Abstract
There is a high prevalence of untreated depression in adults and youth observed at the population level in the United States, and many who would benefit from treatment do not receive it. One proposed effort to increase access to care is the use of measurement-based care (MBC; repeated use of symptom measures for screening and treatment guidance) by primary care physicians to treat non-complex cases of depression. MBC has been shown to improve patient outcomes compared to care as usual, but there are barriers that need to be addressed at the health system level for effective implementation to occur. Herein we provide an overview of MBC and detail benefits and barriers of MBC implementation. Relevant considerations and guidance for implementing MBC are presented, and a case example of a health system implementing MBC is included. Though issues of reimbursement, limited human and technological resources, and resistance to systemic change are barriers to implementing MBC, effective strategies exist to overcome these barriers. In addition to helping health systems align with changes to value-based care models, effective implementation of MBC can likely improve patient outcomes and result in net financial benefits.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The health care system in the United States (U.S.) is a complex network that includes hospitals and health care facilities as well as other actors such as insurance providers, employers, and purchasers of health care services. These elements operate in a variety of configurations that are both public and private, for-profit and not-for-profit, and as state and governmental entities. Though commonly referred to as a system, implying well-ordered and coordinated efforts, the U.S. health care system often lacks communication, collaboration, or systems planning [25]. In addition, the U.S. health care delivery system is among the costliest in the developed world; according to the American Medical Association, health care spending accounts for over 18% of the United States Gross Domestic Product, a much higher proportion than for other high-income nations [4, 22]. In 2021, on average, the U.S. spent $12,914 per capita on health care [4]. Despite this high rate of spending, the U.S. has a lower life expectancy, the highest maternal and infant mortality rates, and some of the highest rates of death and complications from chronic medical conditions among high-income nations [22].
In contrast to the resources and attention expended on medical care in the U.S., mental health care is deprioritized and underfunded [36]. According to the National Institute for Health Care Management, several barriers to mental health care remain unaddressed, including an undersized mental health workforce, insufficient finances to cover costs, and no or limited insurance coverage for care [36]. Yet the prevalence of mental illness in the United States is higher than in other high-income countries [20, 45]. Over 50 million (21%) adults living in the U.S. experienced a mental illness in 2020. In the same year, 1 in 4 adults reported an unmet need for their mental health treatment, and over half of adults (27 million) with mental illness did not receive treatment [36]. Mental illness among youth is highly prevalent in the U.S. as well, with approximately 33% of children between the ages of 3–17 diagnosed with a mental illness [11]. The CDC estimates that mental illnesses among children result in an annual cost of $247 billion due to their impact not only on children, but on families and communities [11]. Depression is one of the most common psychiatric illnesses in the United States, impacting children, adolescents, and adults [42] and is not only burdensome, but also a costly illness when it comes to medical care and impacts of diseases such as loss of productivity [8, 42].
In addition, individuals with chronic medical conditions (e.g., cancer, diabetes, heart disease, etc.) are at increased risk for depression, and likewise depression is a risk factor for chronic illness [10, 52]. When depression is co-occurring with chronic disease, outcomes for both conditions are poor. Individuals with depression and co-occurring medical conditions have a decreased recovery and prolonged course of illness compared to those without depression [10]. [18],). Risk of all-cause mortality is nearly doubled in those with depression [51].
Given the correlation between physical and mental health outcomes, and the costs associated with under treatment of mental illness, it is imperative that our health care systems devote adequate resources to the treatment of both mental and physical health conditions. By addressing both aspects of health simultaneously and comprehensively, health systems can achieve the goal of improving patient outcomes and patient experiences while decreasing overall costs—goals consistent with the national health care system strategy and with the Triple Aim [37].
One of the challenges health systems face in treating depression is that many non-mental health medical providers do not feel equipped to treat depression, often due to insufficient training and lack of resources [1]. However, research indicates that non-mental health providers can achieve similar patient remission rates when treating depression as can specialty mental health providers [19, 47]. Furthermore, according to the APA and the APM, including mental health services in primary care settings reduces stigma and increases care access [6]. One key strategy for improved patient outcomes in primary care settings is utilizing measurement-based care (MBC) for depression assessment and treatment.
MBC in the field of psychiatry is defined as “systematically using measurement tools to monitor progress and guide treatment choices” [46], as well as “the routine measurement of symptoms and side effects using validated clinical measurement instruments at each treatment visit to objectify the assessment, tolerability, functioning, and quality of life in patients with psychiatric disorders” [1]. One of the strengths of using MBC for the identification and treatment of mental illness is the ability to scale efforts based on health care setting resources and infrastructure. MBC can be delivered on a continuum, from simple questionnaires to the collaborative care model (CoCM; [49]). Although MBC specifically refers to use of measurement to inform treatment decisions, any degree of measurement is likely beneficial to both clinician and patient. For example, in settings with limited personnel resources, self-report measures such as the 2-item and 9-item Patient Health Questionnaires (PHQ-2 and PHQ-9, Sptizer, Kroenke, and Williams, 1999), Generalized Anxiety Disorder scale (GAD 7; [44]), and other self-report measures can provide a quick overview of a patient’s mental health. These measurements serve as efficient starting points for clinical review, especially in primary care settings, and allow for the use of true MBC [29].
