Abstract
With the increase in fetal surgeries, the effect of maternal anesthesia on progeny has attracted much attention. Our previous studies have demonstrated that 3.5% sevoflurane maternal exposure resulted in over-activated autophagy and cognitive impairment in the offspring. The autophagy activation resulted in increased apoptosis and decreased proliferation. However, the effects of sevoflurane on neural stem cell (NSC) differentiation is unclear. There is evidence that autophagy might participate in anesthesia-induced NSC differentiation. Firstly, we examined the effects of sevoflurane on NSC differentiation and explored possible mechanisms. Then, we investigated whether autophagy was related to differentiation. On gestational day 14 (G14), rats were exposed to 2% or 3.5% sevoflurane for 2 h, then markers of neurons and astrocytes, and the FOXO3 expression was measured in fetal brains 48 h later. The differentiation of NSCs was detected after autophagy inhibition by 3-MA. Changes in NSC differentiation, autophagy level, and FOXO3 were examined after administration of lithium chloride. After 3.5% sevoflurane exposure, the expressions of β-Tubulin III, NeuN, SYP, GFAP and FOXO3 increased. Autophagy inhibition alleviates improper NSC differentiation. Lithium chloride attenuated FOXO3 and autophagy activation, ameliorated NSC differentiation and the decline of Nestin expression. Our results demonstrated that maternal exposure to 3.5% sevoflurane for 2 h during the mid-trimester induced NSC differentiation in the fetal brain through the activation of FOXO3. Autophagy inhibitor or lithium chloride reversed the improper differentiation of NSCs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years, the developmental neurotoxicity of anesthetics has become a global issue concerned by the medical profession and the public, a large number of animal experiments and clinical studies have shown that general anesthetics have harmful effects on the immature nervous system (Woodward et al. 2019). With the progress of fetal diagnostic technology and the intrauterine surgery, it is urgent to ensure the safety of maternal and fetal anesthesia in the mid-trimester. As the mid-trimester is a crucial period for nervous system development, the influence of anesthetic exposure on the offspring's brain development has attracted increasing attention.
Neurogenesis, defined as the generation and survival of nerve cells from NSCs, is a fundamental event during embryonic brain development and vital to forming an integrated and normal nervous system. Since neurogenesis mainly occurs in the mid-trimester (Palanisamy 2012), the fetal brain is vulnerable and easily affected during this period. Our previous study revealed that 3.5% sevoflurane exposure at embryonic day 14 (E14), equivalent of the human mid-trimester, led to adverse consequences, such as NSC decline and subsequent neurobehavioral dysfunction in offspring (Wang et al. 2018).
NSCs have drawn great attention due to their pluripotency in the generation of nerve lineages in the central nervous system (CNS): neurons, astrocytes, and oligodendrocytes (Renault et al. 2009). The capacity of stem cell self-renewal is indispensable for the lifetime maintenance of the stem cell pool and neurogenesis. Fetal neurodevelopment is a rigorously regulated process whereby differentiation of regions leads to an integrated CNS. Therefore, tight regulation of differentiation during development remains a critical issue. So far, the effects of the anesthetics on NSC differentiation and its mechanisms are still poorly understood.
Our published study has shown that sevoflurane activated autophagy of NSCs via PTEN/Akt/mTOR pathway, and inhibition of autophagy alleviated the NSC apoptosis and proliferation decline (Li et al. 2017). Besides, autophagy has been reported to participate in stem cell remodeling, differentiation, and self-renewal (Zhao et al. 2010; Vazquez et al. 2012). Autophagy is a particularly important process that maintains the stemness of NSCs (Pan et al. 2013). Another study of our team found that lithium chloride improved the performance of offspring in Morris Water Maze (MWM) and alleviated NSC proliferation inhibition (Wang et al. 2018). Besides, it has been reported that lithium chloride can regulate the autophagy level. Therefore, lithium chloride was used as another intervention in this study.
Forkhead box class O (FOXO) transcription factors play important roles in various cellular responses, including differentiation, survival, cell cycle arrest, and stress regulation (Salih and Brunet 2008). FOXO3, a subtype of FoxO transcription factors in mammals, is located downstream of the Akt/mTOR pathway, and highly expressed in the brain (Mao et al. 2007). It was reported that FOXO3 is crucial in maintaining NSC differentiation, and participates in the autophagy process (Renault et al. 2009; Wang et al. 2013; Audesse et al. 2019).
To understand the effect of sevoflurane on NSC differentiation and the role of FOXO3 in the sevoflurane neurotoxicity during the mid-trimester, we used the embryonic day 14 (E14) rat model, and the concentration and duration of anesthesia were maintained. We hypothesize that 3.5% sevoflurane activates FOXO3, which is responsible for the improper differentiation and the decreased NSC pools.
