Abstract
Background
The development of mindfulness parenting programs in recent years offers a promising direction for targeting parental emotional dysregulation in families of children with attention deficit hyperactivity disorder (ADHD). Nevertheless, research on the effectiveness of mindfulness parenting programs is limited, and little is known about the contribution of mindfulness skills to parenting when integrated with parent training (PT).
Objective
The present study evaluated a mindfulness skills augmentation to PT for ADHD. We hypothesized that mindfulness-enhanced PT would improve parental emotion regulation and reduce hostile and coercive parenting.
Method
We developed a 90-min mindfulness skills protocol and integrated it with a nonviolent resistance (NVR) PT program addressing ADHD and behavior difficulties. A total of 79 families were randomly assigned to PT or mindfulness-enhanced PT. Forty-three families completed intervention. We used multilevel modeling to evaluate parental emotion regulation, hostile and coercive parenting, and child behavioral symptoms across treatments and over time.
Results
Across treatment conditions, mothers’ negative feelings, escalating behaviors, and capacity for emotion regulation improved significantly following treatment. Fathers in the mindfulness condition reported greater improvement in the capacity for emotion regulation, reduced negative feelings, and reduced parental submission compared with fathers in the PT condition. We found no differences in child externalizing symptoms, which decreased significantly in both groups.
Conclusions
Study results suggest that PT in NVR is effective in improving maternal capacity for emotion regulation and in reducing hostile and coercive parenting. For fathers, a mindfulness-based skills augmentation may be important for enhancing treatment benefits.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parenting children with attention and behavior difficulties can be emotionally challenging (Laugesen and Grønkjær 2015). Children with ADHD and behavioral problems often require parental support in order to manage their over-reactivity (Melnick and Hinshaw 2000). In addition, because these children tend to express much of their emotional reactivity in the form of anger or opposition, parents’ capacity to manage these behaviors without becoming hostile or aggressive plays an important role in preventing clashes and escalations (Marceau et al. 2015). Moreover, given that some of the behavioral symptoms in ADHD may persist, parents’ ability to manage stress over time affects their capacity to remain sensitive to their child’s regulatory challenges (Halligan et al. 2013).
The parents’ capacity to regulate negative affect, or emotion regulation (ER), is therefore central to parenting children with ADHD effectively. Parents’ own ER impacts their capacity to respond to the child’s behaviors in more containing and sensitive ways, and reduces the parents’ hostile and coercive reactions (Bridgett et al. 2015; Leerkes et al. 2015; Rutherford et al. 2015). By reducing hostile and coercive reactions parents may prevent the development of a negative parent–child relationship, which has been identified as a major contributor to the exacerbation of behavioral and emotional symptoms of ADHD (Burt et al. 2003; Drabick et al. 2006).
Despite the prominent role of parents in managing negative emotions when raising a child with ADHD, parents’ capacity for ER is not directly addressed in parent training (PT) for ADHD and externalizing problems (Maliken and Katz 2013), and the impact of PT on parental affective processes is rarely evaluated (Colalillo and Johnston 2016). We sought to address this clinical and scientific gap by developing a brief mindfulness skills augmentation to PT for ADHD. We were interested in evaluating the impact of mindfulness skills training on both the parents’ capacity for emotion regulation and negative reactions to the child following PT.
Parent Training and Parental Emotion Regulation
The literature has used different phrases to describe parenting programs for ADHD—for example, parent management training (PMT), behavioral parent training (BPT), and parent training (PT). Here, we use the more general phrase “parent training” (PT) to describe our program.
Behavioral PT, a well-established treatment for children diagnosed with ADHD (Evans et al. 2014), was developed to help parents more efficiently and effectively set limits, as well as predict and prevent behavioral escalations. Parent training utilizes principles of behavioral conditioning to reduce child behavior problems by teaching parenting skills such as positive parenting, planned responses to a child’s transgressions, consistent schedule of reinforcements and a more structured home routine. (Kazdin 1997; Kolko et al. 2009). In its traditional form, PT does not address the bidirectional impact of children’s aggressive and dysregulated behavior on the parent–child relationship, nor does it speak to the challenging emotional atmosphere within which the suggested skills should be utilized (Cavell et al. 2013). Failure to address the emotional context of the family and parental characteristics such as high levels of stress and/or mental illness may limit the benefits of PT for some parents in spite of its well-documented efficacy in reducing child behavioral symptoms (Chacko et al. 2009; Lundahl et al. 2006).
Ben-Porath (2010) highlighted the need for greater focus on parenting emotional processes in PT, arguing that the skills and insights parents acquire during controlled and calm therapy sessions may not be sufficient to change parental behaviors. Parents might struggle to use new skills and knowledge when the child’s behavior arouses their own negative emotions. Indeed, an outcome study that compared families who benefitted from PT with those who did not found that parents’ capacity to regulate their own arousal may influence the efficacy of the intervention (Granic et al. 2007). Results showed that those mothers who were more over-reactive and struggled to provide the emotional scaffolding necessary to regulate their child’s arousal were less able to change their reaction to their child’s dysregulation.
Consistent with these findings, a meta-analysis of PT conducted by Beauchine et al. (2005) found that PT was less effective for families who began treatment with high maternal negativity toward the child. Further, Gardner et al. (2006) showed that the “active ingredients” in PT studies involved the parents’ capacity for “positive parenting”, or the parents’ expression of positive affect with the child and parents’ problem-solving behaviors.
Despite mounting evidence that parental emotional regulation and expression are critical to the effectiveness of PT, little is known about the impact of PT on parents’ emotional and cognitive processes. In a recent review of parents’ cognition and affective outcomes following PT, Colalillo and Johnston (2016) demonstrated that although PT was effective in reducing related constructs (such as parenting-related stress and parents’ sense of competency), there were no consistent findings indicating that PT impacts parental functioning in less direct, parenting-related ways (such as parental depression or overall stress). In addition, gender was found to be a partial moderator of treatment benefits, as fathers reported less improvement in parenting outcomes compared with mothers (Colalillo and Johnston 2016; Panter-Brick et al. 2014).
In sum, the aforementioned studies suggest that although parental emotional processes influence parents’ ability to support the child and effectively manage the child’s behavior, little is known about how PT impacts parents’ emotional processes. Moreover, because few studies have focused on measuring parental cognitive and emotional processes as treatment outcomes, it is unclear whether PT is impacting parents’ capacity for ER indirectly, or if parental emotion regulation should be targeted directly in order to improve parenting outcomes following PT.
Mindfulness Training as Possible Path for Improving Parental Emotion Regulation
Over the past three decades, there has been a notable increase in the incorporation of mindfulness practices as a supplement to traditional cognitive behavioral therapy (CBT). Hayes and Feldman (2004) evaluated the impact of adding mindfulness practice to CBT interventions for depression. Their results indicated that patients who practiced mindfulness were better able to process negative experiences without using repression or engaging in negative thought processes. Erisman and Roemer (2010) showed that brief mindfulness interventions in a lab setting can improve ER by increasing awareness of emotions, reducing recovery time from negative emotional experiences, and increasing attention to positive emotional experiences. Kumar et al. (2008) showed that mindfulness training can reduce experiential avoidance.