MBC is not a new concept; in fact, it is widely used in most health care settings, including primary care settings, for management of a variety of non-depression chronic conditions. Common examples of MBC are the collection of patient vitals such as temperature, weight, blood pressure, respiration rate, and routine blood and urine lab work. Absent from these essential and routine health assessments are measurements used to assess mental health. However, self-report screenings for common mental illnesses such as depression, anxiety, and other mood disorders can be incorporated into routine care to provide whole person care [24, 42]. Given the prevalence of depression across the lifespan, screening and MBC for this common disorder is critical.
This article will describe initial considerations of MBC methods and the benefits and barriers to widespread implementation of MBC from a health system perspective. Additionally, we will describe steps for successful implementation, as well as provide specific examples from one health system that has implemented MBC, the challenges they encountered, and strategies to address potential obstacles.
Considerations for MBC Methods
Measurements for the assessment of mental health should include assessment of symptom severity, any impairment in functioning, adherence to treatments, and any adverse effects associated with treatment [34]. At all levels of MBC implementation, measures could be collected either as paper or electronic surveys provided at the time of the visit or electronic surveys given prior to the visit. Either approach should allow the clinician to review the surveys during the visit to inform assessment and guide treatment decisions. MBC provides more objective data to the clinician deciding whether to recommend a new treatment, to change a current treatment, or to refer the patient to specialty care.
Health systems have options in scaling MBC and tailoring implementation based on their resources and infrastructure. Implementation can range from using pen and paper surveys only during the time of appointment to sophisticated use of existing electronic health record features or other software that not only provide data but also help interpret that data to guide treatment decisions and track treatment response over time.
Benefits of MBC for Health Systems
Earlier Identification and Treatment of Depression in Patients
People begin experiencing depression symptoms on average 5 years before receiving a diagnosis [43]. Routine use of MBC can help identify these symptoms and alleviate suffering long before a patient may have normally reported depressive symptoms to their clinician. Any setting that is a medical home for patients, where that patient will be seen recurrently over time, is an ideal setting to implement MBC for early identification of depression. The primary care setting is a clear example of this, specialist settings involved in long-term disease management may also work well. In today’s healthcare landscape, many community providers are either affiliated with or members of larger health system networks. As such, the practices and policies within the health care setting are often set by the larger system. When whole health systems adopt MBC practices the impact to the health and wellbeing of the community is amplified quickly. More patients with mild to moderate depression are identified earlier on and provided the opportunity for education, prevention, and intervention strategies to minimize future crises and therefore need for crisis intervention. Early identification and treatment reduce the pain and suffering of patients and their families, leads to better treatment outcomes, and may reduce the risk of developing treatment-resistant depression [31].
Improved Patient Outcomes
Without measurement it can be difficult to accurately assess treatment effectiveness [27]. Using MBC at each step during treatment provides clinicians with ongoing data points to track patient progress. By actively monitoring symptoms, MBC can help guide clinicians in treatment adjustments and identify problematic adverse effects of treatment that may impact treatment adherence. Meta-analyses and reviews have consistently found that MBC improves patient outcomes compared to care as usual [16]. Past work implementing MBC into health care systems via quality improvement projects have identified improved remission rates using MBC compared to. usual care [24, 42].
MBC implemented in primary care also reduces stigma and increases access to care (American Psychiatric Association & American of Psychosomatic Medicine, 2016). MBC is patient-centered and allows patients to fully participate in their own care. When patients use self-report measures and work with clinicians to guide treatment based on measurement, they increase their knowledge about their condition and keep track of their progress; this may aid in identifying worrisome symptoms that might be indicative of relapse. MBC optimizes efficiency and accuracy of symptom management resulting in increased patient satisfaction and health system performance [16].
MBC Facilitates Data Collection
In addition to improving patient outcomes, data collected as part of MBC can additionally be leveraged by systems for a variety of secondary purposes such as program evaluations, reporting requirements, and quality improvement initiatives. The Affordable Care Act (ACA) requires health systems to report population health metrics [37]. To comply with new value-based federal guidelines, health systems are engaging in practice-based population health. Collecting and reviewing health information across a population is necessary for health care leaders to gain insight to employ the most effective strategies that meet the needs of the population they serve [27]. Using MBC for depression treatment creates measurable and quantifiable outcomes to evaluate the effectiveness of a particular care strategy. A lack of standardized symptom measurement for depressive disorders makes evaluating population wide outcome data difficult. Reviewing MBC data in aggregate allows for the evaluation of health system level patient outcomes. Furthermore, outcomes are reported to federal agencies like Centers for Medicare and Medicaid Services’ Quality Payment Program and Merit-Based Incentive Payment Systems (MIPS) to ensure patients are receiving quality care. A consequence of MBC is the creation of real time data that can be used by health systems for both reporting and implementation efforts. These performance indicators can be used to iteratively revise and refine processes. Collecting population health data allows health system administrators to demonstrate treatment effectiveness which can be used for payment reporting, especially as it relates to benchmarks used in value-based care and Alternative Payment Models (APM) used by the Centers for Medicare and Medicaid Services [50]. Population level data regarding treatment effectiveness can also be used to negotiate value-based contracts with health insurance companies.
