Abstract
Background
Diabetes and dyslipidemia have been linked to an increased risk of colorectal neoplasm (CRN). However, previous studies evaluating these associations have shown inconsistent results, and large-scale studies are few in number.
Aim
To investigate the associations between the parameters of glucose and lipid metabolism and the presence of CRN.
Methods
A cross-sectional study was performed on 38,490 Korean adults aged ≥30 years undergoing their first colonoscopy as part of routine preventive health care between 2010 and 2011.
Results
The prevalence of overall CRN increased with increasing levels of glucose, hemoglobin A1c (HbA1c), insulin, homeostasis model assessment of insulin resistance (HOMA-IR), triglycerides, total cholesterol, low-density lipoprotein cholesterol (LDL-C), and apolipoprotein B (ApoB) and with decreasing level of apolipoprotein A1 (ApoA1). The adjusted prevalence ratios for overall CRN comparing the fourth with the first quartiles of fasting glucose, HbA1c, insulin, HOMA-IR, triglycerides, total cholesterol, LDL-C, ApoB, and ApoA-1 were 1.83 (95 % CI 1.62–2.06), 1.17 (95 % CI 1.03–1.33), 1.09 (95 % CI 0.97–1.23), 1.22 (95 % CI 1.08–1.37), 1.31 (95 % CI 1.16–1.48), 1.19 (95 % CI 1.07–1.33), 1.38 (95 % CI 1.23–1.54), 1.30 (95 % CI 1.14–1.47), and 0.85 (95 % CI 0.76–0.95), respectively. There was also a significant association between higher levels of glucose, LDL-C, and ApoB with a higher prevalence of advanced CRN. Moreover, the risk of CRN increased further in cases in which the parameters of glucose metabolism and lipid metabolism worsened simultaneously.
Conclusions
The levels of parameters of glucose and lipid metabolism are significantly associated with the prevalence of CRN. Altered glucose and lipid metabolism may contribute to the development of CRN.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is the third most common cancer in males and the second in females worldwide, accounting for 8 % of all cancer deaths, making it the fourth most common cause of death from cancer [1]. Moreover, the incidence of CRC is rapidly increasing, especially in Asian countries including Korea [2–5]. The substantial interest in identifying potentially modifiable risk factors, such as cigarette smoking, diabetes, hyperlipidemia, and obesity, have kept pace with the increase in incidence of CRC.
Diabetes [6, 7] and metabolic syndrome [8–11] have been linked to an increased risk of colorectal neoplasm (CRN). A meta-analysis study in which 29 articles were analyzed showed that the risk of individuals with diabetes to develop CRC is 1.22 times higher than that of individuals without diabetes [6]. In addition, previous studies have reported that high fasting glucose level [12, 13], hemoglobin A1c (HbA1c) [13], insulin level [12, 14], and a high homeostasis model assessment of insulin resistance (HOMA-IR) [13, 15] were associated with an increased risk of colorectal adenomas. Dyslipidemia is also an important component of metabolic syndrome. Several studies have demonstrated that hypertriglyceridemia [9, 11, 16–18], high total cholesterol level [16, 17], high low-density lipoprotein cholesterol (LDL-C) level [19], and low high-density lipoprotein cholesterol (HDL-C) level [11, 19, 20] were associated with an increased risk of CRN. These results suggest that diabetes and dyslipidemia may contribute to colorectal carcinogenesis through insulin resistance/hyperinsulinemia, hyperglycemia, oxidative stress, and inflammatory pathways [20, 21]. However, most of these studies included a relatively small number of subjects, and the results were inconsistent [22, 23]. Therefore, the aim of the present study was to investigate the associations between the parameters of glucose and lipid metabolism (including lipoproteins as well as lipids) and the risk of CRN in a very large sample of asymptomatic examinees attending a health screening program.
Patients and Methods
Study Population
The study population consisted of examinees who had undergone a colonoscopy as part of a comprehensive health screening program at the Total Healthcare Center of Kangbuk Samsung Hospital, Seoul and Suwon, Korea, between 2010 and 2011 (N = 62,171) [24]. In Korea, the Industrial Safety and Health Law requires employees to participate in annual or biennial health examinations. Approximately 60 % of the participants were employees of various companies and local governmental organizations or their spouses, and the remaining participants registered individually for the program.
