Abstract
Low-income mothers face numerous challenges that increase their vulnerability to psychological distress. Their perceived or actual difficulty in accessing vital support networks, whether public or private, can significantly amplify this distress. Socially assigned identities, such as nativity, ethnicity, and race, intersect with socioeconomic factors, influencing mental health outcomes. Using data from the Future of Families and Child Wellbeing Study, our research investigated the impact of public and private safety nets on maternal psychological health. We found that, even after accounting for socioeconomic factors, non-Hispanic, US-born White mothers experienced higher levels of psychological distress compared to minoritized mothers. The role of safety nets varied by race and ethnicity, with private safety nets providing unique protection to Black and Hispanic mothers, while support was associated with increased distress only among White mothers. These findings highlight the need to consider sociocultural history when assessing safety net impacts on mental health.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
As a consequence of living in poverty and parenting, low-income mothers encounter many obstacles that contribute to an elevated susceptibility to psychological distress [1,2,3,4]. Maternal distress plays a central role in various aspects of a woman’s well-being during their lifespan, including pregnancy, postpartum, and how they are able to care for their children [5]. A mother’s perceived or actual inability to access essential safety nets, whether public or private, necessary to provide for her family, can significantly amplify psychological distress [6]. This distress can manifest as internalizing symptoms such as depression and externalizing symptoms such as drug use or risky behaviors and is often intertwined with race, ethnicity, and nativity [7]. By 2030, depression is projected to be the main global health burden, with women being 50% more likely to report such occurrences than men [2] Depressive symptoms prompted by multifaceted psychosocial stressors can produce physiological alterations that can translate into risky behaviors and elevated levels of morbidity, mortality, and disability, particularly among socioeconomically disadvantaged and diverse populations [3, 4].
Socially assigned identities like nativity, ethnicity, and race have been shown to interconnect with socio-economic circumstances, exerting influence over mental health and well-being outcomes [8,9,10]. Accumulated cultural and socioeconomic life experiences shape one’s perception and understanding of the world, as well as influence help-seeking behaviors [4, 6, 10]. Nativity introduces an extra layer of diversity within a group, which can offer a better understanding of its distinct characteristics and experiences [7, 11]. Not all minoritized or underserved groups can be considered homogenous; rather, they encompass diverse cultures, beliefs, and varying degrees of health risk [12, 13]. Nativity could offer more accurate insights into tackling psychological distress disparities. Unfortunately, nativity as a cultural concept is frequently overlooked in research. The intricate connection between social and cultural identity and the influence on low-income women’s psychological distress remains inadequately studied. Comprehending these dynamics is imperative for assessing specific social group exposures and experiences concerning their psychological distress in relation to public and private safety nets.
Low-income mothers facing challenges in securing financial stability for their families often attempt to seek aid through a combination of public governmental programs and private non-governmental safety nets, aiming to reduce both social and mental disparities [14,15,16,17]. The configuration, acquisition, and perception of public and private safety nets for low-income women can vary based on socioeconomic status, race, ethnicity, and nativity [1, 18]. Safety nets, whether they are established within the public sector, the private domain, or through a synergistic collaboration, assume a pivotal and proactive role in both the prevention and management of psychological distress [14,15,16,17,18,19]. Certain safety nets may include tangible material assistance, while others may encompass a sense of communal belonging rooted in cultural values and experiences [7, 8, 20].
Given the intersectionality of sociocultural factors, understanding the intricate interplay among these elements is essential for delivering effective support, particularly to low-income women. For instance, a woman from a low-income background who belongs to a marginalized racial or ethnic group may face compounded challenges, resulting in heightened psychological distress [7, 13]. Conversely, a woman with higher socioeconomic status and greater access to resources may still experience psychological distress due to other factors, such as social isolation or personal expectations [7, 13]. This study extends existing research concerning the configuration of safety nets and sociocultural factors. Through this research, our goal was to investigate the interplay between safety nets, as well as race, ethnicity, and nativity, and their combined impact on shaping the degrees of psychological distress (manifesting as both internalizing and externalizing symptoms) encountered by low-income mothers.
Significance
Safety Net Support as Social Determinants of Health (SDoH)
The SDoH framework recognizes five primary determinants (economic stability, education, healthcare access, environment, and social/community context) that impact overall well-being [8,9,10]. Therefore, the availability and effectiveness of social safety nets (public or private) play a significant role in influencing an individual’s health status [7, 19]. The contextual determinants of safety net perceptions and use have been investigated to identify factors that act as both facilitators and barriers, including considerations of psychological distress [8, 21]. For example, while Black and Hispanic mothers receive more private, non-financial support, White mothers both perceive and receive more financial support [22, 23]. Support may operate differently for families of different races and ethnicities. A qualitative study of current and former mothers receiving TANF found that receiving TANF increased distress more so for Black than White mothers [24].
A systematic review of informal support among low-income mothers [14] indicated that perceiving a private safety net was associated with lower levels of maternal psychological distress. In one study [6] it was observed that low-income mothers who relied solely on public safety nets were more prone to psychological distress compared to those with both public and private safety nets. Consequently, the availability of private support emerged as a protective measure against psychological distress. In a contrasting qualitative study conducted by Mazelis and Mykyta [25], seeking or receiving assistance from private safety nets heightened psychological stress in certain instances due to factors such as personal pride, the obligation of reciprocity, or the desire to maintain independent adulthood. Considering the varying outcomes in research, further investigation is warranted concerning private safety nets, particularly related to distinguishing between perceived and received supports. Moreover, comprehensive exploration must encompass social factors like race, ethnicity, and nativity, given that distinct groups possess varied experiences and need diverse interventions.