Methods and Materials
Animals
Animal experiments were conducted at the experimental research center and approved by Animal Care and Use Committee of Shengjing Hospital (NO.2019PS141K) in compliance with laboratory animal care and use guidelines.
Rat feeding and vaginal smear procedures were detailed as described previously (Li et al. 2017). In brief, rats were raised at 22 ± 1 °C with 12 h light/dark cycle, and the pellet diet and water were freely obtained. Every three female rats with 1 male rat were put in the cage at 17:00. The next day, if sperm is observed in the vaginal smear, the female rats were regarded to be pregnant. The day was recorded as gestation 0 day (G0) for female rats and embryonic 0 day (E0) for fetuses.
Sevoflurane Exposure
The sevoflurane exposure procedure was consistent with the previous description (Li et al. 2017). In brief, rats were maintained in the aeration chamber with 30% oxygen at 2 L/min flow rate for 2 h. The remaining rats in 2% sevoflurane (2%SEV) group and 3.5% sevoflurane (3.5%SEV) group were inhaled with 2% and 3.5% sevoflurane, respectively. The fetal brain tissues were taken 48 h after gas exposure through the cesarean section.
Drug Premedication
Rats in 3.5% sevoflurane plus lithium chloride (3.5%SEV + LiCl) group were injected with lithium chloride (2 mmol/kg) intraperitoneally. Lithium chloride was initially conducted at 0.5 h before anesthesia. Based on our previous study, the dosage of lithium chloride was selected. Treatment in 3.5% sevoflurane plus 3-MA (3.5%SEV + 3-MA) group was consistent with the previous study (Li et al. 2017). Other rats were treated with vehicle solution in the same volume.
PCR
Total RNA was isolated from fetal brains with Trizol, extracted using chloroform and isopropanol, and measured by spectrophotometer. Then RNA reverse transcription was conducted using the Takara kit. RT-PCR was performed on the 7500 FAST Real-Time PCR System (Thermo, United States). The FOXO3 primer was listed as follow: 5′- ACGGCTCACTTTGTCCCA -3′ (forward), 5′- CTCTTGCCAGTCCCTTCG -3′ (reverse). Results were analyzed by the − ΔΔCt method.
Western Blot
The fetal brains were dissected and proteins were extracted from the brain tissues. The tissues were homogenized in RIPA buffer with PMSF. After centrifugation, the supernatant was collected then determined with BCA Kit. The protein was separated by electrophoresis, then transferred to PVDF membranes (IPVH0010, Millipore, Germany). The membranes were sealed with 5% nonfat milk and subsequently incubated overnight with the following primary antibodies at 4 °C, LC3B Antibody (2775; Cell Signaling Technology, USA), Beclin-1 Antibody (3738; Cell Signaling Technology, USA), NeuN Antibody (MAB377; Millipore, Germany), GFAP Antibody (ab7260; Abcam, UK), SYP Antibody (17785-1-AP; Proteintech, USA), β-Tubulin III (ab18207; Abcam, Uk), Nestin Antibody (MAB353; Millipore, Germany), FOXO3 Antibody (YT1763; ImmunoWay, USA). Then, the membranes were rinsed and HRP-conjugated second antibodies were then used to probe the membrane at RT for 2 h. Immunoreactivity was detected with SuperSignal® West Pico Chemiluminescent Substrate (34080, Thermo, USA), and membrane images were generated by GE Amersham Imager 600.
Immunohistochemistry
Brain tissues were post-fixed with 4% PFA, dehydrated in graded ethanol, then embedded in paraffin. The specimens were cut at a transverse plane (2.5 μm), and the sections were deparaffinized and heat repaired in citrate buffer and incubated with 0.03% hydrogen peroxide and 10% fetal bovine serum. Then, sections were submerged with Nestin Antibody (MAB353; Millipore, Germany). The slides were incubated with secondary antibody, DAB, and hematoxylin. The slides were magnified at ×400 under Nikon C1 microscope, and 1 ~ 2 visual fields were randomly taken on each glass. OD value was analyzed with NIS-Elements AR Analysis 4.50.00.
Immunofluorescence Staining
The other set of paraffin slides were stained with immunofluorescence. The slides were deparaffinized and transferred to citrate buffer and immersed in 10% FBS for 40 min at RT. Sections were kept in the primary antibodies overnight at 4 °C, then covered with fluorescent labeled secondary antibodies. Nuclei were stained with DAPI for 5 min. The primary antibodies used here were as follows: FOXO3 Antibody (YT1763; ImmunoWay, USA), LC3B Antibody (ab48394; Abcam, UK), and Nestin Antibody (MAB353, Millipore, Germany). Stained sections were captured with the microscope (LSM880, ZEIZZ, Germany).
