Abstract
Investigating differences in the ways that people react to mood-evoking stimuli and regulate subsequent emotions may help to elucidate important mechanisms underlying depressed or hypomanic mood states. Euthymic young adults with bipolar disorder (n = 23) or depression (n = 21) were recruited for a study of emotion and mood. Two mood inductions assessed for differences in mood reactivity. Participants completed measures of current symptoms and emotion regulation strategies. Maladaptive (B = 0.42, p = .021) and adaptive (B = −0.26, p = .011) emotion regulation strategies were significantly associated with depressive symptoms. Bipolar diagnosis (B = 5.51, p = .035), and threat mood reactivity (B = −0.26, p = .015) were associated with hypomanic symptoms. Interaction terms for mood reactivity and emotion regulation were not significant in either model, although net regression indicated significant differences in two trends. Depressed moods, associated with MDD or BD, may be initiated and maintained primarily due to poor choice of emotion regulation strategies. Elevated mood states are more specific to bipolar disorder, and may be triggered by mood reactivity, rather than regulation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The current version of the Diagnostic and Statistical Manual (DSM-5) split the mood disorders into two separate chapters, reflecting the possibility that they have different underlying mechanisms (American Psychiatric Association 2013). Extreme emotional lability is a prominent feature of bipolar disorder (BD; Green et al. 2007; Townsend 2012) that tends to cause chronic impairment, not just during mood episodes (Krüger et al. 2003). The emotion-related deficits in BD encompass multiple processes, from detecting and interpreting emotion, to generating and regulating a response (Phillips et al. 2003a). Consequently, deficits in the emotion processing and regulatory systems perturb individuals’ ability to make and maintain relationships, to advance professionally, and to achieve a high quality of life. Major depressive disorder, on the other hand, is not usually associated with the extreme emotional lability and dysregulation seen in BD. However, research does suggest that emotion processing deficits influence the onset and maintenance of depressive episodes (Fales et al. 2008; Leppanen 2006).
The Research Domain Criteria (RDoC) initiative (Insel et al. 2010) aims to build a better understanding of psychopathology by identifying domains of functioning, deficits in which underlie mental illness. RDoC is beginning to shift research from a diagnostically-bound to a transdiagnostic endeavor. This approach may help to identify processes implicated in multiple disorders, like emotion perception and regulation of emotion response, and build a systems-focused, rather than symptom-focused, approach to conceptualizing mental illness. In addition to elucidating mechanisms underlying various psychological problems, the RDoC initiative also aims to identify mutable intervention treatment targets. Consistent with the RDoC perspective, the goal of the present study is to study the processes of emotion response and regulation transdiagnostically, in order to determine which deficits of emotion processing observed in people with BD are specific to [hypo]manic mood states and which are shared with depressed mood or mood pathology more broadly.
Emotion Response
Face Emotion Processing
Studies of emotion in bipolar disorder have tended to focus on face emotion processing or emotion regulation. Other people’s faces are one of our most salient emotional cues, and people with BD tend to perceive others’ emotions incorrectly (Getz et al. 2003; Hoertnagl et al. 2011; Rocca et al. 2009; Schenkel et al. 2007; Vederman et al. 2012). Specifically, people with BD tend to see others’ faces as more negatively valenced than they are, and to perceive negative emotion when no emotion is shown (i.e., neutral expression) (Murphy et al. 1999; Phillips et al. 2003b). People with unipolar depression show similar deficits in face emotion perception (i.e., negative bias; Kohler et al. 2011), and an attentional bias toward negative expressions (Joormann and Gotlib 2007; Ridout et al. 2003). In fact, both people with MDD and with BD tend to exhibit mood a congruent attentional bias (Donaldson et al. 2007; Erickson et al. 2005; Murphy et al. 1999), which can serve to perpetuate unhealthy mood states.
Neuroimaging research in people with mood disorders finds that differences in face emotion processing observed correspond with elevated amygdalar activation (Blumberg et al. 2005; Chang et al. 2005; Eippert et al. 2007; Hariri et al. 2002; Leppanen 2006). This overactivation is often paired with decreased activity of the medial and lateral prefrontal cortex—areas implicated in the successful regulation of emotion responses (Ochsner et al. 2002; Phillips et al. 2008). The data suggest an exaggerated emotional response coupled with an inadequate regulatory response, which can lead to mood episodes (Yap et al. 2007).
Mood Induction
Though the majority of research on emotion processing has used face emotions as the primary stimuli, other methods of eliciting emotional responses also provide important information about the mechanisms related to emotion response and regulation. For example, studies investigating how positive mood reactivity relates to mania have demonstrated that positive mood induction tends to be more effective in people with bipolar disorder than in controls; the mood induced is rated more strongly, and lasts longer (Gruber 2011; Gruber et al. 2008; Johnson et al. 2007; Roiser et al. 2009). Additionally, positive mood induction in euthymic people with bipolar disorder tends to increase impulsivity and poor judgment (Roiser et al. 2009). These results, considered in the context of evidence from neuroimaging studies, suggest that the combination of highly active limbic system with limited regulatory capability may explain the greater intensity and duration of emotional responses in persons with a history of MDD or BD (Green et al. 2007; Morris et al. 2009; Phillips et al. 2003b).
Among people with a history of depression, a mild induced sad mood is associated with cognitive patterns (e.g., negative thoughts, dysfunctional beliefs) typical of people during an episode of depression (Gemar et al. 2001). Importantly, these mild depressed moods result in a thinking style that predicts future depressive episodes. Greater sensitivity to [negative] emotional stimuli adds to more frequent negative moods and is a risk factor for subsequent mood episodes (Segal et al. 1999). Although people with current or past depression do not report experiencing more intense emotions related to mood induction (LeMoult et al. 2009), the emotional and cognitive impact of the mood change is exaggerated. The little literature on negative mood induction in people with BD suggests that people with BD respond in a similar fashion to those with MDD (Wright et al. 2005). Because people with BD tend to spend three times as many days depressed than manic (Kupka et al. 2007), more research into negative mood reactivity among people with BD is warranted. Together, the results of studies using mood induction paradigms suggest that whether or not a person is currently in a mood episode, those with BD or MDD tend to have stronger reaction to emotional stimuli, which can result in consequences, including new mood episodes.
Behavioral Inhibition and Behavioral Approach
The strong emotional responses associated with mood disorders may be related to sensitivities of the behavioral inhibition (BIS) and behavioral approach (BAS) systems. Both systems are often dysregulated in people with mood disorders. Specifically, a sensitive BAS may lead to impulsivity and approach behaviors, whereas a sensitive BIS may lead to inappropriate reactions in the face of threat or stress (Alloy et al. 2008; Johnson et al. 2003; Meyer et al. 2001). Depression has been conceptualized as overly sensitive BIS, coupled with less sensitive BAS, which results in high levels of inhibition and low reward responsiveness (Kasch et al. 2002; Youngstrom and Izard 2008). Mania, on the other hand, may result from overactive BAS and low BIS sensitivity, leading to excessive pursuit of reward without a natural “braking” system to inhibit impulsive behaviors (Barkley 1997; Johnson et al. 2003; Wright et al. 2005; Youngstrom and Izard 2008)
Emotion Regulation
Regulatory Strategies
In addition to greater sensitivity to emotional stimuli, people with mood disorders tend to struggle more than the average person to successfully regulate their emotions. So, in addition to being more prone to negative emotion (in particular) and to experience these emotions more intensely, people with mood disorders are less well-equipped to manage their emotions. Specifically, people with mood disorders (MDD or BD) consistently show mastery of fewer emotion regulation strategies, and a tendency to have poorly regulated emotions (Aldao et al. 2010; Angst et al. 2003; Dickstein et al. 2009; Green et al. 2007; Gruber et al. 2011a, 2012, 2013). Dysfunctional emotion regulation is thought to develop as a result of many of the same factors that contribute to mood disorder, including both heritable, internal traits and external risk factors (Angst et al. 2003; Calkins 1994; Phillips et al. 2008; Silk et al. 2006).
