Abstract
Background
Circulating endothelial progenitor cells (EPCs) are bone marrow-derived stem cells able to migrate to sites of damaged endothelium and differentiate into endothelial cells. Altered EPC level and function have been described in various inflammatory diseases and have been shown to augment vasculogenesis in murine models. Previous studies of EPC in the context of Crohn’s disease (CD) have yielded conflicting results.
Aim
To determine whether the circulating levels of EPCs are changed in the context of CD.
Methods
CD patients and healthy controls were recruited. Disease activity was assessed by CDAI. Peripheral blood mononuclear cells were isolated and EPC numbers evaluated by FACS analysis using anti-CD34, anti-VEGF receptor-2, anti-CD133, and anti-CD45 markers.
Results
Eighty-three subjects, including 32 CD patients and 51 controls were recruited, including 19 (59.4 %) and 23 (45 %) males (p = 0.26), aged 34.8 ± 14.9 and 43.3 ± 18.5 years (p = 0.64), in cases and controls, respectively. Mean CDAI was 147 ± 97, disease duration was 12.7 ± 11.1 years, and 28 (87.5 %) were receiving biologics for a mean duration of 21.7 ± 16.8 months. The mean level of peripheral EPCs in CD patients was 0.050 ± 0.086 percent and 0.007 ± 0.013 % in controls (p < 0.01). There was no significant correlation between EPC levels and age (r = −0.13, p = 0.47), CDAI (r = −0.26, p = 0.15), disease duration (r = −0.04, p = 0.84), or duration of treatment with biologics (r = 0.004, p = 0.99).
Conclusion
EPCs are elevated in patients with CD. Further studies are needed to examine the function of EPCs and their possible role as a marker of disease severity or therapeutic response.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Crohn’s disease (CD) is a chronic disorder affecting the gastrointestinal tract, characterized by a pathological immune response to luminal antigens, leading to inflammation and endothelial damage in a genetically susceptible host [1]. Endothelial progenitor cells (EPCs) are bone marrow-derived hematopoietic stem cells which are recruited via the peripheral circulation to areas of endothelial damage. EPCs may have an important role in the pathophysiology and treatment of various inflammatory diseases, including lupus, rheumatoid arthritis, and vasculitis [2–4]. EPCs have also been evaluated for the treatment of myocardial ischemia and peripheral vascular disease [5, 6]. Understanding the role of EPCs in CD may be important in the context of disease pathogenesis, disease progression, and disease regression.
Previous studies investigating EPCs in the setting of CD have yielded conflicting results, and it is still unclear whether the absolute peripheral EPC number increases or decreases in the disease [7–9]. Previous studies are small and not adequately controlled for disease activity. EPCs might also warrant investigation in the context of CD treatment. Transplantation of stem cells, including mesenchymal stem cells, seems to be a promising therapeutic strategy due to their ability to selectively home into sites of endothelial injury where they exert immunosuppressive and tissue healing effects [10–12]. There have been no human studies investigating EPC transplantation in subjects with CD. However, EPC transplantation into fetal sheep has been performed, and EPCs have been demonstrate to migrate to the intestinal mucosa and contribution to vasculogenesis in this setting [13]. These results suggest that EPCs might have potential in inflammatory bowel disease (IBD) cellular therapy.
In the current study, we aim to determine whether the circulating levels of EPCs are changed in the context of CD and the relationship with disease activity.
Methods
Patient Recruitment
Consecutive patients with Crohn’s disease presenting to the inflammatory bowel disease clinic at Rabin Medical Center were prospectively recruited. Exclusion criteria for the study were: age < 18 years, atherosclerosis or peripheral vascular disease, prior malignancy, a history of chemotherapy or radiotherapy, renal insufficiency, hematologic disease, and liver disease. Patients with serious or systemic infections, those requiring immediate surgery, as well as female patients with a history of pregnancy in the last 12 months, were also excluded from the study. Sera were obtained at snap frozen at −80 °C. Patients also completed a detailed self-administered questionnaire regarding general medical and disease specific history. Answers were then cross-referenced for accuracy with data from the electronic medical records. Disease activity was assessed by the Crohn’s Disease Activity Index (CDAI). Healthy controls were recruited among hospital staff. All participants provided written informed consent. Approval for the study was granted by the Institutional Review Board at Rabin Medical Center.
