Abstract
Suicidal thoughts and behaviors (STB) are a leading cause of death in adolescence. To date, most research with youth has focused on risk factors for suicide; and less attention has been paid to resilience factors. This study examined whether positive beliefs and social connectedness moderate associations between mental health symptoms and STB. A community sample of 12-year-olds (N = 60) completed self-report questionnaires on their STB, mental health symptoms, positive beliefs and social connectedness. Nearly 20% of the adolescents reported STB. STB was associated with increased mental health symptoms and lower scores on the resilience measures. A significant moderating effect of social connectedness showed that youth with a combination of poor mental health and high levels of social support exhibited lower levels of STB. There was no significant moderating effect of positive beliefs. These results indicate that social support should be screened for in primary care and incorporated into youth suicide prevention programs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Suicide is a serious public health concern and is the leading cause of death among youth aged between 5 and 17 years in Western countries [1]. Consistent with other developed nations, in Australia, suicide is the leading preventable cause of death in young people: in 2018 100 young Australians died by suicide [2]. Although the majority of these deaths (n = 78) were in youth aged 15–17 years; suicide is also serious concern earlier in development with 22 young people aged 5–14 years dying by suicide. Although these figures represent the number of young people who died by suicide, it is important to recognise that many more young people may attempt suicide or have suicidal ideation [3]. Suicidal ideation, which ranges from feeling that life is not worth living through to plans for killing oneself, is relatively common in adolescence with 12–26% reporting such feelings in the past year [4]. Suicidal ideation is a serious matter as it increases risk for suicide attempts and for death by suicide [5, 6]. These youth suicide thoughts and behavior (STB) [7] statistics demonstrate the need to further understand early risk and resilience factors in order to best support vulnerable young people [8, 9].
Historically, identifying risk factors associated with youth STB has been a major, and important, focus of suicide prevention research [10]. To a lesser extent, resilience factors against youth STB have been examined [8, 11]. The construct of resilience are the processes involved in positively adapting or recovering in the face of adverse life-events or trauma [12]. Research shows that low resilience is associated with poor mental health outcomes, such as depression [13], which is a risk-factors for STB [14]; and inversely, resiliency can be a protective factor against youth STB [8].
With regard to suicide prevention research, resilience is conceptualised as factors that buffer individuals from STB under conditions of heightened risk [15]. Using Johnson’s bi-directional framework [11], a resilience factor is a psychological construct involving positive beliefs (e.g., wellbeing or positive mental health) or personal resources (e.g., social connectedness) [16, 17]. According to Johnson and colleagues’ [15] Schematic Appraisal Model of Suicide, high social connectedness results in positive beliefs and this confers resilience to STB in situations of risk, such as heightened mental health problems. This position is similar to Joiner, Van orden [18] Interpersonal Psychology Theory of Suicide (ITPS), whereby the desire for suicide is based on perceptions of oneself as burdensome to family and friends and feelings of low belongingness or social isolation from friends and family. Given that social connectedness and positive beliefs are considered important resilience factors in youth STB, they are the focus of the current paper.
Positive beliefs can be defined in terms of wellbeing and can be differentiated from the absence of mental ill health [16]. Wellbeing can be measured on a continuum from ‘languishing’ (mentally unhealthy) to ‘flourishing’ (mentally healthy) [19]; demonstrating a broad range of psychosocial functioning even in individuals without a diagnosis of a mental disorder [16]. Indeed, research has demonstrated that positive beliefs have protective effects on suicidality in the face of adversity. For example, both cross-sectionally [17] and longitudinally [20] positive beliefs have been found to buffer associations between depressive symptoms and STB. Similar buffering effects of positive beliefs have been documented with university students experiencing cyber-bullying [21] and adult psychiatric inpatients [22]. Teismann and Brailovskaia [23] argue that positive affect is the mechanism accounting for the protective role of positive beliefs on SBT.
Connectedness with family and peers is another variable that has been investigated as a possible resilience factor in SBT [24]. Social connectedness is defined as an individual’s awareness of close relationships with others and having a sense of belonging within a social setting and with family and friends [25]. According to Whitlock and Wyman [26], the mechanism by which connectedness influences SBT in adolescence is via three domains: (1) Interpersonal responses and processes, which is Joiner and Van Orden [18] ITPS whereby a sense of belonging and social inclusion reduce STB. (2) Collective responsibility and actions, whereby connectedness increases the likelihood of disclosure of STB enabling others in the network to intervene and provide meaningful support. (3) Positive norms and expectations, whereby positive group norms facilitate the notion that STB require intervention, and promotes healthy coping strategies and help-seeking behaviours.