The setting of the study was a medical examination center, not a clinic. Before the colonoscopy, interviews by general practitioners were conducted to ensure that all of the screened individuals were asymptomatic (i.e., no lower abdominal pain or hematochezia). Subjects experiencing symptoms were urged to seek medical care.
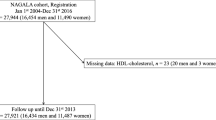
We only included subjects who were undergoing their first colonoscopy screening. Exclusion criteria were as follows: a history of prior colonic examination, colorectal surgery, or colorectal neoplasia (n = 12,205); a history of IBD (n = 225); an incomplete colonoscopy such as poor bowel preparation (n = 5692) or a colonoscopy in which the cecum was not reached (n = 48); lack of an adequate biopsy (n = 667); incomplete questionnaire answers (n = 4488); missing data on anthropometry (n = 206); and 20–29 years of age (n = 150). Some individuals met more than one criterion for exclusion. The total number of potential participants for the study was 38,490 (Fig. 1).
This study was approved by the Institutional Review Board of Kangbuk Samsung Hospital, which exempted the requirement for informed consent due to retrospective access of de-identified data.
Measurements and Definitions
Data on medical history and smoking were collected through a self-administered questionnaire, whereas physical measurements and serum biochemical parameters were measured by trained staff. The amount of smoking (pack-years) was assessed. Family history of CRC was defined as CRC in one or more first-degree relatives at any age. Self-reported use of aspirin (regular use over the past month) was assessed. History of diabetes was defined as a self-reported diagnosis of diabetes or history of use of anti-diabetic medication. History of dyslipidemia was defined as a self-reported diagnosis of dyslipidemia or history of use of medication for dyslipidemia. Body mass index (BMI) was calculated by dividing measured weight (kg) by height squared (m2).
Blood samples were collected from the antecubital vein after at least a 10-h fast. Fasting glucose level was measured using the hexokinase method (Hitachi Modulator D2400; Roche, Tokyo, Japan). HbA1c was measured using an immunoturbidimetric assay with a Cobra Integra 800 automatic analyzer (Roche Diagnostics, Basel, Switzerland) at a reference value of 4.4–6.4 %. Fasting serum insulin was measured by electrochemiluminescence immunoassay (Hitachi Modular E 170; Roche, Tokyo, Japan). Insulin resistance was assessed with HOMA-IR according to the following equation: fasting blood insulin (mU/mL) × fasting blood glucose (mmol/L)/22.5. Serum levels of total cholesterol and triglycerides were determined using an enzymatic colorimetric assay; LDL-C and HDL-C levels were determined using a homogeneous enzymatic colorimetric assay; serum apolipoprotein A1 (ApoA1) and apolipoprotein B (ApoB) levels were determined using an immunoturbidimetric assay.
Colonoscopy and Histologic Examination
Colonoscopy was performed by 1 of 13 experienced gastroenterologists using EVIS LUCERA CV-260 colonoscope (Olympus). All bowel cleansing was performed using 4 L of polyethylene glycol solution. All polypoid lesions were biopsied or removed and histologically assessed by experienced pathologists.
Polyps were classified by number, size, and histologic characteristics (tubular, tubulovillous, or villous adenoma; hyperplastic polyp; sessile serrated adenoma or traditional serrated adenoma). Hyperplastic polyps, inflammatory polyps, and lipomas were considered to be normal findings. The grade of dysplasia was classified as low or high. A neoplasm was defined as a cancer or adenoma. An advanced neoplasm was defined as a cancer or high-risk adenoma that was defined as any adenoma larger than 1 cm, three or more adenomas, any adenoma with a villous component, or high-grade dysplasia [25]. Many studies support that patients with three or more adenomas have a higher risk of advanced neoplasia [26–28]. Therefore, individuals with three or more adenomas were considered to have an advanced neoplasm. For patients with multiple neoplasms, the most advanced lesion was reported (e.g., adenoma with the largest diameter or the most dysplastic histology).
