. Am J Physiol Gastrointest Liver Physiol. 2014;306:G218–G228.
Simone NL, Soule BP, Ly D, et al. Ionizing radiation-induced oxidative stress alters miRNA expression. PLoS ONE. 2009;4:e6377.
Sohn JJ, Schetter AJ, Yfantis HG, et al. Macrophages, nitric oxide and microRNAs are associated with DNA damage response pathway and senescence in inflammatory bowel disease. PLoS ONE. 2012;9:e44156.
Li SQ, Feng L, Jiang WD, et al. Deficiency of dietary niacin impaired gill immunity and antioxidant capacity, and changes its tight junction proteins via regulating NF-kappaB, TOR, Nrf2 and MLCK signaling pathways in young grass carp (Ctenopharyngodon idella). Fish Shellfish Immunol. 2016;55:212–222.
Ouyang J, Zhang ZH, Zhou YX, et al. Up-regulation of tight-junction proteins by p38 mitogen-activated protein kinase/p53 inhibition leads to a reduction of injury to the intestinal mucosal barrier in severe acute pancreatitis. Pancreas. 2016;45:1136–1144.
Xu F, Ye YT, Cai CF, et al. Observation of the middle intestinal tight junction structure, cloning and studying tissue distribution of the four Claudin genes of the grass carp. Fish Physiol Biochem. 2014;6:1783–1792.
Ye D, Guo S, Al-Sadi R, Ma TY. MicroRNA regulation of intestinal epithelial tight junction permeability. Gastroenterology. 2011;4:1323–1333.
Zhi X, Tao J, Li Z, et al. MiR-874 promotes intestinal barrier dysfunction through targeting AQP3 following intestinal ischemic injury. FEBS Lett. 2014;588:757–763.
Wang H, Chao K, Ng SC, et al. Pro-inflammatory miR-223 mediates the cross-talk between the IL23 pathway and the intestinal barrier in inflammatory bowel disease. Genome Biol. 2016;17:58.
Yang Y, Ma Y, Shi C, Chen H, et al. Overexpression of miR-21 in patients with ulcerative colitis impairs intestinal epithelial barrier function through targeting the Rho GTPase RhoB. Biochem Biophys Res Commun. 2013;434:746–752.
Shi C, Liang Y, Yang J, et al. MicroRNA-21 knockout improve the survival rate in DSS induced fatal colitis through protecting against inflammation and tissue injury. PLoS ONE. 2013;8:e66814.
Nijhuis A, Biancheri P, Lewis A, et al. In Crohn’s disease fibrosis-reduced expression of the miR-29 family enhances collagen expression in intestinal fibroblasts. Clin Sci. 2014;127:341–350.
Chen Y, Ge W, Xu L, et al. miR-200b is involved in intestinal fibrosis of Crohn’s disease. Int J Mol Med. 2012;29:601–606.
Zidar N, Boštjančič E, Jerala M, et al. Down-regulation of microRNAs of the miR-200 family and up-regulation of Snail and Slug in inflammatory bowel diseases—hallmark of epithelial-mesenchymal transition. J Cell Mol Med. 2016;20:1813–1820.
Paraskevi A, Theodoropoulos G, Papaconstantinou I, et al. Circulating MicroRNA in inflammatory bowel disease. J Crohns Colitis. 2012;6:900–904.
Min M, Peng L, Yang Y, Guo M, Wang W, Sun G. MicroRNA-155 Is Involved in the Pathogenesis of Ulcerative Colitis by Targeting FOXO3a. Inflamm Bowel Dis. 2014;20:652–659.
Pathak S, Grillo AR, Scarpa M, et al. MiR-155 modulates the inflammatory phenotype of intestinal myofibroblasts by targeting SOCS1 in ulcerative colitis. Exp Mol Med. 2015;47:e164.
Wu F, Zikusoka M, Trindade A, et al. MicroRNAs are differentially expressed in ulcerative colitis and alter expression of macrophage inflammatory peptide-2 alpha. Gastroenterology. 2008;135:1624.e24–1635.e24.
Owaga E, Hsieh RH, Mugendi B, Masuku S, Shih CK, Chang JS. Th17 cells as potential probiotic therapeutic targets in inflammatory bowel diseases. Int J Mol Sci. 2015;16:20841–20858.
Murphy EP, Crean D. Molecular interactions between NR4A orphan nuclear receptors and NF-kappaB are required for appropriate inflammatory responses and immune cell homeostasis. Biomolecules. 2015;5:1302–1318.
