Abstract
Pancreatic cancer is difficult to manage owing to the challenges involved in its treatment and nursing. This study aimed to clarify the roles and mechanisms of action of Poly (A)-binding protein cytoplasmic 1 (PABPC1) on pancreatic cancer. The expression of PABPC1 in pancreatic cancer tissues and cell lines was detected using RT-qPCR and western blotting. The effects of PABPC1 on proliferation, apoptosis, epithelial-mesenchymal transition (EMT), and the PI3K/AKT signaling pathway in pancreatic cancer cells were further investigated using MTT assays, flow cytometry, and western blotting. The expression of PABPC1 was significantly upregulated in pancreatic cancer tissues and cells, whereas PABPC1 downregulation inhibited pancreatic cancer cell proliferation, induced apoptosis, decreased the expression of EMT-associated proteins, and exerted a regulatory effect by inhibiting the PI3K/AKT signaling pathway. In addition, the findings indicated that PABPC1 over-expression significantly promoted pancreatic cancer cell proliferation, inhibited apoptosis, decreased the expression of E-cadherin, enhanced N-cadherin expression, and activating the PI3K/AKT signaling pathway. PABPC1 silencing significantly inhibited proliferation and EMT and induced apoptosis in pancreatic cancer cells. These findings provide novel insights into the role of PABPC1 in the development of pancreatic cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pancreatic cancer is a common malignant tumor of the gastrointestinal tract originating from the glandular ductal epithelial cells in the pancreas, with a highly invasive and metastatic tendency (Andersson et al. 2022; Klein 2021). As early symptoms are not obvious, they are often not detected until the late stage, which not only increases the difficulty of treatment but also leads to a lower survival rate (Stoffel et al. 2023). Currently, the treatment for pancreatic cancer primarily includes surgical resection, chemotherapy, radiotherapy and targeted therapy (Gugenheim et al. 2022; Martino and Boghdady 2023; Mukherji et al. 2022). Nursing care also plays a crucial role in pancreatic cancer (Lei et al. 2020). Acute pain, malnutrition, high body temperature, and complications, such as infection, shock, and bleeding, are currently the main concerns in nursing (Spross et al. 1988).Through scientific drug management, reasonable diet adjustment, and adequate rest, these symptoms can be alleviated, and the quality of life and treatment effects of patients can be improved (Ma et al. 2022; Liu et al. 2022). However, pancreatic cancer usually responds poorly to chemotherapy, radiotherapy, and targeted therapy, and the treatment process is complex and challenging (Luo et al. 2020). This has prompted the exploration of effective therapeutic strategies against pancreatic cancer. To explore the therapeutic pathways in pancreatic cancer, it is necessary to study its pathogenesis in detail.
Poly (A)-binding protein cytoplasmic 1 (PABPC1) is a member of the poly (A) binding protein (PABP) family, which usually binds to the polyadenylate (poly (A) tail) of mRNA, plays an important role in the cytoplasm, and participates in various biological processes, such as the stability, translation, and degradation of mRNA (Ozturk and Uysal 2017, 2018). Recent studies have suggested that PABPC1 plays an important role in cancer initiation and development. The expression level of PABPC1 is significantly elevated in tumor tissues, including gastric, ovarian, and liver cancers (Feng et al. 2021; Tailai An et al. 2021; Meng et al. 2023; Li et al. 2023; Jie Zhu et al. 2015). Several studies have shown that PABPC1 is involved in the proliferation, apoptosis, migration, and invasion of tumor cells. For example, Wu et al. found that PABPC1 deletion inhibits the proliferation and migration of human colorectal cancer cells by blocking the AKT pathway (Wu et al. 2019). These studies suggest that PABPC1 is a potential target for cancer therapy.
Recent studies have shown that the expression level of PABPC1 is significantly higher in pancreatic cancer tissues than that in normal pancreatic tissues, making it a potential independent prognostic risk factor (Wen et al. 2020; Guven 2022). Some studies have shown that PABPC1 promotes adenocarcinoma pancreatic cell proliferation and metastasis by regulating COL12A1 (Yao et al. 2023). These results suggest that PABPC1 is involved in the development of pancreatic cancer. However, several questions remain unanswered regarding the specific roles and molecular mechanisms of action of PABPC1 in pancreatic cancer.