The buffering role of social connectedness and STB has been demonstrated in adults with post-traumatic stress symptoms [27], depression symptoms in Chinese university students [17], and negative life in university students [28]. The buffering effect of social connectedness (including family, friends, peers and school supports) on STB has also been demonstrated adolescence, including clinically diagnosed 12–18-year-olds [29], a population-based cohort over 20,000 adolescents in Grades 7 through 11 [30]; and 14-year-old girls with poor physiological self-regulation, a potential risk for suicidality [31].
In sum, research shows that positive beliefs and social connectedness can moderate associations between risk factors and STB. However, most of this research was conducted in adults; apart from the three studies described above with social connectedness [29,30,31]. Associated research examining other types of buffers against STB (e.g., coping and problem solving, religious beliefs) is also typically conducted with adult participants [11]. Thus, there is a dearth of research addressing resilience factors to STB during the dynamic developmental phase of adolescence during which important physical, emotional and social changes are occurring [32].
The Longitudinal Adolescent Brain Study (LABS) is a prospective longitudinal cohort study conducted at the Thompson Institute (TI), University of the Sunshine Coast, Queensland, Australia. LABS was launched in July 2018, and aims establish the onset and track the trajectory of mental health, psychosocial function, and neurobiology across adolescence (years 7–12). Utilising data from the first wave of participants that had been recruited into LABS when this article was written,Footnote 1 the aim of the current study is to investigate whether wellbeing and social connectedness moderate the effects of mental health symptoms on STB at age 12 years. The hypotheses are that: (1) positive beliefs and good social connectedness will have negative associations with STB; (2) poorer mental health will be positively associated with STB; (3) positive beliefs and social connectedness will moderate the association between mental health symptoms and STB.
Methods
Participants
Adolescents were recruited into LABS via community advertisement, local community events, and by word-of-mouth. The advertising materials included (1) contact details (phone, email) of the LABS research assistants (RA) so interested participants to make contact, and (2) an online link to the LBAS website where potential participants could leave their details for the RA to contact them. Participants were included if they resided in the Sunshine Coast, Queensland and were in their 1st year of high school (Grade 7) and were 12-years-old when consenting to participate in LABS. Exclusion criteria included diagnosis of a neurological disorder, intellectual disability, major medical illness, or a head injury with unconsciousness exceeding 30 min. At the time of writing this paper, 60 adolescents (29 girls and 31 boys) aged 12 years had participated in their first LABS assessment and are included in the current study. Informed consent was obtained prior to participating from both the parent/caregiver and the adolescent. LABS received ethical approval from the University of the Sunshine Coast (HREC # A181064) in June 2018.
Procedure and Measures
LABS participants attended the TI labs and undertook two 2-h assessment sessions. Session 1 included a psychosocial self-report questionnaire, neurocognitive assessments, and a neuropsychiatric interview that were administered face-to-face by a trained RA. Session 2 included neurobiological assessments with fMRI scans performed by a registered radiologist and an EEG administered by a trained RA. Follow-up assessments utilising the same protocol are scheduled at 4-monthly intervals across 5 years of high school. The data from the self-report measures of STB, mental health symptoms, positive beliefs, and social connectedness that were collected at the first assessment time-point are reported on here.
Demographic Variables
The Socio-Economic Indexes for Areas (SEIFA) scores, from the Australian Bureau of Statistics population census [33] were used to assess participants’ socio-economic status. SEIFA scores are based on post-code status (M = 1000, SD = 100) with respect to areas of relative advantage and disadvantage; higher scores indicate areas that are well resourced compared to lower scores. The school type each participant attended was also assessed as: (1) state schools (publically funded) (2) independent state and private schools (publically and privately funded); and (3) Catholic schools.