Cost Savings and Reimbursements
Adoption of MBC leads to cost savings in several ways, especially within primary care settings. Frequent and routine screening, a mandatory component of MBC, catches troublesome medical conditions early, lessening the likelihood of uncontrolled symptoms. When health systems adopt universal depression screening as part of routine care, they identify patients with mild to moderate depression early on and engage them in treatments that are less costly and more readily available; this likely leads to reduced symptom burden and better health outcomes, reducing the need for more expensive specialist care and in-patient hospitalizations [15, 31].
Health systems can now submit annual depression screenings for reimbursement. Annual depression screening is also covered by Medicare Part B. Beginning in 2014, the Medicare Access and CHIP Reauthorization Act (MACRA) became law and enables the Centers for Medicare and Medicaid Services to reimburse clinicians on performance metrics including those related to prevention and patient outcomes [35]. While ongoing (more than annual) measurement of depression may not be covered by insurance (and thus MBC may not, as regular screening is necessary component of MBC), the Collaborative Care Model, which includes MBC, does allow for additional billing codes that can be used for reimbursement.
Barriers to Implementing MBC
Implementing new system-wide programs is challenging. Although MBC is widely used in medical practice, implementing MBC for mental health requires a paradigm shift for health systems and health care workers. Barriers to MBC can be divided into four categories: system-level, organizational-level, provider-level, and patient-level [28, 29].
System-Level and Organization-Level Barriers
System-level and organization-level barriers include change fatigue, inadequate reimbursement, and lack of EHR integration. The health care delivery system in the US continues to undergo rapid change driven by the shift from fee-for-service delivery to value-based care. This shift is transforming every aspect of health care delivery from patient documentation to medical billing and the changes are coming rapidly in succession with little time to absorb new processes before the next one is introduced; this has been particularly relevant in the post COVID-19 pandemic healthcare landscape [33]. Health care workers are reporting increased levels of stress, burnout, and low levels of job satisfaction related to the pace of change in the healthcare workplace [32]. For successful implementation, stakeholders at every level, from the CEO to the medical assistant, will need to invest in championing MBC. The rapid changes in health care not only impact how clinical care is delivered, but also how health systems are reimbursed. Ongoing mental health screening is generally not adequately reimbursed, and, when it is, reimbursement often does not accurately reflect physician time spent. Without additional time, staff or sufficient reimbursement, clinicians struggle to address multiple patient concerns or health problems in one visit or to assess non-disclosed symptoms that are contributing to the presenting symptoms such as depressive symptoms.
Unlike other medical conditions, mental health care and treatment has not been fully integrated in (EHRs). Without health information technologies documenting screenings, tracking of patient progress is done manually, often in text fields that are not easily searchable or quantifiable [30]. Further, screening instruments are often scanned into patient records and considerable effort is required to extract information to assess patient, practice, and system progress. Lack of EHR integration can be a barrier due to time constraints, especially in clinics that are Relative Value Units (RVU) driven. Investing in upfront costs to modify and automate electronic health records (EHRs) to prompt clinical staff to complete mental health screenings, capture and track patient screening scores, provide clinical decision support, and to create patient registries and reports, ultimately provides cost savings to the health system [2, 34].
Provider-Level Barriers
Important provider-level barriers to implementing MBC are insufficient training in mental health assessment and treatments, adequate reimbursements, and time and focus of visits. A key reason providers cite for the slow adoption of MBC for depression care is the lack of brief, concise training for non-specialist medical providers on mental and behavioral health care topics. The misconception that depression care is too complex for those outside the field of psychiatry and other mental health specialist fields continues to persist. However, just as primary care doctors do not need to have extensive training in cardiology to treat common high blood pressure symptoms, primary care doctors do not need extensive training in psychiatry to treat depression and depressive symptoms, and, indeed, treatment outcomes for depression appear to be similar between specialist and non-specialist providers [19, 47]. Providers can obtain relatively brief training and guidance in diagnosis and treatment recommendations for depression through a variety of clinical practice guidelines and continuing education programs from professional associations like the American Psychological Association [5] and the American Psychiatric Association [7, 21]. Importantly, guidelines inform primary care providers on when to refer their patients to a mental health specialist, which is typically when the patient has failed two or more depression treatments or when the patient is experiencing severe suicidal ideation with plans and intent.
Providers, as with systems and organizations, are also impacted by the need to obtain sufficient reimbursements. Often, providers are required to meet specified RVUs monthly, which may necessitate them conducting more visits in shorter periods of time. Addressing multiple patient concerns in a single visit takes more time than typically allotted for uncomplicated conditions or interventions.
Similarly, if depression (or another mental health concern) is not the primary focus of the visit, time-pressure may make addressing mental health concerns a challenge. In a typical visit, PCPs may address multiple patient health needs in order of priority [38]. Unfortunately, unless a patient is presenting acute depressive symptoms, mental health assessments are often not considered a priority despite research that shows the benefits of addressing mental health as part of disease management [38]. Providers may be concerned that assessing for depression will lead to insufficient time to handle the mental health concerns that come up, while also addressing other medical issues; furthermore, mental health concerns may also be considered by some providers to be outside their area of expertise. In many cases, PCPs will refer their patients to behavioral specialists to address their mental health concerns before attempting to manage their care in practice.