This study aimed to clarify the expression of PABPC1 in the cancerous tissues of patients with pancreatic cancer and to analyze its correlation with clinicopathological parameters. Through an in-depth analysis of the regulatory role in the biological behavior of pancreatic cancer cells, we hope to provide novel insights into the molecular mechanisms underlying pancreatic cancer development and a strong scientific basis for future therapeutic and prognostic evaluation.
Materials and methods
Clinical sample collection
In this study, 30 pancreatic cancer tissues and adjacent normal tissues were collected by surgery, and the samples were stored at − 80 °C. All patients signed an informed consent form, with approval from the ethics committee.
Cell culture
The normal human pancreatic ductal epithelial cell line HPDE 6-C7 and pancreatic cancer cell lines PANC-1, CFPAC-1, and SW1990 were purchased from the American Type Culture Collection. DMEM (Basal Media) containing 10% fetal bovine serum (FBS; Biological Industries) was used as the medium. Cells were placed in a 5% CO2, 37 °C incubator. Cell passaging and subsequent experiments were performed when the cells reached 80% confluence.
Cell transfection
CFPAC-1 cells were transfected with control-siRNA (sc-37007, Santa Cruz Biotechnology), PABPC1-siRNA (sc-108012, Santa Cruz Biotechnology), control-plasmid (sc-437275, Santa Cruz Biotechnology), or PABPC1-plasmid (sc-400688-ACT, Santa Cruz Biotechnology) using Lipofectamine 2000 (Invitrogen, Carlsbad, CA, USA) according to the manufacturer’s instructions. After 48 h of incubation, the cells were collected, and the transfection efficiency was analyzed using RT-qPCR.
Western blot assay
Pancreatic cancer tissues or cells were lysed with radioimmunoprecipitation assay buffer (AS1004, ASPEN) containing an inhibitor cocktail (Roche). Total protein was extracted, and protein concentration was measured with a BCA kit (AS1086, ASPEN). Equal amounts of protein were separated via 12% sodium dodecyl sulfate-polyacrylamide gel electrophoresis and transferred to PVDF membranes (Millipore). Membranes were blocked with a blocking solution containing 5% milk. After 1 h, membranes were incubated with the primary antibody at 4 °C overnight, including PABPC1, PCNA, cleaved-caspase3, caspase3, E-cadherin, N-cadherin, p-PI3K, PI3K, p-AKT, and AKT. The next day, membranes were washed with TBST. The membrane was then incubated with an HRP-labeled secondary antibody for 2 h and visualized using ECL luminescent solution (AS1059, ASPEN).
RNA extraction and real-time quantitative PCR (RT-qPCR)
Total RNA was isolated from cells using TRIzol Total RNA Extraction Reagent (EP013; ELK Biotechnology) according to the manufacturer’s instructions. The extracted total RNA was reverse-transcribed as cDNA using EntiLink™ 1st Strand cDNA Synthesis Super Mix (EQ031, ELK Biotechnology). Subsequently, a real-time quantitative PCR with EnTurbo™ SYBR Green PCR SuperMix (EQ001, ELK Biotechnology) used 2− ΔΔCt to calculate the relative mRNA expression of genes, and GAPDH was used as an internal control. The primer sequences are listed in Table 1.
Cell viability detected using MTT assays
Cell viability was assessed using the MTT assay, as described previously (Kumar et al. 2018). Briefly, transfected cells were seeded into 96-well plates and incubated at 37 °C for 24 h. Subsequently, 10 µL of MTT solution was added to each well and incubated for 4 h at 37 °C. Then, 100 µL formazan solution was added to each well and mixed well and further incubated in an incubator until formazan was completely dissolved. Absorbance was measured at 570 nm using a spectrophotometer to assess cell viability.
Detection of apoptosis using flow cytometry (FCM)
FCM was used to detect apoptosis in this study. Apoptosis was assessed using an Annexin V-FITC Apoptosis Detection Kit (Beyotime) according to the manufacturer’s instructions. Briefly, approximately 1 × 105 cells were incubated with 5 µL of Annexin V-FITC for 15 min at room temperature, followed by incubation with 10 µL of propidium iodide (PI) staining solution for 10–20 min at room temperature protected from light. Subsequently, the samples were analyzed using a flow cytometer (BD Biosciences).
Statistical analysis
All data were analyzed using SPSS software and expressed as mean ± SD. Differences between groups were statistically analyzed using one-way analysis of variance, followed by Tukey’s test. p < 0.05 was considered statistically significant difference.