Separation of Blood Leukocytes and Culture
Mononuclear cells were isolated by Ficoll density gradient centrifugation from 20-ml blood samples, and EPC-CFU was assayed after two platings and a 9-day culture on fibronectin-coated 24-well plates, as previously described [14]. Colonies were manually counted in 4 wells.
Flow Cytometry
A total of 1.5 × 106 cells were taken for FACS analysis. FACS analysis was performed with utilization of the following markers: CD45 PerCP-Cy5.5 (R&D Systems, Minneapolis, MN, USA), CD34 PE-Cy7 (R&D Systems, Minneapolis, MN), human phycoerythrin anti-vascular endothelial growth factor (VEGF) receptor-2 (R&D Systems, Minneapolis, MN, USA), and FITC-anti-CD133 (Miltenyi Biotec GmbH, Germany). Cells were incubated with the marker for 30 min in the presence of 100 µL Fluorescence-activated cell sorter staining buffer (FACS buffer) (phosphate-buffered saline and 2 % fetal calf serum) at 4 °C. Subsequently cells were washed with phosphate-buffered saline (PBS) and fixed with formaldehyde for up to 24 h prior to FACS reading. FACS analysis was performed with use of Calibur, Becton–Dickinson equipment, and CellQuest software (BD Bioscience) (Fig. 1). A total of 80,000 cells were counted at each FACS reading.
Statistical Analysis
Data analysis was performed using SPSS 21.0 statistical analysis software (SPSS Inc., Chicago, IL, USA). Continuous variables were reported as mean ± SD. Normality of distribution of continuous variables was assessed using the Kolmogorov–Smirnov test (cut off at p = 0.01). Categorical variables were described using frequency distributions and were presented as frequency [n (%)]. Depending on the distribution, continuous variables were compared across groups using one way analysis of variance (ANOVA) or the Kruskal–Wallis test. Pairwise, post hoc comparisons for significance across differences were assessed by Bonferroni’s test or the Mann–Whitney U. Categorical variables were compared across groups using the Chi-square test (exact as necessary). The Pearson’s correlation coefficient was used to test correlation between variables. All tests were two-sided and considered significant at p < 0.05.
Results
Patients
A total of 83 subjects including 32 CD patients [19 (59.4 %) males, age 34.8 ± 14.9 years] and 51 healthy controls [23 (45.1 %) males, age 43.3 ± 18.5 years] were included in the study. Patient characteristics are displayed in Table 1. Ancestry among CD subjects was reported as Middle Eastern in 8 (25.0 %), North African in 6 (18.8 %), Western European in 6 (18.8 %), Eastern European in 4 (12.5 %), and Former Soviet Union in 4 (12.5 %). Among CD subjects, mean BMI was 24.1 ± 5.2 kg/m2, 6 (18.8 %) were current smokers, disease duration was 12.7 ± 11.1 years, and disease distribution was colonic and ileocolonic in 11 (34.4 %) and 20 (62.5 %) patients, respectively. Mean CDAI was 147.2 ± 97.3. Twenty-eight (87.5 %) subjects were receiving biological therapy (all of whom were treated with infliximab at the time of inclusion, and the mean number of infusions was 10.9 ± 8.4). Twenty-one (65.6 %) subjects were receiving immunomodulators, and 1.3 ± 3.0 (mean ± SD) Crohn’s-related surgical procedures per subject had been performed.