Many of the above barriers relate more to the treatment of depression in primary care settings than to the implementation of MBC specifically. Of note, a key benefit of using MBC in these settings is that the objective nature of the measured outcomes may increase provider confidence in treating patients with depression. Indeed, some MBC “platforms” or integrated MBC-EHR systems may also provide algorithmic guidance for treatment selection and other treatment decision support, which may further reduce barriers for non-specialist clinicians [47].
Patient-Level Barriers
Stigma has been shown to negatively influence help-seeking behavior for mental health concerns [13]. While universal depression screening as part of MBC may engage individuals who would otherwise not seek out care, stigma could result in patients refusing to complete measures or under reporting symptoms of depression [9], Hunt, Auriemma, and Cashaw, 2010). Relatedly, low mental health literacy may be associated with a reduced likelihood of recognizing symptoms as related to a mental illness and a reluctance to undergo traditional medical treatments for depression (Furnham and Swami, 2020). Thus, providers may need to focus concurrently on education for patients that may be reluctant to engage with treatment; culturally adapted education programs have been found to be effective in promoting treatment use and reducing stigma [39].
Like providers, patients also have the barrier of the time and focus of their visit. Often, patients schedule visits with their provider to discuss specific concerns. Thus, when they are being seen, their focus is on the medical concern at hand, leaving any concerns about depression unmentioned. By regularly obtaining depression measures over time and reviewing these self-reports at the beginning of the visit, providers can address depression concerns with their patients directly.
There are important practical considerations to the implementation of self-report measures into clinical care. Limited English fluency in patients will limit their ability to complete English language versions of measures; for this reason, health systems may need to select measures that have been translated and validated in other languages. The PHQ-9, for example, has been validated in a variety of languages including Spanish [14] and Chinese [53]. Those with physical disabilities or low literacy may require assistance in completing the measures,given privacy concerns this may prevent completion of measures in practice waiting rooms, potentially disrupting workflows. Individuals with intellectual disabilities may have difficulty adequately completing self-report measures. Health systems will therefore need to decide how they will gather the relevant data from these patients (for a summary of important considerations of the use of self-report vs. proxy-report measures in those with intellectual disability, please see [40]).
Steps for Integration into Health Systems
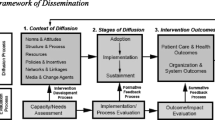
Although implementing MBC into primary care settings is a proven and effective model to increase access to care, there is not a “one size fits all” solution for accomplishing this. Implementation must be tailored to each health care setting based on available resources and infrastructure. There are several key factors that increase the likelihood of successful MBC implementation. Creating a competent and qualified team is imperative, with expertise in project management, health care delivery, clinical integration, and mental health care. Additionally, the goals of the project must be clearly defined and outlined at the onset. Use of common health care setting quality improvement frameworks, such as Plan-Study-Do-Act, will likely benefit MBC implementation [3]. Ensuring that the project team includes experts is crucial to establishing creditably to secure stakeholder buy-in at every level. Key aspects of successful implementation at the health system level include (1) establishing buy-in, (2) identifying method of MBC to implement; (3) evaluating workflows; (4) providing training for all providers and staff and: (5) continuous quality improvement. See Fig. 1 for a summary of each aspect. More detailed information is given below for how an implementation project may consider each aspect.
Establishing Buy-In
Project leadership must tailor informational and persuasive content to diverse audiences and aim to achieve organizational buy-in at a variety of levels, from executives and administrators to frontline care workers and office staff. Developing shared goals, clear expectations, and defined roles and responsibilities are fundamental to this process. Health care administrators are likely to focus on the upfront costs of implementation as well as the return on investment. Buy-in from PCPs greatly impacts the success of any quality improvement project at the clinic implementation level. Useful strategies to get PCP buy-in include evidence demonstrating improved patient outcomes using MBC and emphasizing how poor mental health is a significant barrier to maintaining overall health [10, 52]. Clinic support staff are likely not interested in the costs associated with care, instead their buy-in discussion includes details on workload and workflow.
Identifying Method of MBC to Implement/Evaluating Readiness
Identifying an appropriate MBC implementation method depends on several factors: infrastructure and resources, personnel, and clinic readiness. Universal screening is the foundation that is built upon for all models of MBC and is defined as screening every patient at every visit. Building on the foundational elements of MBC, Integrated Behavioral Health and the Collaborative Care Model are more extensive approaches involving mental health providers working in collaboration with primary care providers [49]. Implementation of Integrated Behavioral Health and Collaborative Care are likely to require more significant upfront costs, and so may encounter more organizational barriers to implementation.
Evaluate Workflows
Regardless of the kind of MBC system adopted in health care settings, workflows will require revision and refinement to incorporate MBC techniques. Workflows should be tailored to the selected MBC method, instrument(s) selected, and clinical setting. There are some commonalities related to workflows; useful questions to address for modifying workflows include, but are not limited to, the following:
-
Which patients will be screened and when (e.g., all visits, annual screens, or sick visits)?
-
What are the parameters for re-screening those with a prior negative depression screen?
-
When and where in the patient visit will measurements be given? Some clinics may opt to utilize pre-visit screenings that are sent to patients prior to their appointment and imported into the EHR. Other clinics may incorporate depression measures in the registration process, opting for patients to complete screenings in clinic using tablets, their mobile device, or paper forms.
-
What is the process when someone screens positive? Answers to this will also depend on which method of MBC is implemented and the severity of the positive screen. As part of MBC implementation, developing a depression screening protocol is useful.