People with BD tend to employ more emotion regulation strategies and report exerting more effort to regulate emotions than healthy controls, but are less successful at managing their reactions (Gruber et al. 2012), suggesting that people with BD may select inappropriate emotion regulation strategies and be less skilled at implemented the strategies that they employ (Gruber et al. 2012). Related, other studies have indicated that people with mood disorders tend to select maladaptive emotion regulation strategies, including self-blame, rumination, catastrophizing and other-blame (Garnefski and Kraaij 2006; Green et al. 2011) that may perpetuate an unhealthy mood, rather than ameliorating it. Additionally, they may be less likely to select emotion regulation strategies, such as positive reappraisal or positive refocusing, that are negatively correlated with depressive symptoms (Garnefski and Kraaij 2006). Maladaptive emotion regulation strategies may also be associated with elevated mood (Gruber et al. 2011a): in a study of people with BD I, rumination was associated with higher scores on measures of both depressive and hypomanic symptoms (Green et al. 2011).
Data from fMRI studies also indicate that people with MDD or BD exhibit abnormal brain activity during emotional states; specifically, functional and structural abnormalities of the amygdala and reduced activation of areas in the prefrontal cortex related to regulation of emotional response (Altshuler et al. 1998; Davidson et al. 2002; Phillips et al. 2008; Strakowski et al. 2005; Townsend 2012). This is similar to the pattern of activity (described above) observed during face emotion processing tasks; importantly, in MDD this effect is stronger among people with more severe symptomatology (Davidson et al. 2002). Among people taking antidepressant medication, an initial regulatory response is observed; but its duration is short, suggesting that the emotion can be regulated, but only for a short time (Erk et al. 2010). Interestingly, studies using self-report or psychophysiological methods to measure emotion reactivity in people with depression tend to indicate less reactivity (relative to healthy controls) (Bylsma et al. 2008), in contrast to neuroimaging studies This suggests that there may be a disconnect between an individual’s neural and behavioral responses to emotion.
A biological predisposition to interpreting neutral stimuli as emotionally-charged and to reacting strongly to observed emotional stimuli is a strong foundation for a mood disorder. Emotion regulation should moderate an instinctual overreaction to an emotional stimulus, but if one has poor emotion regulation skills or tends to choose maladaptive regulation tactics, the reaction could result in extreme mood states. It is not hard to see how the characteristics described above—mood congruent interpretations of emotion, a tendency to seek out emotional content, strong emotional reactions, and an inability to temper emotion—could create a cascade to initiate disordered mood.
Present Study
The objective of the present study was to explore how people with BD or MDD respond to emotional stimuli and to determine whether their preferred method of emotion regulation moderates the relation between their emotional reactivity and self-reported mood symptoms. The RDoC initiative emphasizes the importance of better understanding the mechanisms underlying psychopathology. In the present study, we aim to examine differences in both negative (threat) and positive (reward responsiveness) valence systems in people with mood disorders. Investigating individual differences in reactions to mood-evoking stimuli and subsequent emotion regulation may help to chart important mechanisms underlying depressed or hypomanic mood states. We hypothesized that people with BD would react more strongly to the positive (triumph) mood induction than people with MDD, due to greater reward sensitivity, and that, in both groups, stronger responses to the mood inductions would be associated with more mood symptomatology of the same pole (i.e., a strong response to the threat mood induction would be associated with more depressive symptomatology). We also expected that, in both samples, the use of maladaptive emotion regulation strategies would be associated with higher scores on symptom measures. Related, we anticipated that adaptive emotion regulation strategies would be associated with lower scores on the symptom measures. Finally, we expected emotion regulation strategies to moderate the relations between mood induction response and symptom measure scores, such that maladaptive emotion regulation would exacerbate the relation between mood induction response and symptoms and adaptive emotion regulation would minimize the relation between mood response and symptoms.
Method
Participants
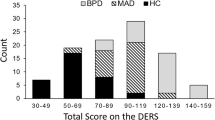
Young adults were recruited through the university psychiatry department for a study of emotion sensitivity and mood (N = 44; average age 28; 61 % female; 86 % Caucasian, 11 % Black, 2 % Other; 5 % Latino). Clinical diagnoses were confirmed using the Mini International Neuropsychiatric Interview (M.I.N.I.; Sheehan et al. 1997).
Twenty-one participants met criteria for major depression, 11 met criteria for bipolar I, five met criteria for bipolar II, and seven met criteria for bipolar NOS. At the time of the study appointment, three of the participants in the bipolar group reported experiencing depressed mood, and none of the participants from the depressed group had depressed mood (as assessed by M.I.N.I.). None of participants reported current hypomanic symptoms (as assessed by M.I.N.I.). No one met full criteria for a current mood episode.
The bipolar and depressed groups were equivalent in gender (X 2(1) = 3.73, p = .06), and racial composition (X 2(1) = 2.72, p = .26). The depressed group was older than the bipolar group (t(42) = 2.76, p = .009). The number of people in each group who reported taking psychotropic medication was equivalent (X 2(1) = 0.22, p = .64), similarly, there was no statistical difference in the number of people who reported being currently in psychotherapy (X 2(1) = 0.19, p = .67). BDI scores were also equivalent in the two groups (t(42) = −0.33, p = .74), HCL-32 scores were significantly higher in the bipolar group, t(42) = −2.48, p = .02 (See Table 1).
Measures
The Mini International Neuropsychiatric Interview (M.I.N.I.)
The M.I.N.I. is a structured diagnostic interview that assesses for multiple psychiatric disorders, including depression and mania, according to DSM-IV criteria. The M.I.N.I. assesses both current and past episodes of psychopathology and has good validity compared with other, more lengthy diagnostic interviews (Lecrubier et al. 1997; Sheehan et al. 1997). Additionally, the M.I.N.I. can be accurately administered by lay interviewers (Black et al. 2004). In the present study, the M.I.N.I. was administered by undergraduate and BA-level research assistants, all of whom were trained to administer the interview through roleplay. The first author also observed interviews conducted by each research assistant until s/he was reliable on diagnoses of depression and bipolar disorder.
Beck Depression Inventory (BDI-I)
The BDI-I (Beck et al. 1961; Beck 1978) has a long history of use to assess symptoms of depression both in research studies and clinical practice (Beck et al. 1988). The BDI-I has good internal consistency; one meta-analysis reported an average alpha for psychiatric populations of 0.86 (Beck et al. 1988). In the present sample, the reliability was similarly good, Cronbach’s α = 0.89.
Hypomanic Checklist (HCL-32)
The HCL-32 is a self-report designed to identify symptoms of hypomania. It has a yes/no answer format and has been validated in diverse, international samples (Angst et al. 2005). In one study of three different patient populations, it had good reliability, Cronbach’s α of 0.82. In our samples, the reliability was comparable, Cronbach’s α = 0.88.
Cognitive Emotion Regulation Questionnaire (CERQ)
The CERQ is a reliable and valid method by which to measure individual differences in emotion regulation strategies (Jermann et al. 2006). The CERQ includes nine scales—self-blame, other-blame, acceptance, refocus on planning, positive refocusing, rumination, positive reappraisal, putting into perspective, and catastrophizing. The scales with higher scores indicate which cognitive strategies the participant uses most. For the purposes of this study, scores on the maladaptive scales (Garnefski and Kraaij 2006) (acceptance, self-blame, rumination, catastrophizing, and other-blame) were summed to create an index score, similarly, the adaptive strategy subscales (refocus on planning, positive refocusing, putting into perspective, and positive appraisal) were summed. Analyses used the two resulting index scores—maladaptive emotion regulation strategy, adaptive emotion regulation strategy. The Cronbach’s alpha of these two scales in our sample was .75 and .95 respectively.
Mood Rating Scale
The visual analog mood scale balances ease of use with sensitivity to individual differences and the impact of a mood induction (Roiser et al. 2009; Standage et al. 2010). In the present study, each participant rated their current mood, (e.g., “How threatened do you feel right now?” “How triumphant do you feel right now?”) using a visual measure (a bar that can be completely or not at all filled in) to indicate how much they felt the specified emotion from “not at all” to “very” (Huntsinger et al. 2010). Mood was assessed both before and after each mood induction. Ratings were based on the length (left to right) of the portion of the bar that is filled in, quantified automatically by the Qualtrics software. Subtracting the pre-induction mood score from the post-induction mood score measure mood change following the induction.