Results
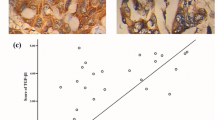
Expression of PABPC1 in tissues from patients with pancreatic cancer
In this study, we collected 30 samples of pancreatic cancer tissues and corresponding paracancerous normal tissues and examined the expression levels of PABPC1 in these tissues using RT-qPCR and western blot assays. The results showed that the expression of PABPC1 was significantly upregulated in pancreatic cancer tissues compared to that in normal paracancerous tissues (Fig. 1A–C).
Expression of PABPC1 in pancreatic cancer cells
We explored the expression of PABPC1 in different pancreatic cancer cell lines. Western blotting and RT-qPCR revealed that the expression of PABPC1 was significantly elevated in PANC-1, CFPAC-1, and SW1990 pancreatic cancer cell lines compared to that in the normal human pancreatic ductal epithelial cell line HPDE6-C7 (Fig. 2A–C).
Effect of PABPC1 on the proliferation of pancreatic cancer cells
To further investigate the effect of PABPC1 on cancer cells, we performed transfection experiments using the CFPAC-1 pancreatic cancer cell line. To regulate the expression of PABPC1, we divided CFPAC-1 cells into three groups: control, control siRNA, and PABPC1-siRNA. Transfection efficiency of PABPC1-siRNA was verified using western blotting and RT-qPCR. The results showed that PABPC1-siRNA significantly reduced the expression level of PABPC1 in CFPAC-1 cells compared to that in the control siRNA group (Fig. 3A–C). Subsequently, cell proliferation was investigated using the MTT assay. Monitoring was performed at the time points of 0, 24, 48, and 72 h of transfection. The results showed that the proliferation in the PABPC1-siRNA-treated group was significantly inhibited, with a significant difference compared to the control-siRNA group (Fig. 3D). The expression levels of cell proliferation-related proteins and genes, including PCNA, were assessed using western blotting and RT-qPCR. The results showed that PABPC1-siRNA treatment resulted in a significant downregulation of the protein and mRNA levels of PCNA compared to the control siRNA group (Fig. 3E–G). Meanwhile, our results indicate that PABPC1 siRNA has no significant effect on the proliferation and apoptosis of normal human pancreatic epithelial cell line HPDE 6-C7 (Supplementary Fig. 1). These results indicate that PABPC1 knockdown significantly inhibited the proliferation of CFPAC-1 cells and reduced the protein and mRNA expression levels of PCNA in pancreatic cancer cells, further demonstrating the critical role of PABPC1 in the regulation of pancreatic cancer cell proliferation.
Effects of PABPC1-siRNA on proliferation of CFPAC-1 cells. CFPAC-1cells were transfected with control-plasmid or PABPC1-plasmid at the presence of PABPC1-siRNA for 48 h. A–C The mRNA and protein levels of PABPC1 in CFPAC-1 cells were determined using RT-qPCR and western blotting; D. Detection of cellular viability with MTT assays; E–G The mRNA and protein levels of PCNA were determined using RT-qPCR and western blotting. **p < 0.01
Effect of PABPC1 on apoptosis in pancreatic cancer cells
The effect of PABPC1 on the apoptosis of pancreatic cancer cells was investigated by transfecting CFPAC-1 cells. The control-siRNA and PABPC1-siRNA were transfected into CFPAC-1 cells, respectively. After transfection for 48 h, apoptosis was determined using FCM. In addition, we used western blotting to detect the protein levels of cleaved-caspase3 and caspase3 and determined the cleaved-caspase3/caspase3 ratio. The results showed that PABPC1-siRNA significantly induced apoptosis in CFPAC-1 cells compared to the control siRNA group (Fig. 4A and B) and increased the expression of cleaved-caspase3 as well as the cleaved-caspase3/caspase3 ratio (Fig. 4C and D). These results indicate that the downregulation of PABPC1 influences the apoptotic process of CFPAC-1 pancreatic cancer cells by regulating the expression of cleaved-caspase3 and caspase3. This study reveals the potential role of PABPC1 in the regulation of apoptosis in pancreatic cancer cells.
