Abstract
Research on positive emotion disturbance has gained increasing attention, yet it is not clear which specific positive emotions are affected by mood symptoms, particularly during the critical period of adolescence. This is especially pertinent for identifying potential endophenotypic markers associated with mood disorder onset and course. The present study examined self-reported discrete positive and negative emotions in association with clinician-rated manic and depressive mood symptoms in a clinically and demographically diverse group of 401 outpatient adolescents between 11 and 18 years of age. Results indicated that higher self reported joy and contempt were associated with increased symptoms of mania, after controlling for symptoms of depression. Low levels of joy and high sadness uniquely predicted symptoms of depression, after controlling for symptoms of mania. Results were independent of age, ethnicity, gender and bipolar diagnosis. These findings extend work on specific emotions implicated in mood pathology in adulthood, and provide insights into associations between emotions associated with goal driven behavior with manic and depressive mood symptom severity in adolescence. In particular, joy was the only emotion associated with both depressive and manic symptoms across adolescent psychopathology, highlighting the importance of understanding positive emotion disturbance during adolescent development.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bipolar spectrum disorders (referred to as BPSD) involve severe and recurring mood symptomatology, affecting up to 4 % of the general population over the course of a lifetime (e.g., Kessler et al. 2005) and roughly 2 % of adolescents world-wide (Van Meter et al. 2011). Severe mood symptoms include both manic symptoms associated with heightened and persistent elevated mood and increased reward seeking and goal pursuit, and depressive symptoms associated with depressed mood and decreased reward seeking and goal pursuit. Importantly, severe mood disturbance is ranked among the top ten causes of medical disability worldwide (Gore et al. 2011; Lopez et al. 2006). In many affected individuals, clear manifestations of manic and depressive mood symptoms do not appear until adolescence (Merikangas et al. 2007). During the adolescent period, pivotal maturational and environmental events occur that can trigger mood symptom onset according to neurodevelopmental models of mood disturbance (Goodwin and Jamison 2007; Johnson and McMurrich 2006). It is important to examine this period of risk in order to improve diagnostic accuracy as well as to validate potential endophenotypic markers of mood disturbance (Gottesman and Gould 2003; Hasler et al. 2006).
Although research on mechanisms underlying mood symptom severity in adolescence has expanded in the last decade (e.g., Geller and Luby 1997; Youngstrom et al. 2008), continued efforts to identify psychosocial processes are needed. These research efforts promise to improve risk assessment, diagnosis, and early targeted treatment (e.g., Miklowitz and Chang 2008; Youngstrom et al. 2005). Adolescence is a developmental period characterized by many changes in affective experience, particularly heightened emotional reactivity. For instance, across negative and positive affective stimuli, adolescents exhibit increased subjective, physiological and neurobiological responding compared with younger children and adults (Larson and Lampman-Petraitis 1989; Quevedo et al. 2009; Somerville et al. 2010; Silk et al. 2009). Subjective negative affect appears to increase while subjective positive affect decreases across adolescence (Larson et al. 2002; Henker et al. 2002). Adolescents also report greater fluctuations in daily emotional states, and this emotional variability itself appears to change over adolescence as happiness, sadness and anger all decline from early to late adolescence (Maciejewski et al. 2015). Given the numerous developmental affective changes occurring during adolescence, we specifically seek to investigate disturbances in emotional valence systems in association with mood symptom disturbance. Understanding these mechanisms may shed light on inter-episode dysfunction and predict subsequent relapse across psychiatric conditions and in BPSDs. This emphasis is highly consistent with recent initiatives to isolate disturbances in positive and negative valence systems through the NIMH Research Domain Criteria or RDoC (e.g., Insel et al. 2010; Sanislow et al. 2010) and more general models of positive emotion disturbance in mood disorders (e.g., Hofmann et al. 2012; Stanton et al. in press; Watson and Naragon-Gainey 2010).
Positive Emotions and Mood Symptom Disturbance: Need for Specificity
Recent theories of mood disturbance, particularly for BPSDs, implicate disturbances in positive emotional systems (e.g., Alloy and Abramson 2010; Gruber et al. 2011; Johnson 2005). A hallmark feature of mania symptomatology includes abnormally elevated and persistent positive mood (American Psychiatric Association 2013). Descriptive accounts of BPSDs prominently feature feelings of “exuberance,” including experiences of excitement, interest, and euphoria (Jamison 2005). More recent empirical work converges with these observations to support the centrality of positive emotional disturbances in bipolar symptomatology (e.g., Gruber et al. 2014).
However, most work on bipolar mood disturbance has traditionally emphasized broad dimensions of positive emotion assessment. This includes measurement of unidimensional constructs of “happiness” or “positive mood” which lack specificity as to which particular emotions are impacted. Recent work in affective science, importantly, supports the validity of differentiating among a variety of functionally distinct positive emotions that differ in their function and response profile (Campos and Keltner 2014; Fredrickson 1998; Shiota et al. 2006; Tracy and Robins 2004). Animal neuroscience models also encourage the utility of differentiating among distinct emotional states (Burgdorf and Panksepp 2006; Panksepp 1998). For example, joy (or happiness) is a reward-oriented emotion experienced when the environment signals an imminent improvement in resources, motivating the individual to acquire material resources and rewards such as joy (e.g., joy; Berridge and Kringelbach 2008; Harmon-Jones and Gable 2009; Rolls 1999). Recent work on joy suggests it is uniquely associated with behavioral displays (i.e., Duchenne smiles) that are robustly associated with self-reported joy (Keltner et al. 2003). Interest (or curiosity) is experienced when people encounter novel information usually consistent with their current worldview, which promote engagement with the environment and knowledge consolidation (Fredrickson 1998; Izard 1977; Shiota et al. 2006). Although, anger—also a common feature of mania symptom severity (American Psychiatric Association 2013)—is negatively valenced, it shares many important neurophysiological and behavioral features with positive emotions, including increased left hemispheric activation (Harmon-Jones and Allen 1998) and approach behavior tendencies towards the pursuit of goals (e.g., Carver 2004; Panksepp 1998; Youngstrom and Izard 2008). As an approach-oriented emotion that mobilizes the body to overcome an obstacle impeding goal pursuit, anger is highly correlated with positive affectivity (Harmon-Jones 2003; Harmon-Jones and Gable 2009).
Positive Emotion and Adolescent Mood Disturbance
Understanding the concurrent relationship between positive emotions and mood symptom severity in adolescence is a high priority (e.g., Forbes and Dahl 2005; Gilbert 2012). Yet there is little known about the ways specific emotions map onto bipolar mood symptomatology. For example, although mania symptoms in adolescents have been associated with decreased neural activity and lower sensitivity to identifying happy faces (Diler et al. 2013; Guyer et al. 2007; Rich et al. 2008), we know little about the specific positive emotions driving these responses. Moreover, adolescents at risk for or with depression demonstrate blunted reward responding that is associated with lower levels of daily positive emotion (Forbes et al. 2009) while decreased happiness predicts the onset of depressive symptoms (Neumann et al. 2011). Similar to adult literature, adolescent BPSDs are characterized by dysregulated reward learning (Dickstein et al. 2009) and increased reward sensitivity and approach-motivated behaviors being associated with elevated manic symptoms (Gruber et al. 2013). Taken together, elevated reward-seeking positive emotions (such as joy) and increased goal approach-motivated emotions (including anger) appear to be linked to manic and depressive symptoms in adolescents. This work underscores the clinical significance of applying a discrete emotions framework to mood disturbance in adolescence.
