Abstract
Objective
To investigate which glycemic index is more strongly associated with colorectal neoplasia.
Method
This cross-sectional study enrolled 2,776 participants in a comprehensive health management program which included measurement of fasting plasma glucose and HbA1c, along with screening colonoscopy. Primary outcome was colorectal adenoma with or without dysplasia. Risk factors for colorectal neoplasia were determined by the multivariate regression analysis, which evaluated the interrelationship among different glycemic indices in a hierarchical way.
Results
Colorectal neoplasms were found in 605 (21.79%) examinees, 68 (2.45%) of whom had high-risk tumors. Glycemic indices including diagnosis of diabetes mellitus, fasting plasma glucose, and HbA1c were all associated with colorectal tumors in the univariate analysis. However, HbA1c outperformed the other two markers as an independent risk factor (adjusted odds ratio, 1.22; 95% confidence interval, 1.10–1.36%) for colorectal neoplasia. Moreover, only HbA1c remained independently associated with colorectal tumor after patients with established diagnosis of diabetes (n = 132) were excluded. We also identified age, male gender, and smoking were independent risk factors for colorectal neoplasia.
Conclusion
HbA1c as compared with fasting plasma glucose is more strongly and independently associated with colorectal neoplasia. Further research is warranted to elucidate the value of HbA1c in stratifying risk of colorectal cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer is a leading cause of morbidity and mortality in the West and has become more and more prevalent in the developed Asia [1, 2]. Since most colorectal cancers transform from adenomatous polyps [3], and endoscopic removal of colorectal adenoma and early cancer has been proven effective for cancer prevention [4], it is imperative to identify risk factors for colorectal neoplasia. Although epidemiological surveys have identified diabetes mellitus (DM) as a risk factor for colorectal cancer [5, 6], studies that investigated association between different markers of hyperglycemia and colorectal neoplasia reported conflicting results [7–16]. It remains unknown which glycemic index is a more robust and independent risk factor for colorectal neoplasia. Specifically, glycated hemoglobin (HbA1c) has not been compared directly against fasting plasma glucose (FPG) in assessing risk of colorectal neogrowth.
HbA1c is a validated biomarker that reflects average concentration of blood glucose over the preceding 6–8 weeks [17]. It has been recommended as the major indicator for monitoring glucose control in diabetic patients [18] and has been adopted by the American Diabetes Association as one of the diagnostic tests for DM, which historically depended exclusively on measurement of plasma glucose, particularly that measured in the fasting state [18]. As a diagnostic test, HbA1c has the advantages over plasma glucose in terms of higher reliability in repetitive examinations and feasibility of measurement in non-fasting conditions [19]. In a large longitudinal study observing a cohort without prior diagnosis of DM, Selvin et al. [20] demonstrated superiority of HbA1c over FPG in risk assessment of cardiovascular outcomes as well as in prediction of mortality.
We undertook this study to explore the respective associations of and mutual interrelations between HbA1c and FPG with colorectal neoplasia. We hypothesized that HbA1c as compared with FPG was a stronger and more independent risk factor associated with colorectal neoplasia.
Materials and methods
Setting and participants
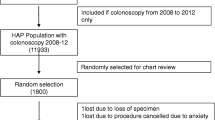
This study analyzed cross-sectional sample of consecutive participants in a voluntary health check-up program (Imperial Clinic, Taipei, Taiwan) during a 2-year period. All subjects submitted written informed consent upon entry, and the study protocol was approved by the institutional review board of Taipei Medical University. This program comprised review of personal history, physical examination, laboratory examination, radiography, and upper as well as lower gastrointestinal endoscopy. All study participants joined in the program for the purpose of comprehensive health examination, instead of seeking care for a specific illness or discomfort. Those whose colonoscopy failed cecal intubation were excluded from analysis (Fig. 1).