Effects of PABPC1-siRNA on apoptosis of CFPAC-1 cells. CFPAC-1cells were transfected with control-plasmid or PABPC1-plasmid at the presence of PABPC1-siRNA for 48 h. A, B Cell apoptosis was detected using flow cytometry; C The protein levels of cleaved-caspase3 and caspase3 were determined using western blotting; D The ratio of cleavage-caspase3/caspase3. **p < 0.01
Effect of PABPC1 on epithelial-mesenchymal transition (EMT) in pancreatic cancer cells
In pancreatic cancer cells, the EMT is closely associated with cell proliferation and apoptosis (Shao et al. 2020). To investigate the effect of PABPC1 on EMT in pancreatic cancer cells, we regulated the expression PABPC1 in transfection experiments using CFPAC-1 cells. The expression of apoptosis-related genes ( E-cadherin and N-cadherin) in pancreatic cancer cell lines was assessed using western blotting and RT-qPCR. As shown in Fig. 5, the PABPC1-siRNA group showed significantly increased expression of E-cadherin in CFPAC-1 cells and decreased expression of N-cadherin, suggesting that downregulation of PABPC1 has the potential to promote the transition of pancreatic cancer cells to a less aggressive phenotype.
Effects of PABPC1-siRNA on EMT in CFPAC-1 cells. CFPAC-1cells were transfected with control-plasmid or PABPC1-plasmid at the presence of PABPC1-siRNA for 48 h. The protein and mRNA levels of E-cadherin and N-cadherin in CFPAC-1 cells were determined using western blotting (A and B) and RT-qPCR (C). **p < 0.01
Effect of PABPC1 knockdown on PI3K/AKT signaling pathway in pancreatic cancer cells
To further investigate the mechanism of PABPC1 in pancreatic cancer cells, we explored the effect of PABPC1 on the PI3K/AKT signaling pathway in pancreatic cancer cells. The PI3K/AKT pathway is an important cellular signaling pathway that plays a key role in the regulation of cell survival, proliferation, apoptosis, and metabolism (Hu et al. 2021; Yu et al. 2022; Chen et al. 2016; Mortazavi et al. 2022). We transfected control-siRNA and PABPC1-siRNA into CFPAC-1 cells. After 48 h of transfection, the expression levels of proteins associated with the PI3K/AKT signaling pathway, including p-PI3K, PI3K, p-AKT, and AKT, were detected using western blotting, and the ratios of p-PI3K/PI3K and p-AKT/AKT were calculated. The results showed that PABPC1-siRNA treatment significantly reduced the expression levels of p-PI3K and p-AKT proteins, as well as the ratios of p-PI3K/PI3K and p-AKT/AKT in CFPAC-1 cells, compared to the control siRNA group (Fig. 6). These findings imply that PABPC1 silencing may exert an inhibitory effect on the growth and proliferation of pancreatic cancer cells by suppressing the activation of the PI3K/AKT signaling pathway. Our study provides important clues for a deeper understanding of the mechanisms of action of PABPC1 in pancreatic cancer development and provides strong support for the further exploration of therapeutic strategies targeting the PI3K/AKT signaling pathway.
Effects of PABPC1-siRNA on PI3K/AKT Signaling in CFPAC-1 cells. CFPAC-1cells were transfected with control-plasmid or PABPC1-plasmid at the presence of PABPC1-siRNA for 48 h. A The protein levels of p-PI3K, PI3K, p-AKT, and AKT in CFPAC-1 cells were determined using western blotting. B The ratio of p-PI3K/PI3K and p-AKT/AKT. **p < 0.01
PABPC1 over-expression significantly reversed the effects of PABPC1-siRNA on pancreatic cancer cells
We finally investigated the effects of PABPC1 over-expression on pancreatic cancer cells. Control-plasmid and PABPC1-plasmid were transfected into CFPAC-1 cells for 48 h, and the expression levels of PABPC1 were determined using RT-qPCR and western blotting. As shown in Fig. 7A–C, compared with the control-plasmid, PABPC1-plasmid significantly enhanced PABPC1 expression in CFPAC-1 cells. Besides, compared with the PABPC1-siRNA + control-plasmid group, PABPC1-plasmid significantly enhanced PABPC1 expression in CFPAC-1 cells (Fig. 7D–F), indicating PABPC1-siRNA induced PABPC1 reduction in CFPAC-1 cells was eliminated by PABPC1-plasmid.