-
For those who are given treatment recommendations, will treatment be provided in the clinic setting or will a referral for care be given, and what are the follow-up procedures (e.g. timing of follow-up, follow-up measures, after-care visits, etc.)?
Training for All Providers and Staff
After clinical settings determine workflows, tailored trainings are developed and initiated. There are some MBC training requirements that are universal. All settings will need a general overview of depression and other common mental health conditions. An overview of MBC, its correlation to better patient outcomes, and details about its implementation and goals will also be vital. Specific focus should be paid to strategies for using self-report depression severity scores, noted side effects, and information on medication compliance to inform and modify treatment. Trainings specific to individual settings include: selected screening instruments, common medications used to treat depression, and common non-medication treatment options, as well as treatment phases and recommendations for follow-up visits. More specialized training may be warranted depending on the degree of MBC implementation.
Determining How to Implement
It will be important to identify internal resources (individuals, department, budgets, technologies) early, and to integrate them into decision making. For clinics that opt for electronic capture of screenings, additional personnel will be required to modify EHRs so that providers can access the screening results. Most large health systems use EHRs that have these features embedded, however modifying the EHR to capture screenings, provide clinical decision support, and populate billing codes requires expertise and dedicated staff.
Continuous Quality Improvement
The final stages of implementation include piloting MBC on a small scale and using continuous quality improvement cycles. Focusing on slow and incremental implementation regardless of the MBC model is recommended to ensure that solid foundational processes are established. Once efficient workflows are developed, frequent and on-going check-ins are recommended to continue to maintain buy-in, engagement, and support throughout the project period. The ultimate goal is for the project to become practice and that MBC is integrated into clinical care.
Implementing MBC in Real Treatment Settings
To illustrate the process of implementing MBC, an example of a large health system experience is detailed below:
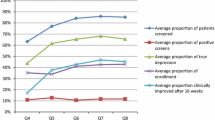
The Health System is an academic medical center serving a rural, medically underserved patient population. As this health system was initially evaluating the need for MBC implementation, several meetings were held with system leadership to get system-wide buy-in and to determine best methods for integrating MBC across the entire system. The health system implemented universal depression screening along with a proprietary clinical decision support system called VitalSign6. VitalSign6 is a software that facilitates MBC and incorporates many of the components of successful MBC implementation [47]. This software was developed based on the idea that the management of depression is comparable to the management of other chronic illnesses, like diabetes, in that regular screening and assessment is useful for identifying patients in need of care and for tailoring treatment over time. For this health system, VitalSigns6 serves not only as the MBC system, but also a patient registry and a means to determine population or clinic level performance. The software, which calculates self-reported scores for providers allowing for easy review, suggested treatment plans, and pre-determined recommended follow-up schedules, was integrated in the health system’s EHR to make access to symptom scores and decision support tools easier for providers. MBC was implemented into 12 clinics including 4 primary clinics, 4 pediatric clinics, 3 psychiatric clinics and a clinic that serves the needs of university students. Providers received training on assessment, MBC concepts, and treatment for depression. Providers and staff were also trained on the VitalSign6 application. At the time of this writing, 16,500 patients have been screened since implementation; approximately 24% of patients screened positive, and 5% were diagnosed with a depressive disorder. Since launching the program, ongoing adjustments to workflows and the MBC software have been made to improve functionality for providers, which is a key step in successful implementation and maintenance of MBC in clinics and large health care systems.
Future Directions
Though barriers to implementation of MBC are real, benefits at the health system, provider, and patient levels warrant its continued adoption. As such, initiatives have formed to promote the use of MBC; one such initiative is the Texas Youth Depression and Suicide Research Network (TX-YDSRN). TX-YDSRN is a collaboration of the large health related universities in Texas; it was created with a mandate to assess the status of youth mental health and to promote the use of MBC for treatment of mental illness within the state [41, 48]. The initiative has worked to implement MBC processes in psychiatric (and affiliated primary care) clinics associated with the universities that constitute the network. Efforts continue to expand adoption of MBC within new partner clinics, and throughout the state.
Summary
In the U.S., nearly 1 in 5 U.S. adults experience a mental illness each year [12]. Unfortunately, less than half of those in need receive care due to a variety of reasons including lack or limited insurance coverage for mental health, lengthy wait times to see mental health providers, and the stigma and lack of education associated with mental illness. Implementation of MBC for depression, particularly in primary care settings, represents one promising solution to address these barriers to access of care. Though real barriers exist to the implementation of MBC at the health system level, effective strategies exist for overcoming them. As the U.S. health care system continues to move towards value-based reimbursement models, implementation of MBC may provide one way for health systems to demonstrate they are achieving the desired results.
Data Availability
Not applicable.