We suggest that a discrete emotions perspective may advance the study of adolescent mood disturbance for several reasons. First, application of a discrete framework has yielded unique insights into better understanding both manic and depressive symptom profiles in adults (e.g., Gruber et al. 2011). For example, adults at risk for mania report specific elevations in high arousal positive emotions (e.g., joy and interest), which prospectively predict increased mania symptom severity (Gruber et al. 2009). Moreover, adults with bipolar disorder report greater approach-related emotions such as anger (Dutra et al. 2014). These findings suggest a potential benefit by applying similar methodological approaches to adolescents. Second, this work is an important contributor to a growing emphasis on understanding a variety of specific positive (and negative) emotions experienced in adolescence (e.g., Leibenluft 2011).
The Present Investigation
The present study examined whether theoretically relevant positive emotions (and approach-related negative emotions) represent an endophenotypic marker that contributes to BPSD-related mood symptoms in adolescents. Given growing emphasis on examining psychopathology processes and associated symptoms dimensionally (Insel et al. 2010; Prisciandaro and Roberts 2011; Prisciandaro and Tolliver 2015), we focused on mania and depression symptom severity across a demographically diverse and diagnostically heterogeneous adolescent outpatient sample. Though we were primarily interested in examining the associations between emotion and mood symptoms dimensionally, we also performed a series of ANOVA models as sensitivity analyses to assess whether there were differences in average emotion scores across diagnostic categories. These results complement the main analyses by providing description of differences between diagnostic groups, which have the advantage of familiarity, combined with limitations due to heterogeneity of symptom presentation and comorbidity. We also examined whether the emotion variables were associated with any of the demographic variables (age, race, sex) using correlational analyses. Following these preliminary analyses, two primary aims were examined focusing on specific positive emotions as predictors of mania and depressive mood symptoms, respectively.
First, based on the supposition that a central psychosocial factor associated with increased manic symptoms in adults involves increased approach or pursuit of goals in the environment (Alloy and Abramson 2010; Johnson 2005; Meyer et al. 2001; Urosevic et al. 2008), we tested whether elevations of specific positive emotions associated with goal approach such as joy (also referred to as excitement or happy) (Shiota et al. 2006) were associated with increased symptoms of mania (Hypothesis 1a). We additionally examined whether elevations in the negative emotions of anger and contempt—closely associated with symptoms of mania and approach behavior in the pursuit of goals (Carver 2004; Harmon-Jones and Allen 1998)—were also associated with increased symptoms of mania (Hypothesis 1b). To test these hypotheses, we first controlled for symptoms of depression, and then examined whether symptoms of mania were uniquely associated with self-reported joy and anger, but not other positive or negative emotions. We also examined whether this same relationship held when examining these same approach-related emotions (i.e., joy, anger, contempt) versus all other emotions using a validated hierarchical linear regression model (Blumberg and Izard 1985, 1986).
Second, based on the supposition that increased depressive symptoms in adults involves decreased pleasure and approach towards goals (Alloy and Abramson 2010; Davidson et al. 2002; Dillon and Pizzagalli 2010), we tested whether a deficit in the specific positive emotion of joy was associated with increased symptoms of depression (Hypothesis 2a). We additionally examined whether the specific negative emotion associated with reduced goal approach and pleasure, or sadness (Gable and Harmon-Jones 2010), was associated with increased symptoms of depression, based on work in children associating specific reports of sadness with increased depressive symptoms (Blumberg and Izard 1986) (Hypothesis 2b). To test these hypotheses, we first controlled for symptoms of mania, and then examined whether symptoms of depression were uniquely associated with self-reported joy (inversely), as well as the negative emotions of sadness, guilt and hostility also implicated with depressive symptoms. To gain greater specificity in our findings, we further examined whether this same relationship held examining these same four emotions (i.e., joy, sadness, guilt, hostility) versus all other emotions using a validated hierarchical linear regression model (Blumberg and Izard 1985, 1986). Finally, we used net regression (Cohen and Cohen 1983) to test whether any of the emotion variables or covariates (age sex, race) was uniquely related to either manic or depressive symptoms (See Table 5).
Methods
Participants
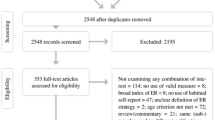
English-speaking adolescents and their primary caregiver were recruited from two agencies: a consecutive case series of youth presenting for services from an urban community mental health center (n = 293) and youth who were recruited for a variety of treatment studies for bipolar disorder or for other childhood disorders from an academic outpatient medical center (n = 108). The resulting sample was demographically and diagnostically diverse; youth from the community mental health center were more likely to be Black [X 2(4) = 219.38, p < .0001] and youth from the academic medical center were more likely to have a BPSD diagnosis (X 2(1) = 21.48, p < .0001). Youth from the community mental health center reported more contempt [t(392) = 2.27, p = .024], youth from the academic medical center reported more self-directed hostility [t(159.37) = 2.92, p = .004]. There were no other significant differences in self-reported positive or negative emotion or on other demographic variables. Potential participants were excluded if they suffered from a pervasive developmental disorder or cognitive disability. For the present study, only youth aged 11–18 were included given our specific a priori interest in adolescents’ self-reported positive emotion. See Table 1 for demographic and clinical characteristics.
Measures
DSM-IV-TR Diagnoses
All DSM-IV-TR diagnoses for adolescent participants were made based on the information provided during a semi-structured interview using the Kiddie Schedule for Affective Disorders and Schizophrenia—Present and Lifetime version (KSADS-PL; Kaufman et al. 1997), along with the mood disorders modules of the WASH-U-K-SADS (Geller et al. 2001), which inquires more extensively about symptoms of depression and mania. Raters were highly trained (criterion of K > .85 at the item level on five interviews conducted by a reliable rater, and then K > .85 on five interviews they led themselves) prior to conducting interviews independently. Adolescent participants and their parents (or caregivers) were interviewed sequentially by the same rater, resolving discrepancies through re-interviewing and clinical judgment. KSADS interviews resulted in DSM-IV diagnoses, including bipolar I, bipolar II, cyclothymic disorder, and bipolar not otherwise specified (NOS). The diagnosis of bipolar NOS was made in cases of hypomanic or manic symptoms that did meet criteria for another bipolar diagnosis, usually due to insufficient duration criteria. KSADS diagnoses were reviewed at a diagnostic consensus meeting, including at least one licensed clinician. The diagnostic consensus meeting followed the Longitudinal Evaluation of All Available Data (LEAD) standard of diagnosis to designate all diagnostic categories (Spitzer 1983). LEAD diagnoses took into account the information collected through the K-SADS interview, prior treatment history, family history, and clinical judgment. For purposes of comparing groups of diagnoses, we used a hierarchical system of categories focused on mood disorders that has been used successfully in previous studies of mood disorders in youth (Youngstrom et al. 2001; Youngstrom et al. 2008). Kappas for both BPSD diagnosis (=.91) and for all diagnoses (=.95) were good comparing consensus versus K-SADS diagnosis (Youngstrom et al. 2005).