Effects of PABPC1-plasmid on PABPC1 expression in CFPAC-1 cells. A–C CFPAC-1 cells were transfected with control-plasmid or PABPC1-plasmid for 48 h, and the mRNA and protein levels of PABPC1 in CFPAC-1 cells were determined by RT-qPCR and western blot analysis. D–F CFPAC-1 cells were transfected with control-plasmid or PABPC1-plasmid at the presence of PABPC1-siRNA for 48 h, and the mRNA and protein levels of PABPC1 in CFPAC-1 cells were determined by RT-qPCR and western blot analysis. **p < 0.01
Functional experiments indicated that PABPC1-siRNA induced cell proliferation reduction (Fig. 8A), PCNA expression decrease (Fig. 8B–D), cell apoptosis increase (Fig. 8E and F), and cleaved-Caspase3 expression enhancement (Fig. 8G and H) in CFPAC-1 cells were significantly reversed by PABPC1-plasmid. Moreover, PABPC1-siRNA induced E-cadherin expression increase, N-cadherin expression decrease (Fig. 9A–C), and PI3K/AKT signaling pathway inhibition (Fig. 10A and B) were eliminated by PABPC1-plasmid.
Effects of PABPC1-plasmid on the proliferation and apoptosis of CFPAC-1 cells. CFPAC-1 cells were transfected with control-plasmid or PABPC1-plasmid at the presence of PABPC1-siRNA for 48 h. A CFPAC-1 cell proliferation was determined by MTT assay. B–D The mRNA and protein levels of PCNA in CFPAC-1 cells were determined by RT-qPCR and western blot analysis. E and F Cell apoptosis was analyzed by FCM. G and H Cleaved-Caspase3 protein expression was determined by western blot assay, and cleaved-Caspase3/GAPDH ratio was calculated and presented. **p < 0.01
Effects of PABPC1-plasmid on the EMT of CFPAC-1 cells. CFPAC-1 cells were transfected with control-plasmid or PABPC1-plasmid at the presence of PABPC1-siRNA for 48 h. A and B The protein levels of E-cadherin and N-cadherin in CFPAC-1 cells were determined by western blot analysis. C The mRNA levels of E-cadherin and N-cadherin in CFPAC-1 cells were determined by RT-qPCR. **p < 0.01
Effects of PABPC1-plasmid on the PI3K/AKT pathway in CFPAC-1 cells. CFPAC-1 cells were transfected with control-plasmid or PABPC1-plasmid at the presence of PABPC1-siRNA for 48 h. A The protein levels of p-PI3K, PI3K, p-AKT, and AKT in CFPAC-1 cells were determined by western blot analysis. B p-PI3K/PI3K and p-AKT/AKT ratio were presented. **p < 0.01
Discussion
Pancreatic cancer is a highly lethal malignancy (Vincent et al. 2011). The pathogenesis of this condition has not been fully elucidated and current therapies are severely limited (Stoffel et al. 2023; Wood et al. 2022). One of the key challenges in the treatment of pancreatic cancer is resistance to traditional treatment modalities, including chemotherapy and radiotherapy (Gugenheim et al. 2022; Martino and Boghdady 2023). Therefore, the exploration of novel biomarkers for early diagnosis is important to overcome this fatal disease and provide key ideas for developing more effective strategies and approaches.
The therapeutic complexity of pancreatic cancer is not only reflected in the treatment method but also involves the critical role of nursing. When managing pancreatic cancer, nursing teams must focus on a range of important issues, including pain management, malnutrition, and potential complications (Spross et al. 1988; Hronek and Reed 2015). Comprehensive care is not only essential to improve the quality of life but also significantly improves the success of treatment. Therefore, in pancreatic cancer treatment, medical teams must work closely together to consider nursing as an integral part of the overall treatment plan. This collaborative work will help to better manage this extremely challenging disease, providing more comprehensive support and care for patients.
PABPC1 has been proved to play a key role in the growth and metastasis of various cancer cells (Feng et al. 2021). Feng et al. indicated that PABPC1 promote the ovarian cancer cell growth and invasion partly by modulating the EMT process (Feng et al. 2021). Zhang et al. reported that PABPC1 overexpression enhanced esophageal squamous cell proliferation and invasion by activating the IFN/IFI27 signaling pathway (Zhang et al. 2022). Meng et al. indicated that PABPC1 is involved in the proliferation and the EMT of bladder cancer cells (Meng et al. 2023). Moreover, PABPC1 accelerates BXPC3 cell proliferation and metastasis by regulating COL12A1 expression (Yao et al. 2023). This study explored the role and molecular regulatory mechanisms of PABPC1 in pancreatic cancer cells. Our studies shown that the expression of PABPC1 is significantly increased in pancreatic cancer tissues and cells and that the downregulation of PABPC1 significantly inhibits the proliferation of pancreatic cancer cells, induces apoptosis, and suppresses the EMT process in pancreatic cancer cells. Furthermore, PABPC1 is associated with the PI3K/AKT signaling pathway, and PABPC1 silencing inhibits the activation of this pathway. PABPC1 overexpression plays an opposite role in pancreatic cancer cells. These findings suggest that PABPC1 is a potential therapeutic target for pancreatic cancer.