Assessment of personal information and anthropometric measurement
All examinees completed structured questionnaires to obtain relevant personal information. The diagnosis of DM and hypertension was based on self-reported history or use of relevant medications. Participants who had any first-degree relative with colorectal cancer were defined as positive for family history [21]. Cigarette smokers were defined as those who had been smoking for at least 1 year with a minimum of one pack per day. Excessive alcohol drinkers were those whose daily consumption converted to more than 40 mL of pure ethanol. Physical activity was categorized into 3 levels according to the frequency of exercise of at least moderate intensity for more than 30 min: less than once per week, once to twice per week, and more than twice per week.
Body weight and height were measured with uniform light clothes on and shoes off. Body mass index (BMI) was calculated as the individual’s body weight in kilograms divided by the square of his or her height in meters. Waist circumference was determined with a tap measuring around the midline between top of the hip bones and bottom of the thoracic cage [22]. Blood pressure was measured by sphygmomanometer with hypertension defined as systolic pressure more than 140 mmHg or diastolic pressure more than 90 mmHg.
Laboratory tests and colonoscopy procedures
All blood samples were collected in the morning after an overnight fast. Percentage of HbA1c was assayed with high-performance liquid chromatography method (AU2700 analyzer, Olympus, Tokyo, Japan). Concentration of plasma glucose was measured using hexokinase method with ultraviolet detection at 340 nm (AU2700 analyzer, Olympus, Tokyo, Japan). Other blood examinations inclusive of total cholesterol, high-density lipoprotein (HDL), low-density lipoprotein (LDL), triglyceride, and C-reactive protein (CRP) were performed according to standardized protocols. This laboratory randomly duplicated sample assays and analyzed intra-assay variation as a routine procedure of quality control.
All colonoscopy procedures were carried out by a single endoscopist (HSL) who had previously performed more than 10,000 colonoscopies. Resected colorectal lesions were interpreted by experienced pathologists in accordance with classification system of World Health Organization. Advanced adenoma was defined as those with diameter larger than 10 mm, with villous component, with high-grade dysplasia, or had invasive features [23]. Subjects with high-risk neoplasia were defined as those with multiple (n ≧ 3) or at least one advanced adenoma [24]. Both the endoscopist and pathologist were blinded to results of all blood examinations.
Statistical analysis
Study participant with any colorectal neoplasia and those with high-risk neoplastic lesions were considered as primary and secondary outcome of this study, respectively. Continuous variables were expressed with mean ± standard error of mean (SEM), and categorical variables were expressed with percentage of occurrence, unless otherwise specified. For univariate comparison, independent t test was used to compare sets of continuous variables, and Fisher’s exact test for proportions.
We conducted multivariate logistic regression analysis with stepwise method to evaluate independent risk factors associated with colorectal neoplasia. Three regression models were developed in a hierarchical way to elucidate the interrelationship among different hyperglycemic indices. In all three models, biologically plausible factors that included age, gender, BMI, waist circumference, diagnosis of DM, hypertension, smoking, alcohol drinking, level of physical exercise, family history of colorectal cancer, serum concentration of cholesterol, LDL, HDL, triglyceride, CRP, and blood leukocyte count were tested as possible explanatory variables [5, 14, 25, 26]. FPG was added in the model 2, and both FPG and HbA1c were added in the model 3. Variance inflation factors (VIF) of each independent variable in all developed models were calculated. A VIF >5 is considered significant for multicollinearity. All statistical analyses were two-tailed and performed by commercial software (Stata, 9.1; College Station, Texas, USA). The results were considered statistically significant if p values were less than 0.05.
Results
Characteristics of the enrolled participants
Among 2,854 participants in the health management program between January 2007 and January 2009, a total of 2,776 (98.20%) participants (aged 18–86 years) were included into analysis (Fig. 1). One hundred and thirty-two subjects (4.8%) reported past history of DM or used diabetic medications (Table 1). The average percentage of blood glycated hemoglobin was 5.73% with SEM of 0.015. Colorectal neoplasia was found in 605 (21.79%) examinees, 68 of whom had high-risk lesions (2.45%). There were two cases of colorectal cancer found in this program.