Mood Symptoms
The KSADS diagnostic interview assessed adolescents’ current and lifetime mood episodes. The KSADS Mania Rating Scale (KMRS) and KSADS Depression Rating Scale (KDRS) provided severity ratings of all mood symptoms relevant to the DSM-IV criteria for mania and depression (Axelson 2002). The KMRS scores ranged from 11 to 58 (M = 20.54, SD = 9.40) and KDRS scores ranged from 12 to 52 (M = 24.17, SD = 9.66) with higher scores indicating greater symptom severity. Scores on both the KMRS and KDRS showed excellent internal consistency (α = .92 and .86 in this sample, respectively). The present analyses used current episode ratings, based on a summary of youth and parent reported symptoms, in order to examine more state-specific associations between current mood symptom severity and emotional experiences in adolescents.
Self-Reported Positive and Negative Emotion
Self-reported positive and negative emotions were provided by the adolescent using the Differential Emotions Survey, Fourth Revision (DES-IV; Izard et al. 1993). Its 36 items are rated on a five-point scale from 1 (rarely or never) to 5 (very often) asking respondents to indicate the extent to which they experience each emotion in their daily life. The present study used all 12 DES-IV emotion subscales: Joy (α = .71), Interest (α = .68), Surprise (α = .67), Sadness (α = .81), Anger (α = .79), Self-directed hostility (α = .80), Shame (α = .73), Guilt (α = .70), Disgust (α = .68), Contempt (α = .64), Fear (α = .84) and Shyness (α = .75).
Procedure
Participants were enrolled consecutively. In rare cases when referrals exceeded capacity, participants were chosen at random. All parents (or caregivers) and adolescents completed the informed consent process. All participants were treatment seeking. The research interview occurred shortly after intake, or served as the intake if the participants were enrolling directly into one of several treatment studies open during the course of the study. During the parent’s KSADS interview, the adolescent participant completed a series of questionnaires and other study components with a second research assistant, including the DES-IV. The adolescent then completed the KSADS with the same rater who had interviewed his/her parent on the same day.
Results
Preliminary Analyses
Before testing our hypotheses, we first assessed bivariate correlations between the DES-IV scores and the demographic variables. Results revealed that age was negatively correlated with joy (r = −.13, p = .01)—consistent with other recent reports (Uusitalo-Malmivaara 2014)—and positively correlated with sadness (r = .23, p < .0005), anger (r = .20, p < .0005), and self-directed-hostility (r = .13, p = .01). However, age was not correlated with interest (r = −.03, p = .51), disgust (r = .05, p = .35), fear (r = .00, p = .94), guilt (r = .04, p = .46), shame (r = .01, p = .80), or contempt (r = .10, p = .06). For sex, females reported higher scores on anger (p < .0005), sadness (p < .0005), contempt (p < .0005), shyness (p < .0005), guilt (p < .0005), shame (p < .0005), self-directed hostility (p = .001), disgust (p = .002), surprise (p = .014), and fear (p = .024). Females reported lower scores on joy (p = .04). For race, Caucasians reported higher contempt (p = .003) and self-directed hostility (p = .001) scores compared to non-Caucasian participants. In order to control for these demographic variables, we included age, gender, and race in Block 1 of the regression models. We also tested whether the average DES-IV scores varied by diagnostic group (BD, MDD, disruptive behavior disorders, and other disorders). There were between group differences for the following emotions: sadness (η 2 = .07, p < .0005), joy (η 2 = .07, p < .0005), self-directed hostility (η 2 = .06, p < .0005), anger (η 2 = .05, p = .001), shame (η 2 = .04, p = .002), guilt (η 2 = .04, p < .0005), shyness (η 2 = .04, p = .003), and contempt (η 2 = .03, p = .022). There were no differences in reported interest, surprise, disgust, or fear (all ps > .05). Given our interest in measuring the relations between specific emotions and symptoms of mania and depression, independent of diagnosis, we decided to include diagnosis (BPSD Y/N) in the final block of our regression analyses, in order to determine whether a bipolar diagnosis, above and beyond specific emotions, accounted for variance in manic or depressive symptoms. Finally, the relationship between symptoms of mania and depression was assessed, and consistent with previous research in adolescents (Youngstrom et al. 2008) mood symptom scores were positively correlated with each other (r = .51, p < .0005).
Aim 1: Emotion as a Predictor of Mania Symptoms
To assess the relationship between specific emotions with symptoms of mania, we computed partial correlations between symptoms of mania and each of the 12 discrete DES-IV subscales while controlling for depression symptom scores.Footnote 1 As indicated in Table 2, symptoms of mania were significantly associated with increased joy (but no other positive emotion terms) and a trend towards decreased sadness (but no other negative emotion terms).
To gain greater specificity in our findings, we further examined whether symptoms of mania were uniquely associated with approach-oriented emotions (i.e., joy, anger, contempt), over and above other emotions (i.e., shyness, guilt, interest, surprise, disgust, self-directed hostility, shame, fear). Towards this aim we conducted a hierarchical multiple regression (Blumberg and Izard 1985, 1986) with Block 1 controlling for of age, gender (Male = 0, Female = 1) and race (Caucasian = 0, Non-Caucasian = 1) as well as depressive symptoms (KDRS). Block 2 included the primary emotions of interest (joy, anger, contempt)Footnote 2 and Block 3 included all other emotions. In Block 4, bipolar diagnosis (Y/N) was added to determine whether diagnosis, above and beyond emotion, was associated with manic symptoms. Missing data were deleted listwise, multicollinearity diagnostics showed satisfactory tolerance statistics, and Cook’s distance and standardized DFBeta for each predictor revealed no influential cases (Cook and Weisberg 1982; Myers 1990). As shown in Table 3, KDRS scores and demographic variables (Block 1) were significant predictors of KMRS scores (R 2 = .29), with control variables of age (β = −.10, p = .04) and KDRS (β = .54, p < .0005) predicting KMRS scores. When mania-related emotions were added in Block 2, the overall model was significant (R 2 = .32, ∆R 2 = .03); both joy (β = .12, p = .01) and contempt (β = .11, p = .04) were positively related to KMRS scores. None of the emotions added in Block 3 were significant. In the final Block, bipolar diagnosis was a significant predictor (β = .69, p < .001; ∆R 2 = .37). Age (β = −.08, p = .02), and KDRS scores (β = .27, p < .0005) also remained significant in the final model. Guilt (β = −.09, p = .047) was the only significant emotion in the final model. In the final model, 70 % of the variance in mania scores was accounted for by the predictors.
Aim 2: Emotion as a Predictor of Depression Symptoms
To assess the relationship between specific positive emotions with symptoms of depression, we computed partial correlations between symptoms of depression and each of the 12 discrete DES-IV subscales while controlling for mania symptom scores. As indicated in Table 2, symptoms of depression were associated with decreased joy (but no other positive emotion terms) and increased sadness, anger, self-directed hostility, shame, guilty, disgust, fear and shyness (but not contempt).