Race, Ethnicity, and Nativity as Social Determinants of Health
There is a discernible correlation between race, ethnicity, nativity, and the prevalence of poverty among low-income women, with certain groups facing disproportionately higher rates of economic hardship [25,26,27]. According to the 2020 Census, while Whites constitute roughly 7% of the impoverished population, Blacks and Hispanics comprise 19% and 16%, respectively [28]. Significant disparities are also seen among immigrant groups, with 13% of foreign-born and 11% of US-born immigrants living in poverty in 2020 [28]. The proportion of immigrants in the United States increased threefold between 1970 and 2019, rising from 4.8 to 14% in that period. This demographic shift represented 44.9 million individuals [29, 30]. Moving beyond race and ethnicity is imperative in identifying high-risk subgroups. For instance, Hummer [12] discovered that considering nativity reveals significant differences in mortality rates between foreign-born individuals and their native-born counterparts. Nativity influences various health behaviors and outcomes, warranting deeper investigation as it presents potential obstacles or sources of support in addressing psychological distress among low-income mothers. The race, ethnicity, and nativity cultural connection underscores the need for targeted research, interventions, and policies to address marginalized populations’ specific challenges.
Plant’s [31] examination of depression revealed that minority group members, who displayed enhanced interpersonal skills compared to White individuals, demonstrated lower depression levels. This observation was linked to the potential influence of a shared cultural heritage that emphasizes community, family, and interpersonal relationships. It is worth highlighting, however, that the study did not investigate the impact of nativity. Despite certain commonalities in immigrant experiences, even greater variations exist within distinct populations [13]. In 2007, Williams and colleagues [13] showed that Caribbean immigrants had lower rates of major depressive disorder (MDD) compared to those born in the U.S. African American Blacks exhibited more severe MDD symptoms than Caribbean Blacks, and the latter received less treatment (22% vs. 48%). By omitting considerations of nativity, race, and ethnicity in health research, we fail to recognize pivotal elements that can contribute to heightened disparities or provide protective properties.
Psychological Distress
The experience of psychological distress arises from the dynamic interplay between an individual and their environment, where the perception of demands exceeding available resources can jeopardize one’s well-being [16, 17, 32]. Frequent and ongoing exposure to situations perceived as threatening and overwhelming, exceeding an individual’s coping capacities, can amplify susceptibility to unfavorable depressive symptoms and maladaptive behaviors such as drug use [16, 17, 32]. For example, Plant’s [31] research showed that maternal emotional well-being is adversely affected when low-income mothers struggle to fulfill their basic needs. This discovery was substantiated by subsequent studies, suggesting that increased stress exposure might raise the probability of experiencing depression [33,34,35]. Numerous studies have established a correlation between prolonged exposure to chronic stress and depressive symptoms, as well as engagement in risky behaviors such as smoking or drug use [36, 37]. In a study conducted by Cook in 2009 [38] involving a cohort of low-income women receiving governmental cash benefits, 53% of these women exhibited a lifetime prevalence of mental disorders, with a concurrent prevalence of 29% for substance use disorders. However, a significant proportion of these cases remained untreated. Rosen et al.’s study [39] not only corroborates these findings but also reports that women facing more barriers are less likely to receive mental health or substance abuse treatment.
Cultural influences and intricate social factors contribute to diminished tendencies to seek assistance within ethnically diverse subgroups [13, 40, 41]. Williams and collaborators [13] revealed that Caribbean Blacks exhibited a higher likelihood of experiencing a lifetime prevalence of MDD compared to African American Blacks. Additionally, the chronicity of MDD was more pronounced in both Black groups when compared to Whites. Moreover, it was observed that MDD among Caribbean Blacks and African Americans typically remained untreated, with their conditions being characterized by greater severity and disability in comparison to non-Hispanic Whites. Despite the treatability of most mental disorders, the gap in care persists among marginalized groups, leading to heightened levels of disability, morbidity, and mortality. This disparity in mental health care can exacerbate physical health issues and perpetuate broader inequalities across diverse populations. The fifth iteration of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) [42] recognizes the significance of factoring in cultural and social aspects in the mental health care of individuals. However, limited research addresses psychological distress from the perspective of safety nets, race, ethnicity, and nativity among low-income mothers. In this study, we investigated the interplay between safety nets, race, ethnicity, and nativity in relation to psychological distress among low-income mothers. Additionally, we explored whether race, ethnicity, and nativity were moderating factors in the relationship between safety nets and psychological distress.
Data and Methods
Data
This study used data from the Future of Families and Child Wellbeing Study (FFCWS), formerly the Fragile Families and Child Wellbeing Study. It is a longitudinal birth cohort study of nearly 5,000 children born to largely unmarried mothers (75%) in large U.S. cities (> 200,000 residents) from 1998 to 2000 [43]. The University Institutional Review Board approved this secondary study procedure, and informed consent was obtained from all participants in the parent study. The study aims to understand the causes and consequences of living conditions and sociocultural problems of the study population. Mothers (and fathers) were enrolled in the study in hospitals within 72 h of giving birth.