Duncan et al. (2009) developed a conceptual model for mindful parenting, which they described as listening with full attention and nonjudgmental acceptance, possessing emotional awareness of self and child, and exercising self-regulation in the parenting relationship. According to this model, mindful parents can bring their full attention to interactions with their child and are therefore capable of more accurately perceiving their child’s experience. Dumas (2005) suggested that parents can use mindfulness techniques to listen more openly to their children, develop emotional awareness, and better regulate their own emotions before reacting. In light of this conceptualization and preliminary research findings, mindfulness may offer direct and structured ways for helping parents of children with ADHD manage their emotions and reduce automatic, negative reactions to the child’s behaviors. These positive benefits may help reduce coercive and escalating parental reactions and provide the child with better scaffolding to regulate distress.
Several mindful parenting programs were developed and evaluated in the past decade, most of which were adapted from mindfulness-based stress reduction (MBSR) interventions (Kabat-Zinn 1990) or mindfulness-based cognitive therapy (MBCT) for parents (Segal et al. 2012). These interventions typically consist of eight to 12 weeks of meditation-based training in a group setting as well as daily meditation practice. Eames et al. (2015) piloted an MBSR intervention with a group of mothers from disadvantaged backgrounds and found improved maternal well-being and reduced parental stress. In another pilot study, van de Weijer-Bergsma et al. (2012) found that an eight-week group mindfulness training for adolescents with ADHD and their parents significantly reduced parenting stress for fathers; however, decreases in maternal reactivity faded at the eight-week follow up. Using a similar intervention with a group of elementary school children with ADHD, van der Oord et al. (2012) found a significant reduction in parental reports of child ADHD symptoms and parenting reactivity, although teacher reports did not change after the intervention. Using a multiple baseline design with two cases of children with ADHD and their mothers, Singh et al. (2010) showed that 12 weeks of mindfulness training increased positive mother–child interactions, children’s level of compliance, and mothers’ satisfaction with parenting. Haydicky et al. (2015) found that eight weeks of parallel MBCT interventions for children with ADHD and their parents led to reduced parental reports of ADHD internalizing and externalizing symptoms, as well as reductions in parental stress. The children’s self-reports, however, did not indicate improvements. Reviewing current mindfulness intervention programs with parents, Townshend et al. (2016) reported overall positive results for mindfulness parenting programs, mainly in relation to child externalizing problems and parents’ emotional dismissal of their children. Townsend et al., however, described these results as preliminary because of the small number of published studies and the significant methodological limitations in the studies reviewed.
To date, only one published study (Coatsworth et al. 2015) has incorporated mindfulness skills training as part of an existing intervention addressing child behavior problems (e.g., strengthening families; Molgaard et al. 2001). The study used a randomized clinical trial (RCT) design to measure the impact of integrating a mindfulness skills protocol into the original program. In spite of adequate power, the results indicated no advantages for the mindfulness-enhanced intervention in relation to parents’ well-being and parent-youth relationship quality. However, fathers in the mindfulness group demonstrated greater emotional awareness and compassionate acceptance of their child.
Despite these encouraging findings, no consistent evidence exists supporting the utility and applicability of mindfulness skills training with parents of children with ADHD and behavior problems. The lack of consistent findings may be related to significant differences in the conceptualization and administration of mindfulness interventions across studies. First, some programs intensively applied mindfulness skills, such as daily meditation practice and weekly mindfulness meetings (e.g., Bögels et al. 2014; Singh et al. 2010), whereas others extracted only the most relevant skills and integrated them within an existing evidence-based treatment (e.g., Coatsworth et al. 2015). Second, only one study used an active comparison group (Coatsworth et al. 2015), making it difficult to assess the added contribution of mindfulness skills to evidence-based treatment interventions, such as PT. Third, all prior studies used a group intervention that was standardized across participating families rather than individual interventions tailored to address specific family needs. Though group interventions have several advantages (e.g., enabling additional peer support, improving motivation for implementation and providing positive modeling), this mode of treatment delivery may not be the optimal for parents in individual treatments (such as PT) or parents with elevated stress levels and psychopathology (Lundahl et al. 2006). Finally, past studies did not assess the effectiveness of mindfulness interventions for families presenting with more acute child behavior difficulties and when delivered by therapists without prior mindfulness training.
These limitations in relation to mindfulness parenting programs call for the development of mindfulness-based interventions that can be integrated effectively with PT and easily implemented in a community setting. Those mindfulness interventions should be so devised that they focus on the difficulties the parents typically experience with children with ADHD. Additionally, because mindfulness interventions are assumed to enhance the parents’ capacity to attend to and regulate their emotions, it will be important to evaluate whether the integration of mindfulness skills with PT can indeed enhance the impact of PT on parents’ affective processes as well as the child’s behavioral symptoms.
The Current Study
Parents’ capacity to regulate negative arousal has been identified as a significant contributor to their capacity to effectively manage the child’s arousal and therefore to benefit from PT. Nonetheless, still unclear is whether parents’ capacity to manage negative affect improves following PT and whether targeting parental ER directly produces a clinical benefit. Because previous research identified mindfulness skills as a possible avenue for improving parental ER, we were interested in developing a mindfulness based skills protocol that could be integrated with PT and in assessing whether the mindfulness-based skills augmentation can enhance parents’ capacity to regulate negative affect following PT.
To achieve these goals, we developed a short mindfulness-based skills protocol that focused on the parents’ capacity to use mindful awareness to regulate negative affect during routine interactions with their child. The protocol was integrated with PT in nonviolent resistance (NVR) for families of children with ADHD and behavior difficulties (Omer 2004). Using an RCT design, we assessed the impact of the mindfulness component on parents’ treatment outcomes (e.g., parents’ emotion regulation, negative emotions, and submissive and coercive behaviors), children’s outcomes (e.g., externalizing symptoms), and treatment attrition. We hypothesized that parents who received the mindfulness augmented PT would show improvement in their capacity to regulate negative affect compared with parents in the control PT group. We also hypothesized that parents in the mindfulness group would demonstrate a reduction in their own hostility, coercive behaviors, and submission to the child. Lastly, we hypothesized that the treatment incorporating mindfulness skills would lead to a greater reduction in child externalizing symptoms compared to the control treatment.
Method
Participants
Participants included 79 families (79 mothers and 73 fathers) enrolling in PT in NVR for ADHD and behavior disorders at a mental health outpatient clinic in a children’s hospital in Israel. The clinic specializes in PT for families of children with ADHD and behavior difficulties. Children of families accepted to treatment have an established diagnosis of ADHD from providers in the community. Inclusion/exclusion criteria were as follows: (a) the child was between 6 and 18 years old; (b) the child had no diagnosed intellectual deficit or history of psychosis; and (c) the primary referral problem was ADHD and child behavior problems occurring for more than 6 months (e.g., noncompliance, social aggression, and oppositional behaviors). In addition to the Child Behavior Checklist questionnaires, child ADHD symptoms and behavior difficulties were evaluated in an intake session conducted by a licensed clinical psychologists. At the intake session a complete anamnesis was collected and the ADHD diagnosis was verified. Each parent signed informed consent to participate in the study prior to completion of the questionnaires and the interview. Parents were informed that their decision to participate or withdraw from the study would not affect their treatment. The families paid for every therapy session and did not receive compensation for participation in the study. We planned to collect data for one year, in line with the training cycles of therapists at the clinic.