Risk factors for colorectal neoplasia by univariate and multivariate analyses
In the univariate analysis, colorectal neoplasia was associated with advanced age, male gender, higher BMI, larger waist circumference, life style with cigarette smoking or alcohol drinking, frequency of physical exercise, diagnosis of DM or hypertension, dyslipidemia with higher total cholesterol, LDL or triglyceride, and lower HDL, elevated blood leukocyte count and CRP level, and hyperglycemia as represented either by FPG or HbA1c. After adjusting for all factors listed in the Table 1, the multivariate model revealed advanced age (adjusted OR, 1.04 per year; 95% CI, 1.03–1.05), male gender (adjusted OR, 1.76; 95% CI, 1.44–2.17), cigarette smoking (adjusted OR, 2.16; 95% CI, 1.74–2.69), and HbA1c (adjusted OR, 1.22; 95%, 1.10–1.36) were independent risk factors for colorectal neoplasm (Table 2).
In the univariate analysis for high-risk colorectal neoplasia, the association of FPG was marginally significant (crude OR, 1.01; 95% CI, 1.0–1.02; p = 0.026) and that of HbA1c was statistically insignificant (crude OR, 1.18; 95% CI, 0.95–1.46; p = 0.138). Independent risk factors were age (adjusted OR, 1.03 per year; 95% CI, 1.01–1.05), smoking (adjusted OR, 2.97; 95% CI, 1.78–4.93), and lower serum HDL (adjusted OR, 0.98 per mg/dL increment; 95% CI, 0.96–1.00) in the multivariate logistic regression analysis. None of the glycemic indices was independently associated with high-risk tumors.
Interrelationship among different glycemic indices in the association with colorectal neoplasm
When inputting pre-existing diagnosis of DM as the sole explanatory variable representative of hyperglycemic index (model 1), we found age, male gender, smoking habit, waist circumference, and DM diagnosis were independent risk factors for colorectal neoplasia (Table 3). In the model 2 in which FPG was added to all variables in model 1 (including DM diagnosis), FPG replaced the diagnosis of DM as the glycemic index associated with colorectal neoplasia and attenuated the effect of waist circumference. Age, male gender, and cigarette smoking remained independently associated with colorectal tumor in the model 2. If all three hyperglycemic indices (DM diagnosis, FPG and HbA1c) were examined as competing covariates (model 3), HbA1c outperformed the other two markers in the independent association of colorectal neoplasia. The link with age, gender, and smoking habit was not changed. When FPG was constrainedly retained as an explanatory covariate, the independent association between HbA1c and colorectal neoplasia remained significant (adjusted OR, 1.25; 95% CI, 1.03–1.51; p = 0.02) despite forced adjustment for FPG (model 4).
In the multivariate regression analysis restricted to 2,644 participants without known diagnosis of DM (Table 4), FPG was not an independent risk factor for colorectal neoplasia among participants without known diagnosis of DM, even if HbA1c was included as a competing variable (model A). In contrast, HbA1c remained independently associated with colorectal tumor in this sensitivity analysis (model B).
Discussion
Although the association between hyperglycemic state and colorectal adenoma-carcinoma development has been reported in the literature, which glycemic index is the strongest and most independent risk factor has not been elucidated. This study demonstrates for the first time that HbA1c outperforms both the diagnosis of DM and level of FPG as a risk indicator for colorectal neoplasia. The association between colorectal tumor and HbA1c remains significant not only after forced adjustment for FPG but also in the sensitivity analysis restricted to participants without history of diabetes. Findings of the present study add to the growing body of evidence supporting that HbA1c is superior to FPG in assessing risk of complications related to chronic hyperglycemia. Moreover, these results warrant further research to explore the value of HbA1c in risk stratification in the screening program for colorectal cancer.