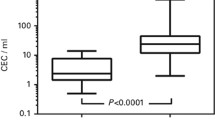
Circulating Levels of EPCs by Flow Cytometry
The percentage of EPCs in the peripheral white blood cells among subjects with CD was significantly higher than in healthy controls (0.050 ± 0.086 and 0.007 ± 0.013), respectively, p < 0.01 (Table 2; Fig. 2). There was no significant correlation between EPC levels and age (r = −0.13, p = 0.47), gender (t = 0.48, p = 0.64), CDAI (r = −0.26, p = 0.15), disease duration (r = −0.04, p = 0.84), duration of treatment with biologics (r = 0.004, p = 0.99), or smoking (t = 0.74, p = 0.47). Associations between patient and disease characteristics and circulating EPC levels among patients with Crohn’s disease are shown in Table 3.
Discussion
In our prospective, controlled cohort we found a higher percentage of EPCs in the circulating leukocytes of CD patients compared to healthy subjects. This is an important finding which adds to the limited and conflicted data previously published. There have been only four prior clinical studies investigating peripheral EPCs in the setting of IBD, and only three involving patients with CD [7–9, 15]. de Toni et al. [15] found that the number of circulating EPCs is reduced among patients with ulcerative colitis (UC), in both the acute and chronic stages of disease. A particular subset of EPCs expressing the CXCR4 antigen, which is specifically involved in cellular homing to areas of acute inflammation, was also found to be lower in subjects with acute UC compared to subjects with chronic UC and controls. Likewise, Garolla, et al. found that the number of circulating EPCs was significantly lower in UC patients than in CD patients and in controls. Similarly, the number of EPCs in CD patients was lower than in controls [7]. Masuda et al. found a reduction in EPC number among subjects with UC compared to subjects with CD, infectious colitis, and controls. The authors suggest that the reduction in peripheral EPC numbers may be due to the sequestration of circulating EPCs in inflamed intestinal vessels [9, 15]. An alternative explanation for reduced numbers of EPCs is impaired differentiation of hematopoietic progenitor cells (EPC precursors) into EPCs, particularly in the acute phase of disease. This hypothesis is supported by the presence of increased numbers of hematopoietic progenitor cells in UC [9].
In contrast, Masuda et al. [9] found no reduction in the circulating number of EPCs among CD patients when compared to controls, nor any correlation between EPC numbers and disease activity. Marlicz et al. [8] found significantly elevated levels of circulating EPCs in both UC and CD patients with active disease, which is consistent with the findings in our study. In addition to EPCs, the authors demonstrated that EPC precursors and pluripotent embryonic-like stem cells are heavily mobilized into peripheral blood in patients with IBD.
Our findings are consistent with mounting evidence that EPCs are directly involved in the regeneration of damaged epithelium. Recruitment of hematopoietic progenitor cells from the bone marrow is multifactorial and involves chemokines, growth factors, and bioactive lipids [16]. In murine models of colitis, transplantation of mesenchymal stem cells and adipose tissue-derived stem cells has been shown to promote intestinal recovery [17–19]. In humans, phase 1 and phase 2 studies have demonstrated feasibility, safety, and efficacy of autologous stem cell transplantation for the treatment of refractory CD and CD-related fistulas [20–22]. Nevertheless, no phase III trials have been published, and long-term data, where available, suggest that the rate of relapse following stem cell therapy is high [23]. Similarly, intravenously administered granulocyte–macrophage colony-stimulating factor (GM-CSF), a potent stimulator of hematopoiesis, has not demonstrated efficacy for the treatment of CD in vivo [24]. EPCs have not been studied specifically in the context of CD; however, in a fetal sheep model exogenously administered EPCs have a demonstrated capacity to migrate to the intestinal crypt region [13]. There have also been no reports of therapeutic use of embryonic or induced pluripotent stem cells in CD. Therefore, direct intravenous administration of stem cells, or of factors which increase EPC mobilization, deserve further study in the context of CD.
A major difference between our CD cohort and previous studies in which EPC were found to be unchanged or reduced is the high proportion of subjects receiving biological therapy (87 %) in our study. This could suggest that biological therapy is associated with recruitment of EPCs and endothelial repair and that increased peripheral EPC numbers could be an indicator of treatment response. Although we did not specifically find an association between biological therapy and EPC number (Table 3), it is likely that our study is underpowered to detect secondary endpoints.