Among the participants in the study, 88% of parents were married and lived together, 7.6% of parents were divorced, and 5% were single parents. Most parents had more than 12 years of education (mothers M = 15.29, SD = 2.51; fathers M = 14.47, SD = 2.38). Children ranged in age from 6 to 15 years (M = 9.56, SD = 2.49), and 64.6% of children were 6–10 years old. The majority of children were boys (82.3%). Most children had one to three siblings (88.6%), and 12% of the children were in special education classes.
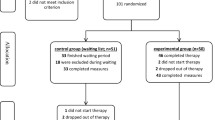
Of the 79 families that enrolled in the study, 22 families (27.84%) did not begin treatment. Reasons provided by families included symptom remission, a desire to begin treatment at a later time, and scheduling difficulties. Of families that began treatment, 12 (15.18%) terminated before the end of treatment. Reasons for termination included parental dispute (2), disagreement with the treatment approach (8), and parenting stress due to other family problems (2). A comparison conducted between families that completed and did not complete treatment revealed no significant differences in child’s age, child’s externalizing symptoms, parental level of escalation, or the parents’ capacity for emotion regulation. The attrition rate documented in the current study is typical for community clinics in which multiple barriers—including parenting stress, scheduling, financial concerns, and disengagement with treatment approach—prevent parents from attending and completing treatment (Kazdin et al. 1997). The flow of participants through the trial is described in Fig. 1.
Parent Training in NVR
Eligible families began PT in NVR, which is a manual-based intervention for behavior problems and ADHD that has been validated in previous studies and yielded significant improvement in child behavior symptoms and parental helplessness compared with a control group (Lavi-Levavi et al. 2013; Newman et al. 2014; Ollefs et al. 2009; Van Holen et al. 2016; Weinblatt and Omer 2008). Six Master’s level clinicians (with at least four years of clinical experience) and student assistants (who served as treatment supporters) conducted the treatment. All therapists were trained to administer the manualized treatment in a 3 day training seminar by the 3rd and 5th authors and received weekly supervision by the 5th author that assured their delivery effectiveness and adherence to the treatment protocol. As is typical for NVR treatment, we conducted 10–12 therapy sessions teaching parents non-escalation techniques, child management strategies, enhancement of parental presence at home, and improvement of community support (Omer 2004). The length of treatment was determined by the therapists in response to the family’s progress, and in relation to the time required for parents to implement the learned skills at home.
Mindfulness Based Skills Augmentation
In the experimental condition (nonviolent resistance and mindfulness; NVRM), a single 90-min mindfulness skills session was added at the third therapy session. The format of the mindfulness training was based on the mindfulness skills training module in dialectical behavior therapy (DBT; Linehan 1993) and the video This One Moment: Skills for Everyday Mindfulness (Linehan et al. 2000). We used a short-term, skills-based mindfulness augmentation because of the need to develop an addendum to treatment that would enhance PT within its short time frame and would enable parents to benefit from both the emotion regulation advantages of mindfulness skills (Neacsiu et al. 2014) and the parenting skills taught in PT. Additionally, we sought a mindfulness intervention that would not require prolonged training and that could be easily implemented at the clinic in the future with new therapists.
To assure that the mindfulness component was consistent with PT goals and language, we developed a pilot version of the model and administered it in the following sequence:
-
1.
The primary investigator wrote a protocol in Hebrew introducing mindfulness skills.
-
2.
Therapists and treatment supporters at the clinic screened the protocol, providing feedback and suggestions for improvements regarding the protocol’s applicability to parenting challenges and integration with the NVR treatment.
-
3.
We developed a parenting version of the protocol, which we then used in pilot sessions with three families.
-
4.
Based on feedback from therapists and families participating in the pilot group, we developed a final version of the protocol.
The main components taught in the mindfulness intervention are summarized in Table 1. The full protocol is available upon request from the first author.
Therapists participating in the study had no prior background in mindfulness. Therapists attended two training workshops conducted by the first author to learn how to administer the mindfulness intervention.Footnote 2 The training included live observations of the first author administering the mindfulness component to the pilot families. The training workshops also involved an experiential phase where therapists learned and practiced mindfulness skills themselves, and a didactic phase where therapists were trained to administer the mindfulness protocol to families. Therapists were encouraged, though not mandated, to practice their newly learned mindfulness skills in their daily life. Therapists began administering the mindfulness protocol once they felt comfortable with the concepts and exercises, and confident in their ability to deliver the protocol. To ensure adherence to the protocol, therapists reported to the primary investigator before and after each mindfulness session.
Procedures
Each participating parent completed study questionnaires (see the upcoming Measures section) before the intake meeting as part of the intake packet. Random, blind assignment to experiment (NVRM) and control (NVR) conditions was completed before intake (e.g., before information was collected on the families), using a random numbers table.
Parents assigned to the NVRM group received a 90-min mindfulness training during the third therapy session. The session was part of the treatment module teaching parents de-escalation techniques at the beginning of treatment. In this module, parents learned de-escalating techniques, such as delayed response, ignoring, taking notes, and distractions. The module, which lasts two to three sessions, focuses on parenting behaviors, does not address emotional processing, and is tailored to the specific escalating dynamic of each family. Families in the NVR condition received the regular anti-escalation module, whereas families in the NVRM condition received a revised version of the module that included the mindfulness skills. After piloting the mindfulness intervention and consulting with the therapists, the third session was chosen for administration of the mindfulness protocol. By the third session, therapists had some familiarity with the parents and a chance to address urgent concerns. Additionally, the administration of the mindfulness protocol at the third session enabled therapists to better integrate the mindfulness concepts with the de-escalation concepts that were taught during the second session, strengthening the rational of supplementing the treatment protocol with mindfulness skills.
At the end of the mindfulness session, parents participating in the NVRM group were provided with a homework sheet to record their practice during the subsequent weeks. Parents in the NVRM group were asked to report the number of times that they practiced mindfulness skills, and were reminded to bring the practice sheet to each therapy session. The therapist and treatment supporter encouraged the parents to use the mindfulness skills at home and helped parents that struggled to implement the skills to identify situations when they could practice them. During the last therapy session, each participating parent completed the same questionnaires.
All procedures performed in the study were approved by the institutional review board and by the Helsinki committee of the hospital where the study took place. An informed consent was obtained from all individual participants included in the study.
Measures
Parental ER
Parental capacity for ER was measured using the Difficulty in Emotion Regulation Scale (DERS; Gratz and Roemer 2004). The scale consists of 36 items. Higher scores indicate greater difficulties in emotion regulation, and the total score represents a global index of affect regulation difficulties. We received permission from the authors of the measure to translate the DERS to Hebrew, and conducted a translation validation using a translation back to English by an independent translator. The DERS was completed individually by each parent. In the current study Cronbach’s alphas for mothers and fathers were .89 and .93 respectively.