Again, we further examined whether symptoms of depression were uniquely associated with reduced approach-oriented emotions (i.e., joy) as well as negative emotions associated with loss and low approach-motivation and self-directed negative feelings common in depression (i.e., sadness, guilt, self-directed hostility), above and all other emotions (i.e., shame, anger, disgust, contempt, shyness, fear, interest, surprise) using the same analytic approach described above (Blumberg and Izard 1985, 1986). As shown in Table 4, KMRS scores and demographic variables (Block 1), were significant (R 2 = .35) with control variables of age (β = .20, p < .001), gender (β = .15, p = .002), and KMRS (β = .50, p < .0005) scores predicting KDRS scores. When hypothesized emotions of interest were added in Block 2, the overall model was significant (R 2 = .43, ∆R 2 = .08), with age (β = .154, p = .001) and KMRS scores (β = .48, p < .0005) remaining significant, along with the emotions of joy (β = −.16, p < .0005) and sadness (β = .18, p = .01). None of the emotions added in Block 3 were significant predictors. In the final Block, bipolar diagnosis was not a significant predictor (β = −.03, p = .68; ∆R 2 = .00). Age (β = .15, p = .001), KMRS scores (β = .51, p < .001), and joy (β = −.19, p < .0005) were also significant predictors in the final model; predictors accounted for 44 % of the variance in depression scores.
Finally, net regression analysis, was used to test whether any of the emotion scores or demographic variables were uniquely related to the mood symptom scales (See Table 5). The results indicated joy is more strongly related to mania scores than to depression scores (p = .002). Additionally, older age was more strongly associated with depression scores than mania scores (p = .005). The other emotion variables did not have a stronger relation with either mood symptom scale.
Discussion
Research on positive emotion disturbance has gained increasing attention, yet it has remained less clear the concurrent and likely bidirectional relationship between positive emotions and mood symptoms during the critical period of adolescence. This is especially pertinent for identifying potential endophenotypic markers associated with illness onset and course. We investigated associations between mood symptoms and self-reported positive and negative emotions in a large adolescent outpatient sample. Results suggested unique associations between symptoms of mania with both increased joy and contempt, and between symptoms of depression with both increased sadness and decreased joy. These patterns were independent of specific diagnosis, underscoring the importance of adopting a dimensional approach to thinking about mood pathology (Helzer et al. 2006; Insel et al. 2010; Sanislow et al. 2010). These findings extend work on specific emotions implicated in mood pathology in adulthood, and illuminate associations between emotions associated with goal driven behavior with mood symptom severity in adolescence.
The first aim assessed the relationship between specific emotions with symptoms of mania in adolescents. Consistent with our predictions, symptoms of mania were associated with joy and contempt, but not with any other positive or negative emotions. With respect to joy, these findings dovetail with a growing literature suggesting mania symptoms involve a heightened focus on the pursuit of rewards and ambitious goals (Alloy and Abramson 2010; Johnson 2005; Meyer et al. 2001). Importantly in the emerging adolescent literature, these findings are consistent with work among outpatient adolescents suggesting that reward-relevant positive emotions were concurrently associated with increased manic symptom severity (Gruber et al. 2013). This work also is also consistent with research in adults with BPSD suggesting that increased reward sensitivity is concurrently associated with increased manic symptoms, providing encouraging support for developmental continuity in positive associations between reward-relevant emotions and mania symptoms (Alloy and Abramson 2010; Johnson 2005; Meyer et al. 2001; Urosevic et al. 2008). Our findings are also aligned with the adult literature suggesting that adults at risk for mania show unique elevations in self-reported positive emotions like joy, but not other types of other-oriented or low-arousal positive emotions (Gruber and Johnson 2009). These findings are also consistent with emerging literature suggesting that heightened reward sensitivity—which covaries with the experience of emotions like joy—may represent a candidate risk indicator for, and targeted treatment foci of, bipolar disorder (e.g., Alloy et al. 2015; Duffy et al. 2015). Interestingly, results between emotions and mania were only significant when controlling for depressive symptoms, but results held for depression when controlling manic symptoms. There are several potential interpretations of these results including potential covariation in symptom presentation common in mixed states, reliance on caregiver reports for symptom ratings scales which may be less sensitive to identifying manic versus depressive symptoms (e.g., Freeman et al. 2011; Youngstrom et al. 2015). Future work is warranted to continue to probe these and other possibilities, underscoring the importance of detecting underlying mechanisms, such as trait affect, driving both mood symptom presentations. Taken together, these findings suggest that increased manic symptoms during this critical neurodevelopmental phase may also be tied to emotional experiences related to goal pursuit and attainment. It will be important to continue to examine the role of specific types of positive emotionality in the developmental trajectory of BPSD across time, with a particular focus on reward-related positive states.
Additionally, the results indicating an association between contempt and manic symptoms in adolescence is consistent with work that has found heightened contempt among both adult (e.g., Dutra et al. 2014, 2016) and adolescent (Leibenluft 2011) bipolar populations. Importantly, elevations in contempt have been associated with heightened sensitivity of the Behavioral Approach System (Carver 2004; Harmon-Jones and Allen 1998), a central process implicated in the etiology of BD (Urosevic et al. 2008). This suggests that heightened contempt may arise when goal pursuit is thwarted and subsequently trigger the generation and exacerbation of mania in adolescents as well as adults (e.g., Johnson 2005). High levels of contempt may also help to explain the conflict and stressful interpersonal relationships common among adolescents with bipolar disorder (Algorta et al. 2011; Coville et al. 2008; Du Rocher Schudlich et al. 2008; Siegel et al. 2015), given a robust literature associating contempt with distinctly toxic effects in interpersonal relationships (Gottman 1994).
The second aim assessed the relationship between specific emotions with symptoms of depression in adolescents. Consistent with our predictions, symptoms of depression were uniquely associated with decreased joy and increased sadness, but not with any other positive or negative emotions, findings that also held when controlling for symptoms of mania and bipolar diagnosis. These results converge with robust findings in adults that postulate a core feature of depression involves decreased pleasure and approach towards goals (Alloy and Abramson 2010; Davidson et al. 2002; Dillon and Pizzagalli 2010) and decreased positive affectivity more generally (Brown et al. 1998; Chorpita and Daleiden 2002; Clark and Watson 1991; McMakin et al. 2011), which would be reflected in reduced joy. Our results associating increased sadness with depression symptoms are highly convergent with clinical observations (American Psychiatric Association 2013) and extant empirical work associating depression with increased reports of sadness in adults (e.g., Rottenberg et al. 2002). In addition, these results are supported by work linking sadness measured from a similar DES-IV self-report scale to prospective prediction of depression symptoms at a 4-month follow-up in children (Blumberg and Izard 1985, 1986). In RDoC terms, depression involves at least two major domains: increased negative affect, and decreased positive affect—corresponding to anhedonia and loss of interest as core features, and the “low PA” component of the tripartite model of depression and anxiety (Clark and Watson 1991). Future work should explore whether emotion-regulation strategies that feed sadness levels heighten adolescent depression (e.g., Millgram et al. 2015).