Procedure
All procedures were approved by the IRB. Potential participants who were expected to meet inclusion criteria based on age and clinical diagnosis were identified through a research database of patients who were treated in the University Psychiatry Department and were then contacted via mail. Research assistants followed up with letter recipients to explain the study and inquire about interest. Those who expressed interest were scheduled for an in-lab study session.
Participants all had a diagnosis of depression or bipolar disorder, but they were not necessarily receiving ongoing care, which may account for the low rates of pharmacologic treatment in this sample, though treatment compliance is often poor among people with bipolar disorder (Lingam and Scott 2002; Sajatovic et al. 2006). Additionally, participants were all outpatients and well enough to participate in a research study.
Following informed consent, each participant was interviewed by a trained research assistant, using the M.I.N.I., to determine whether s/he met lifetime criteria for either major depression or bipolar disorder. Participants who did not meet DSM-IV-TR criteria for major depression or bipolar disorder were excluded (n = 5).
Next, participants completed a series of online questionnaires, including the HCL-32, BDI, and CERQ. Finally, participants participated in two mood induction paradigms. In order to account for the potential that the first mood induction would affect the second, the order of the mood inductions was counterbalanced across participants, and each participant completed a series of demographic questionnaires in between the two inductions as a distracter.
The induction of a particular mood in participants has been the basis for many experiments, and there are many processes that have been used to do so. A meta-analysis evaluated the effectiveness of different mood induction techniques and to compare their effect sizes (Westermann et al. 1996), and found that the most effective mood induction was achieved with the use of a movie clip, combined with the instruction for participants to really notice the intended mood. The average effect size for studies using this method was >.73 for both positive and negative moods (Westermann et al. 1996). In keeping with the results of the meta-analysis, a film-based mood induction was used in the study. Participants each watched two film clips (8 min each); one was taken from the movie Hoosiers, in which an underdog basketball team rallies to win a championship game, and was intended to induce a triumphant (positive) response. The other clip taken from the movie Strangers in which a young woman is threatened by an intruder, and was intended to induce a threat/fear (negative) response. A threat response, rather than sad response, was targeted based on literature suggesting that threat is more likely than sadness to produce a robust response from the amygdala, indicating a strong emotional reaction (Hariri et al. 2002; Killgore and Yurgelun-Todd 2004; Phan et al. 2002). Additionally, because people with mood disorders are likely to have a sensitive behavioral inhibition system, threat may be more likely to elicit a response (Alloy et al. 2008; Kasch et al. 2002; Meyer et al. 1999). The clips were selected by the first author and rated by an independent panel as the most effective for inducing the moods of interest out of a sample of clips.
The clips were presented using online media, the order was randomized in order to reduce the potential for bias. Just prior to the first mood induction, participants rated their mood on a number of dimensions, including Threat (“How threatened do you feel right now?”) and Triumph (“How triumphant do you feel right now?”).
A visual analog mood scale measured mood induction response. The mood rating (length of VAMS bar) pre-induction was subtracted from the post-induction length to determine change for each induction. This mood rating was repeated after each clip.
Analytic Plan
Chi squared and t tests assessed for clinical and demographic differences between the depressed and the bipolar group. Correlations quantified relations between the independent and dependent variables. Linear regression tested the hypothesis that the relation between mood induction response and emotion regulation might help to explain variance in depression and manic symptoms found in mood disorders. In the first regression, BDI scores were regressed on (step one) diagnosis (bipolar Y/N) and age, (step two) triumph and threat mood induction changes, (step three) adaptive and maladaptive emotion regulation strategies, (step four) interaction terms for mean-centered mood reactivity and emotion regulation strategies (triumph-adaptive, triumph-maladaptive, threat-adaptive, threat-maladaptive). The second regression used the same independent variables to determine how they related to HCL-32 scores. Finally, net regression tested whether the independent variables (mood induction response, emotion regulation strategies, interaction terms) have the same influence on both BDI score and HCL-32 score (Cohen and Cohen 1983; Cohen et al. 2003).
Results
Baseline mood scores, assessed prior to the mood induction, were the same across the two groups (triumph [t(42) = −0.93, p = .36], threat [t(42) = 0.05 p = .96)]. There were no differences between the group of people with bipolar disorder and those with depression in response to the mood inductions [triumph (t(42) = −0.29, p = .77) or threat (t(42) = −0.28 p = .77)].
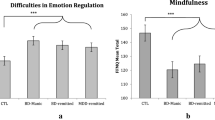
There were no significant differences in scores on the subscales of the CERQ across the two groups (ps = .07–.93). Similarly, there were no differences on the collapsed adaptive (p = .97) and maladaptive (p = .13) emotion regulation categories, indicating that people from the two groups report using emotion regulation strategies with equal frequency.
Correlational analyses tested the zero order relations between diagnosis, mood symptoms, mood induction response, and emotion regulation strategies. Bipolar diagnosis was correlated with HCL-32 scores (r = .36, p = .017). Depression diagnosis was also correlated with HCL-32 scores (r = −.36, p = .016). BDI scores were correlated with maladaptive (r = .45, p = .002) and adaptive emotion regulation strategies (r = −.59, p < .001). Threat and triumphant mood induction responses were related to each other (r = .74, p < .001). No other associations were significant.
The full regression model for BDI scores explained 53 % of the variance in depressive symptoms. In the first step, none of the clinical/demographic variables were significant. In the second step, the two mood reactivity variables were not significant either. In the third step, both maladaptive (B = 0.30, p = .048) and adaptive emotion regulation strategies (B = −0.29, p = .003) were significant predictors. In the final step, when the interaction terms for mood reactivity and emotion regulation were added, maladaptive emotion regulation strategies (B = 0.42, p = .021) and adaptive (B = −0.26, p = .011) remained the only significant independent variables (Table 2).
A similar model explained 56 % of the variance in HCL-32 scores. In step one, bipolar diagnosis was significant (B = 5.68, p = .03). In step two, BD diagnosis was still significant, as was triumphant mood induction response (B = 0.17, p = .014). After the addition of emotion regulations strategies in step three, BD diagnosis and triumph mood induction response were still significant, as was threat mood induction response (B = −0.20, p = .013) and maladaptive emotion regulation (B = 0.30, p = .037). In the final model, BD diagnosis (B = 5.51, p = .035), and threat mood induction response (B = −0.26, p = .015) were the only significant independent variables; triumph mood induction response trended toward significance with coefficients that were similar in magnitude to the earlier blocks (B = 0.19, p = .069) (Table 2).
Net regression measures whether a set of independent variables has the same impact on two different dependent variables in the same sample (Cohen et al. 2003). This method is advantageous because it can test directly whether the independent variables are equally associated with the symptoms of mania and the symptoms of depression. The results of a net regression indicate whether a single IV or set of IVs has the same relation with both dependent variables, or if the relations are different. The coefficients are interpreted to understand the direction of the relation (i.e., which dependent variable the IV is more strongly associated with), not as the actual effect of the IV on the DV (as a coefficient in the ordinary least squares regression would be interpreted). This method is particularly relevant to our goal of determining whether emotion regulation and mood induction response are associated equally with depression and hypomania. Using this method, we investigated whether the effects of emotion regulation, mood induction response and the interaction of the two had the same influence on both depression and hypomania. The results (Table 2, last column) indicated that a bipolar diagnosis is more strongly related to HCL-32 scores than BDI scores (p = .02), as is the interaction of threat mood induction response and maladaptive emotion regulation (p = .013). Threat mood induction response (p = .026) and the interaction of triumph mood induction response and maladaptive emotion regulation (p = .023) were more strongly related to BDI scores than HCL-32 scores. In both cases, the raw regression coefficients suggest a possible change in sign, though the effects were too small to be significant separately. The fully augmented net regression model suggests that the association between the independent variables and BDI scores is significantly different than the association with HCL-32 scores (F(10,23) = 4.10, p = .002).