Suicidal Thoughts and Behaviors
The Suicidal Ideation Attributes Scale (SIDAS; [34] assessed STB and their severity over the past month. The tool has been utilized in youth aged 12–25 years at risk of suicide and in suicide prevention programs [35]. Participants rated five statements from 0 to 10, with total scores ranging from 0 to 50, where higher scores indicate more severe suicidal ideation. Scores are interpreted such that a score of 0 indicates no suicidal ideation, scores from 1 to 20 indicate low risk for suicidal behaviour, and scores over 21 indicate high risk for suicidal behaviour [34].
Mental Health Symptoms
The Somatic and Psychological HEalth Report (SPHERE-12; [36] assessed anxious, depressive, and somatic symptoms during the past few weeks. The SPHERE12 is a 12-item self-report tool utilised as a mental health screener in primary care. Responses are given on a 3-point Likert-type scale ranging from 0 (never or some of the time) to 2 (most of the time). Total scores range from 0 to 24, where higher scores indicate higher levels of mental health symptoms and are categorised as follows: normal (scores 5 or less), somewhat distressed (scores 6–11), and high distress (scores 12 and above). This tool has been validated in a sample of youth aged 8–16 years and has high internal consistency (alpha > 0.78) and moderate 3-month reliability (ICC = 0.47–0.58) [37].
Positive Beliefs
The COMPAS-W Scale of Wellbeing (Composure; Own-Worth; Mastery; Positivity; Achievement; Satisfaction; Wellbeing) [19] was used to assess participants positive beliefs. The COMPAS-W consists of 26 items where participants indicate their agreement with each statement on a 5-point Likert scale from 1 (strongly disagree) to 5 (strongly agree). Items are summed to provide a composite Total Wellbeing score ranging from 26 to 130, with higher scores indicating better wellbeing. Scores can also be categorised as languishing, moderate or flourishing. This scale has very good internal consistency (alpha range 0.82–0.90) in adolescent samples aged 12–17 years [38].
Social Connectedness
The Social Connectedness Scale (SCS [25] assessed the degree to which the participants felt connected to their social environment (e.g., friends, family, and community). The SCS consists of 15 items with participants indicating their agreement to each item on a 6-point Likert scale with responses ranging from 1 (strongly disagree) to 6 (strongly agree) [39]. The scores are summed to give a total score ranging from 15 to 90 with higher scores indicating feeling a greater sense of social connectedness. This scale was designed for an adolescent population and has very high validity and internal consistency (Cronbach’s alpha = 0.92; Lee and Robins 1995).
Duty of Care
A suicidality escalation protocol was implemented as duty of care to any participants who self-reported STB. The protocol involved multiple levels of action, dependent on the participant’s responses to the suicidality items. If “no reported suicidality” was obtained no further action was taken. For participants who scored in the low-medium risk category, a trained staff member initiated a conversation and provided the youth with an information flyer. Those who registered in the high-emergency category were referred for an appointment with an on-site psychologist and/or the option for an ambulance call-out for transportation to the emergency department. Caregivers of youths who scored in the SIDAS risk categories were informed by the RA of this outcome and the level of action recommended; the youth were given the option to be present or absent during this debriefing.
Statistical Analyses
Descriptive analyses (means, standard deviations, and categorisation where appropriate) were performed on the measures of STB (SIDAS), mental health (SPHERE-12), and resilience factors (COMPAS-W and SCS) (see Table 1). Diagnostics revealed outliers on the following measures: SIDAS (n = 1) and SCS (n = 2). These data were Winzorised to the next lowest or highest score (respectively) to maintain rank order but reduce the influence of the outlier in the regression models. As diagnostics showed the data for all measures were skewed, Spearman’s Rho bivariate correlations were conducted to examine the associations among the demographic variables (age, gender, SEIFA, school type) and measures of suicidality, psychological distress and resilience factors (see Table 2). Mann–Whitney U tests were conducted to determine if there were differences in scores across all measures for females and males.
Hierarchical regression analyses were conducted to examine the hypothesised moderating effects of social connectedness and wellbeing on associations between STB and mental health symptoms. The two models were the same for each resilience factor: in step 1, SPHERE-12 total scores were entered, in step 2, one resilience factor was entered (model 1: social connectedness; model 2: positive beliefs). Step 3 included the interaction term between mental health and one of the resilience factors (model 1: social connectedness; model 2: positive beliefs). All correlation and main effect analyses were significant for p-values < .05. Any interaction term with p < .01 was probed using the PROCESS macro 3.4 and the Johnson–Neyman (J–N) technique with simple slope analysis (Hayes 2013). This technique is a tool used in moderation analysis that involves estimating the upper and lower bands at which the moderator’s (resilience factor) effect of X (i.e., SIDAS score) on Y (i.e., SPHERE-12 score) becomes, or ceases to be, significant (Hayes 2013). Analyses were conducted using SPSS v24.