Strengths of our study include the quality of our prospective cohort which included robust data on clinical variables. The number of subjects recruited is relatively high compared to previous cohorts. However, there are several limitations to our study. Firstly, our study lacks endoscopic and laboratory measures of disease activity which might be related to circulating EPCs. Nevertheless, we did include the CDAI which incorporates a laboratory-based criterion. Secondly, we did not assay tissue EPC levels, which might have been useful to better understand the pathophysiological processes at play. However, any tissue assay would have been subject to sampling bias. Thirdly, our study is likely to be underpowered to test for clinical and demographic associations of high circulating EPC levels, due to the low number of patients recruited and the low number of circulating EPCs in each blood sample. Finally, there has been a lack of consensus regarding the definition of EPC [25–27]. Nevertheless, for the past decade CD34+/CD133+/VEGF+ markers have been generally used. CD34 is a common stem cell marker, CD133 is a marker of early bone marrow production, and VEGF receptor-2 is a marker of endothelial precursors [28].
In conclusion, our study demonstrates that the level of circulating EPCs is increased in subjects with CD, regardless of disease activity. Future studies should further investigate whether the extent of EPC mobilization correlates with tissue damage or regeneration of damaged intestine, as well as the signaling pathways involved with endothelial repair. EPCs warrant further study both as a target for therapeutic intervention and as a marker of treatment response.
References
Sartor RB. Mechanisms of disease: pathogenesis of Crohn’s disease and ulcerative colitis. Nat Clin Pract Gastroenterol Hepatol. 2006;3:390–407.
Ablin JN, Boguslavski V, Aloush V, et al. Enhanced adhesive properties of endothelial progenitor cells (EPCs) in patients with SLE. Rheumatol Int. 2011;31:773–778.
Ablin JN, Boguslavski V, Aloush V, et al. Effect of anti-TNFalpha treatment on circulating endothelial progenitor cells (EPCs) in rheumatoid arthritis. Life Sci. 2006;79:2364–2369.
Závada J, Kideryová L, et al. Circulating endothelial progenitor cells in patients with ANCA-associated vasculitis. Kidney Blood Press Res. 2008;31:247–254.
Povsic TJ, Junge C, Nada A, et al. A phase 3, randomized, double-blinded, active-controlled, unblinded standard of care study assessing the efficacy and safety of intramyocardial autologous CD34+ cell administration in patients with refractory angina: design of the RENEW study. Am Heart J. 2013;165:854.e2–861.e2.
Losordo DW, Kibbe MR, Mendelsohn F, et al. A randomized, controlled pilot study of autologous CD34+ cell therapy for critical limb ischemia. Circ Cardiovasc Interv. 2012;5:821–830.
Garolla A, D’Incà R, Checchin D, et al. Reduced endothelial progenitor cell number and function in inflammatory bowel disease: a possible link to the pathogenesis. Am J Gastroenterol. 2009;104:2500–2507.
Marlicz W, Zuba-Surma E, Kucia M, Blogowski W, Starzynska T, Ratajczak MZ. Various types of stem cells, including a population of very small embryonic-like stem cells, are mobilized into peripheral blood in patients with Crohn’s disease. Inflamm Bowel Dis. 2012;18:1711–1722.
Masuda J, Mitsuyama K, Yamasaki H, et al. Depletion of endothelial progenitor cells in the peripheral blood of patients with ulcerative colitis. Int J Mol Med. 2007;19:221–228.
Burt RK, Craig RM, Milanetti F, et al. Autologous nonmyeloablative hematopoietic stem cell transplantation in patients with severe anti-TNF refractory Crohn disease. Blood. 2010;116:6123–6132.
Hawkey CJ, Allez M, Clark MM, et al. Autologous hematopoetic stem cell transplantation for refractory Crohn disease. JAMA. 2015;314:2524.
Griffin MD, Elliman SJ, Cahill E, English K, Ceredig R, Ritter T. Concise review: adult mesenchymal stromal cell therapy for inflammatory diseases: how well are we joining the dots? Stem Cells. 2013;31:2033–2041.