Chronic hyperglycemia is causally associated with a variety of long-term complications including microvascular, macrovascular, and neoplastic diseases. Glycemic levels for the definition of DM are based on the relationship between certain glycemic values and risk of microvascular complications, particularly retinopathy [27]. Therefore, a reliable biomarker standing for hyperglycemia over a longer period of time conceivably makes a better indicator in assessing risk of complications. The value of HbA1c in evaluating outcomes of and in guiding therapy for diabetic patients has long been well established [18], but not until recently has the prognostic performance of HbA1c in non-diabetic population been reported [20, 28]. Along these lines of evidence, our data also support the use of HbA1c in evaluating relevant complications associated with hyperglycemia in the general population.
Our results may have important implications for the population-based colon cancer screening programs, particularly in the health care systems with relatively limited resources. It has been demonstrated that removal of adenomatous polyps effectively prevents development of colorectal cancers [4], and screening colonoscopy may reduce the incidence and mortality of colorectal cancer [29–31]. Nonetheless, screening colonoscopy in the population level incurs huge expense and workload that cannot be practical in most countries. For any screening program to be cost-effective, a thorough understanding of risk stratification is mandatory. In consistence with our findings, Kim and colleagues reported that the risk of finding colorectal adenoma in asymptomatic Korean men in forties with HbA1c >5.4% was similar to that in those in their fifties with average risk of colorectal cancer [16]. More clinical research and cost-effectiveness analyses are now warranted to further investigate whether and how HbA1c, along with other known risk factors, may improve the screening program.
Previous studies that investigate relationship between HbA1c and colorectal neogrowth have reported inconsistent results [7–12, 16]. Discrepancy among these studies may result from different study design, sample size, composition of study population, and definition of outcomes. It was noteworthy that all of the researches with null results enrolled only women, as two of them analyzed data from Nurses’ Health Study, [11, 12] and the other one from Women’s Health Study [10]. Selection bias related to choosing controls is a serious concern in previous research with retrospective case–control design [8, 9, 11, 12]. This shortcoming is of particular importance in the studies whose primary outcome was colorectal adenoma but did not endoscope all individuals [11, 12]. Furthermore, none of the prior studies has compared HbA1c against FPG and diagnosis of DM in evaluating the independent association with colorectal tumors.
Strengths of this study include comprehensive evaluation of participants’ health status with a standardized protocol. For example, BMI and waist circumference were exactly measured, not self-reported. This advantage not only enables consistent definitions but also generates credible information both for the covariates in question and for the outcomes of interest. The fact that all subjects of this cross-sectional sample receive complete colonoscopy minimizes misclassification in defining cases and controls. An exceedingly high proportion (98.5%) of the initially screened examinees enrolled into final analysis further mitigates concerns of selection bias. Furthermore, inter-observer variability of detecting colorectal neoplasia can be eliminated in that all colonoscopic procedures are carried out by a single endoscopist. With complete data from a relatively large sample size of cases (n = 605) and controls (n = 2,171), this study is statistically empowered to distinguish smaller differences between those with and without colorectal neoplasia.
Several limitations merit discussion. Participants in this clinic-based screening program are not randomly picked up from the general population but have to volunteer to join in the program. However, the prevalence of colorectal adenoma and advanced tumors observed in this study are similar to those reported in recent studies investigating average-risk adults from Asia and Taiwan [32, 33]. Besides, these participants do not attend this health management program because of any illness and accordingly they should not be regarded as a hospital-based population. Second, since advanced colorectal neoplasm occurs rarely, the number of patients with high-risk neoplasia (n = 68) is relatively small, limiting statistical power. This limitation probably explains why none of the glycemic index can be shown independently associated with high-risk colorectal neoplasia (type II error). Furthermore, some cases whose colorectal adenomas were resected in previous colonoscopy would have been misclassified as controls. However, this misclassification would have only underestimated the true effect in the association between colorectal neoplasia and HbA1c, which actually remains significant despite this possible limitation. Finally, causality cannot be ascertained in this cross-sectional study. Whether hyperglycemia is, in effect, a proxy of more fundamental metabolic derangement that more directly leads to neogrowth of colorectal epithelium is certainly interesting [34] and deserves further exploration.