Discussion
The goal of this study was to investigate how emotional reactivity and emotion regulation, both implicated in mood disorders, relate to symptoms of depression and hypomania in people with mood disorders. Previous studies have shown that people with mood disorders tend to demonstrate deficits at every stage of the emotion process, from the identification of an emotional stimulus, to the intensity of the resulting response and its regulation (Green et al. 2007; Leppanen 2006). We hypothesized that people with mood disorders are likely to interpret environmental stimuli as emotional more frequently because of their attentional bias toward mood congruent stimuli (MacLeod et al. 2002), resulting in a greater number of emotional responses throughout the day that are poorly regulated due to both skill deficiencies and fatigue (Erk et al. 2010; Garnefski and Kraaij 2006; Gruber et al. 2011b, 2012). Combined, these factors result in a “perfect storm” to ignite and perpetuate pathological mood states.
The results of our study partially support our hypotheses. Interestingly, it seems that depression may be related more to the failure to appropriately regulate emotion, and mania may be more related to the initial reaction to an emotional stimulus. We found that relying on maladaptive emotion regulation strategies was the main correlate of depressive symptoms, even after controlling for diagnosis and mood induction response. Additionally, we hypothesized that strong mood induction reactivity would be associated with more intense mood symptomatology; only three of the people in our study reported current depressed mood, had we recruited a sample with a greater range of current symptomatology, a different pattern of association may have emerged.
The use of adaptive emotion regulation strategies was negatively correlated with depressed mood. These results are consistent with the cognitive model of depression (Beck 1974), which suggests that when people develop negative cognitive schemas and seek out information to confirm their dysfunctional worldview, they are at increased risk for depression. The use of adaptive emotion regulation strategies, may combat negative thinking, whereas maladaptive emotion regulation strategies—acceptance, self-blame, rumination, catastrophizing, other blame—are all consistent with the type of negative thought patterns associated with depression. These include having negative perceptions about oneself, as exemplified by the CERQ prompt, “I feel that I am the one who is responsible for what has happened,” and about one’s situation, “I continually think how horrible the situation has been,” and “I cannot change anything about [the situation].” Another idea often associated with the cognitive model is that of the “downward spiral,” or the tendency for one negative thought to set off a cascade of negative thinking that is difficult to escape and can lead to preservative thoughts, e.g., “I dwell upon the feelings the situation has evoked in me.”
Cognitive therapy, which has shown good effectiveness for combatting depressed mood (Beck 2005), works by targeting these negative thought patterns with a more optimistic–and realistic—perspective. Adaptive cognitive regulation strategies may serve much the same purpose; cognitive reappraisal is often held up as an exemplary emotion regulation strategy (Gruber et al. 2014; Ochsner et al. 2002). On the CERQ, reappraisal is described as, “I look for the positive sides to the matter.” Failure to use reappraisal and other emotion regulation strategies that empower an individual during difficult situations may be an additional risk factor for depression, independent of the use of negative emotion regulations strategies. Interestingly, in a study of people with MDD, those who were treated with cognitive behavioral therapy, versus pharmacotherapy, exhibited normal mood reactivity following a negative mood induction, whereas those treated with pharmacotherapy responded in a way consistent with MDD samples, putting them at risk for a new mood episode (Segal et al. 1999). Some small trials of cognitive therapy for BD have shown promising results, particularly for ameliorating some of the depressive symptoms associated with BD (Ball et al. 2006; Lam et al. 2000, 2003; Scott 2001). Mindfulness-based cognitive therapy, which incorporates the mindfulness practice of being aware of distressing thoughts without engaging with—and potentially exacerbating—them, also shows promise as an intervention to help reduce negative cognitive reactivity (Raes et al. 2009) and to improve emotion regulation (Deckersbach et al. 2012) among people with mood disorders (Lahera et al. 2014; Piet and Hougaard 2011).
Although bipolar depression has unique characteristics that can differentiate it from unipolar depression (Baldessarini et al. 2010; Bowden 2001; Mitchell and Malhi 2004), and bipolar disorder is thought to be more heritable than MDD (Edvardsen et al. 2008; Sullivan et al. 2000), suggesting a larger biological component, the factors that lead to recurrent mood episodes may be shared. From an RDoC perspective, this would support the inclusion of people with depressed mood, regardless of DSM diagnosis, in future studies related to the emotional mechanisms of depression. In this study, we sought to test differences in our sample on the RDoC domains of negative valence (threat) and positive valence (triumph). Interestingly, the main finding was that threat mood induction response—rather than triumph mood response—was related to hypomania scores. We did not hypothesize differences related to negative valence, but this finding is consistent with the literature on inhibition as it relates to mania. Taking a dimensional approach allows for the application of knowledge more broadly, and hopefully, facilitate progress toward better treatments for depressed mood. For example, though psychosocial treatments have demonstrated effectiveness at reducing depressive symptoms and maintaining euthymic mood in people with BD (Colom et al. 1998; Miklowitz 2006), these therapies often focus on other aspects of the disorder (e.g., importance of schedule regularity, medication adherence, sleep hygiene). Bipolar depression is the more common, and impairing, mood state associated with BD (Michalak et al. 2008; Post 2005); applying our knowledge from the cognitive model to bipolar depression may help to reduce the duration and intensity of these episodes.
The fact that mood induction response was not associated with BDI scores is consistent with previous studies; other researchers have found that depression is not associated with a stronger self-reported response to mood induction (Bylsma et al. 2008; LeMoult et al. 2009). However, people with—or at risk for—depression do have a different cognitive and neurological response to a negative mood induction (Gemar et al. 2001; Segal et al. 1999; Siegle et al. 2002). The sustained response to negative emotional stimuli—indicated by prolonged amygdala activation and negative thought patterns—is likely to increase the likelihood of a new or exacerbated episode of depression, even if individuals are unaware of their response to emotional stimuli.
The results of the HCL-32 model suggest that, as expected, mood reactivity is related to manic symptoms. It is interesting that threat mood induction response was negatively associated with HCL-32 scores. We chose to focus on threat as the induced negative mood, due in part, to its association with BIS sensitivity, and these results are consistent with the perspective that BD is primarily a disorder of dysregulated positive emotionality (Gruber et al. 2008; Johnson et al. 2007), wherein people who have low inhibition (as measured by threat induction response), may be more likely to develop manic symptoms because they lack a natural “breaking system.” It was unexpected that the relation between threat mood induction response and hypomanic symptoms was stronger than the relation between triumph mood induction response and hypomanic symptoms. It may be that the positive mood induction used in this study was not a good representation of participants’ positive emotional reactivity in general, and that another, more relevant induction—perhaps something linked more closely to reward responsiveness—would be more strongly related to symptoms.
The fact that maladaptive emotion regulation strategies were associated with manic symptoms (prior to the interaction terms being added to the model) is interesting. This suggests that these strategies can perpetuate unhealthy mood states, whether manic or depressed. Although we tend to think about rumination as it relates to depression, perseverating on thoughts of one’s special talents or exciting new ideas could have similar consequences in terms of exacerbating one’s mood (Eisner et al. 2008; Feldman et al. 2008; Mansell et al. 2007; Reilly-Harrington et al. 1999; Stange et al. 2012).
As expected, having a BD diagnosis was strongly associated with hypomanic symptoms, but the fact that mood induction response and emotion regulation also accounted for variance in HCL-32 scores suggests that there are individual differences in how emotion processes relate to elevated mood states, independent of diagnosis. People with BD did not, as a group, demonstrate differences in mood induction response and emotion regulation, when compared to those with MDD. Further exploration of how these variables relate, using a dimensional approach, may help to build our understanding for the etiology of both depressive and manic mood states. If it appears that distinct processes are leading to clinical extremes of positive versus negative affect, then it could indicate that what we have considered “bipolar disorder” might better be conceptualized as a comorbid occurrence of manic and depressive disorders (Merikangas et al. 2012; Youngstrom and Van Meter 2013).