References
Aboraya A, Nasrallah HA, Elswick DE, Ahmed E, Estephan N, Aboraya D, Berzingi S, Chumbers J, Berzingi S, Justice J, Zafar J, Dohar S (2018) Measurement-based care in psychiatry-past, present, and future. Innov Clin Neurosci 15(11–12):13–26
Abright AR, Grudnikoff E (2020) Measurement-based care in the treatment of adolescent depression. Child Adolesc Psychiatr Clin N Am 29(4):631–643. https://doi.org/10.1016/j.chc.2020.06.003
Agency for Healthcare Research and Quality (2020) Plan-do-study-act (PDSA) directions and examples. Agency for Healthcare Research and Quality
American Medical Association (2023) Trends in health care spending. American Medical Association
American Psychiatric Association (2010) Learn about the collaborative care model. Psychiatry. https://www.psychiatry.org/psychiatrists/practice/professional-interests/integrated-care/learn
American Psychiatric Association, Academy of Psychosomatic Medicine (2016) Dissemination of integrated care within primary care settings: the collaborative care model. Psychiatry. https://www.psychiatry.org/File%20Library/Psychiatrists/Practice/Professional-Topics/Integrated-Care/APA-APM-Dissemination-Integrated-Care-Report.pdf
American Psychological Association (n.d.) Guidelines for practitioners. American Psychological Association. https://www.apa.org/practice/guidelines/
Baik SY, Crabtree BF, Gonzales JJ (2013) Primary care clinicians’ recognition and management of depression: a model of depression care in real-world primary care practice. J Gen Intern Med 28(11):1430–1439. https://doi.org/10.1007/s11606-013-2468-3
Bharadwaj P, Pai MM, Suziedelyte A (2017) Mental health stigma. Econ Lett 159:57–60
Celano CM, Villegas AC, Albanese AM, Gaggin HK, Huffman JC (2018) Depression and Anxiety in Heart Failure: A Review. Harv Rev Psychiatry 26(4):175–184. https://doi.org/10.1097/HRP.0000000000000162
Centers for Disease Control and Prevention (2022) Children’s Mental Health. Centers for Disease Control and Prevention
Centers for Disease Control and Prevention (2023) About mental health. Centers for Disease Control and Prevention
Clement S, Schauman O, Graham T, Maggioni F, Evans-Lacko S, Bezborodovs N, Morgan C, Rüsch N, Brown JSL, Thornicroft G (2015) What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol Med 45(1):11–27. https://doi.org/10.1017/S0033291714000129
Diez-Quevedo C, Rangil T, Sanchez-Planell L, Kroenke K, Spitzer RL (2001) Validation and utility of the patient health questionnaire in diagnosing mental disorders in 1003 general hospital Spanish inpatients. Psychosom Med 63(4):679–686
Fava M (2003) Diagnosis and definition of treatment-resistant depression. Biol Psychiat 53(8):649–659. https://doi.org/10.1016/s0006-3223(03)00231-2
Fortney JC, Unützer J, Wrenn G, Pyne JM, Smith GR, Schoenbaum M, Harbin HT (2017) A tipping point for measurement-based care. Psychiatr Serv 68(2):179–188. https://doi.org/10.1176/appi.ps.201500439
Furnham A, Swami V (2018) Mental health literacy: a review of what it is and why it matters. Int Perspect Psychol 7(4):240–257
Gallo JJ (2017) Multimorbidity and mental health. Am J Geriatr Psychiatry 25(5):520–521. https://doi.org/10.1016/j.jagp.2017.02.007
Gaynes BN, Rush AJ, Trivedi MH, Wisniewski SR, Spencer D, Fava M (2008) The STAR*D study: treating depression in the real world. Clevel Clin J Med 75(1):57–66. https://doi.org/10.3949/ccjm.75.1.57
GBD 2019 Mental Disorders Collaborators (2022) Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. The Lancet Psychiatry 9(2):137–150. https://doi.org/10.1016/S2215-0366(21)00395-3
Gelenberg AJ, Freeman MP, Markowitz JC, Rosenbaum JF, Thase ME, Trivedi MH, Van Rhoads RS (2010) American psychiatric association practice guidelines for the treatment of patients with major depressive disorder. Am J Psychiatry 167(Suppl 10):9–118
Gunja MZ, Gumas ED, Williams RD II (2023) U.S. health care from a Global Perspective, 2022: accelerating spending, worsening outcomes. Commonwealth Fund
Hunt M, Auriemma J, Cashaw ACA (2003) Self-report bias and underreporting of depression on the BDI-II. J Pers Assess 80(1):26–30. https://doi.org/10.1207/S15327752JPA8001_10
Jha MK, Grannemann BD, Trombello JM, Clark EW, Eidelman SL, Lawson T, Greer TL, Rush AJ, Trivedi MH (2019) A structured approach to detecting and treating depression in primary care: vitalsign6 project. Ann Fam Med 17(4):326–335. https://doi.org/10.1370/afm.2418
Institute of Medicine, Board on Health Promotion, Disease Prevention, & Committee on Assuring the Health of the Public in the 21st Century (2003) The Future of the Public’s Health in the 21st Century, 1st edn. National Academies Press
Katon W, Unützer J, Wells K, Jones L (2010) Collaborative depression care: history, evolution and ways to enhance dissemination and sustainability. Gen Hosp Psychiatry 32(5):456–464. https://doi.org/10.1016/j.genhosppsych.2010.04.001