The analysis included data from the maternal follow-up telephone interviews conducted 1, 3, 5, and 9 years after the mothers gave birth to the focal child. Response rates ranged from 90% (Year 1) to 76% (Year 9). We limited the sample to mothers who lived below 200% of the poverty line at least once during the analyzed waves (83% of records) as families typically require an income twice the poverty line to meet their basic needs [44]. We excluded participants who did not live with their children after baseline (n = 4), and, due to their small number and our interest in race, ethnicity, and nativity, immigrants of another non-Hispanic race (n = 80). After listwise deletion, the sample included all mothers with complete data for at least one data point (n = 3,741). Missing data analyses indicated that mothers with missing data were similar to those included on all measured variables with one exception: included mothers were more likely to have lived with both biological parents at age 15.
Measures
Maternal Psychological Distress. We measured internalizing and externalizing symptoms of psychological distress, two important components of distress when measuring the potential impact of safety nets [45, 46]. Symptoms were measured during each wave.
Internalizing symptoms. The Composite International Diagnostic Interview Short From (CIDI-SF) [47] was used to measure if mothers likely had a major depressive episode in the previous year. Using scoring from the developers, mothers who experienced depressive symptoms for at least half of the day and at least three additional symptoms were coded as a probable case for internalizing symptoms (1), 0 otherwise.
Externalizing symptoms. Heavy drinking or illicit drug use constitutes externalizing symptoms of depression in the past year. Mothers who consumed 4 or more drinks in one sitting (5 + drinks at Y1 survey) or used an illicit drug without following a prescription (amphetamines, analgesics, cocaine, heroin, inhalants, LSD/hallucinogens, marijuana, sedatives, or tranquilizers) were coded as 1, 0 otherwise. Year 1 measures referred to behavior in the previous month rather than the preceding year. Models beginning at Year 3 did not differ substantively from the longer time period. Therefore, we included Year 1 data in the analysis.
Safety nets. To measure perceived private support, mothers indicated whether they could rely on family or friends to provide (a) $200, (b) child care, or (c) a place to live in an emergency. We added the available supports to create an index of available support. Mothers indicated whether or not they had received any money from family or friends in the past year. This dichotomous indicator reflected received support. We created an index of public support to indicate the number of public program benefits that mothers received. Mothers indicated whether they received (a) Temporary Assistance for Needy Families (TANF), (b) Supplemental Nutrition Assistance Program benefits, also known as food stamps, (c) housing assistance in the form of Sect. 8 vouchers or public housing, and (d) Medicaid or Children’s Health Insurance Program benefits.
Race, ethnicity, and nativity. We used three items to construct a measure of race, ethnicity, and nativity. Mothers indicated if they were of Hispanic or Latina origin. They also indicated their race based on the U.S. Census categorization. To measure nativity, participants answered whether or not they were born in the U.S. From these measures, we created five mutually exclusive categories: Hispanic, U.S. born; non-Hispanic Black, U.S. born; Hispanic immigrant; non-Hispanic immigrant; and non-Hispanic White, U.S. born.
Sociodemographic covariates. We included covariates previously associated with safety nets and health [48, 49]. We included two predictors measured at baseline. FFCWS staff members constructed maternal age measured in years at the baseline survey. As an indicator of socioeconomic background, mothers reported whether they lived with both biological parents at age 15, coded 1, 0 otherwise. We treated the remaining covariates as time-varying, including a measure at each wave. Mothers indicated their highest level of education including their highest degree. We created a three-category ordinal variable distinguishing among less than high school (1), high school or equivalent only (2), and some college, college degree, or above (3). Living arrangements included those who were single (1), cohabiting (2), or married (3). We used FFCWS-created measures for the number of children under age 18 currently living in the household and the household poverty level as the percentage of the federal poverty guidelines. Mothers reported whether they had worked for pay in the previous two weeks (1 = yes, 0 = otherwise).
Analytic Strategy
After providing a sample description, we conducted random-effects logistic regression modeling to examine the relationships between safety nets and depressive symptomology and whether the relationships were conditioned by race, ethnicity, and nativity. Random effects models estimated depressive symptomology as a function of safety net components; race, ethnicity, nativity; and socioeconomic covariates. In Stata 17.0, we converted the data in a mother-wave format such that each mother contributed data up to four points in time. We estimated multiple random effects models separately for internalizing and externalizing symptomology. The first model estimated the relationships among safety nets; race, ethnicity, and nativity; and depressive symptomology, without additional predictors. The second model, the full model, included both time-invariant (i.e., age at focal child’s birth, whether or not mother lived with both biological parents at age 15) and time-varying maternal covariates (educational level, relationship status, number of children in the household, household’s percent of the federal poverty guidelines, employment status). Next, we tested race-ethnicity-nativity interactions separately with each safety net component (i.e., number of private supports, whether or not the mother received cash, and number of public supports) and identified the best-fitting models with significant interactions. Because both public and private safety nets may operate in combination to influence maternal distress [6], we present the interaction models separately for perceiving and receiving support to present two different facets of the same construct of safety nets.
Sample Characteristics
Table 1 presents mothers’ time-invariant characteristics measured at the time of the focal child’s birth (i.e., baseline). The sample is racially and ethnically diverse. One-half of mothers were non-Hispanic Black, U.S.-born, and 18% were Hispanic U.S.-born. The sample included a large proportion of immigrants (16%), who were largely Hispanic (12%). The oversampling of unmarried mothers resulted in a relatively young sample (M = 24 years). Only 38% of mothers reported living with both of their biological parents at age 15.