Parenting Behaviors
Parental negative feelings, escalating behaviors, and submitting behaviors toward their children were measured using the 21-item Escalation Questionnaire (Lavi-Levavi 2009). This measure yields four scores: Coercive Behavior, Negative Feelings, Parental Submission, and Parental Supervision. The measure was previously validated with parents receiving treatment in NVR and was found to be sensitive to treatment changes for both mothers and fathers (Lavi-Levavi et al. 2013). In the current study we excluded the Parental Supervision scale due to inadequate consistency levels. The Escalation Questionnaire was completed individually by each parent. Cronbach’s alphas for the remaining scales achieved a low to medium level of consistency (mothers’ coercive behavior α = .70; fathers’ coercive behavior α = .65; mothers’ negative feelings α = .79; fathers’ negative feelings α = .81; mothers’ submission α = .74; fathers’ submission α = .75).
Child Problem Behaviors
The parents’ perceptions of their child’s problem behaviors were assessed using the Externalizing scale of the Child Behavior Checklist (CBCL; Achenbach 1991). We used the Hebrew version of the questionnaire, which has shown good reliability and validity (Zilber et al. 1994). The CBCL was completed by the parents together. For the current study, Cronbach’s alpha for the Externalizing scale was α = .99.
Mindfulness Practice
Parents were asked to complete a daily practice sheet following the mindfulness session. The practice sheet was based on Linehan’s DBT practice sheet (Linehan 1993). Parents were instructed to mark on the practice sheet whether they used mindful observation and mindful description during the day, and were asked to bring the practice sheet with them to the following sessions. In the current study, despite recurrent encouragements by therapists and treatment supporters, few parents returned the practice sheet. As a result the practice sheet was not included in the data analysis.
Data Analysis Strategy
A multilevel linear modeling approach (MLM; in STATA 14) was used to assess changes in parenting and child variables across treatment conditions and time. The MLM approach was chosen as it offers several benefits over a traditional repeated measures ANOVA approach for a community sample. First, the MLM has higher tolerance to missing data as it models parameter estimates based on each available data point rather than on list-wise deletion of cases. Second, MLM makes no assumptions about normality of variables or balanced groups.
For the current data analysis, we used the MLM to estimate a restricted maximum-likelihood random-effects model with structured components of variance. Level 1 functioning variables over time from pre- to post-treatment were nested within individual mothers and fathers (within-person), and the treatment group was evaluated as a Level 2 (between-person) moderator of change over time. For estimates of effect sizes, a pseudo R-square statistic was calculated, which represents the percentage of the residual variance explained by the addition of the parameter of interest (Singer and Willett 2013); at Level 1 this represents each parent’s (within-person) change over time, and at Level 2 this represents differences in change between the treatments (between-person).
Results
Participants’ Flow and Group Comparisons at Baseline
Families in the NVR and NVRM conditions did not differ in terms of child’s age or parents’ education. No differences were observed between the NVR and NVRM conditions also in relation to child’s externalizing behaviors or in terms of parental emotion regulation, negative feelings, coercive behavior, and submission (see Table 2). An additional comparison of the number of sessions completed by the end of treatment revealed no difference in session number between families in the NVRM and NVR groups (t (40 (= −.31, p = .75); thus, on average, the mindfulness augmentation did not change the number of sessions that families completed. An additional post hoc analysis did not reveal any significant correlation between treatment length and family characteristics.
Consistent with our hypothesis, a Chi square analysis comparing families who terminated treatment earlier indicated a nonsignificant trend toward lower early termination in the NVRM condition (χ2(1, 57) = 2.12, p = .14). Early termination was defined as families that began treatment but did not complete it (e.g., arrived to at least one therapy sessions but decided to discontinue treatment). In the current sample beside one case of early termination due to parents’ dispute, families terminated after the 3rd session (the session where the mindfulness intervention was delivered).
Intervention-Related Improvement in Child and Parental Functioning
The MLM findings are summarized in Table 2.
Parental ER
Following the intervention, mothers across treatment conditions reported reduced emotional dysregulation (β = −7.01 (2.79), t = −2.51, p = .01); change over time represented 23% of the within-person variance. This reduction, however, was not moderated by treatment condition. For fathers, we found an interaction effect of Time × Treatment Condition (β = –10.22 (5.14), t = −1.99, p = .04); this treatment interaction explained 7% of between-person variance in change over time. Fathers in the NVRM condition experienced a greater decrease in paternal emotional dysregulation following treatment than did fathers in the NVR condition. The interaction effect is presented in Fig. 2.
Parenting Behaviors
Coercive Behavior Scale
Following intervention, mothers across treatment conditions reported a significant reduction in coercive behaviors (β = −2.37 (1.15), t = −2.07, p = .04); change over time represented 20% of the within-person variance. This reduction was not moderated by treatment condition. For fathers, we found no change in coercive behavior over time in either treatment condition.
Submission Scale
We found no significant change in mothers’ submission levels following intervention across treatment conditions. For fathers, we found an interaction effect of Time × Treatment Condition (β = −4.29 (2.17), t = −1.98, p = .04); this treatment interaction explained 4% of between-person variance in change over time. This indicates a greater decrease in paternal submission in the NVRM treatment condition (see Fig. 2).
Negative Feelings Scale
Mothers across treatment conditions reported a significant reduction in negative feelings following intervention (β = −3.05 (0.89), t = −3.41, p = .01); change over time represented 40% of the within-person variance. This reduction was not moderated by treatment condition. For fathers, we found a trend toward a reduction in negative feelings following intervention in both treatment conditions (β = −1.27 (0.75), t = −1.69, p = .09); change over time represented 35% of the within-person variance. Additionally, we found a trend for an interaction effect of Time × Treatment Condition (β = −1.79 (1.06), t = −1.69, p = .09); this treatment interaction explained 5% of between-person variance in change over time. This suggests a trend towards a greater decrease in paternal negative feelings in the NVRM treatment condition (see Fig. 2).
Child Problem Behaviors
Following intervention, parents across treatment conditions reported a significant reduction in child externalizing symptoms on the CBCL externalizing scale (β = −4.73 (1.56), t = −3.04, p = .002); change over time represented 51% of the within-person variance. This reduction was not moderated by treatment condition.
Discussion
In this study, we sought to assess the impact of integrating mindfulness-based skills with PT in NVR for children with ADHD and behavior difficulties. The mindfulness component was designed as an augmentation of PT in NVR and tailored so as to match the specific program and treatment population. Using an RCT design, we compared the efficacy of NVR with NVRM. We expected that families receiving mindfulness skills in addition to NVR would show greater improvement in parental capacity for emotion regulation; reduced parental hostility, coerciveness, and submission; and greater reported reduction in child behavioral symptoms. Our findings provided mixed results in relation to the effectiveness of mindfulness-enhanced PT. We found no group differences in the parents’ report of reduction in child behavior problems, maternal emotion dysregulation, maternal negative feelings, and maternal coercive behaviors. For fathers, however, small but significant treatment effects emerged with regard to changes in paternal emotion dysregulation, paternal submission, and paternal hostility, suggesting that fathers may receive improved benefits from PT following the addition of mindfulness skills.