Pedros C, Duguet F, Saoudi A, Chabod M. Disrupted regulatory T cell homeostasis in inflammatory bowel diseases. World J Gastroenterol. 2016;22:974–995.
Chuang AY, Chuang JC, Zhai Z, Wu F, Kwon JH. NOD2 expression is regulated by microRNAs in colonic epithelial HCT116 cells. Inflamm Bowel Dis. 2014;20:126–135.
Wu W, He C, Liu C, et al. miR-10a inhibits dendritic cell activation and Th1/Th17 cell immune responses in IBD. Gut. 2015;64:1755–1764.
Xue X, Feng T, Yao S, et al. Microbiota downregulates dendritic cell expression of miR-10a, which targets IL-12/IL-23p40. J Immunol. 2011;187:5879–5886.
Ghorpade DS, Sinha AY, Holla S, Singh V, Balaji KN. NOD2-nitric oxide-responsive microRNA-146a activates sonic hedgehog signaling to orchestrate inflammatory responses in murine model of inflammatory bowel disease. J Biol Chem. 2013;288:33037–33048.
Pierdomenico M, Cesi V, Cucchiara S, et al. NOD2 is regulated by mir-320 in physiological conditions but this control is altered in inflamed tissues of patients with inflammatory bowel disease. Inflamm Bowel Dis. 2016;22:315–326.
Ayyadurai S, Charania MA, Xiao B, Viennois E, Zhang Y, Merlin D. Colonic miRNA expression/secretion, regulated by intestinal epithelial PepT1, plays an important role in cell-to-cell communication during colitis. PLoS ONE. 2014;2:e87614.
Xue X, Cao AT, Cao X, et al. Downregulation of microRNA-107 in intestinal CD11c(+) myeloid cells in response to microbiota and proinflammatory cytokines increases IL-23p19 expression. Eur J Immunol. 2014;44:673–682.
Maharshak N, Shenhar-Tsarfaty S, Aroyo N, et al. MicroRNA-132 modulates cholinergic signaling and inflammation in human inflammatory bowel disease. Inflamm Bowel Dis. 2013;19:1346–1353.
Xu XM, Zhang HJ. MiRNAs as new molecular insights into inflammatory bowel disease: crucial regulators in autoimmunity and inflammation. World J Gastroenterol. 2016;22:2206–2218.
Wu F, Dong F, Arendovich N, Zhang J, Huang Y, Kwon JH. Divergent influence of microRNA-21 deletion on murine colitis phenotypes. Inflamm Bowel Dis. 2014;20:1972–1985.
Singh UP, Murphy AE, Enos RT, et al. miR-155 deficiency protects mice from experimental colitis by reducing T helper type 1type 17 responses. Immunology. 2014;3:478–489.
Kohlhaas S, Garden OA, Scudamore C, Turner M, Okkenhaug K, Vigorito E. Cutting edge: the Foxp3 target miR-155 contributes to the development of regulatory T cells. J Immunol. 2009;182:2578–2582.
Chinen I, Nakahama T, Kimura A, et al. The aryl hydrocarbon receptor/microRNA-212/132 axis in T cells regulates IL-10 production to maintain intestinal homeostasis. Int Immunol. 2015;27:405–415.
Wang H, Flach H, Onizawa M, Wei L, McManus MT, Weiss A. Negative regulation of Hif1a expression and TH17 differentiation by the hypoxia-regulated microRNA miR-210. Nat Immunol. 2014;15:393–401.
Mizoguchi A, Mizoguchi E. Inflammatory bowel disease, past, present and future: lessons from animal models. J Gastroenterol. 2008;43:1–17.
Kaser A, Niederreiter L, Blumberg RS. Genetically determined epithelial dysfunction and its consequences for microflora-host interactions. Cell Mol Life Sci. 2011;68:3643–3649.
Zhang P, Zhang H. Autophagy modulates miRNA-mediated gene silencing and selectively degrades AIN-1/GW182 in C. elegans. EMBO Rep. 2013;14:568–576.
Gibbings D, Mostowy S, Jay F. Selective autophagy degrades DICER and AGO2 and regulates miRNA activity. Nat Cell Biol. 2012;14:1314–1321.
Petkova DS, Viret C, Faure M. IRGM in autophagy and viral infections. Front Immunol. 2012;3:426.
Brest P, Lapaquette P, Souidi M, et al. A synonymous variant in IRGM alters a binding site for miR-196 and causes deregulation of IRGM-dependent xenophagy in Crohn’s disease. Nat Genet. 2011;43:242–245.