In conclusion, we demonstrate that HbA1c is superior to FPG in assessing the association between hyperglycemia and colorectal neoplasia. Findings of this study support that HbA1c is a better risk indicator for evaluating complications related to hyperglycemia, even in individuals without the diagnosis of DM. Our study implicates that HbA1c may be useful for screening adults at risk of colorectal neoplasia and calls for further research to elucidate its role in population-based colon cancer screening programs.
References
Jemal A, Siegel R, Ward E et al (2006) Cancer statistics, 2006. CA Cancer J Clin 56:106–130
Sung JJ, Lau JY, Goh KL, Leung WK (2005) Increasing incidence of colorectal cancer in Asia: implications for screening. Lancet Oncol 6:871–876
Vogelstein B, Fearon ER, Hamilton SR et al (1988) Genetic alterations during colorectal-tumor development. N Engl J Med 319:525–532
Winawer SJ, Zauber AG, Ho MN et al (1993) Prevention of colorectal cancer by colonoscopic polypectomy. The National Polyp Study Workgroup. N Engl J Med 329:1977–1981
Larsson SC, Orsini N, Wolk A (2005) Diabetes mellitus and risk of colorectal cancer: a meta-analysis. J Natl Cancer Inst 97:1679–1687
Jee SH, Ohrr H, Sull JW, Yun JE, Ji M, Samet JM (2005) Fasting serum glucose level and cancer risk in Korean men and women. JAMA 293:194–202
Khaw KT, Wareham N, Bingham S, Luben R, Welch A, Day N (2004) Preliminary communication: glycated hemoglobin, diabetes, and incident colorectal cancer in men and women: a prospective analysis from the European prospective investigation into cancer-Norfolk study. Cancer Epidemiol Biomarkers Prev 13:915–919
Saydah SH, Platz EA, Rifai N, Pollak MN, Brancati FL, Helzlsouer KJ (2003) Association of markers of insulin and glucose control with subsequent colorectal cancer risk. Cancer Epidemiol Biomarkers Prev 12:412–418
Rinaldi S, Rohrmann S, Jenab M et al (2008) Glycosylated hemoglobin and risk of colorectal cancer in men and women, the European prospective investigation into cancer and nutrition. Cancer Epidemiol Biomarkers Prev 17:3108–3115
Lin J, Ridker PM, Pradhan A et al (2005) Hemoglobin A1c concentrations and risk of colorectal cancer in women. Cancer Epidemiol Biomarkers Prev 14:3010–3012
Platz EA, Hankinson SE, Rifai N, Colditz GA, Speizer FE, Giovannucci E (1999) Glycosylated hemoglobin and risk of colorectal cancer and adenoma (United States). Cancer Causes Control 10:379–386
Wei EK, Ma J, Pollak MN et al (2006) C-peptide, insulin-like growth factor binding protein-1, glycosylated hemoglobin, and the risk of distal colorectal adenoma in women. Cancer Epidemiol Biomarkers Prev 15:750–755
Schoen RE, Tangen CM, Kuller LH et al (1999) Increased blood glucose and insulin, body size, and incident colorectal cancer. J Natl Cancer Inst 91:1147–1154
Nilsen TI, Vatten LJ (2001) Prospective study of colorectal cancer risk and physical activity, diabetes, blood glucose and BMI: exploring the hyperinsulinaemia hypothesis. Br J Cancer 84:417–422
Chung YW, Han DS, Park YK et al (2006) Association of obesity, serum glucose and lipids with the risk of advanced colorectal adenoma and cancer: a case–control study in Korea. Dig Liver Dis 38:668–672
Kim BJ, Kim YH, Sinn DH et al (2010) Clinical usefulness of glycosylated hemoglobin as a predictor of adenomatous polyps in the colorectum of middle-aged males. Cancer Causes Control 21:939–944