Statistical Analysis
The data equal variances and normality were checked with Bartlett's test and Shapiro–Wilk test. Parametric data comparisons were carried out with one-way ANOVA with Student–Newman–Keuls post hoc test, and nonparametric data comparisons were performed with Kruskal–Wallis followed by the Dunn’s Multiple comparison test using GraphPad Prism 5.0 software and SPSS 20.0 software. Datasets are expressed as mean ± SD. Statistical significance was calculated when P < 0.05.
Results
3.5% Sevoflurane Anesthesia Induced FOXO3 Activation in Fetal NSCs
Our published study has reported that 3.5% sevoflurane maternal exposure led to autophagy activation in fetal NSCs, whereas the 2% sevoflurane group and the control group did not show difference. Then we examined the expression of FOXO3 48 h after the exposure to sevoflurane (Fig. 1). Our PCR results revealed 3.5% sevoflurane increased FOXO3 expression, and 2% sevoflurane did not (Fig. 1a, 3.5%SEV vs. CON: 2.07 ± 0.72 vs. 1.01 ± 0.14, P < 0.05; 3.5%SEV vs. 2%SEV: 2.07 ± 0.72 vs. 1.07 ± 0.19, P < 0.05). Protein expression detected by Western Blot was also used to strengthen these results, and elevation in FOXO3 level was shown in the 3.5%SEV group (Fig. 1b and c, 3.5%SEV vs. CON: 2.71 ± 1.09 vs. 1.00 ± 0.08, P < 0.05; 3.5%SEV vs. 2%SEV: 2.71 ± 1.09 vs. 1.16 ± 0.52, P < 0.05). To prove the sevoflurane-induced FOXO3 activation, we performed immunofluorescence. In the slides of the 3.5%SEV group, FOXO3 is expressed in the nucleus, whereas in the CON group and 2%SEV group red light was labeled in cytoplasm (Fig. 1d). To sum up, these results suggest that 3.5% sevoflurane maternal exposure activated FOXO3 expression in the fetal brains.
Sevoflurane activated FOXO3 in the fetal brain. a Quantitation of FOXO3 mRNA by RT-PCR. b and c Quantitation of FOXO3 protein expression by Western blot. n = 5, *P < 0.05 versus the CON group, #P < 0.05 versus the 2%SEV group. d Immunofluorescence detection of FOXO3 (red) and DAPI (blue), scale bar = 50 μm
3.5% Sevoflurane Anesthesia Induced NSC Differentiation
We have reported that 3.5% sevoflurane exposure resulted in NSC decline in fetus. To determine whether sevoflurane affects NSC differentiation potential, NeuN, GFAP, β-Tubulin III and SYP were detected with Western Blot (Fig. 2). Our results revealed that in the 3.5%SEV group expression of NeuN, SYP, and GFAP were higher than the CON and 2%SEV group (Fig. 2, 3.5%SEV vs. CON: NeuN: 2.37 ± 0.65 vs. 1.02 ± 0.20, P < 0.01; SYP: 2.49 ± 1.22 vs. 1.00 ± 0.21, P < 0.05; GFAP: 3.95 ± 1.11 vs. 1.00 ± 0.24, P < 0.05; 3.5%SEV vs. 2%SEV: NeuN: 2.37 ± 0.65 vs. 1.22 ± 0.39, P < 0.01; SYP: 2.49 ± 1.22 vs. 0.95 ± 0.38, P < 0.05; GFAP: 3.95 ± 1.11 vs. 1.15 ± 0.52, P < 0.05); the 2%SEV and CON groups showed no difference; Expression of β-Tubulin III in the 3.5%SEV group was elevated compared with the CON group, however, although the expression was higher in the 3.5% group than in the 2% group, the difference was not statistically significant (Fig. 2, 3.5%SEV vs. CON: 3.32 ± 1.02 vs. 1.00 ± 0.23, P < 0.01; 3.5%SEV vs. 2%SEV: 3.32 ± 1.02 vs. 1.35 ± 0.36, P > 0.05). These results indicated that 3.5% sevoflurane effectively promoted NSC differentiation.
Lithium Chloride Attenuated FOXO3 Activation after 3.5% Sevoflurane Anesthesia
To demonstrate whether lithium chloride could reduce FOXO3 activation, lithium chloride pretreatment was conducted. The results showed that FOXO3 expression was decreased in the 3.5%SEV + LiCl group compared to the 3.5%SEV group (Fig. 3a, 3.5%SEV + LiCl vs. 3.5%SEV: 1.17 ± 0.25 vs. 1.73 ± 0.48, P < 0.05; Fig. 3b and c, 3.5%SEV + LiCl vs. 3.5%SEV: 1.03 ± 0.33 vs. 2.76 ± 1.06, P < 0.05). In slides of the 3.5%SEV group, FOXO3 is expressed mainly in the nucleus, whereas FOXO3 fluorescence in the 3.5%SEV + LiCl group was partly in the nucleus and partly in the cytoplasm, and red light labeling in the CON group and CON + LiCl group was in the cytoplasm (Fig. 3d). These results showed that lithium chloride reduced 3.5% sevoflurane-induced FOXO3 activation.