Table 2 displays the time-varying characteristics at 1, 3, 5, and 9 years after the focal child’s birth. A large minority of mothers (16–22%) reported internalizing symptoms that suggested major depression within the past year. The rates of internalizing symptoms did not change over data collection phases. Fewer mothers, at least when their children were very young, reported externalizing symptoms. The percentage reporting problematic drinking or illicit drug use more than doubled over time from 9% in Year 1 to 22% in Year 9. Perceptions and use of private and public safety nets were relatively high and stable across time. Mothers, on average, perceived help in two of three areas. Additional analyses indicated that about three-fourths of mothers perceived access to all supports; among those without access in all three domains, financial access was the most common missing component at each wave. Up to about half of mothers (41–52%) received cash from family or friends in the last year. Mothers typically received government assistance from one or two programs, regardless of year. The remainder of Table 2 reveals mothers’ high level of vulnerability one year after giving birth that dissipates somewhat in the subsequent eight years. Although only 31% of mothers had more than a high school education at Year 1, for example, this percentage surpassed 50% by Year 9. Employment increased from 49 to 61%, although poverty remained high, with the average mother gaining few additional resources (120–140% of the poverty level from Year 1 to Year 9).
Results
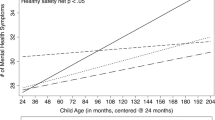
Tables 3 and 4 display the random effects logistic regression models of internalizing and externalizing symptoms of psychological distress, respectively. Examining internalizing symptoms, Model A indicated race, ethnicity, nativity, and each safety net component were strongly related to internalizing symptoms. Hispanic mothers, both U.S.-born and immigrant, and non-Hispanic Black U.S.-born had lower odds of probable depression compared to their White, U.S.-born counterparts (OR = 0.43, − 0.63). Black mothers, for example, had 37% lower odds of having a concerning level of internalizing symptoms compared to White mothers. Perceiving additional support from private networks decreased the odds of internalizing symptoms, while receiving network cash or public assistance increased the odds. The interclass correlation coefficient (Rho) of 0.45 indicates a high degree of residual autocorrelation and that differences between mothers account for almost half of the total variance in the probability of a concerning level of internalizing symptoms. The addition of individual-level socioeconomic covariates in Model B demonstrated that having lived with both parents at age 15 and being employed decreased the odds of a concerning level of symptoms while being single as compared to being married increased the odds. The addition of the covariates, however, did little to attenuate the relationship between race, ethnicity, and nativity or safety net characteristics to internalizing symptoms. Models C and D indicated significant race-ethnic-nativity and safety net interactions. Figure 1, Panel A illustrates the relationship between race/ethnicity/nativity and the number of perceived supports. Although perceived supports decreased the probability of a concerning level of internalizing symptoms for all groups, the negative slope was significantly steeper for Hispanic, U.S.-born, and Black, U.S.-born mothers than for White, U.S.-born mothers. Perceiving more support decreased the probability more so for the ethnoracial groups. Network cash receipt, alternatively, increased the probability of internalizing symptoms. The slope was steeper for White, U.S.-born mothers compared to their Hispanic and Black counterparts. Receiving network cash did not increase the level of internalizing symptoms for Hispanic, U.S.-born and Black, U.S.-born mothers to the degree that it did for their white U.S.-born counterparts.
Table 4 provides parallel results for externalizing symptoms. Similar to findings for internalizing symptoms, Model A shows that non-White ethnoracial groups, particularly immigrant minority mothers, experienced lower odds of heavy drinking or substance use. U.S.-born Black mothers, for example, experienced 58% lower odds of these behaviors than non-Hispanic White mothers. In terms of safety nets, mothers who received network money experienced twice the odds of externalizing symptoms compared to those who did not. The interclass correlation coefficient of 0.40 indicates that, similar to internalizing symptoms, differences in mothers account for a large portion of the total variance in the probability of externalizing symptoms. The addition of socioeconomic covariates in Model B indicated that the odds of substance misuse or use increased over time and increased for single and cohabiting mothers as compared to married mothers. Alternatively, mothers who lived with both biological parents at age 15 experienced lower odds of substance use compared to those who did not, and use decreased as mothers aged. Similar to internalizing symptoms, including sociodemographic covariates did little to attenuate the relationships between race, ethnicity, and nativity and safety net characteristics and externalizing symptoms. Model C demonstrated that race, ethnicity, nativity, and number of perceived supports interacted such that the number of supports decreased the probability of externalizing symptoms for Black, U.S.-born mothers and increased the probability of symptoms for their non-Hispanic White counterparts (see Fig. 2).
Discussion
This study examined the effects of sociocultural factors (race, ethnicity, and nativity) and safety nets on psychological distress (internalizing and externalizing symptoms). The current findings help to clarify the relationships among these variables among low-income women. This study contributes to the existing literature by presenting a different perspective. Our findings indicate that White low-income mothers exhibited an elevated susceptibility to internalized symptoms of depression, along with a heightened likelihood of engaging in externalizing behaviors such as heavy drinking or substance misuse. These vulnerabilities exceed those noted within both U.S.- and non-U.S.-born Hispanic and Black populations. While prior research commonly considers nativity’s protective role in differentiating U.S.-born and non-U.S.-born individuals, this contrast is less evident in this study’s findings. This study demonstrates that internalizing symptoms are similarly prevalent among Hispanic or Black mothers, whether U.S.- or non-U.S.-born, in comparison to non-Hispanic White mothers. The study emphasizes the need for a more in-depth exploration of race, ethnicity, nativity, and cultural viewpoints related to utilizing various safety nets among low-income subgroups.