Statistical Analysis
The Chi-square test for categorical variables and t test or Mann–Whitney U test for continuous variables were used to compare differences in descriptive statistics between the no CRN and CRN groups (any CRN, non-advanced CRN, and advanced CRN).
The study end point was the prevalence of CRN, recorded as one of the three categories: any CRN, non-advanced CRN, and advanced CRN. Robust Poisson regression was used to model the associations of the individual glucose and lipid markers with the prevalence of any CRN, non-advanced CRN, and advanced CRN. We calculated prevalence ratios and 95 % confidence intervals (CIs) of CRN by comparing quartiles 2–4 of markers of glucose and lipid metabolism with the first quartile. In regression analyses, we fitted three models for each marker of glucose and lipid metabolism: a crude model, a model adjusted for age and sex, and a model further adjusted for smoking status, family history of CRC, use of aspirin, BMI, history of diabetes (only in markers of lipid metabolism), and history of dyslipidemia (only in markers of glucose metabolism).
Two-sided P values <0.05 were considered to be statistically significant. Statistical analyses were performed using Stata version 13.0 (StataCorp LP, College Station, TX, USA).
Results
Study Population: Comparisons Between No CRN and Other CRN Groups
A total of 38,490 participants were eligible for analysis (Fig. 1). Average age of the study participants was 41.4, and the proportion of males was 73 %. The prevalence rate of overall CRN, non-advanced CRN, and advanced CRN was 7.4 % (n = 2863), 6.3 % (n = 2421), and 1.1 % (n = 442), respectively. A total of 23 CRCs (0.06 %) were detected in the study population. The prevalence of CRN was significantly higher among older participants, males, current or ex-smokers, and among subjects with diabetes, dyslipidemia, and a higher BMI. Compared with participants without any CRN, those with CRN had higher levels of serum fasting glucose, insulin, HbA1c, HOMA-IR, triglycerides, total cholesterol, LDL-C, and ApoB and lower levels of serum HDL-C and ApoA-1 (Table 1).
Associations Between Parameters of Glucose Metabolism and Risk of CRN
The prevalence of overall CRN, non-advanced CRN, and advanced CRN increased linearly with increasing quartiles of fasting glucose, HbA1c, insulin, and HOMA-IR (Table 2). In multivariable-adjusted models, the associations between markers of glucose metabolism and prevalence of overall CRN weakened slightly but remained significant for all markers. The prevalence ratios for overall CRN comparing the fourth with the first quartiles of fasting glucose, HbA1c, insulin, and HOMA-IR were 1.83 (95 % CI 1.62–2.06; P trend < 0.001), 1.17 (95 % CI 1.03–1.33; P trend < 0.001), 1.09 (95 % CI 0.97–1.23; P trend = 0.041), and 1.22 (95 % CI 1.08–1.37; P trend < 0.001), respectively. Similar associations were seen for non-advanced CRN except for insulin, while the prevalence of advanced CRN was associated with only glucose level. The prevalence of advanced CRN comparing the fourth with the first quartiles of glucose was 1.53 (95 % CI 1.14–2.07; P trend = 0.002) (Supplementary Table 1).
Associations Between Parameters of Lipid Metabolism and Risk of CRN
The prevalence of overall CRN, non-advanced CRN, and advanced CRN increased linearly with increasing quartiles of triglycerides, total cholesterol, LDL-C, and ApoB, whereas it decreased linearly with increasing quartiles of HDL-C and ApoA-1 (Table 3). In multivariable-adjusted models, the associations between markers of lipid metabolism and prevalence of overall CRN weakened slightly but remained significant for all markers except for HDL-C. The prevalence ratios for overall CRN comparing the fourth with the first quartiles of triglycerides, total cholesterol, LDL-C, ApoB, ApoA-1, and HDL-C were 1.31 (95 % CI 1.16–1.48; P trend < 0.001), 1.19 (95 % CI 1.07–1.33; P trend < 0.001), 1.38 (95 % CI 1.23–1.54; P trend < 0.001), 1.30 (95 % CI 1.14–1.47; P trend < 0.001), 0.85 (95 % CI 0.76–0.95; P trend = 0.008), and 1.11 (95 % CI 0.99–1.24; P trend = 0.235), respectively. Similar associations were seen for non-advanced CRN, while the prevalence of advanced CRN was associated with only LDL-C and ApoB levels. The prevalence ratios for advanced CRN comparing the fourth with the first quartiles of LDL-C and ApoB were 1.42 (95 % CI 1.08–1.86; P trend = 0.016) and 1.49 (95 % CI 1.07–2.09; P trend = 0.045), respectively (Supplementary Table 2).