The findings that both NVR and NVRM significantly reduced parents’ reported child externalizing symptoms and improved maternal reports of negative affect and escalating behaviors provide further support for the effectiveness of PT in NVR in families of children with ADHD, both in terms of child-related reported symptoms and maternal processes. The moderate effects we found for reductions in parental report of their child’s externalizing symptoms is consistent with previous studies of NVR (Lavi-Levavi et al. 2013; Weinblatt and Omer 2008) as well as other forms of behavioral PT for families of children with ADHD (Bjørnebekk et al. 2015). A previous meta-analysis of behavioral PT for children with ADHD reported on average a moderate effect size (r = .34, k = 40) for treatment compared to controls or waitlist. The effect sizes were reported for child symptoms and for parents’ behaviors (Lee et al. 2012).
Additionally, our study results show that, although not directly addressed in PT, mothers’ capacity to regulate negative affect can improve significantly and with moderate effects following treatment. This finding provides further evidence for the positive impact of PT in NVR on distal parenting processes. It is consistent with Colalillo and Johnston’s (2016) review of PT, which suggested that the benefits from participating in PT may extend beyond child-related symptoms and can positively improve maternal experiences of parenting as well as maternal cognitive and affective processes. The results reported by Colalillo and Johnston (2016) indicated an average reduction in maternal parenting stress from the 78th to the 53rd percentile in the intervention group.
Our results show that, unlike mothers who seemed to improve significantly following treatment, fathers in the control condition showed minimal improvement in their capacity for emotion regulation, coercive behaviors, or negative feelings following treatment. For fathers, small but significant effects were observed in improvements in cognitive and affective processes only in the NVRM condition. The limited impact of PT on fathers is consistent with previous research that compared paternal and maternal reactions to PT. Research has repeatedly indicated that fathers are less involved in PT and, when involved, often report less improvement compared with mothers and describe treatment as less relevant for addressing their parenting needs (Gershy & Omer, 2017;Lundahl et al. 2006; Panter-Brick et al. 2014). Our finding that mindfulness training may improve paternal processes following treatment was indicated in previous studies on mindfulness parenting programs. Van de Weijer-Bergsma et al. (2012) reported that following an eight-week program of MBCT administered to parents of adolescents with ADHD, fathers (but not mothers) showed a significant reduction in parenting stress. Coatsworth et al. (2015) assessed a mindfulness-enhanced parenting program and found that fathers in the mindfulness-enhanced condition, but not mothers, demonstrated small to moderate level of improvement in emotional awareness and compassionate acceptance of their child.
The literature on paternal affective processes during parent–child conflict offers a preliminary explanation of our findings. Marceau et al. (2015) found that fathers’ adaptive coping during parent–child conflict often included a problem-solving strategy, whereas mothers tended to use a more emotion-focused coping strategy. In reaction to a child who coped with conflict in an angry/hostile way, fathers tended to respond in an angry/hostile way (i.e., to deviate from their usual problem-solving coping strategies), whereas mothers continued using an emotion-focused coping strategy. DeKlyen et al. (1998) found that fathers’ responses to their children’s behavioral transgressions tended to vacillate between punitive reactions and disengagement. In contrast, mothers maintained contact with their child even when the relationship was hostile. Given these findings, perhaps the mindfulness skills taught in our study provided fathers with a concrete and applicable strategy to manage negative affect. This strategy, when applied successfully, may enable fathers to reduce their emotional reactivity and consequently improve their capacity to solve problems without reverting to punishment or disengagement (DeKlyen et al. 1998; Roemer et al. 2015).
The following example demonstrates this process. A father in the NVRM condition used to lose control and lash out at his 8-year-old son every time the son ignored his request to go to bed. The father described feeling humiliated and helpless in changing his son’s reaction, which lead him to respond with hostility and anger that grew over time. The father explained that after the mindfulness training, when his son refused his request to go to bed, he went himself to the child’s bedroom, laid down near the bed, practiced mindful breathing, and waited patiently until the child calmed down and joined him. The father reported that he knew the child had difficulty transitioning to sleep, but only after learning to manage his emotional reaction using the mindfulness skills was he able to allow the child to wind down gradually without becoming enraged by his initial refusal. Although anecdotal, this scenario illustrates a potential mechanism by which the added mindfulness component may have helped fathers to implement PT more successfully by providing them with a clear strategy to detect and manage their own emotional reactivity.
The improvement we observed in mothers’ emotional reactivity across treatment conditions suggests that other therapeutic components of NVR may have been effective in reducing maternal reactivity and in increasing their regulation of negative affect. Possible regulatory mechanisms in the NVR may involve the increased family and community support that mothers received during conflicts with the child, as well as de-escalation strategies that provided mothers with permission to respond to the child’s negative behaviors at a later time, when they feel better equipped to respond. Perhaps these mechanisms expanded the emotional resources available to the mothers during conflict with the child and therefore enabled them to experience the conflict as less stressful and more manageable. In line with this assumption there is a possibility that introducing the mindfulness augmentation to mothers at a later stage of treatment- when they feel more supported and less dysregulated- could increase their benefit from the mindfulness skills.
Evaluation of the Mindfulness Intervention
We based our mindfulness protocol on Marsha Linehan’s mindfulness intervention for borderline personality disorder. The skills base and practical focus of Linehan’s model seemed to fit the challenging requirements of the PT context: a short-term treatment that emphasizes behavioral change; parents who are interested in creating change but mostly focus on the child’s behavior and emotional difficulties; and therapists with limited exposure to mindfulness training and practice. We assumed that the model of MBCT that involves daily practice of mindfulness skills and longer training duration (around 12 weeks) would be incongruous with the characteristics of the families seen at the clinic and the already heavy assignment load for parents in PT.
Our findings suggest that small but significant effects for fathers can also be achieved with a short, skills-based mindfulness intervention weaved into an effective PT program. Nevertheless, because our skills-based approach to mindfulness is not as extensive as typical mindfulness-based parenting programs, our intervention may be criticized for delivering an insufficient dosage of mindfulness instruction and practice—a limitation that may account for the lack of significant differences between the groups in relation to reported child symptoms and maternal measures. Moreover, as we were not able to collect practice sheets to measure the frequency of mindfulness skills practice, it was difficult to assess the extent to which parents utilized the mindfulness skills, or to evaluate a possible relationship between skill utilization and treatment change.
To date, only one published study (Coatsworth et al. 2015) evaluated the clinical utility of adding mindfulness skills to PT, comparing mindfulness enhanced PT, standard PT, and a control condition. The effect sizes reported by Coatsworth et al. (2015) indicated small to medium effect sizes for treatment versus control group (d = .18−.25) for both child and parents measures. Nonetheless, consistent with our findings, the effect sizes for the comparison between the mindfulness enhanced PT and standard PT conditions yielded inconsistent results. While for mothers no effects were indicated, for father small to moderate effects were reported in the areas of mindfulness in parenting and relationship quality (d = .27−.36).