For Hispanics and Blacks, regardless of U.S. birth status, both perceived and received private safety nets lowered the risk of potential internalizing depressive symptoms compared to Whites. However, receiving cash or perceiving private support did not protect Whites against depressive symptoms. Boyd’s study [50] likewise indicated elevated rates of mood disorders in White mothers compared to African American and Caribbean Black mothers. Consistent research examining various forms of distress has also reaffirmed that factors like parental stress [20], socioeconomic status [33], and involvement in welfare programs [37] are associated with increased distress levels in White women, in contrast to Black, Hispanic, and Asian women. Other research [14, 51] found that informal support from friends and families is less accessible to low-income women, yet it acts as a protective factor against negative maternal health and well-being outcomes. This holds true for our findings, but solely for Hispanic and Black groups influenced by their sociocultural experiences.
Plant’s [31] study sheds light on this anomaly, revealing that some minority groups showed superior interpersonal functioning compared to White participants, potentially shielding them from depression and demoralization. It also suggested that these differences might be rooted in cultural influences arising from the collective emphasis on family and interpersonal relationships within minority groups, in contrast to cultures focused on independence. Another explanation lies in ethnic identity, supported by research [1, 52] as a factor in maintaining mental well-being. Elements like ethnic pride, involvement in ethnic activities, and a cultural dedication to one’s racial or ethnic community contribute to this protective influence. Our study presents a compelling argument to redirect the focus away from nativity, race, or ethnicity separately. Instead, emphasis should be placed on understanding how these cultural factors interact to determine why certain safety nets function as social protective mechanisms for some groups while contributing to heightened psychological distress in others. This suggests that private support plays a more influential role in explaining certain outcomes than sociocultural factors when examined in isolation. However, it is important to note that when accounting for variables such as race, ethnicity, and nativity, the significance of sociocultural factors diminishes, emphasizing the significance of private support in understanding these outcomes.
Regarding externalizing symptoms of psychological distress, such as an elevated susceptibility to substance and alcohol use, the outcomes mirrored those observed for internalizing symptoms. In exploring the connections between race, ethnicity, nativity, and safety nets, the study discovered that immigrant mothers had lower odds of heavy drinking or substance use than U.S.-born Black mothers. Moreover, U.S.-born Black mothers exhibited a 58% lower likelihood of such behaviors in contrast to non-Hispanic White mothers. Consistent with earlier research [38], our study revealed that low-income mothers face an increased likelihood of drug and alcohol abuse compared to a community sample of single mothers. An additional study [37] substantiated a reduced risk of substance use disorder (SUD) among Hispanics and Blacks whereas White welfare recipients exhibited an elevated level of substance use compared to their African American and Hispanic counterparts. Furthermore, the study also affirmed that psychological distress among low-income White mothers was connected to nicotine and alcohol dependence. Our study found that White mothers experience more depressive symptoms than Black and Hispanic mothers, potentially leading to self-medication for distress. Research [51] links depression to increased alcohol use as a coping mechanism, particularly among those facing negative life events and limited family support. These vulnerabilities underline the association between depression and coping through externalizing symptoms such as substance use or abuse.
Obtaining cash from a social network doubled the odds of externalizing symptoms (such as alcohol or drug use), while a greater number of perceived supports reduced odds for U.S.-born Black mothers but increased odds for non-Hispanic White mothers. This tendency could be partly explained by the results of qualitative interviews involving 51 low-income White mothers receiving public assistance [53]. The study found that participants aimed for self-sufficiency and independence and hesitated to seek help due to the prevailing stigma tied to single mothers on welfare. These mothers’ worries centered on being perceived as dependent and misusing public safety nets. The study indicated that these mothers isolate themselves despite community encouragement, aiming to cultivate a positive self-image and command respect. This response arises from societal stereotypes of people who receive public assistance, categorizing them as embedded in a dysfunctional culture, rather than acknowledging their status as casualties of poverty. This interpretation gains support from two studies [25, 54] which highlight that reciprocity among low-income individuals can foster relational stress, leading to network exclusion and self-isolation to avoid criticism. This triggers resource scarcity and efforts to project normalcy for self-worth and financial autonomy, resulting in substantial stress and susceptibility to externalizing symptoms. Such behavior is attributed to pride, expectations of reciprocity, and notions of self-sufficiency in adulthood.
Disparities in cultural perspectives may help clarify these divergent trends. Specifically, the inclination of White low-income mothers to pursue self-reliance and abstain from assistance contrasts with the perspective of Hispanic and Black low-income mothers, who perceive their communities as embracing support from both familial and non-familial sources. This perception aligns with the notion of a community-based belief, where a collective effort is deemed essential for survival. This sentiment stems from a historical context of trauma, marginalization, and limited government support, combined with experiences of discrimination and stigmatization [55,56,57]. Consequently, reliance on community support has been strengthened within minority communities.
Limitations
While this study contributes valuable insights into the realm of safety net measures and their implications, it is essential to acknowledge several limitations. These limitations warrant consideration and caution when interpreting the findings. First, the safety net measures are crude in nature and may lack the accuracy to measure the complexity of the interplay of race, ethnicity, and nativity. Second, the safety net measures included in this study provide an initial and broad understanding of the support landscape and may lack the depth required to capture the intricacies of various safety net components. As such, the study’s ability to comprehensively analyze the multifaceted safety net landscape may be constrained by the basic nature of these measures. Third, the omission of certain private safety net information, such as emotional support and receipt of private charity, may result in an incomplete representation of the actual safety net landscape, potentially affecting the accuracy of the study’s conclusions.