Targeting the PI3K/Akt signaling pathway is a cutting-edge approach in cancer therapy. It has been found that the Akt pathway is activated in bronchial precancerous lesions in smokers and patients with lung cancer (Gadgeel and Wozniak 2013). Preclinical in vivo studies have demonstrated the preventive activity of deguelin and inositol in lung tumorigenesis, in part through inhibition of the PI3K/AKT pathway (Kyung-Hee Chun et al. 2003). The PI3K/ AKT signaling pathway plays a key role in cell growth, survival, proliferation, metabolism, and motility. Studies have reported that HOXD9-mediated PAXIP1-AS1 regulates gastric cancer progression via PABPC1/PAK1 (Li et al. 2023). In addition, PABPC1L inhibits the proliferation and migration of human colorectal cancer cells by blocking the AKT pathway (Wu et al. 2019). Our study indicated that PABPC1 activated the PI3L/AKT pathway in pancreatic cancer cells. These studies imply that PABPC1 may play a role in inhibiting the biological behavior of pancreatic cancer cells by interfering with the proliferation and metastasis of gastric cancer cells via regulation of the PI3K/AKT pathway. Further studies are needed to determine how PABPC1 affects the PI3K/AKT pathway by regulating the expression of E- and N-calmodulinAlthough the current experimental results showed potential anticancer effects in cellular assays in vitro, further animal experiments and clinical studies are needed to verify the feasibility of these findings. Therefore, future studies should focus on these issues to fully understand the potential and limitations of using PABPC1 as a therapeutic target for pancreatic cancer.
In summary, our study demonstrated that PABPC1 silencing inhibited proliferation, promoted apoptosis, and slowed the EMT process of pancreatic cancer cells by inhibiting the PI3K/AKT pathway. These findings provide novel molecular targets and mechanisms for the therapeutic and prognostic evaluation of pancreatic cancer. In clinical practice, nursing care of patients with pancreatic cancer should be strengthened to improve early diagnosis and comprehensive treatment to achieve better efficacy.
Data availability
The datasets used and/or analyzed in the current study are available from the corresponding author upon reasonable request.
References
Andersson R, Haglund C, Seppanen H, Ansari D (2022) Pancreatic cancer-the past, the present, and the future. Scand J Gastroenterol 57:1169–1177. https://doi.org/10.1080/00365521.2022.2067786
Chen H, Zhou L, Wu X, Li R, Wen J, Sha J, Wen X (2016) The PI3K/AKT pathway in the pathogenesis of prostate cancer. Front Biosci (Landmark Ed) 21:1084–1091. https://doi.org/10.2741/4443
Di Martino M, El Boghdady M (2023) Pancreatic cancer surgery. BMC Surg 23:196. https://doi.org/10.1186/s12893-023-02091-7
Feng C, Han YH, Qi N, Li J, Sheng QH, Liu Y, Yang LL (2021) Functional implications of PABPC1 in the development of ovarian cancer. Open Med 16:805–815. https://doi.org/10.1515/med-2021-0278
Gadgeel SM, Wozniak A (2013) Preclinical rationale for PI3K/Akt/mTOR pathway inhibitors as therapy for epidermal growth factor receptor inhibitor-resistant non-small-cell lung cancer. Clin Lung Cancer 14:322–332. https://doi.org/10.1016/j.cllc.2012.12.001
Gugenheim J, Crovetto A, Petrucciani N (2022) Neoadjuvant therapy for pancreatic cancer. Updates Surg 74:35–42. https://doi.org/10.1007/s13304-021-01186-1
Guven E (2022) Gene expression characteristics of tumor and adjacent non-tumor tissues of pancreatic ductal adenocarcinoma (PDAC) in-silico. Iran J Biotechnol 20:e3092. https://doi.org/10.30498/ijb.2021.292558.3092