Results
Descriptive Analyses
Descriptive statistics for all measures are shown in Table 1. For the demographic variables, there was close to an even split for male and female participants. Based on the SEIFA scores, these young people came from a range of socio-economic backgrounds; although the mean score was situated above the standardised mean of 1000, indicating a relative well-resourced group. Approximately half the participants attended state schools, one-third independent or private schools, followed by attendance at Catholic schools (13%).
At the overall group level, the mean scores on the SIDAS were in the low range. The majority (78%) of the young people reported no STB in the past month on the SIDAS. However, 17% of participants (n = 10; 6 female, 4 male) were classified at low risk of suicidal behaviour and 5% (n = 3; 2 female, 1 male) were at high risk. The duty of care protocol was activated for 10 participants scoring in the low-medium risk category and three in the high-emergency category.
For mental health symptoms, total scores on the SPHERE-12 showed that approximately two-thirds of the participants (n = 38; 15 female, 23 male) had good mental health, 33% (n = 20; 12 female, 8 male) were classified as experiencing mild mental distress, with 3% (n = 2 female) as having high levels of distress. For the measure of positive beliefs (the COMPAS-W) 37% of young people (n = 22; 13 female, 9 male) scored in the flourishing category, 52% (n = 31; 11 female, 20 male) were classified as having moderate wellbeing, and 12% (n = 7; 5 female, 2 male) were classified as languishing. Mean scores on the social connectedness scale were towards the higher end: an average score of 74 (SD = 12.60) out of a maximum of 90, suggesting a well-connected group. Mann–Whitney U tests revealed that there were no differences in scores for females or males on any of the scales.
Correlations
Spearman Rho’s correlations between demographic and outcome variables are shown in Table 2. The correlation coefficients showed strong associations (p < .01) between most of the outcome measures in the matrix. The SPHERE-12 was positively associated with the SIDAS (r = .56), suggesting that poorer mental health was associated with increased STB. Also, there were significant negative associations between the SIDAS and resilience measures (COMPAS-W r = − .51; SCS r = − .46), suggesting that lower (i.e., less STB) SIDAS scores were associated with increased positive beliefs and social connectedness. However, there were no significant correlations between the demographic variables themselves (age, gender, SEIFA, school type), nor between the demographic variables and the outcome variables (SIDAS, COMPAS-W, SPHERE-12, SOC). As the associations between demographics and outcome measures were not significant the demographic variables were not included in the regression analyses.
Hierarchical Regression Analyses
The results of the regression analyses examining the moderating influence of positive beliefs (model 1) on the association between SIDAS and SPHERE-12 scores are shown in Table 3. In step 1, mental health symptoms accounted for 27.2% of variance (p < .001); showing that increased mental health problems were associated with increased STB on the SIDAS. In step 2, the association between mental health and STB remained significant, and a significant negative association between positive beliefs and STB explained a significant additional 7.3% of variance in adolescents’ suicidality (p = .014); indicating increased scores on the COMPAS-W were associated with lower scores on the SIDAS. However, in the final step (3), there was no significant interaction effect between mental health symptoms and positive beliefs and SIDAS score; indicating that positive beliefs do not significantly moderate the association between mental health symptoms and STB.
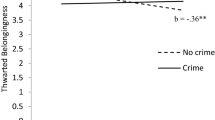
The results of the regression analyses examining the moderating influence of social connectedness (model 2) on the association between SIDAS and SPHERE-12 scores are shown in Table 4. In step 1, mental health accounted for 27.2% of variance (p < .001); showing that increased mental health problems were associated with increased STB on the SIDAS. In step 2, the association between mental health and STB was no longer significant, but a significant negative association showed that social connectedness explained an additional 19.2% of variance in adolescents’ STB (p < .001), indicating that lower social connectedness scores were associated with increased STB. In the final step (3), there was a significant interaction effect between mental health symptoms and social connectedness, explaining an additional unique 16% of variance in STB (p = .001), showing a significant moderating effect of social connectedness on association between mental health and STB. This interaction was probed with PROCESS macro by testing the conditional effects of mental health at three levels of social connectedness (− 1 SD mean, mean, + 1 SD mean) and is shown in Fig. 1. Mental health symptoms were significantly related to STB when social connectedness was 1 SD below the mean (p = .001); but not when social connectedness was at the mean (p = .19) or 1SD above the mean (p = .31). The J–N technique revealed that the association between mental health symptoms and STB was significant with a social connectedness scores lower than 71.08; but not significant above this score.