Fourth, the potential exists for perceptions related to the accessibility of safety nets to reflect subjective beliefs instead of accurately reflecting the actual availability of supportive resources. This introduces a potential confounding factor that might influence the study’s outcomes and necessitates caution in attributing results solely to the presence or absence of safety net measures. Fifth, despite attempts to analyze public safety net components, the models failed to modify the outcomes significantly. This suggests that certain public program contexts might not have been fully accounted for, possibly limiting the study’s ability to comprehensively assess the effects of specific public programs. Using self-reported data to assess participation in public programs may introduce recall bias and underreporting, potentially leading to underestimation of participation. Thus, findings on program effects might lack precision and inadequately reflect usage. Sixth, it’s important to highlight that nativity was evaluated using binary variables (U.S.-born or non-U.S.-born), lacking the inclusion of culturally intricate details. Factors such as the duration of U.S. residency or affiliation with distinct subgroups within the Hispanic or Black diaspora could offer richer cultural insights. This broader perspective would enhance our understanding of how cultural influences shape perceptions concerning safety nets. Lastly, our decision to measure internalizing symptoms through major depressive episodes in the previous year and externalizing symptoms through heavy drinking and illicit drug use was guided by their established relevance and prevalence in the literature [58, 59] as indicators of these behaviors. However, we recognize the limitation that other forms of internalizing symptoms (e.g., anxiety) and externalizing symptoms (e.g., aggression, delinquency, hyperactivity) were not included. This is indeed a limitation of our study, as it focuses primarily on depression and substance use. Future studies should incorporate a wider array of behaviors to capture the full spectrum of internalizing and externalizing symptoms.
Summary
In conclusion, maternal psychological distress results from a complex interplay of race, ethnicity, nativity, and safety nets (public and private). Clinicians and researchers must recognize that an individual’s identity extends beyond their skin color. Considering historical and cumulative sociocultural experiences that shape our perceptions of safety nets is essential. Some low-income mother groups find them favorable, while others experience harm due to the associated stress, influenced by the societal view of low-income women receiving safety net support. By illuminating these intricate dynamics, the study significantly advances the understanding of mental health and substance use risk and protective factors, including safety net support, within low-income mothers. The approach to care should move beyond a homogeneous solution but instead be inclusive of health beliefs and social help-seeking patterns. Recognizing inherent diversity and adopting a nuanced and personalized approach to care becomes vital. This ensures tailored interventions meet unique needs, ultimately promoting equitable and effective social service delivery.
Data Availability
The present study drew upon data derived from the Future of Families and Child Wellbeing Study, previously identified as the Fragile Families and Child Wellbeing Study. Access to this dataset necessitates strict compliance with the formal request procedures established by the custodians of this dataset.
References
McDonald A, Thompson AJ, Perzow SED, Joos C, Wadsworth ME (2020) The protective roles of ethnic identity, social support, and coping on depression in low-income parents: a test of the adaptation to poverty-related stress model. J Consult Clin Psychol 88:504–515. https://doi.org/10.1037/ccp0000477
Brody DJ, Pratt LA, Hughes JP Prevalence of depression among adults aged 20 and over: United States, 2013–2016. NCHS Data Brief, no. 303. https://www.cdc.gov/nchs/products/data
Dunn EC, Wiste A, Radmanesh F, Almli LM, Gogarten SM, Smoller JW (2016) Genome-wide association study (GWAS) and genome-wide by environment interaction study (GWEIS) of depressive symptoms in African American and Hispanic/Latina women. Depress Anxiety 33:265–280. https://doi.org/10.1002/da.22484
U.S. Department of Health and Human Services Mental health: culture, race, and ethnicity: A supplement to mental health: A report of the surgeon general.2001. https://www.ncbi.nlm.nih.gov/pubmed/20669516
Radey M, Brewster K (2013) Predictors of stability and change in private safety nets of unmarried mothers. J Soc Serv Res 39:397–415. https://doi.org/10.1080/01488376.2013.775090
Radey M, McWey L, Cu M (2020) Psychological distress among low-income mothers: the role of public and private safety nets. Women Health 60:692–706. https://doi.org/10.1080/03630242.2019.1700586
Williams DR (2018) Stress and the mental health of populations of color: advancing our understanding of race-related stressors. J Health Soc Behav 59:466. https://doi.org/10.1177/0022146518814251
Healthy P (2030) U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. https://health.gov/healthypeople/priority-areas/social-determinants-health
Wilkinson M, Marmot R (2006) Social determinants of health, 2nd edn. Oxford University Press, Oxford, NY
Brunner E, Marmot M Social organization, stress, and health. In Marmot MG, Wilkinson RG (eds) Social determinants of health. 2nd ed. New York: Oxford University Press. pp. 6–30