Kilbourne AM, Beck K, Spaeth-Rublee B, Ramanuj P, O’Brien RW, Tomoyasu N, Pincus HA (2018) Measuring and improving the quality of mental health care: a global perspective. World Psychiatry 17(1):30–38. https://doi.org/10.1002/wps.20482
Krishna R, Jeffrey J, Patel PD (2020) Implementing measurement-based care in various practice settings. Child Adolesc Psychiatr Clin N Am 29(4):573–586. https://doi.org/10.1016/j.chc.2020.06.007
Lewis CC, Boyd M, Puspitasari A, Navarro E, Howard J, Kassab H, Hoffman M, Scott K, Lyon A, Douglas S, Simon G, Kroenke K (2018) Implementing measurement-based care in behavioral health: a review. JAMA Psychiat 76(3):324–335. https://doi.org/10.1001/jamapsychiatry.2018.3329
Mamykina L, Vawdrey DK, Stetson PD, Zheng K, Hripcsak G (2012) Clinical documentation: composition or synthesis? J Am Med Inform Assoc 19(6):1025–1031. https://doi.org/10.1136/amiajnl-2012-000901
Mayes TL, Deane AE, Aramburu H, Yagnik K, Trivedi MH (2023) Improving identification and treatment outcomes of treatment-resistant depression through measurement-based care. Psychiatr Clin North Am 46(2):227–245. https://doi.org/10.1016/j.psc.2023.02.002
McMillan K, Perron A (2020) Change fatigue in nurses: a qualitative study. J Adv Nurs 76(10):2627–2636. https://doi.org/10.1111/jan.14454
Moreno C, Wykes T, Galderisi S, Nordentoft M, Crossley N, Jones N, Cannon M, Correll CU, Byrne L, Carr S, Chen EYH, Gorwood P, Johnson S, Kärkkäinen H, Krystal JH, Lee J, Lieberman J, López-Jaramillo C, Männikkö M, Phillips MR, Arango C (2020) How mental health care should change as a consequence of the COVID-19 pandemic. The lancet. Psychiatry 7(9):813–824. https://doi.org/10.1016/S2215-0366(20)30307-2
Morris DW, Trivedi MH (2011) Measurement-based care for unipolar depression. Curr Psychiatry Rep 13(6):446–458. https://doi.org/10.1007/s11920-011-0237-8
National Committee for Quality Assurance (n.d.) Medicare Access and CHIP Reauthorization Act (MACRA). National Committee for Quality Assurance. https://www.ncqa.org/public-policy/macra/
National Institute for Health Care Management (2022) Prioritizing Mental Health Care in America. NIHCM
Patient Protection and Affordable Care Act of 2010, Pub. L. No. 111–148, 124 Stat. 119 (2010). https://www.congress.gov/111/plaws/publ148/PLAW-111publ148.pdf
Poghosyan L, Norful AA, Ghaffari A, George M, Chhabra S, Olfson M (2019) Mental health delivery in primary care: the perspectives of primary care providers. Arch Psychiatr Nurs 33(5):63–67. https://doi.org/10.1016/j.apnu.2019.08.001
Sanchez K, Killian MO, Eghaneyan BH, Cabassa LJ, Trivedi MH (2019) Culturally adapted depression education and engagement in treatment among Hispanics in primary care: outcomes from a pilot feasibility study. BMC Fam Pract 20(1):1–9
Scott HM, Havercamp SM (2018) Comparisons of self and proxy report on health-related factors in people with intellectual disability. J Appl Res Intellect Disabil: JARID 31(5):927–936. https://doi.org/10.1111/jar.12452
Slater H, AlZubi Y, Rezaeizadeh A, Hughes JL, Gorman A, Mayes TL, Elmore JS, Storch EA, Wakefield SM, Trivedi MH (2024) Characterizing measurement-based care in the texas youth depression and suicide research network (TX-YDSRN). Child Psychiatry Hum Dev. https://doi.org/10.1007/s10578-023-01653-3
Siniscalchi KA, Broome ME, Fish J, Ventimiglia J, Thompson J, Roy P, Pipes R, Trivedi M (2020) Depression screening and measurement-based care in primary care. J Prim Care Community Health 11:2150132720931261. https://doi.org/10.1177/2150132720931261
Solmi M, Radua J, Olivola M, Croce E, Soardo L, Salazar de Pablo G, Il Shin J, Kirkbride JB, Jones P, Kim JH, Kim JY, Carvalho AF, Seeman MV, Correll CU, Fusar-Poli P (2021) Age at onset of mental disorders worldwide: large-scale meta-analysis of 192 epidemiological studies. Mol Psychiatry. https://doi.org/10.1038/s41380-021-01161-7
Spitzer RL, Kroenke K, Williams JB, Löwe B (2006) A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 166(10):1092–1097
Tikkanen R, Fields K, Williams II RD, Abrams M K (2020) Mental health conditions and substance use: comparing U.S. needs and treatment capacity with those in other high-income countries. The Commonwealth Fund. https://www.commonwealthfund.org/sites/default/files/2020-05/Tikkanen_mental_hlt_intl_comparison_db.pdf
Trivedi MH (2009) Tools and strategies for ongoing assessment of depression: a measurement-based approach to remission. J Clin Psychiatry 70(6):26–31. https://doi.org/10.4088/JCP.8133su1c.04
Trivedi MH, Jha MK, Kahalnik F, Pipes R, Levinson S, Lawson T, Rush AJ, Trombello JM, Grannemann B, Tovian C, Kinney R, Clark EW, Greer TL (2019) VitalSign6: a primary care first (PCP-First) model for universal screening and measurement-based care for depression. Pharmaceuticals (Basel, Switzerland) 12(2):71. https://doi.org/10.3390/ph12020071