Hronek JW, Reed M (2015) Nursing implications of chemotherapy agents and their associated side effects in patients with pancreatic cancer. Clin J Oncol Nurs 19:751–757. https://doi.org/10.1188/15.CJON.751-757
Hu Y, Jing J, Shi Y, Zhang P, Dong D, Wu Y, Dong X, Li E, Fan Y (2021) Apatinib inhibits pancreatic cancer growth, migration and invasion through the PI3K/AKT and ERK1/2/MAPK pathways. Trans Cancer Res 10:3306–3316. https://doi.org/10.21037/tcr-21-207
Jie Zhu HD, Wang X, Lu Q (2015) PABPC1 exerts carcinogenesis in gastric carcinoma by targeting miR-34c. Int J Clin Exp Pathol 8:3794–3802
Klein AP (2021) Pancreatic cancer epidemiology: understanding the role of lifestyle and inherited risk factors. Nat Rev Gastroenterol Hepatol 18:493–502. https://doi.org/10.1038/s41575-021-00457-x
Kumar P, Nagarajan A, Uchil PD (2018) Analysis of cell viability by the MTT assay. Cold Spring Harbor Protoc. https://doi.org/10.1101/pdb.prot095505
Kyung-Hee Chun JWKI, Shihua Sun JM, Pezzuto R, Lotan WK, Lee HH-Y (2003) Effects of deguelin on the phosphatidylinositol 3-Kinase/Akt pathway and apoptosis in Premalignant Human bronchial epithelial cells. J Natl Cancer Inst 95:291–302. https://doi.org/10.1093/jnci/95.4.291
Lei Y, Liu B, Su L, Xie X, Kuang M, Chen M, Lan H, Zhao H, Lin M (2020) Perioperative nursing of patients with pancreatic cancer treated with a nanoknife. J Nanosci Nanotechnol 20:6584–6590. https://doi.org/10.1166/jnn.2020.18603
Li J, Pei M, Xiao W, Liu X, Hong L, Yu Z, Peng Y, Zhang J, Yang P, Lin J, Wu X, Lin Z, Tang W, Zhi F, Li G, Xiang L, Li A, Liu S, Chen Y, Wang J (2023) The HOXD9-mediated PAXIP1-AS1 regulates gastric cancer progression through PABPC1/PAK1 modulation. Cell Death Dis 14:341. https://doi.org/10.1038/s41419-023-05862-5
Liu X, Wen L, Gao C (2022) Effect of evidence-based nursing on quality of life and nursing satisfaction of patients with severe pancreatic cancer. Minerva Gastroenterol 68:495–497. https://doi.org/10.23736/S2724-5985.22.03241-7
Luo W, Tao J, Zheng L, Zhang T (2020) Current epidemiology of pancreatic cancer: challenges and opportunities. Chin J Cancer Res 32:705–19
Ma W, Zhang L, Wang C, Xu X (2022) Effect of multidisciplinary team collaborative nursing model combined with mind mapping teaching method on postoperative complications and mental health of patients with advanced pancreatic cancer. Iran J Public Health 51:535–543. https://doi.org/10.18502/ijph.v51i3.8929
Meng X, Xiao W, Sun J, Li W, Yuan H, Yu T, Zhang X, Dong W (2023) CircPTK2/PABPC1/SETDB1 axis promotes EMT-mediated tumor metastasis and gemcitabine resistance in bladder cancer. Cancer Lett 554:216023. https://doi.org/10.1016/j.canlet.2022.216023
Mortazavi M, Moosavi F, Martini M, Giovannetti E, Firuzi O (2022) Prospects of targeting PI3K/AKT/mTOR pathway in pancreatic cancer. Crit Rev Oncol/Hematol 176:103749. https://doi.org/10.1016/j.critrevonc.2022.103749
Mukherji R, Debnath D, Hartley ML, Noel MS (2022) The role of immunotherapy in pancreatic cancer. Curr Oncol 29:6864–6892. https://doi.org/10.3390/curroncol29100541
Ozturk S, Uysal F (2017) Poly(A)-binding proteins are required for translational regulation in vertebrate oocytes and early embryos. Reprod Fertil Dev 29:1890–1901. https://doi.org/10.1071/RD16283
Ozturk S, Uysal F (2018) Potential roles of the poly(A)-binding proteins in translational regulation during spermatogenesis. J Reprod Dev 64:289–296. https://doi.org/10.1262/jrd.2018-026
Shao Q, Zhang Z, Cao R, Zang H, Pei W, Sun T (2020) CPA4 promotes EMT in pancreatic cancer via stimulating PI3K-AKT-mTOR signaling. OncoTargets Therapy 13:8567–8580. https://doi.org/10.2147/OTT.S257057