The results of the present study need to be interpreted within the confines of several limitations. First, the results of the present study were assessed exclusively with self-report indices of emotional states. Although this represented a good first step, future studies should utilize experimental inductions of distinct types of emotional states (e.g., emotion-eliciting films or images) and measuring concurrent physiological and behavioral indices of reward sensitivity. In addition, it will be valuable to more carefully examine a broader array of distinct positive emotional states moving forward. Second, the sample was comprised of a demographically diverse sample that contained a high percentage of low-income African-American adolescent families. Although this represents a strength of the present research by representing underserved and understudied minority groups, it may complicate direct comparisons with previous work. Third, we did not assess for pubertal status and its influence on emotion experience, especially important given differences in reward processing associated with pubertal timing. Fourth, the current study was cross-sectional and, as such, a longitudinal prospective high-risk sample design is warranted to more clearly disentangle the causal relationship between emotions and mood symptoms.
Despite these limitations, the present study adds to the small, but growing, literature examining associations between emotional experience and mood symptom severity, extending this work in a demographically diverse adolescent sample. Such findings advance our understanding of the relevance of these valenced systems in the etiology of mood psychopathology and targeted remediation with an explicit focus on emotional processing. The availability of free scales that measure focal constructs such as contempt and joy make it possible for both researchers and clinicians to examine the relevance of these constructs (Izard et al. 1993). Future steps include should identifying behavioral and pathophysiological processes associated with disrupted emotion processes in adolescents that may ultimately inform preventative treatment development.
Notes
Given that the individual emotion ‘interest’ may be dysregulated in mania (e.g., interest and engagement in goal-directed activities is a symptom of mania) and depression (e.g., decreased interest usually pleasurable activities is a symptom of depression) we also moved interest into Block 2 of regressions as a primary emotion of study. When doing so, Blocks and individual emotion significance remained unchanged and interest was not a significant predictor of symptoms.
Given the high rate of mixed symptom presentations among adolescents with mood disorders, and high degree of depressive features in hypo(mania) (e.g., Kraepelin 1921; Hunt et al. 2009; Kowatch et al. 2005; Van Meter et al. 2016), we chose to statistically control for symptoms in our planned analyses.
References
Algorta, G. P., Youngstrom, E. A., Frazier, T. W., Freeman, A. J., Youngstrom, J. K., & Findling, R. L. (2011). Suicidality in pediatric bipolar disorder: Predictor or outcome of family processes and mixed mood presentation? Bipolar Disorders, 13, 76–86. doi:10.1111/j.1399-5618.2010.00886.x.
Alloy, L. B., & Abramson, L. Y. (2010). The role of the behavioral approach system (BAS) in bipolar spectrum disorders. Current Directions in Psychological Science, 19, 189–194. doi:10.1177/0963721410370292.
Alloy, L. B., Nusslock, R., & Boland, E. M. (2015). The development and course of bipolar spectrum disorders: An integrated reward and circadian rhythm dysregulation model. Annual Review of Clinical Psychology, 11, 213–250. doi:10.1146/annurev-clinpsy-032814-112902.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing.
Axelson, D. A. (2002). KSADS mania rating scale. Pittsburgh, PH: University of Pittsburgh Medical Center.
Berridge, K., & Kringelbach, M. (2008). Affective neuroscience of pleasure: Reward in humans and animals. Psychopharmacology (Berl), 199(3), 457–480. doi:10.1007/s00213-008-1099-6.
Blumberg, S. H., & Izard, C. E. (1985). Affective and cognitive characteristics of depression in 10- and 11-year-old children. Journal of Personality and Social Psychology, 49(1), 194–202. Retrieved from http://europepmc.org/abstract/MED/4020613.
Blumberg, S. H., & Izard, C. E. (1986). Discriminating patterns of emotions in 10-and 11-yr-old children’s anxiety and depression. Journal of Personality and Social Psychology, 51, 852.
Brown, T. A., Chorpita, B. F., & Barlow, D. H. (1998). Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. Journal of Abnormal Psychology, 107, 179–192.
Burgdorf, J., & Panksepp, J. (2006). The neurobiology of positive emotions. Neuroscience and Biobehavioral Reviews, 30(2), 173–187. doi:10.1016/j.neubiorev.2005.06.001.
Campos, B., & Keltner, D. (2014). Shared and differentiating features of the positive emotion domain. In J. T. Moskowitz, & J. Gruber (Eds.), Positive emotion: Integrating the light sides and dark sides (pp. 52–71).
Carver, C. S. (2004). Negative affects deriving from the behavioral approach system. Emotion, 4(1), 3–22. doi:10.1037/1528-3542.4.1.3.
Chorpita, B. F., & Daleiden, E. L. (2002). Tripartite dimensions of emotion in a child clinical sample: Measurement strategies and implications for clinical utility. Journal of Consulting and Clinical Psychology, 70(5), 1150–1160. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=12362965.
Clark, L. A., & Watson, D. (1991). Tripartite model of anxiety and depression: Psychometric evidence and taxonomic implications. Journal of Abnormal Psychology, 100(3), 316–336.
Cohen, J., & Cohen, P. (1983). Applied multiple regression/correlation analysis for the behavioral sciences (3rd ed.). Hillsdale, NJ: Lawrence Erlbaum.
Cook, R. D., & Weisberg, S. (1982). Residuals and influence in regression. New York, NY: Chapman & Hall.
Coville, A. L., Miklowitz, D. J., Taylor, D. O., & Low, K. G. (2008). Correlates of high expressed emotion attitudes among parents of bipolar adolescents. Journal of Clinical Psychology, 64, 438–449. doi:10.1002/jclp.20463.
Davidson, R. J., Lewis, D. A., Alloy, L., Armaral, D. G., Bush, G., Cohen, J. D., et al. (2002). Neural and behavioral substrates of mood and mood regulation. Biological Psychiatry, 52, 478–502. doi:10.1016/S0006-3223(02)01458-0.
Dickstein, D. P., Finger, E. C., Brotman, M. A., Rich, B. A., Pine, D. S., Blair, J. R., et al. (2009). Impaired probabilistic reversal learning in youths with mood and anxiety disorders. Psychological Medicine, 40, 1089–1100. doi:10.1017/s0033291709991.
Diler, R. S., de Almeida, J. R. C., Ladouceur, C., Birmaher, B., Axelson, D., & Phillips, M. (2013). Neural activity to intense positive versus negative stimuli can help differentiate bipolar disorder from unipolar major depressive disorder in depressed adolescents: A pilot fMRI study. Psychiatry Research: Neuroimaging, 214(3), 277–284. doi:10.1016/j.pscychresns.2013.06.013.
Dillon, D. G., & Pizzagalli, D. (2010). Maximizing positive emotions: A translational, transdiagnostic look at positive emotion regulation. In A. Kring & D. S. Sloan (Eds.), Emotion regulation and psychopathology: A transdiagnostic approach to etiology and treatment (pp. 229–252). New York, NY: Guilford Press.
Du Rocher Schudlich, T. D., Youngstrom, E. A., Calabrese, J. R., & Findling, R. L. (2008). The role of family functioning in bipolar disorder in families. Journal of Abnormal Child Psychology, 36(6), 849–863. doi:10.1007/s10802-008-9217-9.