Prevalence of CRN with Increasing Parameters of Both Glucose and Lipid Metabolism
We sought to identify whether the risk of CRN further increases in cases in which parameters of glucose metabolism and lipid metabolism worsen simultaneously. Prevalence ratios were adjusted for age, sex, smoking status, family history of CRC, aspirin use, BMI, and interaction effects of glucose and lipid parameters. The adjusted prevalence ratios of overall CRN increased with increasing quartiles of both glucose and lipid parameters including triglycerides (Fig. 2a), LDL (Fig. 2b), and ApoB (Fig. 2c). The prevalence ratios for overall CRN comparing the fourth with the first quartiles of both glucose and lipid parameters including triglycerides, LDL, and ApoB were 1.94 (95 % CI 1.59–2.37, P < 0.001), 2.41 (95 % CI 1.89–3.08, P < 0.001), and 2.30 (95 % CI 1.78–2.98, P < 0.001), respectively.
Adjusted prevalence ratios for colorectal neoplasm by quartiles of glucose and lipid parameters [TG (a), LDL (b), and ApoB (c)]. Prevalence ratios were adjusted for age, sex, smoking status, family history of colorectal cancer, aspirin use, BMI, and interaction effects of glucose and lipid parameters. FBG fasting blood glucose, TG triglycerides, LDL low-density lipoprotein, ApoB apolipoprotein B, CRN colorectal neoplasm, PR prevalence ratio
Discussion
In this large cross-sectional study, we found that levels of parameters of glucose and lipid metabolism were associated with the prevalence of CRN. The prevalence of overall CRN increased with increasing levels of glucose, HbA1c, insulin, HOMA-IR, triglycerides, total cholesterol, LDL-C, and ApoB and with decreasing levels of HDL-C and ApoA-1. These associations, with the exception of HDL-C, persisted after adjusting for multiple risk factors for CRN. In addition, higher levels of glucose, LDL-C, and ApoB were significantly associated with an increasing prevalence of advanced CRN. Furthermore, the risk of CRN further increased in cases in which the parameters of glucose metabolism (including glucose) and lipid metabolism (including triglycerides, LDL-C, and ApoB) worsened simultaneously.
Although the mechanisms linking altered glucose metabolism, dyslipidemia, and CRN risk are not fully understood, there are several possible explanations. First, hyperinsulinemia has been reported to promote carcinogenesis through the effect of insulin-like growth factor 1 (IGF-1). Insulin reduces the production of IGF binding protein 1 and consequently increases the level of bioactive IGF-1. IGF-1 has mitogenic and anti-apoptotic activities and can act as a stimulus for growing preneoplastic and neoplastic cells [21]. Second, hyperglycemia and dyslipidemia can promote the formation of reactive oxygen species (ROS), which can damage DNA and trigger cancer progression by the modulation of gene expression, mutation, and chromosomal rearrangement [29]. Third, glucose and/or triglycerides may contribute to colorectal carcinogenesis through an increase in bile acids or energy supply to neoplastic cells [30]. Fourth, dyslipidemia can also increase the production of inflammatory cytokines such as interleukin-6 and tumor necrosis factor-α, creating a protumorigenic environment [31].
Several, but not all, studies have found associations between the parameters of glucose and lipid metabolism and the risk of CRN. Previous studies have reported that high fasting glucose level [12, 13], HbA1c [13, 32, 33], insulin level [12, 14, 34], and HOMA-IR [13, 15, 34] were associated with an increased risk of colorectal adenoma. On the other hand, a few studies have shown no statistically significant associations among HbA1c [22, 23, 35] and insulin level [36] and risk of CRN.