Spross JA, Manolatos A, Thorpe M (1988) Pancreatic cancer: nursing challenges. Semin Oncol Nurs 4:274–284. https://doi.org/10.1016/0749-2081(88)90079-4
Stoffel EM, Brand RE, Goggins M (2023) Pancreatic cancer: changing epidemiology and new approaches to risk assessment, early detection, and prevention. Gastroenterology 164:752–765. https://doi.org/10.1053/j.gastro.2023.02.012
Tailai An LD, Wang Y, Yang Z, Chai C, Ouyang J, Lu X, Zhang C (2021) The prognostic impacts of PABPC1 expression on gastric cancer patients. FutureOncol 17:4471–4479
Vincent A, Herman J, Schulick R, Hruban RH, Goggins M (2011) Pancreatic cancer. Lancet 378:607–620. https://doi.org/10.1016/s0140-6736(10)62307-0
Wen X, Shao Z, Chen S, Wang W, Wang Y, Jiang J, Ma Q, Zhang L (2020) Construction of an RNA-binding protein-related prognostic model for pancreatic adenocarcinoma based on TCGA and GTEx databases. Front Genet 11:610350. https://doi.org/10.3389/fgene.2020.610350
Wood LD, Canto MI, Jaffee EM, Simeone DM (2022) Pancreatic cancer: pathogenesis, screening, diagnosis, and treatment. Gastroenterology 163:386–402. https://doi.org/10.1053/j.gastro.2022.03.056
Wu YQ, Ju CL, Wang BJ, Wang RG (2019) PABPC1L depletion inhibits proliferation and migration via blockage of AKT pathway in human colorectal cancer cells. Oncol Lett 17:3439–3445. https://doi.org/10.3892/ol.2019.9999
Yao W, Yao Y, He W, Zhao C, Liu D, Wang G, Wang Z (2023) PABPC1 promotes cell proliferation and metastasis in pancreatic adenocarcinoma by regulating COL12A1 expression. Immun Inflamm Dis 11:e919. https://doi.org/10.1002/iid3.919
Yu L, Wei J, Liu P (2022) Attacking the PI3K/Akt/mTOR signaling pathway for targeted therapeutic treatment in human cancer. Sem Cancer Biol 85:69–94. https://doi.org/10.1016/j.semcancer.2021.06.019
Zhang Y, Chen C, Liu Z, Guo H, Lu W, Hu W, Lin Z (2022) PABPC1-induced stabilization of IFI27 mRNA promotes angiogenesis and malignant progression in esophageal squamous cell carcinoma through exosomal miRNA-21-5p. J Exp Clin Cancer Res 41:111. https://doi.org/10.1186/s13046-022-02339-9
Acknowledgements
Not applicable.
Funding
No fundings were recieved.
Author information
Authors and Affiliations
Contributions
Changren Zhu and Cuimei Wang contributed to data collection, statistical analysis, data interpretation and manuscript preparation. Jun Zheng contributed to data collection and manuscript preparation. Xiaodong Wang, Shuangshuang Dong, and Qing Xu contributed to data collection and data interpretation. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
This study was approved by the Ethics Committee of Northern Jiangsu People’s Hospital of Jiangsu Province.
Consent to participant
All participants providedsigned informed consent.
Consent for publication
All patients agreed for publication.
Additional information
Publisher’s Note
Springer nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary material 1 (TIF 1380.6 kb)
Effect of PABPC1-siRNA on the proliferation and apoptosis of normal human pancreatic epithelial cell line HPDE 6-C7.HPDE 6-C7 cells were transfected with control-siRNA of PABPC1-siRNA for 48 h. A Cell proliferation was assessed by MTT assay. B and C Cell apoptosis was determined by FCM
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhu, C., Wang, C., Wang, X. et al. PABPC1 silencing inhibits pancreatic cancer cell proliferation and EMT, and induces apoptosis via PI3K/AKT pathway. Cytotechnology 76, 351–361 (2024). https://doi.org/10.1007/s10616-024-00626-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10616-024-00626-1