Duffy, A., Jones, S. H., Goodday, S., & Bentall, R. P. (2015). Candidate risk indicators for bipolar disorder: Early intervention opportunities in high-risk youth. International Journal of Neuropsychopharmacology. doi:10.1093/ijnp/pyv071.
Dutra, S. J., Reeves, E. J., Mauss, I. B., & Gruber, J. (2014). Boiling at a different degree: An investigation of trait and state anger in remitted bipolar I disorder. Journal of Affective Disorders, 168, 37–43. doi:10.1016/j.jad.2014.06.044.
Dutra, S. J., Siegle, G., Reeves, E. J., Mauss, I. B., & Gruber, J. (2016). Feeling without thinking? Anger provocation task predicts impaired cognitive performance in bipolar disorder but not major depression or healthy adults. Cognitive Therapy and Research, 40(2), 139–149. doi:10.1007/s10608-015-9734-0.
Forbes, E., & Dahl, R. (2005). Neural systems of positive affect: Relevance to understanding child and adolescent depression? Development and Psychopathology, 17, 827–850. doi:10.1017/S095457940505039X.
Forbes, E., Hariri, A. R., Martin, S. L., Moyles, D. L., Fisher, P. M., Brown, S. M., et al. (2009). Altered striatal activation predicting real-world positive affect in adolescent major depressive disorder. American Journal of Psychiatry. doi:10.1176/appi.ajp.2008.07081336.
Fredrickson, B. L. (1998). What good are positive emotions? Review of General Psychology, 2, 300–319.
Freeman, A. J., Youngstrom, E. A., Freeman, M. J., Youngstrom, J. K., & Findling, R. L. (2011). Is caregiveradolescent disagreement due to differences in thresholds for reporting manic symptoms? Journal of Child and Adolescent Psychopharmacology, 21, 425–432. doi:10.1089/cap.2011.0033.
Gable, P. A., & Harmon-Jones, E. (2010). The blues broaden, but the nasty narrows: Attentional consequences of negative affects low and high in motivational intensity. Psychological Science, 21, 211–215. doi:10.1177/0956797609359622.
Geller, B., & Luby, J. (1997). Child and adolescent bipolar disorder: A review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry, 36(9), 1168–1176. doi:10.1097/00004583-199709000-00008.
Geller, B., Zimmerman, B., & Williams, M. (2001). Reliability of the Washington University in St. Louis Kiddie Schedule for Affective Disorders and Schizophrenia (WASH-UKSADS) mania and rapid cycling sections. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 450–455. doi:10.1097/00004583-200104000-00014.
Gilbert, K. E. (2012). The neglected role of positive emotion in adolescent psychopathology. Clinical Psychology Review, 32(6), 467–481. doi:10.1016/j.cpr.2012.05.005.
Goodwin, F. K., & Jamison, K. R. (2007). Manic-depressive illness. New York, NY: Oxford University Press.
Gore, F. M., Bloem, P. J., Patton, G. C., Ferguson, J., Joseph, V., Coffey, C., et al. (2011). Global burden of disease in young people aged 10–24 years: A systematic analysis. Lancet, 377(9783), 2093–2102. doi:10.1016/S0140-6736(11)60512-6.
Gottesman, I. I., & Gould, T. D. (2003). The endophenotype concept in psychiatry: Etymology and strategic intentions. American Journal of Psychiatry, 160(4), 636–645. doi:10.1176/appi.ajp.160.4.636.
Gottman, J. M. (1994). What predicts divorce? The relationship between marital processes and marital outcomes. Hillsdale, NJ: Erlbaum.
Gruber, J., Culver, J. L., Johnson, S. L., Jennifer, N. Y., Keller, K. L., & Ketter, T. A. (2009). Do positive emotions predict symptomatic change in bipolar disorder? Bipolar Disorders, 11, 330–336. doi:10.1111/j.1399-5618.2009.00679.x.
Gruber, J., Dutra, S. J., Hay, A. C., & Devlin, H. C. (2014). Positive emotion disturbance across clinical disorders. In M. Tugade, M. N. Shiota, & L. D. Kirby (Eds.), Handbook of positive emotions. New York, NY: Guilford Press.
Gruber, J., Gilbert, K. E., Youngstrom, E. A., Youngstrom, J. K., Feeny, N. C., & Findling, R. L. (2013). Reward dysregulation and mood symptoms in an adolescent outpatient sample. Journal of Abnormal Child Psychology, 41, 1053–1065. doi:10.1007/s10802-013-9746-8.
Gruber, J., & Johnson, S. L. (2009). Positive emotional traits and ambitious goals among people at risk for mania: The need for specificity. International Journal of Cognitive Therapy, 2(2), 179–190. doi:10.1521/ijct.2009.2.2.176.
Gruber, J., Oveis, C., Keltner, D., & Johnson, S. L. (2011). A discrete emotions approach to positive emotion disturbance in depression. Cognition and Emotion, 25, 40–52. doi:10.1080/02699931003615984.
Guyer, A. E., McClure, E. B., Adler, A. D., Brotman, M. A., Rich, B. A., Kimes, A. S., et al. (2007). Specificity of facial expression labeling deficits in childhood psychopathology. Journal of Child Psychology and Psychiatry, 48, 863–871. doi:10.1111/j.1469-7610.2007.01758.x.
Harmon-Jones, E. (2003). Anger and the behavioral approach system. Personality and Individual Differences, 35, 995–1005. doi:10.1016/S0191-8869(02)00313-6.
Harmon-Jones, E., & Allen, J. B. (1998). Anger and frontal brain activity: EEG asymmetry consistent with approach motivation despite negative affective valence. Journal of Personality and Social Psychology, 74, 1310–1316. doi:10.1037/0022-3514.74.5.1310.
Harmon-Jones, E., & Gable, P. A. (2009). Incorporating motivational intensity and direction into the study of emotions: Implications for brain mechanisms of emotion and cognition-emotion interactions. Netherlands Journal of Psychology, 64, 132–142. doi:10.1007/BF03076416.
Hasler, G., Drevets, W. C., Gould, T. D., Gottesman, I. I., & Manji, H. K. (2006). Toward constructing an endophenotype strategy for bipolar disorders. Biological Psychiatry, 60(2), 93–105. doi:10.1016/j.biopsych.2005.11.006.
Helzer, J. E., Kraemer, H. C., & Krueger, R. F. (2006). The feasibility and need for dimensional psychiatric diagnoses. Psychological Medicine, 36, 1671–1680. doi:10.1017/S003329170600821X.
Henker, B., Whalen, C. K., Jamner, L. D., & Delfino, R. J. (2002). Anxiety, affect, and activity in teenagers: Monitoring daily life with electronic diaries. Journal of American Academy of Child and Adolescent Psychiatry, 41(6), 660–670. doi:10.1097/00004583-200206000-00005.
Hofmann, S. G., Sawyer, A. T., Fang, A., & Asnaani, A. (2012). Emotion dysregulation model of mood and anxiety disorders. Depression and Anxiety, 29, 409–416. doi:10.1002/da.21888.