Additional explanations for our mixed results may be related to the methodological challenge of assessing the effectiveness of treatment augmentation. Kazdin (2005) challenged the usefulness of adding additional modules like stress-reduction interventions, arguing that because only some families need additional interventions, treatment augmentations are of little utility for a larger group of participants, making it difficult to show the effectiveness of these augmentations compared with the regular intervention. A review by Maliken and Katz (2013) supports the argument that stress-reduction treatment augmentations demonstrate inconsistent benefits and that it is generally difficult to show significant differences between the augmented and the standard treatments. Maliken and Katz suggested two reasons for these findings. First, the recruitment for PT is based on the child’s psychopathology and not the parents’ psychopathology, making it difficult to tailor the treatment’s augmentation to the population of parents who may benefit from it the most. Second, it is difficult to address parents’ emotional difficulties in a short-term intervention without overburdening the treatment and creating a further barrier for the treatment’s completion. According to Maliken and Katz, for the parents who suffer from significant emotional distress, spending so few treatment hours to address their own emotions may not be sufficient to create a meaningful change.
An example from our study demonstrates Maliken and Katz’s second argument. One of the participants in the mindfulness group was a single mother who presented symptoms of major depression at intake. The mother was interested in the mindfulness-based intervention and seemed to benefit from practicing mindfulness at home. Nevertheless, the positive experience was not sufficient to address her high level of emotional dysregulation, and she eventually dropped out of treatment. This case example highlights the variability in parenting needs in relation to treatment augmentation, and the challenges in tailoring the dosage of the augmentation to particular parenting needs. In order to show the effectiveness of mindfulness-based treatment augmentation, we may need to identify a subgroup of parents who are in higher need for such intervention and to tailor the dosage of the added intervention to fit their unique parenting characteristics and needs.
Finally, there is a need to note some cultural aspects related to the implementation of mindfulness skills with the current sample of Israeli families. A frequent concern voiced by parents in the study was related to the association of mindfulness skills with yoga practice and meditation, practices some parents perceived negatively as “spiritual”, “new age”, or foreign to the parents’ cultural values. To overcome this worry, in teaching the mindfulness concepts there was a need to focus on the practicality of the skills for parenting and to avoid referring to mindfulness as a way of life. This approach helped dismantle some of the initial resistance we encountered in families learning the mindfulness concepts and improved engagement with the mindfulness exercises during the third session.
Limitations and Future Directions
The current study was conducted at an outpatient clinic for children with ADHD and behavior difficulties. Although this provided us with a naturalistic sample of families referred for treatment with an acute need for intervention, this sample has several limitations. First, the statistical power of the study was limited because of the attrition rate and small sample size of families who completed treatment. Second, although substantial attrition is expected in a setting such as ours, we cannot rule out the possibility that families who did not begin treatment share unique characteristics that were not captured in our sample and may have responded differently to the mindfulness augmentation. Third, the lack of a waitlist or treatment-as-usual control condition (i.e., versus our active intervention comparison condition) reduces our capacity to rule out maturational effects as an explanation for observed changes over the treatment duration. Finally, our sample represented a limited demographic. Families who participated in the study were mostly two-parent households with working parents who were able to pay for treatment. The sample did not include families from lower socioeconomic statuses for whom higher levels of external stress may contribute to different responses to the mindfulness intervention. Additionally, conclusions are limited by our reliance on parents’ reports of both parenting behaviors and child symptoms and by the multiple comparisons that raise the Type I error rate (6 significant results out of 27 comparisons). An additional RCT with a larger group of participants from more diverse socioeconomic backgrounds, a third waitlist condition, and an observational measure of parenting behavior would allow a more thorough assessment of the efficacy of our program. A larger sample would also enable an assessment of the impact of mindfulness augmentation on families with high versus low stress levels, as well as for families with varying coping strategies at baseline.
Furthermore, the varied response to mindfulness skills observed in our study suggests that the utility of targeting parents’ emotion regulation may require a more individualized approach that links the skill to the parent’s coping style, as well as their available emotional resources(Teasdale, Segal & Williams, 2003). Future research should further develop mindfulness interventions for use in conjunction with PT while systematically assessing new directions for implementing such protocols. Consistent with directions calling for the use of a tailored, modular approach to address particular family needs instead of a standard, manualized program, these directions may include, for example, developing an elastic mindfulness protocol with extended flexibly when working with parents who have great need for emotion regulation treatment (Bearman & Weisz, 2015). Tailoring mindfulness training to specific families may capitalize on the important contribution of mindfulness skills training that we observed for some parents in our sample, and enable therapists to offer an adequate dosage of mindfulness practice to specific parents without overburdening standard PT treatment protocols.
Conclusions
The current study suggests that mothers’ capacity for emotion regulation can be effectively targeted in PT in NVR and that mindfulness-based skills augmentation may be an efficient mechanism by which to target paternal emotion regulation and improve treatment outcomes for fathers.
Notes
The first author’s prior experience with mindfulness involved the study and practice of mindful meditation, training in mindfulness at the school setting and administration of mindfulness groups with adolescents.
References
Achenbach, T. M. (1991). Manual for the Child behavior checklist. Burlington: University of Vermont, Department of Psychiatry.
Bearman, S. K., & Weisz, J. R. (2015). Review: Comprehensive treatments for youth comorbidity–evidence-guided approaches to a complicated problem. Child and adolescent mental health, 20(3), 131–141. doi:10.1111/camh.12092.
Beauchaine, T. P., Webster-Stratton, C., & Reid, M. J. (2005). Mediators, moderators and predictors of 1-year outcomes among children treated for early-onset conduct problems: A latent growth curve analysis. Journal of Consulting and Clinical Psychology, 73(3), 371–388. doi:10.1037/0022-006X.73.3.371.
Ben-Porath, D. D. (2010). Dialectical behavior therapy applied to parent skill training: Adjunctive treatment for parents with difficulties in affect regulation. Cognitive and Behavioral Practice, 17(4), 458–465. doi:10.1016/j.cbpra.2009.07.005.
Bjørnebekk, G., Kjøbli, J., & Ogden, T. (2015). Children with conduct problems and co-occurring ADHD: Behavioral improvements following parent management training. Child & Family Behavior Therapy, 37(1), 1–19. doi:10.1080/07317107.2015.1000227.
Bögels, S., Hellemans, J., van Deursen, S., Römer, M., & van der Meulen, R. (2014). Mindful parenting in mental health care: Effects on parental and child psychopathology, parental stress, parenting, coparenting, and marital functioning. Mindfulness, 5, 536–551. doi:10.1007/s12671-013-0209-7.
Bridgett, D. J., Burt, N. M., Edwards, E. S., & Deater-Deckard, K. (2015). Intergenerational transmission of self-regulation: A multidisciplinary review and integrative conceptual framework. Psychological Bulletin, 141(3), 602–654. doi:10.1037/a0038662.
Burt, S. A., Krueger, R. F., McGue, M., & Iacono, W. (2003). Parent-child conflict and the comorbidity among childhood externalizing disorders. Archive of Genetic Psychiatry, 60(5), 505–513. doi:10.1001/archpsyc.60.5.505.