Plantinga TS, Crisan TO, Oosting M. Crohn’s disease-associated ATG16L1 polymorphism modulates pro-inflammatory cytokine responses selectively upon activation of NOD2. Gut. 2011;9:1229–1235.
Ohsumi Y. Historical landmarks of autophagy research. Cell Res. 2014;24:9–23.
Salem M, Ammitzboell M, Nys K, et al. ATG16L1: a multifunctional susceptibility factor in Crohn disease. Autophagy. 2015;11:585–594.
Zhai Z, Wu F, Dong F, et al. Human autophagy gene ATG16L1 is post-transcriptionally regulated by MIR142-3p. Autophagy. 2014;10:468–479.
Nguyen HT, Dalmasso G, Müller S, Carrière J, Seibold F, Darfeuille-Michaud A. Crohn’s disease-associated adherent invasive Escherichia coli modulate levels of microRNAs in intestinal epithelial cells to reduce autophagy. Gastroenterology. 2014;146:508–519.
Gibbings D, Mostowy S, Jay F, Schwab Y, Cossart P, Voinnet O. Selective autophagy degrades DICER and AGO2 and regulates miRNA activity. Nat Cell Biol. 2012;14:1314–1321.
Gibbings D, Mostowy S, Voinnet O. Autophagy selectively regulates miRNA homeostasis. Autophagy. 2013;9:781–783.
Sibony M, Abdullah M, Greenfield L, et al. Microbial disruption of autophagy alters expression of the RISC component AGO2, a critical regulator of the miRNA silencing pathway. Inflamm Bowel Dis. 2015;21:2778–2786.
Iwańczak B, Iwańczak F. Indicators of inflammatory process in stool in diagnostics and monitoring of inflammatory bowel diseases. Pol Merkur Lekarski. 2015;39:389–392.
Vavricka SR, Rogler G, Gantenbein C, et al. Chronological order of appearance of extraintestinal manifestations relative to the time of IBD diagnosis in the swiss inflammatory bowel disease cohort. Inflamm Bowel Dis. 2015;8:1794–1800.
Vucelic B. Inflammatory bowel diseases: controversies in the use of diagnostic procedures. Dig Dis. 2009;27:269–277.
Sinh P, Shen B. Endoscopic evaluation of surgically altered bowel in patients with inflammatory bowel diseases. Inflamm Bowel Dis. 2015;21:1459–1471.
Canavese G, Villanacci V, Sapino A, et al. The diagnosis of inflammatory bowel disease is often unsupported in clinical practice. Dig Liver Dis. 2015;47:20–23.
Bor R, Balanyi Z, Farkas K, et al. Comparison of symptoms, laboratory parameters and illness perception in patients with irritable bowel syndrome and inflammatory bowel disease. Orv Hetil. 2015;156:933–938.
Guo Z, Wu R, Gong J, et al. Altered microRNA expression in inflamed and non-inflamed terminal ileal mucosa of adult patients with active Crohn’s disease. J Gastroenterol Hepatol. 2015;30:109–116.
Schaefer JS, Attumi T, Opekun AR, et al. MicroRNA signatures differentiate Crohn’s disease from ulcerative colitis. BMC Immunol. 2015;16:5.
Jensen MD, Andersen RF, Christensen H, Nathan T, Kjeldsen J, Madsen JS. Circulating microRNAs as biomarkers of adult Crohn’s disease. Eur J Gastroenterol Hepatol. 2015;27:1038–1044.
Peck BC, Weiser M, Lee SE, et al. MicroRNAs classify different disease behavior phenotypes of Crohn’s disease and may have prognostic utility. Inflamm Bowel Dis. 2015;21:2178–2187.
Lin J, Welker NC, Zhao Z, et al. Novel specific microRNA biomarkers in idiopathic inflammatory bowel disease unrelated to disease activity. Mod Pathol. 2014;27:602–608.
Duttagupta R, DiRienzo S, Jiang R, et al. Genome-wide maps of circulating miRNA biomarkers for ulcerative colitis. PLoS ONE. 2012;2:e31241.
Zahm AM, Thayu M, Hand NJ, Horner A, Leonard MB, Friedman JR. Circulating microRNA is a biomarker of pediatric crohn disease. J Pediatr Gastroenterol Nutr. 2011;53:26–33.
Brain O, Owens BM, Pichulik T, et al. The intracellular sensor NOD2 induces microRNA-29 expression in human dendritic cells to limit IL-23 release. Immunity. 2013;39:521–536.
Lewis A, Mehta S, Hanna LN, et al. Low serum levels of microRNA-19 are associated with a stricturing Crohn’s disease phenotype. Inflamm Bowel Dis. 2015;21:1926–1934.