Lithium chloride pretreatment inhibited FOXO3 activation induced by sevoflurane. a Quantitation of FOXO3 mRNA by RT-PCR. b and c Quantitation of FOXO3 protein expression by Western blot. n = 5, *P < 0.05, **P < 0.01 versus the CON group, #P < 0.05 versus the 3.5%SEV group. d Immunofluorescence detection of FOXO3 (red) and DAPI (blue), scale bar = 50 μm
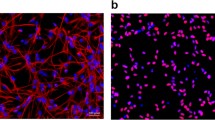
Lithium Chloride Ameliorated 3.5% Sevoflurane Anesthesia Activated Autophagy in Fetal NSCs
The following experiments investigated the effects of lithium chloride on NSCs autophagy. We evaluated changes in the expressions of LC3B and Beclin-1. Both of the autophagy markers expression in the 3.5%SEV + LiCl group were reduced versus the 3.5%SEV group (Fig. 4a and b, 3.5%SEV + LiCl vs. 3.5%SEV: LC3BII: 0.82 ± 0.31 vs. 1.65 ± 0.18, P < 0.01; Beclin-1: 0.67 ± 0.12 vs. 2.04 ± 0.72, P < 0.001). Following the Western blots, we monitored immunofluorescence of LC3B and Nestin, a characteristic NSC marker. In the sections of the 3.5%SEV group, LC3B presenting punctate dot formation, while in the 3.5%SEV + LiCl group, LC3B showed diffused green light. In a word, lithium chloride ameliorated autophagy in NSCs after 3.5% sevoflurane exposure (Fig. 4c).
Lithium chloride pretreatment alleviated sevoflurane-induced autophagy activation in the NSCs. a and b Quantitation of autophagy marker expressions by Western blot. n = 5, **P < 0.01 versus the CON group, ##P < 0.01, ###P < 0.001 versus the 3.5%SEV group. c Immunofluorescence detection of autophagy marker, LC3B (green), and NSC marker, Nestin (red), scale bar = 50 μm
Lithium Chloride Prevented 3.5% Sevoflurane Induced NSC Differentiation in Fetal Rats
To prove that differentiation was regulated by FOXO3, the following experiments investigated the effects of lithium chloride on NSC differentiation, assessing expressions of β-Tubulin III, NeuN, SYP, and GFAP. All expressions of the proteins mentioned above were decreased after lithium chloride administration (Fig. 5, 3.5%SEV + LiCl vs. 3.5%SEV: β-Tubulin III: 1.00 ± 0.40 vs. 1.75 ± 0.54, P < 0.05; NeuN: 0.63 ± 0.44 vs. 2.02 ± 0.38, P < 0.001; SYP: 1.03 ± 0.41 vs. 3.10 ± 0.89, P < 0.001; GFAP: 0.71 ± 0.29 vs. 1.57 ± 0.36, P < 0.001). In accordance with the previous report, 3.5% sevoflurane interfered with NSC content in the fetal brains as Nestin expression decreased compared with the CON group. The Nestin Western blot and immunohistochemistry results showed increased expression in the 3.5%SEV + LiCl than 3.5% SEV group (Fig. 6a and b, 3.5%SEV + LiCl vs. 3.5%SEV: 0.75 ± 0.28 vs. 0.41 ± 0.19, P < 0.05; Fig. 6c and d, 3.5%SEV + LiCl vs. 3.5%SEV: 0.35 ± 0.03 vs. 0.32 ± 0.01, P < 0.05).
Lithium chloride pretreatment alleviated sevoflurane-induced NSC reduction. a and b Quantitation of Nestin expression by Western blot. c and d Quantitation of Nestin expression by immunohistochemistry. n = 5, *P < 0.05, **P < 0.01 versus the CON group, #P < 0.05 versus the 3.5%SEV group, scale bar = 50 μm
3-MA Prevented NSC Differentiation After 3.5% Sevoflurane Exposure in Fetal Rats on E14
In order to further investigate whether sevoflurane-induced autophagy activation is involved in NSC differentiation, autophagy inhibitor (3-MA) pretreatment was conducted. 3-MA usage was consistent with the previous description (Li et al. 2017). Then we evaluated the expressions of β-Tubulin III, NeuN, SYP and GFAP by Western blot. In accordance with the preceding results, all of the differentiation markers expression were increased after 3.5% sevoflurane treatment, and reduced after 3-MA administration (Fig. 7, 3.5%SEV + 3-MA vs. 3.5%SEV: β-Tubulin III: 1.01 ± 0.39 vs. 1.93 ± 0.67, P < 0.01; NeuN: 0.73 ± 0.44 vs. 1.98 ± 0.51, P < 0.001; SYP: 1.36 ± 0.28 vs. 5.21 ± 1.22, P < 0.01; GFAP: 0.82 ± 0.46 vs. 2.02 ± 0.58, P < 0.01).