Trivedi MH, Minhajuddin A, Slater H, Baronia R, Blader JC, Blood J, Brown R, Claassen C, DeFilippis M, Farmer D, Garza C, Hughes JL, Kennard BD, Liberzon I, Martin S, Mayes TL, Soares JC, Soutullo CA, Storch EA, Wakefield SM (2023) Texas youth depression and suicide research network (TX-YDSRN) research registry and learning healthcare network: rationale, design, and baseline characteristics. J Affect Disord 340:88–99. https://doi.org/10.1016/j.jad.2023.07.035
Unützer J, Katon W, Callahan CM, Williams JW Jr, Hunkeler E, Harpole L, Hoffing M, Della Penna RD, Noël PH, Lin EH, Areán PA, Hegel MT, Tang L, Belin TR, Oishi S, Langston C, IMPACT Investigators, Improving Mood-Promoting Access to Collaborative Treatment (2002) Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA 288(22):2836–2845. https://doi.org/10.1001/jama.288.22.2836
U.S. Centers for Medicare & Medicaid Services (2023) APMs overview. Quality Payment Program. https://qpp.cms.gov/apms/overview
Walker ER, McGee RE, Druss BG (2015) Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiat 72(4):334–341. https://doi.org/10.1001/jamapsychiatry.2014.2502
Wang YH, Li JQ, Shi JF, Que JY, Liu JJ, Lappin JM, Leung J, Ravindran AV, Chen WQ, Qiao YL, Shi J, Lu L, Bao YP (2020) Depression and anxiety in relation to cancer incidence and mortality: a systematic review and meta-analysis of cohort studies. Mol Psychiatry 25(7):1487–1499. https://doi.org/10.1038/s41380-019-0595-x
Yeung A, Fung F, Yu SC, Vorono S, Ly M, Wu S, Fava M (2008) Validation of the patient health questionnaire-9 for depression screening among Chinese Americans. Compr Psychiatry 49(2):211–217. https://doi.org/10.1016/j.comppsych.2006.06.002
Funding
This manuscript was funded in part by the Center for Depression Research and Clinical Care at the University of Texas Southwestern Medical Center and the Texas Youth Depression and Suicide Research Network (TX-YDSRN), a research initiative of the Texas Child Mental Health Care Consortium (TCMHCC). The TCMHCC was created by the 86th Texas Legislature and, in part, funds multi-institutional research to improve mental health care for children and adolescents in Texas. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding organizations. The TX-YDSRN is implemented under the leadership of the central UT Southwestern HUB (Madhukar Trivedi, M.D., Principal Investigator, Sarah Wakefield, M.D., Medical Director [Texas Tech University Health Science Center Lubbock], Abu Minhajuddin, PhD, Data/Statistics Lead, Maria Monastirsky, M.A., Regulatory Oversight, and Holli Slater, PhD, Project Lead).
Author information
Authors and Affiliations
Contributions
Deane: Conceptualization; Writing—Original Draft Preparation. Elmore: Conceptualization; Writing—Original Draft Preparation. Mayes: Conceptualization; Writing—Original Draft Preparation. Robinson: Writing—Review & Editing. AlZubi: Writing—Review & Editing. Wakefield: Conceptualization; Project Administration; Writing—Review & Editing. Trivedi: Conceptualization; Project Administration; Funding Acquisition; Supervision; Writing—Review & Editing.
Corresponding author
Ethics declarations
Competing Interests
Dr. Trivedi has provided consulting services to Alkermes Inc, Axsome Therapeutics, Biogen MA Inc., Cerebral Inc., Circular Genomics Inc, Compass Pathfinder Limited, GH Research Limited, Heading Health Inc, Janssen, Legion Health Inc, Merck Sharp & Dohme Corp., Mind Medicine (MindMed) Inc, Merck Sharp & Dhome LLC, Naki Health, Ltd., Neurocrine Biosciences Inc, Noema Pharma AG, Orexo US Inc, Otsuka American Pharmaceutical Inc, Otsuka Canada Pharmaceutical Inc, Otsuka Pharmaceutical Development & Commercialization Inc, Praxis Precision Medicines Inc, SAGE Therapeutics, Sparian Biosciences Inc, Takeda Pharmaceutical Company Ltd, WebMD. He sits on the Scientific Advisory Board of Alto Neuroscience Inc, Cerebral Inc., Compass Pathfinder Limited, Heading Health, GreenLight VitalSign6 Inc, Legion Health Inc, Merck Sharp & Dohme Corp, Orexo US Inc, Signant Health. He holds stock in Alto Neuroscience Inc, Cerebral Inc, Circular Genomics Inc, GreenLight VitalSign6 Inc, Legion Health Inc. Additionally, he has received editorial compensation from American Psychiatric Association, and Oxford University Press. Dr. Deane, Mr. Elmore, Ms. Mayes, Dr. Wakefield, Ms. Alzubi, and Ms. Robinson have no declarations to report.
Ethical Approval
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Deane, A.E., Elmore, J.S., Mayes, T.L. et al. Shifting From Best Practice to Standard Practice: Implementing Measurement-Based Care in Health Systems. Child Psychiatry Hum Dev (2024). https://doi.org/10.1007/s10578-024-01715-0
Accepted:
Published:
DOI: https://doi.org/10.1007/s10578-024-01715-0