Hunt, J., Birmaher, B., Leonard, H., Strober, M., Axelson, D., Ryan, N., et al. (2009). Irritability without elation in a large bipolar youth sample: Frequency and clinical description. Journal of the American Academy of Child and Adolescent Psychiatry, 48, 730–739. doi:10.1097/CHI.0b013e3181a565db.
Insel, T., Cuthbert, B. N., Garvey, M., Kozak, M. J., Pine, D., Quinn, K., et al. (2010). Research domain criteria (RDoC): Toward a new classification framework for research of mental disorders. American Journal of Psychiatry, 167, 1–4. doi:10.1176/appi.ajp.2010.09091379.
Izard, C. E. (1977). Human emotions. New York, NY: Plenum.
Izard, C. E., Libero, D. Z., Putnam, P., & Haynes, O. M. (1993). Stability of emotion experiences and their relations to traits of personality. Journal of Personality and Social Psychology, 64(5), 847–860. doi:10.1037/0012-1649.27.3.432.
Jamison, K. R. (2005). Exuberance: The passion for life. New York, NY: Vintage Books.
Johnson, S. L. (2005). Mania and dysregulation in goal pursuit: A review. Clinical Psychology Review, 25(2), 241–262. doi:10.1016/j.cpr.2004.11.002.
Johnson, S. L., & McMurrich, S. (2006). Life events and juvenile bipolar disorder: Conceptual issues and early findings. Development and Psychopathology, 18(04), 1169–1179.
Kaufman, J., Birmaher, B., Brent, D., Rao, U., Flynn, C., Moreci, P., et al. (1997). Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry, 36(7), 980–988. doi:10.1097/00004583-199707000-00021.
Keltner, D., Ekman, P., Gonzaga, G. C., & Beer, J. (2003). Facial expression of emotion. In R. J. Davidson, K. R. Scherer, & H. H. Goldsmith (Eds.), Handbook of affective sciences (pp. 415–432). New York, NY: Oxford University Press.
Kessler, R. C., Chiu, W. T., Demler, O., & Walters, E. E. (2005). Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62, 617–627. doi:10.1001/archpsyc.62.6.617.
Kowatch, R. A., Youngstrom, E. A., Danielyan, A., & Findling, R. L. (2005). Review and meta-analysis of the phenomenology and clinical characteristics of mania in children and adolescents. Bipolar Disorders, 7, 483–496. doi:10.1111/j.1399-5618.2005.00261.x.
Kraepelin, E. (1921). Manic-depressive insanity and paranoia. Edinburgh, UK: Livingstone.
Larson, R., & Lampman-Petraitis, C. (1989). Daily emotional states as reported by children and adolescents. Child Development, 60(5), 1250–1260. doi:10.2307/1130798.
Larson, R., Moneta, G., Richards, M., & Wilson, S. (2002). Continuity, stability, and change in daily emotional experience across adolescence. Child Development, 73(4), 1151–1165.
Leibenluft, E. (2011). Severe mood dysregulation, irritability, and the diagnostic boundaries of bipolar disorder in youths. American Journal of Psychiatry, 168(2), 129–142. doi:10.1176/appi.ajp.2010.10050766.
Lopez, A. D., Mathers, C. D., Ezzati, M., Jamison, D. T., & Murray, C. J. L. (2006). Global and regional burden of disease and risk factors, 2001: Systematic analysis of population health data. The Lancet, 367(9524), 1747–1757. doi:10.1016/s0140-6736(06)68770-9.
Maciejewski, D. F., van Lier, P. A. C., Branje, S. J. T., Meeus, W. H. J., & Koot, H. M. (2015). A 5-year longitudinal study on mood variability across adolescence using daily diaries. Child Development, 86, 1908–1921. doi:10.1111/cdev.12420.
McMakin, D., Siegle, G., & Shirk, S. (2011). Positive affect stimulation and sustainment (PASS) module for depressed mood: A preliminary investigation of treatment-related effects. Cognitive Therapy and Research, 35(3), 217–226. doi:10.1007/s10608-010-9311-5.
Merikangas, K. R., Akiskal, H. S., Angst, J., Greenberg, P. E., Hirschfeld, R. M. A., Petukhova, M., et al. (2007). Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication. Archives of General Psychiatry, 64(5), 543–552. doi:10.1001/archpsyc.64.5.543.
Meyer, B., Johnson, S. L., & Winters, R. (2001). Responsiveness to threat and incentive in bipolar disorder: Relations of the BIS/BAS scales with symptoms. Journal of Psychopathology and Behavioral Assessment, 23, 133–143. doi:10.1023/A:1010929402770.
Miklowitz, D. J., & Chang, K. D. (2008). Prevention of bipolar disorder in at-risk children: Theoretical assumptions and empirical foundations. Development and Psychopathology, 20(3), 881–897. doi:10.1017/S0954579408000424.
Millgram, Y., Joormann, J., Huppert, J. D., & Tamir, M. (2015). Sad as a matter of choice? Emotion-regulation goals in depression. Psychological Science, 26(8), 1216–1228. doi:10.1177/0956797615583295.
Myers, R. (1990). Classical and modern regression with applications (2nd ed.). Boston, MA: Duxbury.
Neumann, A., Lier, P. A. C., Frijns, T., Meeus, W., & Koot, H. M. (2011). Emotional dynamics in the development of early adolescent psychopathology: A one-year longitudinal study. Journal of Abnormal Child Psychology, 39(5), 657–669. doi:10.1007/s10802-011-9509-3.
Panksepp, J. (1998). Affective neuroscience: The foundations of human and animal emotions. New York, NY: Oxford University Press.
Prisciandaro, J. J., & Roberts, J. E. (2011). Evidence for the continuous latent structure of mania in the Epidemiologic Catchment Area from multiple latent structure and construct validation methodologies. Psychological Medicine, 41(3), 575–588. doi:10.1017/S0033291710001078.
Prisciandaro, J. J., & Tolliver, B. K. (2015). Evidence for the continuous latent structure of mania and depression in out-patients with bipolar disorder: Results from the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). Psychologial Medicine, 45(12), 2595–2603. doi:10.1017/S0033291715000513.
Quevedo, K. M., Benning, S. D., Gunnar, M. R., & Dahl, R. E. (2009). The onset of puberty: Effects on the psychophysiology of defensive and appetitive motivation. Development and Psychopathology, 21(01), 27. doi:10.1017/s0954579409000030.
Rich, B. A., Grimley, M. E., Schmajuk, M., Blair, K. S., Blair, R. J. R., & Leibenluft, E. (2008). Face emotion labeling deficits in children with bipolar disorder and severe mood dysregulation. Development and Psychopathology. doi:10.1017/s0954579408000266.
Rolls, E. T. (1999). The brain and emotion. New York, NY: Oxford University Press.
Rottenberg, J., Kasch, K. L., Gross, J. J., & Gotlib, I. H. (2002). Sadness and amusement reactivity differentially predict concurrent and prospective functioning in major depressive disorder. Emotion, 2(2), 135–146. doi:10.1037//1528-3542.2.2.135.