Discussion
The influence of anesthetic on the developing brain has attracted more and more attention. A large number of animal experiments have found that general anesthesia drugs can affect the synaptic morphology and cognitive function of the developing brain (Jevtovic-Todorovic et al. 2003; Fang et al. 2012), and clinical studies have also suggested that general anesthesia may lead to abnormal learning or behavior in children (Warner et al. 2018). With the development of prenatal diagnosis and intrauterine treatment technology, more and more pregnant women experienced general anesthesia in the mid-trimester, which puts forward higher requirements for the validity of anesthesia and the safety of mother and fetus. As an important period of fetal neurodevelopment, whether the exposure of anesthetics in the mid-trimester interferes with the neurodevelopment of the offspring has aroused concern.
The mid-trimester is an important period of fetal nervous system development, during which neurogenesis is widely present in the brain. Neurogenesis is the biological process that neural stem/progenitor cells undergo proliferation and asymmetric division to produce functional postmitotic neurons and integrate them into the neural network (Sanes et al. 2006; Perna et al. 2015). Neurogenesis is a complex process that is finely regulated by coordinated signaling molecules. γ-aminobutyric acid (GABA) and glutamate are important neurotransmitters in the brain, which are involved in regulating the NSC self-renewal and differentiation in early nervous system development. Given that most general anesthetics act on GABAA and NMDA receptors (Li and Yu 2014), exposure to general anesthetics in the mid-trimester is likely to affect the NSC fate transition from proliferation to differentiation. Our study found that sevoflurane exposure in the mid-trimester reduced the number of NSCs in the offspring brain tissues and impaired long-term learning and memory ability with a concentration dependence of sevoflurane.
To elucidate the effect of different concentration sevoflurane on NSC differentiation, we used the concentrations according to our previous studies. Since the minimum alveolar concentration (MAC) of sevoflurane in rodents is about 2.4% (Abreu et al. 2012), and 99% of the effective concentration of sevoflurane for general clinical anesthesia is 1.3MAC, that is, 3.0% sevoflurane (Zhang et al. 2015). However, in order to reduce the dosage of intravenous anesthetics, prevent uterine contractions, and achieve satisfactory anesthesia depth, higher concentration is often required, even up to 1.6 ~ 1.7MAC. Thus 2% and 3.5% respectively represent the general concentration and relatively high concentration. Our previous results showed that 3.5% sevoflurane exposure reduced the NSC content, but 2% showed no such damage (Wang et al. 2018).
Besides NSC decline, our previous results revealed that autophagy also participated in anesthesia-induced neurotoxicity. In our previous study, we observed the autophagy levels 2 ~ 48 h after 3.5% sevoflurane exposure at E14, all of which were increased (Li et al. 2017). However, since the differentiation process was relatively significant from E16, the observation time point of this study was selected at the moment of 48 h after exposure. Autophagy has been demonstrated to be highly active during differentiation (Asanuma et al. 2003; Wang et al. 2010). Interference with the autophagy disturbs the coordination of cell proliferation, differentiation and death necessary for the establishment of complex CNS structure (Boya et al. 2008), which may be potential mechanisms of sevoflurane-induced cognitive decline. Autophagy inhibitors or autophagy-related gene knockdown inhibited the differentiation of NSCs, as revealed by reduced expression of neuronal and astrocyte markers (Vazquez et al. 2012).
Our previous results suggested that sevoflurane-induced autophagy was mediated by the PTEN/Akt/mTOR pathway. Akt/mTOR pathway has been reported as a key negative regulatory factor of autophagy (Heras-Sandoval et al. 2014). However, there are many other downstream targets of Akt, such as FOXO3 (Dong et al. 2018; Lee et al. 2019). FOXO3 is a member of Forkhead box class O transcription factors, which participates in regulating various biological activities including cell metabolism, differentiation, and apoptosis (Caballero-Caballero et al. 2013). Inactive FOXO3 exists in the cytoplasm and rapidly translocates into the nucleus after dephosphorylation, where it can regulate the gene transcription that involves in the cell cycle, differentiation, and metabolism (Burgering and Kops 2002; Greer and Brunet 2005). FoxOs is expressed in all mammalian embryonic tissues, among which FOXO3 expression gradually increased in brain tissues from E10.5 day (Qian et al. 2000), and finally widely distributed in adult brain (Furuyama et al. 2000; Hoekman et al. 2006). Lack of FOXO activity in vivo is characterized by an increase in brain volume, and constitutive activation of FOXO3 results in a decrease in brain size in developing murine (Schmidt-Strassburger et al. 2012).