Cavell, T. A., Harrist, A. W., & Del Vecchio, T. (2013). Working with parents of aggressive children: Ten principles and the role of authoritative parenting. In R. E. Larzelere, A. S. Morris, & A. W. Harrist (Eds.), Authoritative parenting: Synthesizing nurturance and discipline for optimal child development (pp. 165–188). Washington, DC: American Psychological Association.
Chacko, A., Wymbs, B. T., Wymbs, F. A., Pelham, W. E., Swanger-Gagne, M. S., Girio, E., et al. (2009). Enhancing traditional behavioral parent training for single mothers of children with ADHD. Journal of Clinical Child & Adolescent Psychology, 38(2), 206–218. doi:10.1080/15374410802698388.
Coatsworth, J. D., Duncan, L. G., Nix, R. L., Greenberg, M. T., Gayles, J. G., Bamberger, K. T., et al. (2015). Integrating mindfulness with parent training: Effects of the mindfulness-enhanced strengthening families program. Developmental Psychology, 51(1), 26–35. doi:10.1037/a0038212.
Colalillo, S., & Johnston, C. (2016). Parenting cognition and affective outcomes following parent management training: A systematic review. Clinical Child and Family Psychology Review, 19(3), 216–235. doi:10.1007/s10567-016-0208-z.
DeKlyen, M., Speltz, M. L., & Greenberg, M. T. (1998). Fathering and early onset conduct problems: Positive and negative parenting, father–son attachment, and the marital context. Clinical Child and Family Psychology Review, 1(1), 3-21. doi:10.1023/A:1021844214633
Drabick, D. A. G., Gadow, K. D., & Sprafkin, J. (2006). Co-occurrence of conduct disorder and depression in a clinic-based sample of boys with ADHD. Journal of Child Psychology and Psychiatry, 47, 766–774. doi:10.1111/j.1469-7610.2006.01625.x.
Dumas, J. E. (2005). Mindfulness-based parent training: Strategies to lessen the Grip of automaticity in families with disruptive children. Journal of Clinical Child & Adolescent Psychology, 34, 779–791. doi:10.1207/s15374424jccp3404_20.
Duncan, L. G., Coatsworth, J. D., & Greenberg, M. T. (2009). A model of mindful parenting: implications for parent-child relationships and prevention research. Clinical Child and Family Psychological Review, 12(3), 255–270. doi:10.1007/s10567-009-0046-3.
Eames, C., Crane, R., Gold, E., & Pratt, S. (2015). Mindfulness-based wellbeing for socio-economically disadvantaged parents: a pre-post pilot study. Journal of Children’s Services, 10(1), 17–28. doi:10.1108/JCS-09-2014-0040.
Erisman, S. M., & Roemer, L. (2010). A preliminary investigation of the effects of experimentally induced mindfulness on emotional responding to film clips. Emotion, 10(1), 72–82. doi:10.1037/a0017162.
Evans, S. W., Owens, J. S., & Bunford, N. (2014). Evidence based psychosocial treatments for children and adolescents with attention-deficit/hyperactivity disorder. Journal of Clinical Child & Adolescent Psychology, 43(4), 527–551. doi:10.1080/15374416.2013.850700.
Gardner, F., Hutchings, J., Bywater, T., & Whitaker, C. (2010). Who benefits and how does it work? Moderators and mediators of outcome in an effectiveness trial of a parenting intervention. Journal of Clinical Child & Adolescent Psychology, 39(4), 568–580. doi:10.1080/15374416.2010.486315.
Gershy, N., & Omer, H. (2017). Can we have the session without the father? A qualitative study of father-resistance and a data-informed model of father-recruitment. Journal of Family Psychotherapy, 28(1), 38–58. doi:10.1080/08975353.2017.1283143.
Granic, I., O’Hara, A., Pepler, D., & Lewis, M. (2007). A dynamic systems analysis of parent–child changes associated with successful “real-world” interventions for aggressive children. Journal of Abnormal Child Psychology, 35(5), 845–857. doi:10.1007/s10802-007-9133-4.
Gratz, K., & Roemer, L. (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment, 26(1), 41–54. doi:10.1023/B:JOBA.0000007455.08539.94.
Halligan, S. L., Cooper, P. J., Fearon, P., Wheeler, S. L., Crosby, M., & Murray, L. (2013). The longitudinal development of emotion regulation capacities in children at risk for externalizing disorders. Development and Psychopathology, 25(2), 391–406. doi:10.1017/S0954579412001137.
Haydicky, J., Shecter, C., Wiener, J., & Ducharme, J. (2015). Evaluation of MBCT for adolescents with ADHD and their parents: Impact on individual and family functioning. Journal of Child and Family Studies, 24(1), 76–94. doi:10.1007/s10826-013-9815-1.
Hayes, A. M., & Feldman, G. (2004). Clarifying the construct of mindfulness in the context of emotion regulation and the process of change in therapy. Clinical Psychology: Science and Practice, 11(3), 255–262. doi:10.1093/clipsy.bph080.
Kabat-Zinn, J. (1990). Full catastrophe living: How to cope with stress, pain and illness using mindfulness meditation. London: Pitakus.
Kazdin, A. E. (1997). Parent management training: evidence, outcomes, and issues. Journal of the American Academy for Child and Adolescent Psychiatry, 36(10), 1349–1356. doi:10.1097/00004583-199710000-00016.
Kazdin, A. E. (2005). Parent management training: Treatment for oppositional aggressive and antisocial behavior in children and adolescents. New York: Oxford University Press.
Kazdin, A. E., Holland, L., & Crowley, M. (1997). Family experience of barriers to treatment and premature termination from child therapy. Journal of Consulting and Clinical Psychology, 65(3), 453–463. doi:10.1037/0022-006X.65.3.453.
Kolko, D. J., Dorn, L. D., Bukstein, O. G., Pardini, D., Holden, E. A., & Hart, J. (2009). Community versus clinic-based modular treatment of children with early-onset ODD or CD: A clinical trial with 3-year follow-up. Journal of Abnormal Child Psychology, 37(5), 591–609. doi:10.1007/s10802-009-9303-7.
Kumar, S., Feldman, G., & Hayes, A. (2008). Changes in mindfulness and emotion regulation in an exposure-based cognitive therapy for depression. Cognitive Therapy and Research, 32(6), 734–744. doi:10.1007/s10608-008-9190-1.
Laugesen, B., & Grønkjær, M. (2015). Parenting experiences of living with a child with attention deficit hyperactivity disorder: a systematic review of qualitative evidence. JBI Database of Systematic Reviews and Implementation Reports, 13(11), 169–234. doi:10.11124/jbisrir-2015-2449.
Lavi- Levavi, I. (2009). Improvement in systemic intra-familial variables by “Non- violent resistance” treatment for parents of children and adolescents with behavioral problems. Unpublished doctoral dissertation, Tel Aviv University, Tel Aviv, Israel.
Lavi-Levavi, I., Shachar, I., & Omer, H. (2013). Training in nonviolent resistance for parents of violent children: Differences between fathers and mothers. Journal of Systemic Therapies, 32, 79–93. doi:10.1521/jsyt.2013.32.4.79.