Limitations
Overall, there were few differences observed between the MDD and BD samples. A benefit is that there are fewer extraneous variables to consider, but the small sample size would limit power to detect small but potentially meaningful differences. Related, we were unable to test our models in each diagnostic group separately or to test the hypothesis that a three-way interaction between diagnosis, emotion reactivity, and emotion regulation would influence mood symptoms.
Another limitation is that most of the participants were euthymic; previous studies have investigated differences in emotion reactivity and regulation during manic or depressed mood states. Though that is helpful for better understanding emotional processes during a mood episode, investigating people while they are euthymic is important, as one of the key implications of the disordered emotional response system is mood episode recurrence. Additionally, the lack of a comparison group of people without mood disorders limits our ability to determine whether the BD of MDD samples differ from healthy people on the constructs measured.
A related limitation is the cross-sectional design, which precludes us from making predictions about the long-term impact of emotion reactivity and regulation. Though we have theoretical reasons to hypothesize that mood reactivity and emotion regulation, together, influence the development of mood symptoms, given our cross-sectional data, it is possible that mood symptoms were actually driving differences observed on mood induction reactivity and emotion regulation. Although the use of a euthymic sample should minimize the effects of mood, in order to better test our hypotheses, a longitudinal design would be necessary. Rather than focusing on current symptoms, future work could relate emotion reactivity and regulation to the frequency, duration, and severity of mood episodes, ideally in a prospective design, to provide a clearer picture of how these emotional processes impact disorder course.
Although the CERQ is generally a good way to evaluate how people regulate their emotions, it may not fully capture how people regulated their emotions during the mood induction in this study. The instruction to “really notice” the target mood may have changed how people regulated their responses. The interaction between one’s typical emotion regulation strategies with current reactivity may not generalize to how people react/regulate in their daily lives. Future research employing in vivo measurement of mood reactivity and regulation might more accurately depict how emotion processes relate to the onset and maintenance of mood episodes (Aldao 2013; Egloff et al. 2006).
Finally, the interaction between mood induction response and regulation were not significantly related to either depressive or hypomanic symptoms. We expected adaptive emotion regulation strategies to compensate for intense mood induction responses, and maladaptive strategies to exacerbate the relation between mood induction response and symptoms. In research, emotional reactivity and regulation are not usually separated—high reactivity implies poor regulation—likely because it is difficult to parse the measurement of these processes. However, though the constructs of emotion response and emotion regulation are related, an important goal for the field is to find ways by which to measure the extent of the overlap and the independent effects of each construct. Doing so may provide information about the nature of the emotion dysfunction evident in people with mood disorders.
Conclusion
People with mood disorders experience deficits in their ability to accurately process and appropriately regulate their emotion. Historically, research on emotion processes has focused on negative biases and cognitive aspects of emotion as they relate to MDD, and on positive mood reactivity and failure to down-regulate positive emotions as they relate to BD. Present results suggest that MDD and BD share emotion regulation deficits that contribute to depressed moods. Studying emotion processes related to depressed moods from a more dimensional perspective may help to leverage knowledge in order to help people who experience depression, regardless of diagnosis. Similarly, though manic symptoms are more specific to BD, study results suggest that mood response to both threatening and triumphant stimuli is linked with manic symptoms, even after controlling for diagnosis. More precise, objective methods of measurement across the process of emotion generation and regulation in people experiencing a spectrum of mood problems may lead to the identification of treatment targets for future psychosocial interventions.
References
Aldao, A. (2013). The future of emotion regulation research: Capturing context. Perspectives on Psychological Science, 8(2), 155–172. doi:10.1177/1745691612459518.
Aldao, A., Nolen-Hoeksema, S., & Schweizer, S. (2010). Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review, 30(2), 217–237. doi:10.1016/j.cpr.2009.11.004.
Alloy, L. B., Abramson, L. Y., Walshaw, P. D., Cogswell, A., Grandin, L. D., Hughes, M. E., et al. (2008). behavioral approach system and behavioral inhibition system sensitivities and bipolar spectrum disorders: Prospective prediction of bipolar mood episodes. Bipolar Disorders, 10(2), 310–322.
Altshuler, L., Bartzokis, G., Grieder, T., Curran, J., & Mintz, J. (1998). Amygdala enlargement in bipolar disorder and hippocampal reduction in schizophrenia: An MRI study demonstrating neuroanatomic specificity. Archives of General Psychiatry, 55(7), 663.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: American Psychiatric Association.
Angst, J., Adolfsson, R., Benazzi, F., Gamma, A., Hantouche, E., Meyer, T., et al. (2005). The HCL-32: Towards a self-assessment tool for hypomanic symptoms in outpatients. Journal of Affective Disorders, 88(2), 217–233. doi:10.1016/j.jad.2005.05.011.
Angst, J., Gamma, A., & Endrass, J. (2003). Risk factors for the bipolar and depression spectra. Acta Psychiatrica Scandinavica, 108(s418), 15–19. doi:10.1034/j.1600-0447.108.s418.4.x.
Baldessarini, R. J., Vieta, E., Calabrese, J. R., Tohen, M., & Bowden, C. L. (2010). Bipolar depression: Overview and commentary. Harvard Review of Psychiatry, 18(3), 143–157. doi:10.3109/10673221003747955.
Ball, J. R., Mitchell, P. B., Corry, J. C., Skillecorn, A., Smith, M., & Malhi, G. S. (2006). A randomized controlled trial of cognitive therapy for bipolar disorder: Focus on long-term change. The Journal of Clinical Psychiatry, 67(2), 277–286.
Barkley, R. A. (1997). Behavioral inhibition, sustained attention, and executive functions: Constructing a unifying theory of ADHD. Psychological Bulletin, 121(1), 65–94. doi:10.1037/0033-2909.121.1.65.
Beck, A. T. (1974). The development of depression: A cognitive model. In R. J. F. M. M. Katz (Ed.), The psychology of depression: Contemporary theory and research (pp. xvii, 318). Oxford: Wiley.
Beck, A. T. (1978). BDI: Aaron T. Beck.
Beck, A. T. (2005). The current state of cognitive therapy: A 40-year retrospective. Archives of General Psychiatry, 62(9), 953–959. doi:10.1001/archpsyc.62.9.953.
Beck, A., Steer, R., & Carbin, M. (1988). Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review, 8(1), 77–100. doi:10.1016/0272-7358(88)90050-5.
Beck, A., Ward, C., Mendelson, M., Mock, J., & Erbaugh, J. (1961). An inventory for measuring depression. Archives of General Psychiatry, 4(6), 561–571. doi:10.1001/archpsyc.1961.01710120031004.
Black, D., Arndt, S., Hale, N., & Rogerson, R. (2004). Use of the Mini International Neuropsychiatric Interview (MINI) as a screening tool in prisons: Results of a preliminary study. Journal of the American Academy of Psychiatry and the Law Online, 32(2), 158–162.
Blumberg, H., Fredericks, C., Wang, F., Kalmar, J., Spencer, L., Papademetris, X., et al. (2005). Preliminary evidence for persistent abnormalities in amygdala volumes in adolescents and young adults with bipolar disorder. Bipolar Disorders, 7(6), 570–576. doi:10.1111/j.1399-5618.2005.00264.x.
Bowden, C. L. (2001). Strategies to reduce misdiagnosis of bipolar depression. Psychiatric Services, 52(1), 51–55.
Bylsma, L. M., Morris, B. H., & Rottenberg, J. (2008). A meta-analysis of emotional reactivity in major depressive disorder. Clinical Psychology Review, 28(4), 676–691. doi:10.1016/j.cpr.2007.10.001.
Calkins, S. D. (1994). Origins and outcomes of individual differences in emotion regulation. Monographs of the Society for Research in Child Development, 59(2/3), 53–72.
Chang, K., Karchemskiy, A., Barnea-Goraly, N., Garrett, A., Simeonova, D., & Reiss, A. (2005). Reduced amygdalar gray matter volume in familial pediatric bipolar disorder. Journal of American Academy of Child and Adolescent Psychiatry, 44(6), 565–573. doi:10.1097/01.chi.0000159948.75136.0d.
Cohen, J., & Cohen, P. (1983). Applied multiple regression/correlation analysis for the behavioral sciences. Hillsdale, NJ: Lawrence Erlbaum Associates.