FOXO transcription factors are known as autophagy regulators (Sengupta et al. 2009; van der Vos et al. 2012; Filomeni et al. 2015). FOXO3 is a transcriptional activator of autophagy-related genes in different cell types and sufficient for the induction of differentiation in vivo (Webb and Brunet 2014). As expected, FOXO3 is activated after 3.5% sevoflurane exposure. In addition to autophagy, FOXO3 promotes cell differentiation, cell cycle arrest, stress resistance, and apoptosis. FOXO3 was shown to regulate the homeostasis and self-renewal of hematopoietic stem cells (Miyamoto et al. 2007) and NSCs (Paik et al. 2009; Renault et al. 2009). In addition, the expression of FOXO3 has been demonstrated to be upregulated when iPS cells differentiate into neuronal lineages (Wang et al. 2013). The ability of NSCs isolated from foxo3a-null mice to produce different nerve lineages was impaired (Yalcin et al. 2010). In conclusion, these results suggest that FOXO3 is important for differentiation. In the current study, we found that autophagy inhibition could protect NSC from sevoflurane-induced differentiation, and we propose that neuroprotective effect might be related to FOXO3 inhibition, which regulates autophagy as a mechanism for sevoflurane-induced NSC differentiation.
Our previous study showed that lithium chloride pretreatment had a beneficial effect on NSC proliferation, and could ameliorate the decline of NSCs and impairments of learning and memory performance (Wang et al. 2018). Lithium was demonstrated to regulate autophagy negatively. For instance, lithium has been reported to reduce autophagy in neonates after hypoxic ischemia, possibly by increasing the activity of mTOR (Li et al. 2010). More importantly, a study by Mao et al. revealed that lithium significantly reduced the transcription and activity level of FOXO3 (Mao et al. 2007). In the current study, results showed that lithium chloride pretreatment played the role of inhibiting FOXO3 transcription, subsequent autophagy and improper NSC differentiation. Neuroprotective effects of lithium in sevoflurane anesthesia during the mid-trimester may be mediated by mechanisms above.
Strengths and Limitations
Our study represents the robust examination of the effects of sevoflurane on the fetus in the mid-trimester. This study provided a highly extensive examination of NSC differentiation after sevoflurane exposure. The major finding of the study is that maternal sevoflurane exposure induced improper NSC differentiation via FOXO3 with a novel finding that autophagy is associated with it.
Our study still has a few limitations. In the previous study, we performed blood gas analysis on pregnant rats at the end of sevoflurane exposure, and remarkable hypoxia or hypercarbia was not detected. Thus no physiological index monitoring was conducted. Furthermore, we did not determine the long-term and dose-dependent effects of lithium chloride on neurodevelopment. Since lithium chloride has not been widely used in clinical practice, more studies are needed to clarify the mechanism of sevoflurane neurotoxicity and to find clinically feasible prevention and treatment methods.
Conclusion
Collectively, the study demonstrated that 3.5% sevoflurane anesthesia in the mid-trimester induced improper NSC differentiation via FOXO3 activation. Autophagy inhibition with 3-MA or lithium chloride could alleviate autophagy activation, as well as suppress both the differentiation markers and FOXO3 expression. The results above provide strong evidence to speculate that targeting autophagy might be vital to preventing sevoflurane-induced neurotoxicity and developing novel treatment strategies to alleviate anesthesia-related neurotoxicity.
References
Abreu M, Aguado D, Benito J, Gomez de Segura IA (2012) Reduction of the sevoflurane minimum alveolar concentration induced by methadone, tramadol, butorphanol and morphine in rats. Lab Anim 46(3):200–206
Asanuma K, Tanida I, Shirato I, Ueno T, Takahara H, Nishitani T, Kominami E, Tomino Y (2003) MAP-LC3, a promising autophagosomal marker, is processed during the differentiation and recovery of podocytes from PAN nephrosis. FASEB J 17(9):1165–1167
Audesse AJ, Dhakal S, Hassell LA, Gardell Z, Nemtsova Y, Webb AE (2019) FOXO3 directly regulates an autophagy network to functionally regulate proteostasis in adult neural stem cells. PLoS Genet 15(4):e1008097