The significant moderating effect of social connectedness for low (− 1 SD; 61.45), medium, (74.05) and high (+ 1 SD; 86.65) scores (SCS) on mental health (SPHERE-12) and suicidality (SIDAS); such that at higher levels of mental health problems, youth with lower social connectedness had significantly elevated suicidality (blue line) vs youth with high levels of mental health problems and higher social connectedness scores had reduced suicidality (yellow line) (Color figure online)
Discussion
The results from this study showed that approximately one in five 12-year-olds from a community sample reported some level of STB in the past month, highlighting the need to identify resilience factors that may offer some protection for vulnerable youth. The aims of the study were to examine associations between risk and resilience factors and SBT in adolescence and to examine whether two resilience factors buffer adolescents with increased mental health symptoms against STB: positive beliefs and social connectedness.
Results of the regression analyses show that Hypotheses 1 and 2 were upheld and Hypothesis 3 was partially upheld: Hypothesis 1 was supported as we found that higher scores on the resilience measures of positive beliefs and social connectedness both had negative associations with STB. Similarly, Hypothesis 2 was supported as increased mental health symptoms were positively associated with STB. Finally, Hypothesis 3 was partly supported as social connectedness moderated the association between mental health symptoms and STB; yet this buffering effect was not significant for the measure of positive beliefs.
With respect to the significant moderating effect of social connectedness, when social connectedness was moderate to high, young people with poor mental health were less likely to experience STB; whereas low social connectedness in the presence of mental health symptoms was associated with increased STB. This finding is consistent with the literature also finding that social connectedness buffers associations between risk factors and STB, although usually in adult samples with clinical diagnoses [17, 27, 28, 40, 41]. However, three studies have demonstrated that adolescent social connectedness buffers at-risk youth from STB [29,30,31].
The current results support Whitlock and Wyman [26] proposed three-pronged mechanistic pathways of how social connectedness influences STB. Social connectedness may be potential buffer in adolescence as it is during this developmental phase that social networks become a major source of emotional support as teens begin to spend more time with their friends rather than family [42], providing them with a sense of belonging and inclusion. This orientation towards peers, and strong peer attachments, particularly with positive group norms, are associated with improved wellbeing [43] and self-regulation [44]. Active social connections at home, with friends, and at school are related to lower STB [31, 41] as these networks may facilitate detection and promote intervention in youth with STB.
There are limited intervention programs available to increase social connectedness for youth STB [35, 45]. The Sources of Strength is an evidence-based school suicide prevention program that aims to increase social connectedness to reduce STB [46]. Another recent intervention demonstrated that an on-line social networking program (“Affinity”) significantly reduced pre-post intervention STB in youth [47]. Thus, social connectedness presents an opportunity for clinical intervention that could be incorporated into youth suicide prevention programs at schools or in the community.
Although the regression analyses demonstrated that higher levels of positive beliefs were associated with decreased likelihood of STB in this early adolescent sample, we also found that positive beliefs did not significantly moderate the association between mental health symptoms and STB. This is in contrast to a several studies in adult participants reporting that positive beliefs moderated at-risk individuals (e.g., depression, bullying victims) against STB [17, 20, 23, 48]. However, rather than the COMPAS-W measure of subjective and psychological wellbeing used here to assess positive beliefs, these adult studies utilised other measures, such as the Positive Mental Health (PMH) scale assessing psychological aspects of wellbeing; which may account for different findings between the studies. However, there is currently limited research examining aspects of positive beliefs as a buffer in youth suicide. The current study did not find support for the moderating effect of positive beliefs on STB in a community 12-year-old sample; although this may change across the course of adolescent development, particularly in youth whose mental health symptoms may worsen over time and changes in positive beliefs may co-occur.