With regard to lipid parameters, research has been conducted on the association between triglycerides and CRN, but the results are inconsistent. In the Metabolic Syndrome and Cancer Project (Me-Can), higher serum triglyceride level was associated with risk of CRC in men of a large European cohort (n = 578,700) [10]. An association between triglyceride level and colorectal adenoma has also been observed in some Asian [9, 11, 18, 37, 38] and European populations [16]. However, the European Prospective Investigation into Cancer and Nutrition (EPIC), composed of a cohort of 521,448 participants [20], and an American study [39] did not confirm an association between triglyceride level and CRC.
We also found that increasing levels of total cholesterol, LDL-C, and ApoB and decreasing levels of HDL-C and ApoA-1 were associated with an increased risk of CRN, although the association with HDL-C did not persist after adjusting for multiple risk factors for CRN. There have been very few studies on the associations between total cholesterol, its fractions, or apolipoproteins, and CRN. Similar to our results, several previous studies have reported that high total cholesterol level [10, 16, 17], high LDL-C level [19], and low HDL-C level [11, 19] were associated with an increased risk of CRN. Also, in the EPIC study, concentrations of HDL-C and ApoA were associated with lower risk of CRC, while total cholesterol level was inversely associated with CRC risk, and there was no association between ApoB level and CRC risk [20]. In contrast to our results, another Korean study showed that higher levels of ApoA-1 and HDL-C were associated with an increased prevalence of colorectal adenomas [18].
To date, most of the studies on the association between altered glucose and/or lipid metabolism and CRN risk have included a relatively small number of subjects or were limited by lack of adjustment for CRN risk factors. These limitations may be contributing to the discrepancy of results among studies. Although there have been a few large-scale studies about CRC such as Me-Can and EPIC, there have been very few large-scale studies about colorectal adenoma. To the best of our knowledge, our study included the largest number of patients (n = 38,490) on colorectal adenoma. Similar to our study, two recent studies, which were conducted in a Korean medical center, investigated the associations of markers of glucose and lipid metabolism with the prevalence of colorectal adenoma in a large number of persons (approximately 19,000) and confirmed the association between high levels of markers of glucose and triglycerides and colorectal adenoma [13, 18]. However, our study had several additional strengths compared to that study. First, our study included a larger number of subjects. Second, no final participants had missing data in our study, while the previous study included participants with missing data; 49 % of their study population did not have information on apolipoproteins. Finally, our study included only subjects who underwent their first colonoscopy screening, whereas the previous study did not exclude subjects with a history of prior colonic examination, although they adjusted for history of polyps. These limitations may have resulted in unexpected ApoA-1 and HDL-C findings.
Another uniqueness of our study is that our cohort included a relatively young population. The mean age of the study participants was 41 years, and most of the study participants were younger than 50 years of age (44 % were 30–39 years old, and 43 % were 40–49 years old). This is the reason why the prevalence of CRN is low in our study. However, this unique quality of our cohort made it possible to determine that altered glucose metabolism, dyslipidemia, and dyslipoproteinemia are associated with a risk of CRN in a young population. Furthermore, this is the first study to demonstrate that the risk of CRN further increased if both glucose and lipid parameters worsened simultaneously. Healthy lifestyles and eating habits in younger adults may be important for the prevention of CRC. In addition, our study showed that the associations of the parameters of glucose and lipid metabolism with CRN were within the normal ranges. Our results suggest that the risk of CRN may increase early in insulin resistance and in the chain of altered glucose and lipid metabolism.
The current study had several limitations. First, this was not a population-based study but rather was a retrospective study that included a cohort composed of ethnic Korean individuals who had been seen for a regular health maintenance examination in two centers. As a result, there was likely some degree of selection bias. Interpretation of our findings requires careful consideration when applied to other populations or settings. Second, data on dietary, economic, and occupational factors, which could be possible confounders, were not available. Finally, the cross-sectional design precludes the determination of causality because temporality cannot be established.