Boya P, Mellen MA, de la Rosa EJ (2008) How autophagy is related to programmed cell death during the development of the nervous system. Biochem Soc Trans 36:813–817
Burgering BM, Kops GJ (2002) Cell cycle and death control: long live Forkheads. Trends Biochem Sci 27(7):352–360
Caballero-Caballero A, Engel T, Martinez-Villarreal J, Sanz-Rodriguez A, Chang P, Dunleavy M, Mooney CM, Jimenez-Mateos EM, Schindler CK, Henshall DC (2013) Mitochondrial localization of the forkhead box class O transcription factor FOXO3a in brain. J Neurochem 124(6):749–756
Dong P, Zhang X, Zhao J, Li D, Li L, Yang B (2018) Anti-microRNA-132 causes sevofluraneinduced neuronal apoptosis via the PI3K/AKT/FOXO3a pathway. Int J Mol Med 42(6):3238–3246
Fang F, Xue Z, Cang J (2012) Sevoflurane exposure in 7-day-old rats affects neurogenesis, neurodegeneration and neurocognitive function. Neurosci Bull 28(5):499–508
Filomeni G, De Zio D, Cecconi F (2015) Oxidative stress and autophagy: the clash between damage and metabolic needs. Cell Death Differ 22(3):377–388
Furuyama T, Nakazawa T, Nakano I, Mori N (2000) Identification of the differential distribution patterns of mRNAs and consensus binding sequences for mouse DAF-16 homologues. Biochem J 349(Pt 2):629–634
Greer EL, Brunet A (2005) FOXO transcription factors at the interface between longevity and tumor suppression. Oncogene 24(50):7410–7425
Heras-Sandoval D, Perez-Rojas JM, Hernandez-Damian J, Pedraza-Chaverri J (2014) The role of PI3K/AKT/mTOR pathway in the modulation of autophagy and the clearance of protein aggregates in neurodegeneration. Cell Signal 26(12):2694–2701
Hoekman MF, Jacobs FM, Smidt MP, Burbach JP (2006) Spatial and temporal expression of FoxO transcription factors in the developing and adult murine brain. Gene Expr Patterns 6(2):134–140
Jevtovic-Todorovic V, Hartman RE, Izumi Y, Benshoff ND, Dikranian K, Zorumski CF, Olney JW, Wozniak DF (2003) Early exposure to common anesthetic agents causes widespread neurodegeneration in the developing rat brain and persistent learning deficits. J Neurosci 23(3):876–882
Lee JW, Nam H, Kim LE, Jeon Y, Min H, Ha S, Lee Y, Kim SY, Lee SJ, Kim EK, Yu SW (2019) TLR4 (toll-like receptor 4) activation suppresses autophagy through inhibition of FOXO3 and impairs phagocytic capacity of microglia. Autophagy 15(5):753–770
Li G, Yu B (2014) Elevation of protective autophagy as a potential way for preventing developmental neurotoxicity of general anesthetics. Med Hypotheses 82(2):177–180
Li Q, Li H, Roughton K, Wang X, Kroemer G, Blomgren K, Zhu C (2010) Lithium reduces apoptosis and autophagy after neonatal hypoxia-ischemia. Cell Death Dis 1:e56
Li X, Wu Z, Zhang Y, Xu Y, Han G, Zhao P (2017) Activation of autophagy contributes to sevoflurane-induced neurotoxicity in fetal rats. Front Mol Neurosci 10:432
Mao Z, Liu L, Zhang R, Li X (2007) Lithium reduces FoxO3a transcriptional activity by decreasing its intracellular content. Biol Psychiatry 62(12):1423–1430
Miyamoto K, Araki KY, Naka K, Arai F, Takubo K, Yamazaki S, Matsuoka S, Miyamoto T, Ito K, Ohmura M, Chen C, Hosokawa K, Nakauchi H, Nakayama K, Nakayama KI, Harada M, Motoyama N, Suda T, Hirao A (2007) Foxo3a is essential for maintenance of the hematopoietic stem cell pool. Cell Stem Cell 1(1):101–112
Paik JH, Ding Z, Narurkar R, Ramkissoon S, Muller F, Kamoun WS, Chae SS, Zheng H, Ying H, Mahoney J, Hiller D, Jiang S, Protopopov A, Wong WH, Chin L, Ligon KL, DePinho RA (2009) FoxOs cooperatively regulate diverse pathways governing neural stem cell homeostasis. Cell Stem Cell 5(5):540–553
Palanisamy A (2012) Maternal anesthesia and fetal neurodevelopment. Int J Obstet Anesth 21(2):152–162
Pan H, Cai N, Li M, Liu GH, Izpisua Belmonte JC (2013) Autophagic control of cell “stemness.” EMBO Mol Med 5(3):327–331
Perna RB, Loughan AR, Le JA, Hertza J (2015) Prenatal and perinatal anesthesia and the long-term cognitive sequelae: a review. Appl Neuropsychol Child 4(1):65–71
Qian X, Shen Q, Goderie SK, He W, Capela A, Davis AA, Temple S (2000) Timing of CNS cell generation: a programmed sequence of neuron and glial cell production from isolated murine cortical stem cells. Neuron 28(1):69–80
Renault VM, Rafalski VA, Morgan AA, Salih DA, Brett JO, Webb AE, Villeda SA, Thekkat PU, Guillerey C, Denko NC, Palmer TD, Butte AJ, Brunet A (2009) FoxO3 regulates neural stem cell homeostasis. Cell Stem Cell 5(5):527–539