Cohen, J., Cohen, P., West, S. G., & Aiken, L. (2003). Applied multiple regression/correlation analysis for the behavioral sciences (3rd ed.). Mahwah, NJ: Lawrence Erlbaum Associates.
Colom, F., Vieta, E., Martinez, A., Jorquera, A., & Gasto, C. (1998). What is the role of psychotherapy in the treatment of bipolar disorder? Psychotherapy and Psychosomatics, 67(1), 3–9. doi:10.1159/000012252.
Davidson, R., Lewis, D., Alloy, L., Amaral, D., Bush, G., Cohen, J., et al. (2002a). Neural and behavioral substrates of mood and mood regulation. Biological Psychiatry, 52(6), 478–502. doi:10.1016/s0006-3223(02)01458-0.
Davidson, R. J., Pizzagalli, D., Nitschke, J. B., & Putnam, K. (2002b). Depression: Perspectives from affective neuroscience. Annual Review of Psychology, 53(1), 545–574. doi:10.1146/annurev.psych.53.100901.135148.
Deckersbach, T., Hölzel, B. K., Eisner, L. R., Stange, J. P., Peckham, A. D., Dougherty, D. D., et al. (2012). Mindfulness-based cognitive therapy for nonremitted patients with bipolar disorder. CNS Neuroscience & Therapeutics, 18(2), 133–141. doi:10.1111/j.1755-5949.2011.00236.x.
Dickstein, D., Brazel, A., Goldberg, L., & Hunt, J. (2009). Affect regulation in pediatric bipolar disorder. Child and Adolescent Psychiatric Clinics of North America, 18(2), 405–420.
Donaldson, C., Lam, D., & Mathews, A. (2007). Rumination and attention in major depression. Behaviour Research and Therapy, 45(11), 2664–2678. doi:10.1016/j.brat.2007.07.002.
Edvardsen, J., Torgersen, S., Røysamb, E., Lygren, S., Skre, I., Onstad, S., & Øien, P. A. (2008). Heritability of bipolar spectrum disorders. Unity or heterogeneity. Journal of Affective Disorders, 106(3), 229–240.
Egloff, B., Schmukle, S. C., Burns, L. R., & Schwerdtfeger, A. (2006). Spontaneous emotion regulation during evaluated speaking tasks: Associations with negative affect, anxiety expression, memory, and physiological responding. Emotion, 6(3), 356–366. doi:10.1037/1528-3542.6.3.356.
Eippert, F., Veit, R., Weiskopf, N., Erb, M., Birbaumer, N., & Anders, S. (2007). Regulation of emotional responses elicited by threat-related stimuli. Human Brain Mapping, 28(5), 409–423. doi:10.1002/hbm.20291.
Eisner, L. R., Johnson, S. L., & Carver, C. S. (2008). Cognitive responses to failure and success relate uniquely to bipolar depression versus mania. Journal of Abnormal Psychology, 117(1), 154–163. doi:10.1037/0021-843X.117.1.154.
Erickson, K., Drevets, W., Clark, L., Cannon, D. M., Bain, E. E., Zarate, C. A, Jr, et al. (2005). Mood-congruent bias in affective Go/No-Go performance of unmedicated patients with major depressive disorder. American Journal of Psychiatry, 162(11), 2171–2173. doi:10.1176/appi.ajp.162.11.2171.
Erk, S., Mikschl, A., Stier, S., Ciaramidaro, A., Gapp, V., Weber, B., & Walter, H. (2010). Acute and sustained effects of cognitive emotion regulation in major depression. The Journal of Neuroscience, 30(47), 15726–15734. doi:10.1523/jneurosci.1856-10.2010.
Fales, C., Barch, D., Rundle, M., Mintun, M., Snyder, A., Cohen, J., et al. (2008). Altered emotional interference processing in affective and cognitive-control brain circuitry in major depression. Biological Psychiatry, 63(4), 377–384.
Feldman, G., Joormann, J., & Johnson, S. (2008). Responses to positive affect: A self-report measure of rumination and dampening. Cognitive Therapy and Research, 32(4), 507–525. doi:10.1007/s10608-006-9083-0.
Garnefski, N., & Kraaij, V. (2006). Relationships between cognitive emotion regulation strategies and depressive symptoms: A comparative study of five specific samples. Personality and Individual Differences, 40(8), 1659–1669.
Gemar, M. C., Segal, Z. V., Sagrati, S., & Kennedy, S. J. (2001). Mood-induced changes on the implicit association test in recovered depressed patients. Journal of Abnormal Psychology, 110(2), 282–289. doi:10.1037/0021-843X.110.2.282.
Getz, G., Shear, P., & Strakowski, S. (2003). Facial affect recognition deficits in bipolar disorder. Journal of the International Neuropsychological Society, 9, 623–632.
Green, M. J., Cahill, C. M., & Malhi, G. S. (2007). The cognitive and neurophysiological basis of emotion dysregulation in bipolar disorder. Journal of Affective Disorders, 103(1–3), 29–42. doi:10.1016/j.jad.2007.01.024.
Green, M. J., Lino, B. J., Hwang, E. J., Sparks, A., James, C., & Mitchell, P. B. (2011). Cognitive regulation of emotion in bipolar I disorder and unaffected biological relatives. Acta Psychiatrica Scandinavica, 124(4), 307–316. doi:10.1111/j.1600-0447.2011.01718.x.
Gruber, J. (2011). Can feeling too good be bad? Positive emotion persistence (PEP) in bipolar disorder. Current Directions in Psychological Science, 20(4), 217–221. doi:10.1177/0963721411414632.
Gruber, J., Eidelman, P., Johnson, S. L., Smith, B., & Harvey, A. G. (2011a). Hooked on a feeling: Rumination about positive and negative emotion in inter-episode bipolar disorder. Journal of Abnormal Psychology, 120(4), 956.
Gruber, J., Harvey, A. G., & Gross, J. J. (2012). When trying is not enough: Emotion regulation and the effort–success gap in bipolar disorder. Emotion, 12(5), 997–1003. doi:10.1037/a0026822.
Gruber, J., Harvey, A. G., & Purcell, A. (2011b). What goes up can come down? A preliminary investigation of emotion reactivity and emotion recovery in bipolar disorder. Journal of Affective Disorders, 133(3), 457–466. doi:10.1016/j.jad.2011.05.009.
Gruber, J., Hay, A. C., & Gross, J. J. (2014). Rethinking emotion: Cognitive reappraisal is an effective positive and negative emotion regulation strategy in bipolar disorder. Emotion, 14(2), 388–396. doi:10.1037/a0035249.
Gruber, J., Johnson, S. L., Oveis, C., & Keltner, D. (2008). Risk for mania and positive emotional responding: Too much of a good thing? Emotion, 8(1), 23.
Gruber, J., Kogan, A., Mennin, D., & Murray, G. (2013). Real-world emotion? An experience-sampling approach to emotion experience and regulation in bipolar I disorder. Journal of Abnormal Psychology, 122(4), 971.
Hariri, A. R., Tessitore, A., Mattay, V. S., Fera, F., & Weinberger, D. R. (2002). The amygdala response to emotional stimuli: A comparison of faces and scenes. NeuroImage, 17(1), 317–323.
Hoertnagl, C. M., Muehlbacher, M., Biedermann, F., Yalcin, N., Baumgartner, S., Schwitzer, G., et al. (2011). Facial emotion recognition and its relationship to subjective and functional outcomes in remitted patients with bipolar I disorder. Bipolar Disorders, 13(5–6), 537–544. doi:10.1111/j.1399-5618.2011.00947.x.
Huntsinger, J., Sinclair, S., Dunn, E., & Clore, G. (2010). Affective regulation of stereotype activation: It’s the (Accessible) thought that counts. Personality and Social Psychology Bulletin, 36(4), 564–577. doi:10.1177/0146167210363404.
Insel, T., Cuthbert, B., Garvey, M., Heinssen, R., Pine, D. S., Quinn, K., et al. (2010). Research domain criteria (RDoC): Toward a new classification framework for research on mental disorders. American Journal of Psychiatry, 167(7), 748–751. doi:10.1176/appi.ajp.2010.09091379.