It is important to note that prior research has identified other resilience factors that influence STB, such as hope [9], problem-solving skills [49], and resiliency [8, 50]. An avenue of future research would be to examine whether these variables also operate as protective factors in adolescents with STB. Once there is a more comprehensive understanding of various resilience factors in young people with STB a model or action of variables that function together can be proposed that will be important in reducing suicide rates in this vulnerable population.
Another interesting finding from this study was that there were no significant associations between the demographic variables and the young peoples’ scores on the outcome measures. This is the lack of difference in STB for males and females in this cohort contrasted with one other study with 12-year-old participants, which showed that males had increased levels of STB compared to females: 43–28% respectively [51]. However, this study also demonstrated that socio-economic status was not associated with youth STB [51]. We will be interested to see whether these findings with respect to demographics, especially for gender, change as we track this LABS cohort across adolescence.
There are several limitations to the current study to be noted. First is the relatively small sample size that may limit generalising these findings. However, it should be noted that only a small number of other studies on suicide prevention have included a group of early adolescence who are all aged 12 years [51]. Second is the cross-sectional nature of the study, which was necessary as the participants had not yet completed sufficient follow-up assessments to enable detection of statistically significant results in a longitudinal analysis. Third is the possibility that the sample was prone to self-selection bias as young people with concerns about their mental health may have been more likely to volunteer to participate. Forth, the data relied solely on self-report measures rather than clinical interview. This was due to the low levels of detection of mental disorders in the sample from the neuropsychiatric interview. Finally, the range of scores on the measure of mental health was mostly in the healthy range, which would be expected in a community cohort.
In conclusion, the current results demonstrate that nearly one in five 12-year-olds from a community sample experienced STB over the past month. This study demonstrates that social connectedness can buffer associations between increased mental health symptoms and STB, showing that this is a potentially important resilience factor that should be included in youth suicide prevention programs to protect young people at risk for suicide. We will track the progression of the LABS cohort over time to determine the longitudinal effects of these buffering variables on STB across adolescence.
Summary
This study examined whether resilience factors (positive beliefs and social connectedness) buffered the association between mental health symptoms and suicidal thoughts and behaviours (STB) in 12-year-olds. Sixty young adolescence participating in the Longitudinal Adolescent Brain Study (LABS) completed self-report questionnaires on their STB, mental health symptoms, positive beliefs and social connectedness at their first intake into the study. Nearly 20% of the 12-year-olds reported STB. STB was associated with increased mental health symptoms and lower scores on the resilience measures. A significant moderating effect of social connectedness showed that youth with a combination of poor mental health and high levels of social support exhibited lower levels of STB. Although high positive self-beliefs were associated with lower levels of STB, there was no significant moderating effect of these beliefs between poor mental health and STB. These results extend on prior research that is mostly focused on risk factors for STB to examine resilience. In the coming years, once the LABS sample is of sufficient size, we will be in a position to determine longitudinal moderating associations between these important variables. The current findings indicate that social support should be screened for in primary care and social connectedness skill building should be incorporated into youth suicide prevention programs in school and the community.
Notes
At the time this paper was written there was insufficient data from subsequent assessments to run longitudinal analyses: T1 (n = 60), T2 (n = 39), T3 (n = 31) and T4 (n = 5).