Hummer RA, Hamilton ER (eds) (2019) Population health in America. University of California Press, Berkeley
Hummer RA, Rogers RG, Nam CB, LeClere FB (1999) Race/ethnicity, nativity, and U.S. adult mortality. Soc Sci Quar 80:136–153. https://www.jstor.org/stable/48728438
Williams DR, González HM, Neighbors H, Nesse R, Abelson JM, Sweetman J, Jackson JS (2007) Prevalence and distribution of major depressive disorder in African americans, Caribbean Blacks, and non-hispanic whites: results from the National Survey of American Life. Arch Gen Psychiatry 64:305–315. https://doi.org/10.1001/archpsyc.64.3.305
Radey M (2018) Informal support among low-income mothers post welfare reform: a systematic review. J Child Fam Stud 27:3782–3805. https://doi.org/10.1007/s10826-018-1223-0
McCloskey RJ, Pei F (2019) The role of parenting stress in mediating the relationship between neighborhood social cohesion and depression and anxiety among mothers of young children in fragile families. J Community Psychol 47:869–881. https://doi.org/10.1002/jcop.22160
World Health Organization Social determinants of mental health. https://apps.who.int/iris/bitstream/handle/10665/112828/9789241506809_eng.pdf
World Health Organization. Social determinants of health. Geneva: World Health Organization (2020) https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1
Flores M, Ruiz JM, Goans C, Butler EA, Uchino BN, Hirai M, Tinajero R, Smith TW (2020) Racial-ethnic differences in social networks and perceived support: measurement considerations and implications for disparities research. Cultur Divers Ethnic Minor Psychol 26:189–199. https://doi.org/10.1037/cdp0000283
Uchino BN (2009) Understanding the links between social support and physical health: a life-span perspective with emphasis on the separability of perceived and received support. Perspect Psychol Sci 4:236–255. https://doi.org/10.1111/j.1745-6924.2009.01122.x
Franco LM, Pottick JK, Huang C-C (2010) Early parenthood in a community context: neighborhood conditions, race-ethnicity, and parenting stress. J Community Psychol 38:574–590. https://doi.org/10.1002/jcop.20382
National Academies of Sciences, Engineering, and, Medicine (2019) A Roadmap to reducing child poverty. National Academies, Washington, DC. https://doi.org/10.17226/25246
Sarkisian N, Gerstel N (2004) Kin support among blacks and whites: race and family organization. Am Sociol Rev 69:812–837
Sarkisian N, Gerena M, Gerstel N (2007) Extended family integration among Euro and Mexican americans: ethnicity, gender, and class. J Marriage Family 69:40–54
Spencer RA, Lemon ED, Komro KA, Livingston MD, Woods-Jaeger B (2022) Women’s lived experiences with Temporary Assistance for needy families (TANF): how TANF can better support women’s wellbeing and reduce intimate Partner violence. Int J Environ Res Public Health 19(3):1170
Mazelis JM, Mykyta L (2020) I might stay to myself: activation and avoidance of assistance from kin. J Marriage Fam 82:1479–1494. https://doi.org/10.1111/jomf.12680
Williams DR (2018) Stress and the mental health of populations of color: advancing our understanding of race-related stressors. J Health Soc Beh 59:466–485. https://doi.org/10.1177/0022146518814251
Williams DR, Priest N, Anderson NB (2016) Understanding associations among race, socioeconomic status, and health: patterns and prospects. Health Psychol 35:407–411. https://doi.org/10.1037/hea0000242
U.S. Census Bureau. Inequalities persist despite decline in poverty for all major race and Hispanic origin groups. (2020) https://www.census.gov/library/stories/2020/09/poverty-rates-for-blacks-and-hispanics-reached-historic-lows-in-2019.html
American Immigration Council. Immigrants in the United States (2021) https://www.americanimmigrationcouncil.org/research/immigrants-in-the-united-states
U.S. Department of Labor (2022) Foreign-born workers: labor force characteristics 2021. USDL-23-1013. https://www.bls.gov/news.release/pdf/forbrn.pdf
Plant EA, Sachs-Ericsson N (2004) Racial and ethnic differences in depression: the roles of social support and meeting basic needs. J Consul Clin Psychol 72:41–52. https://doi.org/10.1037/0022-006X.72.1.41
Silva M, Loureiro A, Cardoso G (2016) Social determinants of mental health: a review of the evidence. Eur J Psychiatry 30:259–292. https://psycnet.apa.org/record/2017-05809-003
Gavin AR, Walton E, Chae DH, Alegria M, Jackson JS, Takeuchi D (2009) The associations between socioeconomic status and major depressive disorder among blacks, latinos, asians, and non-hispanic whites: findings from the Collaborative Psychiatric Epidemiology Studies. Psychol Med 40:51–61. https://doi.org/10.1017/S0033291709006023
McGovern ME, Rokicki S, Von Jaglinsky A, Reichman NE (2023) Neighborhood-level housing affordability and maternal depression. SSM Ment Health 3:100192. https://doi.org/10.1016/j.ssmmh.2023.100192
Amutah-Onukagha NN, Doamekpor LA, Gardner M (2017) An examination of the sociodemographic and health determinants of major depressive disorder among black women. J Racial Ethn Health Disparities 4:1074–1082. https://doi.org/10.1007/s40615-016-0312
Herd D, Grube J (1996) Black identity and drinking in the US: a national study. Addiction 91:845–857. https://doi.org/10.1046/j.1360-0443.1996.91684510.x
Lee KH, Hines LD (2014) Racial disparity: substance dependency and psychological health problems among welfare recipients. Soc Work Public Health 29:207–219. https://doi.org/10.1080/19371918.2013.776322
Cook JA, Mock LO, Jonikas JA, Burke-Miller JK, Carter TM, Taylor A, Petersen CA, Gre DD, Gruenenfelder D (2009) Prevalence of psychiatric and substance use disorders among single mothers nearing lifetime welfare eligibility limits. Arch Gen Psychiatry 66:249–258. https://doi.org/10.1001/archgenpsychiatry.2008.539