Fasseu M, Tréton X, Guichard C, et al. Identification of restricted subsets of mature microRNA abnormally expressed in inactive colonic mucosa of patients with inflammatory bowel disease. PLoS ONE. 2010;10:e13160.
Zahm AM, Hand NJ, Tsoucas DM, Le Guen CL, Baldassano RN, Friedman JR. Rectal microRNAs are perturbed in pediatric inflammatory bowel disease of the colon. J Crohns Colitis. 2014;8:1108–1117.
Wu F, Guo NJ, Tian H, et al. Peripheral blood microRNAs distinguish active ulcerative colitis and Crohn’s disease. Inflamm Bowel Dis. 2011;17:241–250.
Zhang C, Zhao Z, Osman H, Watson R, Nalbantoglu I, Lin J. Differential expression of miR-31 between inflammatory bowel disease and microscopic colitis. Microrna. 2014;3:155–159.
Matijašić M, Meštrović T, Perić M, et al. Modulating composition and metabolic activity of the gut microbiota in IBD patients. Int J Mol Sci. 2016;17:578.
Coskun M, Bjerrum JT, Seidelin JB, Troelsen JT, Olsen J, Nielsen OH. miR-20b, miR-98, miR-125b-1*, and let-7e* as new potential diagnostic biomarkers in ulcerative colitis. World J Gastroenterol. 2013;19:4289–4299.
Koukos G, Polytarchou C, Kaplan JL, et al. A microRNA signature in pediatric ulcerative colitis: deregulation of the miR-4284/CXCL5 pathway in the intestinal epithelium. Inflamm Bowel Dis. 2015;21:996–1005.
Feng X, Wang H, Ye S, et al. Up-regulation of microRNA-126 may contribute to pathogenesis of ulcerative colitis via regulating NF-kappaB inhibitor IκBα. PLoS ONE. 2012;12:e52782.
Polytarchou C, Oikonomopoulos A, Mahurkar S, et al. Assessment of circulating microRNAs for the diagnosis and disease activity evaluation in patients with ulcerative colitis by using the nanostring technology. Inflamm Bowel Dis. 2015;21:2533–2539.
Krissansen GW, Yang Y, McQueen FM, et al. Overexpression of miR-595 and miR-1246 in the sera of patients with active forms of inflammatory bowel disease. Inflamm Bowel Dis. 2015;21:520–530.
Rogler G. Where are we heading to in pharmacological IBD therapy? Pharmacol Res. 2015;100:220–227.
Cheng X, Zhang X, Su J, et al. miR-19b downregulates intestinal SOCS3 to reduce intestinal inflammation in Crohn’s disease. Sci Rep. 2015;5:10397.
Chen Y, Wang C, Liu Y, et al. miR-122 targets NOD2 to decrease intestinal epithelial cell injury in Crohn’s disease. Biochem Biophys Res Commun. 2013;438:133–139.
Huang Z, Shi T, Zhou Q, et al. miR-141 Regulates colonic leukocytic trafficking by targeting CXCL12β during murine colitis and human Crohn’s disease. Gut. 2014;63:1247–1257.
Huang Z, Shi T, Zhou Q, et al. MicroRNA-146b improves intestinal injury in mouse colitis by activating nuclear factor-kappaB and improving epithelial barrier function. J Gene Med. 2013;15:249–260.
Zwiers A, Kraal L, Van de Pouw Kraan T, Wurdinger T, Bouma G, Kraal G. Cutting edge: a variant of the IL-23r gene associated with inflammatory bowel disease induces loss of microRNA regulation and enhanced protein production. J Immunol. 2012;4:1573–1577.
Van der Goten J, Vanhove W, Lemaire K, et al. Integrated miRNA and mRNA expression profiling in inflamed colon of patients with ulcerative colitis. PLoS ONE. 2014;12:e116117.
El-Gowelli HM, Saad EI, Abdel-Galil AG, Ibrahim ER. Co-administration of α-lipoic acid and cyclosporine aggravates colon ulceration of acetic acid-induced ulcerative colitis via facilitation of NO/COX-2/miR-210 cascade. Toxicol Appl Pharmacol. 2015;288:300–312.
Ludwig K, Fassan M, Mescoli C, et al. PDCD4/miR-21 dysregulation in inflammatory bowel disease-associated carcinogenesis. Virchows Arch. 2013;462:57–63.
Leva GD, Garofalo M, Croce CM. MicroRNAs in cancer. Annu Rev Pathol. 2014;9:287–314.