References
World Health Organization (2018) Global health estimates 2016: deaths by cause, age, sex, by country and by region, 2000–2016. World Health Organization, Geneva
Australian Bureau of Statistics (2019) Casuses of death. Australian Bureau of Statistics, Canberra
Sanchez-Teruel D, Robles-Bello MA, Camacho-Conde JA (2020) Self-inflicted injuries in adolescents and young adults: a longitudinal study. Psicothema 32(3):322–328
Nock MK et al (2008) Suicide and suicidal behavior. Epidemiol Rev 30:133–154
Franklin JC et al (2017) Risk factors for suicidal thoughts and behaviors: a meta-analysis of 50 years of research. Psychol Bull 143:187–232
Stewart SL et al (2020) Risk of suicide and self-harm in kids: the development of an algorithm to identify high-risk individuals within the children’s mental health system. Child Psychiatry Hum Dev. https://doi.org/10.1007/s10578-020-00968-9
Silverman MM et al (2007) Rebuilding the Tower of Babel: a revised nomenclature for the study of suicide and suicidal behaviors. Part 2: suicide-related ideations, communications, and behaviors. Suicide Life Threat Behav 37:264–277
Sanchez-Teruel D, Auxiliadora M, Robles-Bello MA (2014) Protective factors promoting resilience to suicide in young people and adolescents. Pap Psychol 35:181–192
Sanchez-Teruel D, Robles-Bello MA, Camacho-Conde JA (2020) Adaptation and psychometric properties in Spanish of the Herth Hope Index in people who have attempted suicide. Psychiatr Quart. https://doi.org/10.1007/s11126-020-09766-x
Kim H-S, Kim HS (2008) Risk factors for suicide attempts among Korean adolescents. Child Psychiatry Hum Dev 39(3):221–235
Johnson J et al (2011) Resilience to suicidality: the buffering hypothesis. Clin Psychol Rev 31(4):563–591
Masten A (2011) Resilience in children threatened by extreme adversity: frameworks for research, practice, and translational synergy. Dev Psychopathol 23:493–506
Cicchetti D (2013) Annual research review: resilient functioning in maltreated children–past, present, and future perspectives. J Child Psychol Psychiatry 54:402–422
Kim KM (2020) What makes adolescents psychologically distressed? Life events as risk factors for depression and suicide. Eur J Child Adolesc Psychol. https://doi.org/10.1007/s00787-020-01520-9
Johnson J et al (2010) Resilience as positive coping appraisals: testing the schematic appraisals model of suicide (SAMS). Behav Res Ther 48(3):179–186
Keyes CL (2005) Mental illness and/or mental health? Investigating axioms of the complete state model of health. J Consult Clin Psychol 73(3):539–548
Siegmann P et al (2018) Resilience to suicide ideation: a cross-cultural test of the buffering hypothesis. Clin Psychol Psychother 25(1):e1–e9
Joiner TE et al (2009) Main predictions of the interpersonal-psychological theory of suicidal behavior: empirical tests in two samples of young adults. J Abnorm Psychol 118:634–646
Gatt JM et al (2014) The heritability of mental health and wellbeing defined using COMPAS-W, a new composite measure of wellbeing. Psychiatry Res 2019:204–213
Teismann T et al (2018) Positive mental health moderates the association between depression and suicide ideation: a longitudinal study. Int J Clin Health Psychol 18(1):1–7
Brailovskaia J, Teismann T, Margraf J (2018) Cyberbullying, positive mental health and suicide ideation/behavior. Psychiatry Res 267:240–242
Brailovskaia J et al (2019) Positive mental health moderates the association between suicide ideation and suicide attempts. J Affect Disord 245:246–249
Teismann T, Brailovskaia J, Margraf J (2019) Positive mental health, positive affect and suicide ideation. Int J Clin Health Psychol 19(2):165–169
Gunn JF, Goldsetin SE, Gager CT (2018) A longitudinal examination of social connectedness and suicidal thoughts and behaviors among adolescents. Child Adolesc Mental Health 23:341–350
Lee RM, Robbins SB (1995) Measuring belongingness: the social connectedness and the social assurance scales. J Couns Psychol 42:232–241
Whitlock J, Wyman PA, Moore SR (2014) Connectedness and suicide prevention in adolescents: pathways and implications. Suicide Life Threat Behav 44:246–272
Panagioti M et al (2014) Perceived social support buffers the impact of PTSD symptoms on suicidal behavior: implications into suicide resilience research. Compr Psychiatry 55(1):104–112
Kleiman EM, Riskind JH, Schaefer KE (2014) Social support and positive events as suicide resiliency factors: examination of synergistic buffering effects. Arch Suicide Res 18(2):144–155
Miller AB, Esposito-Smythers C, Leichtweis RN (2015) Role of social support in adolescent suicidal ideation and suicide attempts. J Adolesc Health 56(3):286–292
Kidd S et al (2006) The social context of adolescent suicide attempts: interactive effects of parent, peer, and school social relations. Suicide Life Threat Behav 36:386–395