Rosen D, Tolman RM, Warner LA (2004) Low-income women’s use of substance abuse and mental health services. J Health Care Poor Underserved 15:206–219. https://doi.org/10.1353/hpu.2004.0028
Office of the Surgeon General (U.S.), Center for Mental Health Services (U.S.), & National Institute of Mental Health (U.S.). Mental health: culture, race, and ethnicity: a supplement to mental health: A report of the Surgeon General (2001) https://pubmed.ncbi.nlm.nih.gov/20669516/
David R (2002) Racial/ethnic variations in women’s health: the social embeddedness of health. Am J Public Health 92:588–597. https://ajph.aphapublications.org/doi/full/https://doi.org/10.2105/AJPH.92.4.588
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed (2013) https://doi.org/10.1176/appi.books.9780890425596
Reichman NE, Teitler JO, Garfinkel I, McLanahan SS (2001) Fragile families: sample and design. Childr Youth Ser Rev 23. https://doi.org/10.1016/S0190-7409(01)00141-4. :303 – 26
Cauthen NK, Fass S (2008) Measuring income and poverty in the United States. New York: National Center for Children in Poverty, Columbia University, Mailman School of Public Health. http://www.nccp.org/publications/pub_825.html
Meadows SO, McLanahan SS, Brooks-Gunn J (2008) Stability and change in family structure and maternal health trajectories. Am Sociol Rev 73:314–334. https://doi.org/10.1177/000312240807300207
Umberson D, Williams K, Anderson K (2002) Violent behavior: a measure of emotional upset? J Health Soc Beh 43:189–206. https://www.jstor.org/stable/3090196
Kessler RC, Andrews G, Mroczek D, Ustun B, Wittchen H-U (1998) The World Health Organization composite international diagnostic interview short-form (CIDI‐SF). Int J Methods Psychiatr Res 7:171–185. https://doi.org/10.1002/mpr.47
Reid KM, Taylor MG (2015) Social support, stress, and maternal postpartum depression: a comparison of supportive relationships. Soc Sci Res 54:246–262. https://doi.org/10.1016/j.ssresearch.2015.08.009
Wilmot NA, Dauner KN (2016) Examination of the influence of social capital on depression in fragile families. J Epidemiol Community Health 71:296–302. https://www.jstor.org/stable/44363652
Boyd RC, Joe S, Michalopoulos L, Davis E, Jackson JS (2011) Prevalence of mood disorders and service use among US mothers by race and ethnicity: results from the National Survey of American Life. J Clin Psychiatry 72:1538–1545. https://doi.org/10.4088/JCP.10m06468
Holahan CJ, Moos RH, Holahan CK, Cronkite RC, Randall PK (2004) Unipolar depression, life context vulnerabilities, and drinking to cope. J Consul Clin Psychol 72:269–275. https://doi.org/10.1037/0022-006X.72.2.269
Mossakowski KN (2003) Coping with perceived discrimination: does ethnic identity protect mental health? J Health Soc Beh 44:318–331. https://doi.org/10.2307/1519782
Nelson MK (2002) The challenge of self-sufficiency: women on welfare redefining independence. J Contemp Ethnogr 31:582–614. https://doi.org/10.1177/089124102236543
Offer S (2012) The burden of reciprocity: processes of exclusion and withdrawal from personal networks among low-income families. Curr Sociol 60:788–805. https://doi.org/10.1177/0011392112454754
Williams DR, Sternthal M (2010) Understanding racial-ethnic disparities in health: sociological contributions. J Health Soc Beh 51:S15–S27. https://doi.org/10.1177/0022146510383838
Williams DR, Mohammed SA (2009) Discrimination and racial disparities in health: evidence and needed research. J Behav Med. ;3220–47. doi: 10.1007/s10865-008-9185-0 Williams DR, Jackson PB. Social sources of racial disparities in health. Health Aff. 2005;24:325–34. https://doi.org/10.1377/hlthaff.24.2.325
Williams DR (2018) Stress and the mental health of populations of color: advancing our understanding of race-related stressors. J Health Soc Behav 59:466–485. https://doi.org/10.1177/0022146518814251
Hussong AM, Jones DJ, Stein GL, Baucom DH, Boeding S (2008) An internalizing pathway to substance use: linkages between parenting, emotion regulation, and internalizing symptoms. J Adolesc 31(5):615–635
Substance Abuse and Mental Health Services Administration (2019) Key substance use and mental health indicators in the United States: Results from the 2018 National Survey on Drug Use and Health
Funding
This work was supported by a grant from the Health Resources and Services Administration (HRSA) R42 1R42MC45809-01‐00. In addition, Dr. Eugenia Flores Millender has received research support from the National Heart, Lung, and Blood Institute grant number: 2L30HL154217-02.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation was performed by Drs. EFM, MR and CS. The analysis was performed by Dr.MR. All authors contributed to the first draft of the manuscript and commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Ethics Approval
The Institutional Review Board of Florida State University granted approval to conduct this study.
Consent to Participate
Informed consent was obtained from all individual participants included in the parent study. This study is a secondary data analysis using de-identified data.
Consent to Publish
The authors affirm that human research participants provided informed consent for publication.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Millender, E.F., Radey, M., Sabuncu, B.C. et al. Exploring the Interplay of Social Safety Nets, Race, Ethnicity, and Nativity on Psychological Distress Among Low-Income Mothers. Child Psychiatry Hum Dev (2024). https://doi.org/10.1007/s10578-024-01744-9
Accepted:
Published:
DOI: https://doi.org/10.1007/s10578-024-01744-9