Wood JA, Colletti E, Mead LE, et al. Distinct contribution of human cord blood-derived endothelial colony forming cells to liver and gut in a fetal sheep model. Hepatology. 2012;56:1086–1096.
Hill JM, Zalos G, Halcox JP, et al. Circulating endothelial progenitor cells, vascular function, and cardiovascular risk. N Engl J Med. 2003;348:593–600.
de Toni L, Di Nisio A, Magagna S, et al. Altered chemokine signalling in endothelial progenitor cells from acute ulcerative colitis patients. Gastroenterol Res Pract. 2015;2015:843980.
Ratajczak MZ, Lee H, Wysoczynski M, et al. Novel insight into stem cell mobilization-plasma sphingosine-1-phosphate is a major chemoattractant that directs the egress of hematopoietic stem progenitor cells from the bone marrow and its level in peripheral blood increases during mobilization due to activation of complement cascade/membrane attack complex. Leukemia. 2010;24:976–985.
Tanaka H, Arimura Y, Yabana T, et al. Myogenic lineage differentiated mesenchymal stem cells enhance recovery from dextran sulfate sodium-induced colitis in the rat. J Gastroenterol. 2011;46:143–152.
Ando Y, Inaba M, Sakaguchi Y, et al. Subcutaneous adipose tissue-derived stem cells facilitate colonic mucosal recovery from 2,4,6-trinitrobenzene sulfonic acid (TNBS)-induced colitis in rats. Inflamm Bowel Dis. 2008;14:826–838.
González MA, Gonzalez-Rey E, Rico L, Büscher D, Delgado M. Adipose-derived mesenchymal stem cells alleviate experimental colitis by inhibiting inflammatory and autoimmune responses. Gastroenterology. 2009;136:978–989.
Garcia-Olmo D, Herreros D, Pascual I, et al. Expanded adipose-derived stem cells for the treatment of complex perianal fistula: a phase II clinical trial. Dis Colon Rectum. 2009;52:79–86.
García-Olmo D, García-Arranz M, Herreros D, Pascual I, Peiro C, Rodríguez-Montes JA. A phase I clinical trial of the treatment of Crohn’s fistula by adipose mesenchymal stem cell transplantation. Dis Colon Rectum. 2005;48:1416–1423.
Duijvestein M, Vos ACW, Roelofs H, et al. Autologous bone marrow-derived mesenchymal stromal cell treatment for refractory luminal Crohn’s disease. Gut. 2010;59:1662–1669.
Guadalajara H, Herreros D, De-La-Quintana P, Trebol J, Garcia-Arranz M, Garcia-Olmo D. Long-term follow-up of patients undergoing adipose-derived adult stem cell administration to treat complex perianal fistulas. Int J Colorectal Dis. 2012;27:595–600.
Korzenik JR, Dieckgraefe BK, Valentine JF, Hausman DF, Gilbert MJ. Sargramostim for active Crohn’s disease. N Engl J Med. 2005;352:2193–2201.
Case J, Mead Le, Bessler WK, et al. Human CD34+AC133+VEGFR-2+ cells are not endothelial progenitor cells but distinct, primitive hematopoietic progenitors. Exp Hematol. 2007;35:1109–1118.
Gehling UM, Ergün S, Schumacher U, et al. In vitro differentiation of endothelial cells from AC133-positive progenitor cells. Blood. 2000;95:3106–3112.
Masuda H, Alev C, Akimaru H, et al. Methodological development of a clonogenic assay to determine endothelial progenitor cell potential. Circ Res. 2011;109:20–37.
Ingram DA. Unresolved questions, changing definitions, and novel paradigms for defining endothelial progenitor cells. Blood. 2005;106:1525–1531.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Boltin, D., Kamenetsky, Z., Perets, T.T. et al. Circulating Bone Marrow-Derived CD45−/CD34+/CD133+/VEGF+ Endothelial Progenitor Cells in Adults with Crohn’s Disease. Dig Dis Sci 62, 633–638 (2017). https://doi.org/10.1007/s10620-016-4234-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-016-4234-y