In conclusion, higher levels of glucose, HbA1c, insulin, HOMA-IR, triglycerides, total cholesterol, and LDL-C and lower levels of ApoB were associated with an increased prevalence of overall CRN. There was also a significant association between higher levels of glucose, LDL-C, and ApoB and a higher prevalence of advanced CRN. Moreover, the risk of CRN was further increased if both glucose and lipid parameters worsened simultaneously. Our study provides strong evidence that altered glucose and lipid metabolism play a role in colorectal carcinogenesis. Considering that glucose and lipid levels are modifiable via lifestyle changes or medications, our study will contribute to CRC prevention strategies.
References
Ferlay J, Shin HR, Bray F, et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–2917.
Kim ER, Kim YH. Clinical application of genetics in management of colorectal cancer. Intest Res. 2014;12:184–193.
Sung JJ, Lau JY, Young GP, et al. Asia Pacific consensus recommendations for colorectal cancer screening. Gut. 2008;57:1166–1176.
Cha JM. Colonoscopy quality is the answer for the emerging issue of interval cancer. Intest Res. 2014;12:110–116.
Cha JM. Would you recommend screening colonoscopy for the very elderly? Intest Res. 2014;12:275–280.
Wu L, Yu C, Jiang H, et al. Diabetes mellitus and the occurrence of colorectal cancer: an updated meta-analysis of cohort studies. Diabetes Technol Ther. 2013;15:419–427.
Luo W, Cao Y, Liao C, et al. Diabetes mellitus and the incidence and mortality of colorectal cancer: a meta-analysis of 24 cohort studies. Colorectal Dis. 2012;14:1307–1312.
Wang YY, Lin SY, Lai WA, et al. Association between adenomas of rectosigmoid colon and metabolic syndrome features in a Chinese population. J Gastroenterol Hepatol. 2005;20:1410–1415.
Kim BC, Shin A, Hong CW, et al. Association of colorectal adenoma with components of metabolic syndrome. Cancer Causes Control. 2012;23:727–735.
Stocks T, Lukanova A, Bjorge T, et al. Metabolic factors and the risk of colorectal cancer in 580,000 men and women in the metabolic syndrome and cancer project (Me-Can). Cancer. 2011;117:2398–2407.
Liu CS, Hsu HS, Li CI, et al. Central obesity and atherogenic dyslipidemia in metabolic syndrome are associated with increased risk for colorectal adenoma in a Chinese population. BMC Gastroenterol. 2010;10:51.
Keku TO, Lund PK, Galanko J, et al. Insulin resistance, apoptosis, and colorectal adenoma risk. Cancer Epidemiol Biomark Prev. 2005;14:2076–2081.
Rampal S, Yang MH, Sung J, et al. Association between markers of glucose metabolism and risk of colorectal adenoma. Gastroenterology. 2014;147:78.e73–87.e73.
Vidal AC, Lund PK, Hoyo C, et al. Elevated C-peptide and insulin predict increased risk of colorectal adenomas in normal mucosa. BMC Cancer. 2012;12:389.
Ortiz AP, Thompson CL, Chak A, et al. Insulin resistance, central obesity, and risk of colorectal adenomas. Cancer. 2012;118:1774–1781.
Misciagna G, De Michele G, Guerra V, et al. Serum fructosamine and colorectal adenomas. Eur J Epidemiol. 2004;19:425–432.
Yamada K, Araki S, Tamura M, et al. Relation of serum total cholesterol, serum triglycerides and fasting plasma glucose to colorectal carcinoma in situ. Int J Epidemiol. 1998;27:794–798.
Yang MH, Rampal S, Sung J, et al. The association of serum lipids with colorectal adenomas. Am J Gastroenterol. 2013;108:833–841.
Bayerdorffer E, Mannes GA, Richter WO, et al. Decreased high-density lipoprotein cholesterol and increased low-density cholesterol levels in patients with colorectal adenomas. Ann Intern Med. 1993;118:481–487.
van Duijnhoven FJ, Bueno-De-Mesquita HB, Calligaro M, et al. Blood lipid and lipoprotein concentrations and colorectal cancer risk in the European Prospective Investigation into Cancer and Nutrition. Gut. 2011;60:1094–1102.