Giletta M et al (2017) Suicide ideation among high-risk adolescent females: examining the interplay between parasympathetic regulation and friendship support. Dev Psychopathol 29:1161–1175
Sawyer SM et al (2012) Adolescence: a foundation for future health. Lancet 379:1630–1640
Australian Bureau of Statistics (2016) Census of population and housing: Socio-Economic Indexes for Areas (SEIFA). Australian Bureau of Statistics, Canberra
van Spijker B et al (2014) The suicidal ideation attributes scale (SIDAS): community-based validation study of a new scale for the measurement of suicidal ideation. Suicide Life Threat Behav 44:408–419
Calear AL et al (2016) A systematic review of psychosocial suicide prevention interventions for youth. Eur J Child Adolesc Psychol 25:467–482
Hickie IB et al (2001) SPHERE: a national depression project. SPHERE National Secretariat. Med J Aust 175(Suppl):S4–S5
Couvy-Duchensne B et al (2017) Validation and psychometric properties of the Somatic and Psychological HEalth REport (SPHERE) in a young Australian-based population sample using non-parametric item response theory. BMC Psychiatry 17:279
Gatt JM et al (2020) Trauma, resilience and mental health in migrant and non-migrant youth: an international cross-sectional study across six countries. Front Psychiatry 10:997
Lee RM, Dean BL, Jung K-R (2008) Social connectedness, extraversion, and subjective well-being: testing a mediation model. Pers Individ Differ 45:414–419
Johnson J et al (2010) Resilience to suicidal ideation in psychosis: positive self-appraisals buffer the impact of hopelessness. Behav Res Ther 48(9):883–889
Kleiman EM, Liu RT (2013) Social support as a protective factor in suicide: findings from two nationally representative samples. J Affect Disord 150:540–545
Gorrese A, Ruggieri R (2012) Peer attachment: a meta-analytic review of gender and age differences and associations with parent attachment. J Youth Adolesc 41:650–672
Gorrese A (2016) Peer attachment and youth internalizing problems: a meta-analysis. Child Youth Care Forum 45:177–204
Zeman J, Cassano M, Adrian MC (2013) Socialization influences on children’s and adolescents’ emotional self-regulation processes. In: Barrett KC, et al. (eds) Handbook of self-regulatory processes in development: new directions and international perspectives. Psychology Press, New York
Boehm KE, Campbell NB (1995) Suicide: a review of calls to an adolescent peer listening phone service. Child Psychiatry Hum Dev 26:61–66
Wyman PA et al (2010) An outcome evaluation of the Sources of Strength suicide prevention program delivered by adolescent peer leaders in high schools. Am J Public Health 100:1653–1661
Bailey E et al (2020) An enhanced social networking intervention for young people with active suicidal ideation: safety, feasibility and acceptability outcomes. Int J Environ Res Public Health 17:7
Siegmann P et al (2019) Positive mental health as a moderator of the association between risk factors and suicide ideation/behavior in psychiatric inpatients. Psychiatry Res 273:678–684
McAuliffe C et al (2006) Problem-solving ability and repetition of deliberate self-harm: a multicentre study. Psychol Med 36:45–55
Sher L (2019) Resilience as a focus of suicide research and prevention. Acta Psychiatr Scand 140:169–180
Adrian M et al (2015) Suicidal ideation in early to middle adolescence: sex-specific trajectories and predictors. J Child Psychol Psychiatry 57:645–653
Acknowledgements
Many thanks to the young people who generously participated in this research and to the LABS research assistants: Amanda Boyes and Genevieve Roberts. Thank you also to Dr Paul Schwen for preparing the dataset.
Funding
This study was funded by a grant from the Australian Commonwealth Government’s ‘Prioritizing Mental Health Initiative’ (2018–2019) 4-7R154BP.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that they have no competing or potential conflicts of interest.
Ethical Approval
All procedures performed in this study were in accordance with the ethical standards of the institutional ethics committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Research Involving Human Rights
The study protocol was approved by the University of the Sunshine Coast Human Research Ethics Board (# A181064) and was conducted ethically in accordance with the Declaration of Helsinki.
Informed Consent
Both the young people participating in this study and their parent or guardian provided written informed consent to participate.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Simcock, G., Andersen, T., McLoughlin, L.T. et al. Suicidality in 12-Year-Olds: The Interaction Between Social Connectedness and Mental Health. Child Psychiatry Hum Dev 52, 619–627 (2021). https://doi.org/10.1007/s10578-020-01048-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10578-020-01048-8