Bunn HF, Gabbay KH, Gallop PM (1978) The glycosylation of hemoglobin: relevance to diabetes mellitus. Science 200:21–27
Association AD (2010) Standards of medical care in diabetes—2010. Diabetes Care 33:S11–S61
Selvin E, Crainiceanu CM, Brancati FL, Coresh J (2007) Short-term variability in measures of glycemia and implications for the classification of diabetes. Arch Intern Med 167:1545–1551
Selvin E, Steffes MW, Zhu H et al (2010) Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults. N Engl J Med 362:800–811
Taylor DP, Burt RW, Williams MS, Haug PJ, Cannon-Albright LA (2010) Population-based family history-specific risks for colorectal cancer: a constellation approach. Gastroenterology 138:877–885
Lean ME, Han TS, Morrison CE (1995) Waist circumference as a measure for indicating need for weight management. BMJ 311:158–161
Winawer SJ, Zauber AG (2002) The advanced adenoma as the primary target of screening. Gastrointest Endosc Clin N Am 12:1–9, v
Lieberman DA, Weiss DG, Harford WV et al (2007) Five-year colon surveillance after screening colonoscopy. Gastroenterology 133:1077–1085
Chiu HM, Lin JT, Shun CT et al (2007) Association of metabolic syndrome with proximal and synchronous colorectal neoplasm. Clin Gastroenterol Hepatol 5:221–229; quiz 141
Chiu HM, Lin JT, Chen TH et al (2008) Elevation of C-reactive protein level is associated with synchronous and advanced colorectal neoplasm in men. Am J Gastroenterol 103:2317–2325
(1997) Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care 20:1183–1197
Sabanayagam C, Liew G, Tai ES et al (2009) Relationship between glycated haemoglobin and microvascular complications: is there a natural cut-off point for the diagnosis of diabetes? Diabetologia 52:1279–1289
Lieberman DA, Weiss DG, Bond JH, Ahnen DJ, Garewal H, Chejfec G (2000) Use of colonoscopy to screen asymptomatic adults for colorectal cancer. Veterans Affairs Cooperative Study Group 380. N Engl J Med 343:162–168
Baxter NN, Goldwasser MA, Paszat LF, Saskin R, Urbach DR, Rabeneck L (2009) Association of colonoscopy and death from colorectal cancer. Ann Intern Med 150:1–8
Rabeneck L, Paszat LF, Saskin R, Stukel TA (2010) Association between colonoscopy rates and colorectal cancer mortality. Am J Gastroenterol 105:1627–1632
Byeon JS, Yang SK, Kim TI et al (2007) Colorectal neoplasm in asymptomatic Asians: a prospective multinational multicenter colonoscopy survey. Gastrointest Endosc 65:1015–1022
Soon MS, Soon A, Lin TY, Lin OS (2008) Distribution of colon neoplasia in Chinese patients: implications for endoscopic screening strategies. Eur J Gastroenterol Hepatol 20:642–647
Liou JM, Shun CT, Liang JT et al (2010) Plasma insulin-like growth factor-binding protein-2 levels as diagnostic and prognostic biomarker of colorectal cancer. J Clin Endocrinol Metab 95:1717–1725
Acknowledgments
We wish to express our gratitude to all staff of the Imperial Clinic, for their collaboration in this study. Research grant from E-Da Hospital, Kaohsiung.
Conflict of interest
All authors declared no conflict of interests.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Hsu, YC., Chiu, HM., Liou, JM. et al. Glycated hemoglobin A1c is superior to fasting plasma glucose as an independent risk factor for colorectal neoplasia. Cancer Causes Control 23, 321–328 (2012). https://doi.org/10.1007/s10552-011-9880-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-011-9880-y