Shikata K, Ninomiya T, Kiyohara Y. Diabetes mellitus and cancer risk: review of the epidemiological evidence. Cancer Sci. 2013;104:9–14.
Platz EA, Hankinson SE, Rifai N, et al. Glycosylated hemoglobin and risk of colorectal cancer and adenoma (United States). Cancer Causes Control. 1999;10:379–386.
Tsilidis KK, Brancati FL, Pollak MN, et al. Metabolic syndrome components and colorectal adenoma in the CLUE II cohort. Cancer Causes Control. 2010;21:1–10.
Yun KE, Chang Y, Jung HS, et al. Impact of body mass index on the risk of colorectal adenoma in a metabolically healthy population. Cancer Res. 2013;73:4020–4027.
Lieberman DA, Rex DK, Winawer SJ, et al. Guidelines for colonoscopy surveillance after screening and polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2012;143:844–857.
Martinez ME, Baron JA, Lieberman DA, et al. A pooled analysis of advanced colorectal neoplasia diagnoses after colonoscopic polypectomy. Gastroenterology. 2009;136:832–841.
Saini SD, Kim HM, Schoenfeld P. Incidence of advanced adenomas at surveillance colonoscopy in patients with a personal history of colon adenomas: a meta-analysis and systematic review. Gastrointest Endosc. 2006;64:614–626.
Lieberman DA, Weiss DG, Harford WV, et al. Five-year colon surveillance after screening colonoscopy. Gastroenterology. 2007;133:1077–1085.
Cowey S, Hardy RW. The metabolic syndrome: A high-risk state for cancer? Am J Pathol. 2006;169:1505–1522.
McKeown-Eyssen G. Epidemiology of colorectal cancer revisited: are serum triglycerides and/or plasma glucose associated with risk? Cancer Epidemiol Biomark Prev. 1994;3:687–695.
Esteve E, Ricart W, Fernandez-Real JM. Dyslipidemia and inflammation: an evolutionary conserved mechanism. Clin Nutr. 2005;24:16–31.
Hsu YC, Chiu HM, Liou JM, et al. Glycated hemoglobin A1c is superior to fasting plasma glucose as an independent risk factor for colorectal neoplasia. Cancer Causes Control. 2012;23:321–328.
Kim BJ, Kim YH, Sinn DH, et al. Clinical usefulness of glycosylated hemoglobin as a predictor of adenomatous polyps in the colorectum of middle-aged males. Cancer Causes Control. 2010;21:939–944.
Sasaki Y, Takeda H, Sato T, et al. Serum Interleukin-6, insulin, and HOMA-IR in male individuals with colorectal adenoma. Clin Cancer Res. 2012;18:392–399.
Wei EK, Ma J, Pollak MN, et al. C-peptide, insulin-like growth factor binding protein-1, glycosylated hemoglobin, and the risk of distal colorectal adenoma in women. Cancer Epidemiol Biomark Prev. 2006;15:750–755.
Nishii T, Kono S, Abe H, et al. Glucose intolerance, plasma insulin levels, and colon adenomas in Japanese men. Jpn J Cancer Res. 2001;92:836–840.
Otani T, Iwasaki M, Ikeda S, et al. Serum triglycerides and colorectal adenoma in a case–control study among cancer screening examinees (Japan). Cancer Causes Control. 2006;17:1245–1252.
Sun ZJ, Huang YH, Wu JS, et al. The association of serum lipids with the histological pattern of rectosigmoid adenoma in Taiwanese adults. BMC Gastroenterol. 2011;11:54.
Saydah SH, Platz EA, Rifai N, et al. Association of markers of insulin and glucose control with subsequent colorectal cancer risk. Cancer Epidemiol Biomark Prev. 2003;12:412–418.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Jung, Y.S., Ryu, S., Chang, Y. et al. Associations Between Parameters of Glucose and Lipid Metabolism and Risk of Colorectal Neoplasm. Dig Dis Sci 60, 2996–3004 (2015). https://doi.org/10.1007/s10620-015-3713-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-015-3713-x