Salih DA, Brunet A (2008) FoxO transcription factors in the maintenance of cellular homeostasis during aging. Curr Opin Cell Biol 20(2):126–136
Sanes DH, Reh TA, Harris WA (2006) Development of the nervous system. Elsevier, Amsterdam
Schmidt-Strassburger U, Schips TG, Maier HJ, Kloiber K, Mannella F, Braunstein KE, Holzmann K, Ushmorov A, Liebau S, Boeckers TM, Wirth T (2012) Expression of constitutively active FoxO3 in murine forebrain leads to a loss of neural progenitors. FASEB J 26(12):4990–5001
Sengupta A, Molkentin JD, Yutzey KE (2009) FoxO transcription factors promote autophagy in cardiomyocytes. J Biol Chem 284(41):28319–28331
van der Vos KE, Eliasson P, Proikas-Cezanne T, Vervoort SJ, van Boxtel R, Putker M, van Zutphen IJ, Mauthe M, Zellmer S, Pals C, Verhagen LP, Groot Koerkamp MJ, Braat AK, Dansen TB, Holstege FC, Gebhardt R, Burgering BM, Coffer PJ (2012) Modulation of glutamine metabolism by the PI(3)K-PKB-FOXO network regulates autophagy. Nat Cell Biol 14(8):829–837
Vazquez P, Arroba AI, Cecconi F, de la Rosa EJ, Boya P, de Pablo F (2012) Atg5 and Ambra1 differentially modulate neurogenesis in neural stem cells. Autophagy 8(2):187–199
Wang H, Ma J, Tan Y, Wang Z, Sheng C, Chen S, Ding J (2010) Amyloid-beta1-42 induces reactive oxygen species-mediated autophagic cell death in U87 and SH-SY5Y cells. J Alzheimers Dis 21(2):597–610
Wang Y, Tian C, Zheng JC (2013) FoxO3a contributes to the reprogramming process and the differentiation of induced pluripotent stem cells. Stem Cells Dev 22(22):2954–2963
Wang Y, Yin S, Xue H, Yang Y, Zhang N, Zhao P (2018) Mid-gestational sevoflurane exposure inhibits fetal neural stem cell proliferation and impairs postnatal learning and memory function in a dose-dependent manner. Dev Biol. https://doi.org/10.1016/j.ydbio.2018.01.022
Warner DO, Zaccariello MJ, Katusic SK, Schroeder DR, Hanson AC, Schulte PJ, Buenvenida SL, Gleich SJ, Wilder RT, Sprung J, Hu D, Voigt RG, Paule MG, Chelonis JJ, Flick RP (2018) Neuropsychological and behavioral outcomes after exposure of young children to procedures requiring general anesthesia: The Mayo Anesthesia Safety in Kids (MASK) study. Anesthesiology 129(1):89–105
Webb AE, Brunet A (2014) FOXO transcription factors: key regulators of cellular quality control. Trends Biochem Sci 39(4):159–169
Woodward TJ, Timic Stamenic T, Todorovic SM (2019) Neonatal general anesthesia causes lasting alterations in excitatory and inhibitory synaptic transmission in the ventrobasal thalamus of adolescent female rats. Neurobiol Dis 127:472–481
Yalcin S, Marinkovic D, Mungamuri SK, Zhang X, Tong W, Sellers R, Ghaffari S (2010) ROS-mediated amplification of AKT/mTOR signalling pathway leads to myeloproliferative syndrome in Foxo3(-/-) mice. EMBO J 29(24):4118–4131
Zhang DX, Jiang S, Yu LN, Zhang FJ, Zhuang Q, Yan M (2015) The effect of sevoflurane on the cognitive function of rats and its association with the inhibition of synaptic transmission. Int J Clin Exp Med 8(11):20853–20860
Zhao Y, Huang Q, Yang J, Lou M, Wang A, Dong J, Qin Z, Zhang T (2010) Autophagy impairment inhibits differentiation of glioma stem/progenitor cells. Brain Res 1313:250–258
Acknowledgements
This study was supported by the National Natural Science Foundation of China [Grant Numbers 81870838; Liaoning Province Distinguished Professor Support Program [Grant Numbers XLYC1802096]; Shenyang Clinical Medicine Research Center of Anesthesiology [Grant Numbers 19-110-4-24, 20-204-4-44]; Outstanding Scientific Fund of Shengjing Hospital [Grant Number 201708].
Author information
Authors and Affiliations
Contributions
XL: study conception and design, experimental operation, data analysis, and writing-original draft. XJ: experimental operation and data collection. QG: writing-reviewing and editing. PZ: supervision and guidance.
Corresponding author
Ethics declarations
Conflict of interest
No author claims competing interests or relationships with other people or organizations that could inappropriately influence this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, X., Jiang, X., Gao, Q. et al. FOXO3 Regulates Sevoflurane-Induced Neural Stem Cell Differentiation in Fetal Rats. Cell Mol Neurobiol 42, 1777–1786 (2022). https://doi.org/10.1007/s10571-021-01055-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10571-021-01055-w