Sohn JJ, Schetter AJ, Yfantis HG, et al. Macrophages, nitric oxide and microRNAs are associated with DNA damage response pathway and senescence in inflammatory bowel disease. PLoS ONE. 2012;7:e44156.
Chen Y, Xiao Y, Ge W, et al. miR-200b inhibits TGF-b1-induced epithelial-mesenchymal transition and promotes growth of intestinal epithelial cells. Cell Death Dis. 2013;4:e541.
Olaru AV, Yamanaka S, Vazquez C, et al. MicroRNA-224 negatively regulates p21 expression during late neoplastic progression in inflammatory bowel disease. Inflamm Bowel Dis. 2013;19:471–480.
Necela BM, Carr JM, Asmann YW, Thompson EA. Differential Expression of microRNAs in tumors from chronically inflamed or genetic (APC Min/+) models of colon cancer. PLoS ONE. 2011;6:1–12.
Thomas J, Ohtsuka M, Pichler M, Ling H. MicroRNAs: clinical relevance in colorectal cancer. Int J Mol Sci. 2015;16:28063–28076.
Goel A. MicroRNAs as therapeutic targets in colitis and colitis-associated cancer: tiny players with a giant impact. Gastroenterology. 2015;149:859–861.
Polytarchou C, Hommes DW, Palumbo T, et al. MicroRNA214 is associated with progression of ulcerative colitis, and inhibition reduces development of colitis and colitis-associated cancer in mice. Gastroenterology. 2015;149:981–992.
Olaru AV, Selaru FM, Mori Y, et al. Dynamic changes in the expression of MicroRNA-31 during inflammatory bowel disease-associated neoplastic transformation. Inflamm Bowel Dis. 2011;17:221–231.
Kanaan Z, Rai SN, Eichenberger MR, et al. Differential microRNA expression tracks neoplastic progression in inflammatory bowel disease-associated colorectal cancer. Hum Mutat. 2012;33:551–560.
Chen G, Cao S, Liu F, Liu Y. miR-195 plays a role in steroid resistance of ulcerative colitis by targeting Smad7. Biochem J. 2015;471:357–367.
Fujioka S, Nakamichi I, Esaki M, Asano K, Matsumoto T, Kitazono T. Serum microRNA levels in patients with Crohn’s disease during induction therapy by infliximab. J Gastroenterol Hepatol. 2014;6:1207–1214.
Collins PD. Strategies for detecting colon cancer and dysplasia in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2013;19:860–863.
Benderska N, Dittrich AL, Knaup S, et al. miRNA-26b overexpression in ulcerative colitis-associated carcinogenesis. Inflamm Bowel Dis. 2015;21:2039–2051.
Bai J, Li Y, Shao T, et al. Integrating analysis reveals microRNA-mediated pathway crosstalk among Crohn’s disease, ulcerative colitis and colorectal cancer. Mol Biosyst. 2014;9:2317–2328.
Ueda Y, Ando T, Nanjo S, Ushijima T, Sugiyama T. DNA methylation of microRNA-124a is a potential risk marker of colitis-associated cancer in patients with ulcerative colitis. Dig Dis Sci. 2014;59:2444–2451.
Wan J, Xia L, Xu W, Lu N. Expression and function of miR-155 in diseases of the gastrointestinal tract. Int J Mol Sci. 2016;17:709.
Svrcek M, El-Murr N, Wanherdrick K, et al. Overexpression of microRNAs-155 and 21 targeting mismatch repair proteins in inflammatory bowel diseases. Carcinogenesis. 2013;34:828–834.
Tan YG, Zhang YF, Guo CJ, Yang M, Chen MY. Screening of differentially expressed microRNA in ulcerative colitis related colorectal cancer. Asian Pac J Trop Med. 2013;6:972–976.
Takagi T, Naito Y, Mizushima K, et al. Increased expression of microRNA in the inflamed colonic mucosa of patients with active ulcerative colitis. J Gastroenterol Hepatol. 2010;25:129–133.
Acknowledgments
This study was supported in part by grant from the National Natural Scientific Foundation of China (81171923) and grant from the State Key Laboratory of Cancer Biology (CBSKL2014Z13).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared that they have no conflicts of interest to this work.
Rights and permissions
About this article
Cite this article
Cao, B., Zhou, X., Ma, J. et al. Role of MiRNAs in Inflammatory Bowel Disease. Dig Dis Sci 62, 1426–1438 (2017). https://doi.org/10.1007/s10620-017-4567-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-017-4567-1