Lee, P. C., Niew, W. I., Yang, H. J., Chen, V. C. H., & Lin, K. C. (2012). A meta-analysis of behavioral parent training for children with attention deficit hyperactivity disorder. Research in Developmental Disabilities, 33(6), 2040–2049. doi:10.1016/j.ridd.2012.05.011.
Leerkes, E. M., Supple, A. J., O’Brien, M., Calkins, S. D., Haltigan, J. D., Wong, M. S., et al. (2015). Antecedents of maternal sensitivity during distressing tasks: Integrating attachment, social information processing, and psychobiological perspectives. Child Development, 86(1), 94–111. doi:10.1111/cdev.12288.
Linehan, M. M. (1993). Cognitive-behavioral treatment of borderline personality disorder. New York: Guilford Press.
Linehan, M. M., Waltz, J., Dimeff, L., & Koerner, K. (2000). This one moment: skills for everyday mindfulness. Seattle: The Behavioral Technology Transfer Group.
Lundahl, B., Risser, H. J., & Lovejoy, M. C. (2006). A meta-analysis of parent training: Moderators and follow-up effects. Clinical Psychology Review, 26(1), 86–104. doi:10.1016/j.cpr.2005.07.004.
Maliken, A., & Katz, L. (2013). Exploring the impact of parental psychopathology and emotion regulation on evidence-based parenting interventions: A transdiagnostic approach to improving treatment effectiveness. Clinical Child and Family Psychology Review, 16(2), 173–186. doi:10.1007/s10567-013-0132-4.
Marceau, K., Zahn-Waxler, C., Shirtcliff, E. A., Schreiber, J. E., Hastings, P., & Klimes-Dougan, B. (2015). Adolescents’, mothers’, and fathers’ gendered coping strategies during conflict: Youth and parent influences on conflict resolution and psychopathology. Development and Psychopathology, 27(4), 1025–1044. doi:10.1017/S0954579415000668.
Melnick, S., & Hinshaw, S. (2000). Emotion regulation and parenting in AD/HD and comparison boys: Linkages with social behaviors and peer preference. Journal of Abnormal Child Psychology, 28(1), 73–86. doi:10.1023/A:1005174102794.
Molgaard, V. M., Kumpfer, K. L., & Fleming, E. (2001). The strengthening families program: For parents and youth 10–14; A videobased curriculum. Ames, IA: Iowa State University Extension.
Neacsiu, A. D., Bohus, M., & Linehan, M. M. (2014). Dialectical behavior therapy: An intervention for emotion dysregulation. In J. J. Gross (Ed.), Handbook of emotion regulation (pp. 491–507). New York: Guilford publications.
Newman, M., Fagan, C., & Webb, R. (2014). Innovations in practice: The efficacy of nonviolent resistance groups in treating aggressive and controlling children and young people: A preliminary analysis of pilot NVR groups in Kent. Child and Adolescent Mental Health, 19(2), 138-141. doi: 10.1111/camh.12049.
Ollefs, B., Schlippe, A. V., Omer, H., & Kriz, J. (2009). Youngster with externalizing behavior problems: Effects of parent training. Familiendynamik, 34, 256–265. (in German).
Omer, H. (2004). Nonviolent resistance. A new approach to violent and self-destructive children. Cambridge: Cambridge University Press.
Panter-Brick, C., Burgess, A., Eggerman, M., McAllister, F., Pruett, K., & Leckman, J. F. (2014). Practitioner review: Engaging fathers—recommendations for a game change in parenting interventions based on a systematic review of the global evidence. Journal of Child Psychology and Psychiatry, 55(11), 1187–1212. doi:10.1111/jcpp.12280.
Roemer, L., Williston, S. K., & Rollins, L. G. (2015). Mindfulness and emotion regulation. Current Opinion in Psychology, 3, 52–57. doi:10.1016/j.copsyc.2015.02.006.
Rutherford, H. J. V., Wallace, N. S., Laurent, H. K., & Mayes, L. C. (2015). Emotion regulation in parenthood. Developmental Review, 36, 1–14. doi:10.1016/j.dr.2014.12.008.
Segal, Z. V., Williams, J. M. G., & Teasdale, J. D. (2012). Mindfulness-based cognitive therapy for depression. New York: Guilford Press.
Singer, J. D., & Willett, J. B. (2013). Applied longitudinal data analysis: Modeling change and event occurrence. New York: Oxford University Press.
Singh, N. N., Singh, A. N., Lancioni, G. E., Singh, J., Winton, A. S. W., & Adkins, A. D. (2010). Mindfulness training for parents and their children with ADHD increases the children’s compliance. Journal of Child and Family Studies, 19(2), 157–166. doi:10.1007/s10826-009-9272-z.
Teasdale, J. D., Segal, Z. V., & Williams, J. M. G. (2003). Mindfulness training and problem formulation. Clinical Psychology: Science and Practice, 10(2), 157–160. doi:10.1093/clipsy.bpg017.
Townshend, K., Jordan, Z., Stephenson, M., & Tsey, K. (2016). The effectiveness of mindful parenting programs in promoting parents’ and children’s wellbeing: a systematic review. JBI Database of Systematic Reviews and Implementation Reports, 14(3), 139–180. doi:10.11124/JBISRIR-2016-2314.
van de Weijer-Bergsma, E., Formsma, A., de Bruin, E., & Bögels, S. (2012). The effectiveness of mindfulness training on behavioral problems and attentional functioning in adolescents with ADHD. Journal of Child and Family Studies, 21(5), 775–787. doi:10.1007/s10826-011-9531-7.
van der Oord, S., Bögels, S., & Peijnenburg, D. (2012). The effectiveness of mindfulness training for children with ADHD and mindful parenting for their parents. Journal of Child and Family Studies, 21(21), 139–147. doi:10.1007/s10826-011-9457-0.
Van Holen, F., Vanderfaeillie, J., & Omer, H. (2016). Adaptation and evaluation of a nonviolent resistance intervention for foster parents: A progress report. Journal of marital and family therapy, 42(2), 256–271. doi:10.1111/jmft.12125.
Weinblatt, U., & Omer, H. (2008). Nonviolent resistance: A treatment for parents of children with acute behavior problems. Journal of Marital & Family Therapy., 34(1), 75–92. doi:10.1111/j.1752-0606.2008.00054.x.
Zilber, N., Auerbach, J., & Lerner, Y. (1994). Israeli norms for the Achenbach Child Behavior Checklist: Comparison of clinically-referred and non-referred children. Israeli Journal of Psychiatry and Related Sciences, 31, 5–12.
Acknowledgements
We would like to thank the therapists at the Clinic for Systems Based Treatment for ADHD at Schneider Children Hospital for their important contribution to the development of the mindfulness protocol and for their enthusiasm to implement it in their work. We are also thankful to Michael Partas and Eyal Ronen Ackerman for their help with data collection and data analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in this study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Gershy, N., Meehan, K.B., Omer, H. et al. Randomized Clinical Trial of Mindfulness Skills Augmentation in Parent Training. Child Youth Care Forum 46, 783–803 (2017). https://doi.org/10.1007/s10566-017-9411-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10566-017-9411-4