Sanislow, C. A., Pine, D. S., Quinn, K. J., Kozak, M. J., Garvey, M. A., Heinssen, R. K., et al. (2010). Developing constructs for psychopathology research: Research domain criteria. Journal of Abnormal Psychology, 119, 631–639. doi:10.1037/a0020909.
Shiota, M. N., Keltner, D., & John, O. P. (2006). Positive emotion dispositions differentially associated with Big Five personality and attachment style. The Journal of Positive Psychology, 1(2), 61–71. doi:10.1080/17439760500510833.
Siegel, R. S., Freeman, A. J., La Greca, A. M., & Youngstrom, E. A. (2015). Peer relationship difficulties in adolescents with bipolar disorder. Child & Youth Care Forum, 44(3), 355–375. doi:10.1007/s10566-014-9291-9.
Silk, J. S., Siegle, G. J., Whalen, D. J., Ostapenko, L. J., Ladouceur, C. D., & Dahl, R. E. (2009). Pubertal changes in emotional information processing: Pupillary, behavioral, and subjective evidence during emotional word identification. Development and Psychopathology, 21(01), 7–26. doi:10.1017/s0954579409000029.
Somerville, L. H., Jones, R. M., & Casey, B. J. (2010). A time of change: Behavioral and neural correlates of adolescent sensitivity to appetitive and aversive environmental cues. Brain and Cognition, 72(1), 124–133. doi:10.1016/j.bandc.2009.07.003.
Spitzer, R. L. (1983). Psychiatric diagnosis: Are clinicians still necessary? Comprehensive Psychiatry, 24(5), 399–411.
Stanton, K., Gruber, J., & Watson, D. (in press). Basic dimensions defining mania risk: A structural approach. Psychological Assessment.
Tracy, J. L., & Robins, R. W. (2004). Putting the self into self-conscious emotions: A theoretical model. Psychological Inquiry, 15, 103–125. doi:10.1207/s15327965pli1502.
Urosevic, S., Abramson, L., Harmon-Jones, E., & Alloy, L. (2008). Dysregulation of the behavioral approach system (BAS) in bipolar spectrum disorders: Review of theory and evidence. Clinical Psychology Review, 28(7), 1188–1205. doi:10.1016/j.cpr.2008.04.004.
Uusitalo-Malmivaara, L. (2014). Happiness decreases during early adolescence—A study on 12- and 15-year-old finnish students. Psychology, 05, 541–555. doi:10.4236/psych.2014.56064.
Van Meter, A. R., Burke, C., Kowatch, R. A., Findling, R. L., & Youngstrom, E. A. (2016). Ten-year updated meta-analysis of the clinical characteristics of pediatric mania and hypomania. Bipolar Disorders. doi:10.1111/bdi.12358.
Van Meter, A., Moreira, A. L., & Youngstrom, E. A. (2011). Meta-analysis of epidemiological studies of pediatric bipolar disorder. Journal of Clinical Psychiatry, 72, 1250–1256. doi:10.4088/JCP.10m06290.
Watson, D., & Naragon-Gainey, K. (2010). On the specificity of positive emotional dysfunction in psychopathology: Evidence from the mood and anxiety disorders and schizophrenia/schizotypy. Clinical Psychology Review, 30, 839–848.
Youngstrom, E. A., Birmaher, B., & Findling, R. L. (2008a). Pediatric bipolar disorder: Validity, phenomenology, and recommendations for diagnosis. Bipolar Disorders, 10, 194–214. doi:10.1111/j.1399-5618.2007.00563.x.
Youngstrom, E. A., Findling, R. L., Danielson, C. K., & Calabrese, J. R. (2001). Discriminative validity of parent report of hypomanic and depressive symptoms on the General Behavior Inventory. Psychological Assessment, 13(2), 267–276. doi:10.1037//1040-3590,13.2.267.
Youngstrom, E. A., Findling, R. L., Kogos Youngstrom, J., & Calabrese, J. R. (2005a). Toward an evidence-based assessment of pediatric bipolar disorder. Journal of Clinical Child and Adolescent Psychology, 34(3), 433–448. doi:10.1207/s15374424jccp3403_4.
Youngstrom, E. A., Frazier, T. W., Demeter, C., Calabrese, J. R., & Findling, R. L. (2008b). Developing a ten item mania scale from the parent general behavior inventory for children and adolescents. Journal of Clinical Psychiatry, 69(5), 831–839.
Youngstrom, E. A., Genzlinger, J. E., Egerton, G. A., & Van Meter, A. R. (2015). Multivariate meta-analysis of the discriminative validity of caregiver, youth, and teacher rating scales for pediatric bipolar disorder: Mother knows best about mania. Archives of Scientific Psychology, 3, 112–137. doi:10.1037/arc0000024.
Youngstrom, E. A., & Izard, C. E. (2008). Functions of emotions and emotion-related dysfunction. In A. J. Elliot (Ed.), Handbook of approach and avoidance motivation (pp. 367–384). New York: Psychology Press.
Youngstrom, E., Meyers, O., Demeter, C., Youngstrom, J., Morello, L., Piiparinen, R., et al. (2005b). Comparing diagnostic checklists for pediatric bipolar disorder in academic and community mental health settings. Bipolar Disorders, 7, 507–517. doi:10.1111/j.1399-5618.2005.00269.x.
Acknowledgments
This work was supported in part by NIH R01 MH066647 to Eric Youngstrom. Dr. Youngstrom has consulted with Pearson, Otsuka, Janssen, Lundbeck, Joe Startup Technologies, and Western Psychological Services about psychological assessment. Dr. Findling receives or has received research support, acted as a consultant, received royalties from, and/or served on a speaker’s bureau for Abbott, Addrenex, Alexza, American Psychiatric Press, AstraZeneca, Biovail, Bristol-Myers Squibb, Dainippon Sumitomo Pharma, Forest, GlaxoSmithKline, Guilford Press, Johns Hopkins University Press, Johnson and Johnson, KemPharm Lilly, Lundbeck, Merck, National Institutes of Health, Neuropharm, Novartis, Noven, Organon, Otsuka, Pfizer, Physicians’ Post-Graduate Press, Rhodes Pharmaceuticals, Roche, Sage, Sanofi-Aventis, Schering-Plough, Seaside Therapeutics, Sepracore, Shionogi, Shire, Solvay, Stanley Medical Research Institute, Sunovion, Supernus Pharmaceuticals, Transcept Pharmaceuticals, Validus, WebMD and Wyeth.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
June Gruber, Anna Van Meter, Kirsten Gilbert, Jennifer Kogos Youngstrom, and Norah Feeny declare that they have no conflict of interest.
Informed Consent
Informed consent procedures were followed in accordance with the ethical standards of the responsible committees on human experimentation at the University Hospitals of Cleveland and Applewood Centers. Informed consent was obtained from all individual subjects participating in the study.
Animal Rights
No animal studies were carried out by the authors for this article.
Rights and permissions
About this article
Cite this article
Gruber, J., Van Meter, A., Gilbert, K.E. et al. Positive Emotion Specificity and Mood Symptoms in an Adolescent Outpatient Sample. Cogn Ther Res 41, 393–405 (2017). https://doi.org/10.1007/s10608-016-9796-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10608-016-9796-7