Jermann, F., Van der Linden, M., d’Acremont, M., & Zermatten, A. (2006). Cognitive Emotion Regulation Questionnaire (CERQ): Confirmatory factor analysis and psychometric properties of the French translation. European Journal of Psychological Assessment, 22(2), 126–131.
Johnson, S., Gruber, J., & Eisner, L. (2007). Emotion and Bipolar Disorder. In J. R. S. L. Johnson (Ed.), Emotion and psychopathology: Bridging affective and clinical science (pp. 123–150). Washington, DC, US: American Psychological Association.
Johnson, S. L., Turner, R. J., & Iwata, N. (2003). BIS/BAS levels and psychiatric disorder: An epidemiological study. Journal of Psychopathology and Behavioral Assessment, 25(1), 25–36. doi:10.1023/A:1022247919288.
Joormann, J., & Gotlib, I. H. (2007). Selective attention to emotional faces following recovery from depression. Journal of Abnormal Psychology, 116(1), 80–85. doi:10.1037/0021-843X.116.1.80.
Kasch, K. L., Rottenberg, J., Arnow, B. A., & Gotlib, I. H. (2002). Behavioral activation and inhibition systems and the severity and course of depression. Journal of Abnormal Psychology, 111(4), 589.
Killgore, W. D. S., & Yurgelun-Todd, D. A. (2004). Activation of the amygdala and anterior cingulate during nonconscious processing of sad versus happy faces. NeuroImage, 21(4), 1215–1223. doi:10.1016/j.neuroimage.2003.12.033.
Kohler, C. G., Hoffman, L. J., Eastman, L. B., Healey, K., & Moberg, P. J. (2011). Facial emotion perception in depression and bipolar disorder: A quantitative review. Psychiatry Research, 188(3), 303–309. doi:10.1016/j.psychres.2011.04.019.
Krüger, S., Seminowicz, D., Goldapple, K., Kennedy, S. H., & Mayberg, H. S. (2003). State and trait influences on mood regulation in bipolar disorder: Blood flow differences with an acute mood challenge. Biological Psychiatry, 54(11), 1274–1283.
Kupka, R. W., Altshuler, L. L., Nolen, W. A., Suppes, T., Luckenbaugh, D. A., Leverich, G. S., et al. (2007). Three times more days depressed than manic or hypomanic in both bipolar I and bipolar II disorder1. Bipolar Disorders, 9(5), 531–535. doi:10.1111/j.1399-5618.2007.00467.x.
Lahera, G., Bayon, C., Fe Bravo-Ortiz, M., Rodriguez-Vega, B., Barbeito, S., Saenz, M., et al. (2014). Mindfulness-based cognitive therapy versus psychoeducational intervention in bipolar outpatients with sub-threshold depressive symptoms: A randomized controlled trial. BMC Psychiatry, 14, 215. doi:10.1186/s12888-014-0215-x.
Lam, D. H., Bright, J., Jones, S., Hayward, P., Schuck, N., Chisholm, D., & Sham, P. (2000). Cognitive therapy for bipolar illness: A pilot study of relapse prevention [Article], Cognitive Therapy & Research. Springer Science & Business Media B.V.
Lam, D. H., Watkins, E. R., Hayward, P., et al. (2003). A randomized controlled study of cognitive therapy for relapse prevention for bipolar affective disorder: Outcome of the first year. Archives of General Psychiatry, 60(2), 145–152. doi:10.1001/archpsyc.60.2.145.
Lecrubier, Y., Sheehan, D. V., Weiller, E., Amorim, P., Bonora, I., Sheehan, K. H., et al. (1997). The Mini International Neuropsychiatric Interview (MINI). A short diagnostic structured interview: Reliability and validity according to the CIDI. European Psychiatry, 12(5), 224–231. doi:10.1016/S0924-9338(97)83296-8.
LeMoult, J., Joormann, J., Sherdell, L., Wright, Y., & Gotlib, I. H. (2009). Identification of emotional facial expressions following recovery from depression. Journal of Abnormal Psychology, 118(4), 828–833. doi:10.1037/a0016944.
Leppanen, J. M. (2006). Emotional information processing in mood disorders: A review of behavioral and neuroimaging findings. Current Opinion in Psychiatry, 19, 34–39.
Lingam, R., & Scott, J. (2002). Treatment non-adherence in affective disorders. Acta Psychiatrica Scandinavica, 105(3), 164–172. doi:10.1034/j.1600-0447.2002.1r084.x.
MacLeod, C., Rutherford, E., Campbell, L., Ebsworthy, G., & Holker, L. (2002). Selective attention and emotional vulnerability: Assessing the causal basis of their association through the experimental manipulation of attentional bias. Journal of Abnormal Psychology, 111(1), 107–123. doi:10.1037//0021-843x.111.1.107.
Mansell, W., Morrison, A. P., Reid, G., Lowens, I., & Tai, S. (2007). The interpretation of, and responses to, changes in internal states: An integrative cognitive model of mood swings and bipolar disorders. Behavioural and Cognitive Psychotherapy, 35(05), 515–539. doi:10.1017/S1352465807003827.
Merikangas, K. R., Cui, L., Kattan, G., Carlson, G. A., Youngstrom, E. A., & Angst, J. (2012). Mania with and without depression in a community sample of US adolescents. Archives of General Psychiatry, 69, 943–951. doi:10.1001/archgenpsychiatry.2012.38.
Meyer, B., Johnson, S. L., & Carver, C. S. (1999). Exploring behavioral activation and inhibition sensitivities among college students at risk for bipolar spectrum symptomatology. Journal of Psychopathology and Behavioral Assessment, 21(4), 275–292.
Meyer, B., Johnson, S., & Winters, R. (2001). Responsiveness to threat and incentive in bipolar disorder: Relations of the BIS/BAS sales with symptoms. Journal of Psychopathology and Behavioral Assessment, 23(3), 133–143. doi:10.1023/a:1010929402770.
Michalak, E. E., Murray, G., Young, A. H., & Lam, R. W. (2008). Burden of bipolar depression. CNS Drugs, 22(5), 389–406.
Miklowitz, D. J. (2006). A review of evidence-based psychosocial interventions for bipolar disorder. Journal of Clinical Psychiatry, 67(Suppl 11), 28–33.
Mitchell, P. B., & Malhi, G. S. (2004). Bipolar depression: Phenomenological overview and clinical characteristics. Bipolar Disorders, 6(6), 530–539. doi:10.1111/j.1399-5618.2004.00137.x.
Morris, B. H., Bylsma, L. M., & Rottenberg, J. (2009). Does emotion predict the course of major depressive disorder? A review of prospective studies. British Journal of Clinical Psychology, 48(3), 255–273. doi:10.1348/014466508X396549.
Murphy, F. C., Sahakian, B. J., Rubinsztein, J. S., Michael, A., Rogers, R. D., Robbins, T. W., & Paykel, E. S. (1999). Emotional bias and inhibitory control processes in mania and depression. Psychological Medicine, 29(06), 1307–1321.
Ochsner, K. N., Bunge, S. A., Gross, J. J., & Gabrieli, J. D. E. (2002). Rethinking feelings: An fMRI study of the cognitive regulation of emotion. Journal of Cognitive Neuroscience, 14(8), 1215–1229. doi:10.1162/089892902760807212.
Phan, K. L., Wager, T., Taylor, S. F., & Liberzon, I. (2002). Functional neuroanatomy of emotion: A meta-analysis of emotion activation studies in PET and fMRI. NeuroImage, 16(2), 331–348. doi:10.1006/nimg.2002.1087.
Phillips, M. L., Drevets, W. C., Rauch, S. L., & Lane, R. (2003a). Neurobiology of emotion perception I: The neural basis of normal emotion perception. Biological Psychiatry, 54(5), 504–514. doi:10.1016/S0006-3223(03)00168-9.
Phillips, M. L., Drevets, W. C., Rauch, S. L., & Lane, R. (2003b). Neurobiology of emotion perception II: Implications for major psychiatric disorders. Biological Psychiatry, 54(5), 515–528. doi:10.1016/S0006-3223(03)00171-9.
Phillips, M. L., Ladouceur, C. D., & Drevets, W. C. (2008). A neural model of voluntary and automatic emotion regulation: Implications for understanding the pathophysiology and neurodevelopment of bipolar disorder. Molecular Psychiatry, 13(9), 833–857.
Piet, J., & Hougaard, E. (2011). The effect of mindfulness-based cognitive therapy for prevention of relapse in recurrent major depressive disorder: A systematic review and meta-analysis. Clinical Psychology Review, 31(6), 1032–1040. doi:10.1016/j.cpr.2011.05.002.
Post, R. M. (2005). The impact of bipolar depression. The Journal of Clinical Psychiatry, 66(5), 5.
Raes, F., Dewulf, D., Van Heeringen, C., & Williams, J. M. G. (2009). Mindfulness and reduced cognitive reactivity to sad mood: Evidence from a correlational study and a non-randomized waiting list controlled study. Behaviour Research and Therapy, 47(7), 623–627. doi:10.1016/j.brat.2009.03.007.
Reilly-Harrington, N. A., Alloy, L. B., Fresco, D. M., & Whitehouse, W. G. (1999). Cognitive styles and life events interact to predict bipolar and unipolar symptomatology. Journal of Abnormal Psychology, 108(4), 567–578.
Ridout, N., Astell, A., Reid, I., Glen, T., & O’Carroll, R. (2003). Memory bias for emotional facial expressions in major depression. Cognition and Emotion, 17(1), 101–122. doi:10.1080/02699930302272.
Rocca, C. C. A., Heuvel, E. v. d., Caetano, S. C., & Lafer, B. (2009). Facial emotion recognition in bipolar disorder: A critical review. Revista Brasileira de Psiquiatria, 31, 171–180.
Roiser, J., Farmer, A., Lam, D., Burke, A., O’Neill, N., Keating, S., et al. (2009). The effect of positive mood induction on emotional processing in euthymic individuals with bipolar disorder and controls. Psychological Medicine, 39(05), 785–791. doi:10.1017/S0033291708004200.
Sajatovic, M., Valenstein, M., Blow, F. C., Ganoczy, D., & Ignacio, R. V. (2006). Treatment adherence with antipsychotic medications in bipolar disorder. Bipolar Disorders, 8(3), 232–241. doi:10.1111/j.1399-5618.2006.00314.x.
Schenkel, L., Pavuluri, M., Herbener, E., Harral, E., & Sweeney, J. (2007). Facial Emotion processing in acutely ill and euthymic patients with pediatric bipolar disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 46(8), 1070–1079.
Scott, J. (2001). Cognitive therapy as an adjunct to medication in bipolar disorder. The British Journal of Psychiatry, 178(41), s164–s168. doi:10.1192/bjp.178.41.s164.
Segal, Z. V., Gemar, M., & Williams, S. (1999). Differential cognitive response to a mood challenge following successful cognitive therapy or pharmacotherapy for unipolar depression. Journal of Abnormal Psychology, 108(1), 3–10. doi:10.1037/0021-843X.108.1.3.
Sheehan, D. V., Lecrubier, Y., Sheehan, K. H., Janavs, J., Weiller, E., Keskiner, A., et al. (1997). The validity of the mini international neuropsychiatric interview (MINI) according to the SCID-P and its reliability. European Psychiatry, 12(5), 232–241. doi:10.1016/S0924-9338(97)83297-X.
Siegle, G. J., Steinhauer, S. R., Thase, M. E., Stenger, V. A., & Carter, C. S. (2002). Can’t shake that feeling: Event-related fMRI assessment of sustained amygdala activity in response to emotional information in depressed individuals. Biological Psychiatry, 51(9), 693–707. doi:10.1016/S0006-3223(02)01314-8.
Silk, J. S., Shaw, Daniel S., Skuban, Emily M., Oland, Alyssa A., & Kovacs, Maria. (2006). Emotion regulation strategies in offspring of childhood-onset depressed mothers. Journal of Child Psychology and Psychiatry, 47(1), 69–78.
Standage, H., Ashwin, C., & Fox, E. (2010). Is manipulation of mood a critical component of cognitive bias modification procedures? Behaviour Research and Therapy, 48(1), 4–10. doi:10.1016/j.brat.2009.08.005.
Stange, J. P., Molz, A. R., Black, C. L., Shapero, B. G., Bacelli, J. M., Abramson, L. Y., & Alloy, L. B. (2012). Positive overgeneralization and Behavioral Approach System (BAS) sensitivity interact to predict prospective increases in hypomanic symptoms: A behavioral high-risk design. Behaviour Research and Therapy, 50(4), 231–239. doi:10.1016/j.brat.2012.01.003.
Strakowski, S. M., Delbello, M. P., & Adler, C. M. (2005). The functional neuroanatomy of bipolar disorder: A review of neuroimaging findings. Molecular Psychiatry, 10(1), 105–116. doi:10.1038/sj.mp.4001585.
Sullivan, P. F., Neale, M. C., & Kendler, K. S. (2000). Genetic epidemiology of major depression: Review and meta-analysis. American Journal of Psychiatry, 157(10), 1552–1562. doi:10.1176/appi.ajp.157.10.1552.
Townsend, J. (2012). Emotion processing and regulation in bipolar disorder: A review. Bipolar Disorders, 14(4), 326–339. doi:10.1111/j.1399-5618.2012.01021.x.
Vederman, A. C., Weisenbach, S. L., Rapport, L. J., Leon, H. M., Haase, B. D., Franti, L. M., et al. (2012). Modality-specific alterations in the perception of emotional stimuli in bipolar disorder compared to healthy controls and major depressive disorder. Cortex, 48(8), 1027–1034. doi:10.1016/j.cortex.2011.03.017.
Westermann, R., Spies, K., Stahl, G., & Hesse, F. W. (1996). Relative effectiveness and validity of mood induction procedures: A meta-analysis. European Journal of Social Psychology, 26(4), 557–580. doi:10.1002/(sici)1099-0992(199607)26:4<557:aid-ejsp769>3.0.co;2-4.
Wright, K., Lam, D., & Newsom-Davis, I. (2005). Induced mood change and dysfunctional attitudes in remitted bipolar I affective disorder. Journal of Abnormal Psychology, 114(4), 689–696. doi:10.1037/0021-843X.114.4.689.
Yap, M. B. H., Allen, N. B., & Sheeber, L. (2007). Using an emotion regulation framework to understand the role or temperament and family processes in risk for adolescent depressive disorders. Clinical Child and Family Psychology, 10(2), 180–196.
Youngstrom, E., & Izard, C. E. (2008). Function of emotions functions of emotions and emotion-related dysfunction. In A. J. Elliot (Ed.), Handbook of approach and avoidance motivation (p. 367). New York, NY: Taylor & Francis.
Youngstrom, E. A., & Van Meter, A. (2013). Comorbidity of bipolar disorder and depression. In S. Richards & M. W. O’Hara (Eds.), Oxford handbook of depression and comorbidity. New York, NY: Oxford University Press.
Acknowledgments
This study was funded by the North Carolina Translational and Clinical Sciences Institute (grant #2KR341108).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Anna Van Meter was the recipient of the grant listed above; she has no other conflicts of interest. Eric Youngstrom has received research grants from NIMH and has served as a consultant about assessment to Lundbeck and Otsuka in the past.
Informed Consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (national and institutional). Informed consent was obtained from all individual subjects participating in the study. If any identifying information is contained in the paper the following statement is also necessary. Additional informed consent was obtained from any subjects for whom identifying information appears in this paper.
Animal Rights
No animal studies were carried out by the authors for this article.
Rights and permissions
About this article
Cite this article
Van Meter, A.R., Youngstrom, E.A. Distinct Roles of Emotion Reactivity and Regulation in Depressive and Manic Symptoms Among Euthymic Patients. Cogn Ther Res 40, 262–274 (2016). https://doi.org/10.1007/s10608-015-9738-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10608-015-9738-9