Abstract
Prognosis from pancreatic ductal adenocarcinoma (PDAC) continues to be poor despite the many efforts channeled to improve its management. Although the mainstay treatment is still traditional chemotherapy, recent advances highlighted a promising potential for targeted therapy in the management of this disease. Those advances emphasize the significance of timely genomic profiling of tumor tissue as well as germline testing of patients to identify potential markers of targeted therapy. While targeted therapy is reserved for a relatively small subset of patients with PDAC, ongoing research is uncovering additional markers, and targeted agents, that will hopefully translate to better outcomes for patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
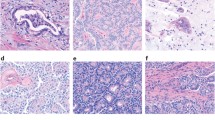
Pancreatic ductal adenocarcinoma (PDAC) comprises 85% of pancreatic malignancies [1]. The three precursor lesions are pancreatic intraepithelial neoplasia (PanIN), mucinous cystic neoplasm (MCN), and intraductal papillary mucinous neoplasms (IPMN) [2]. Progression to adenocarcinoma is driven by genetic mutations and alterations of the surrounding stroma including the extracellular matrix, immune cells, stromal cells, and cytokines [3,4,5]. Treatment of pancreatic adenocarcinoma has been a challenge. The poor prognosis of advanced/metastatic disease with conventional chemotherapy triggered the research on molecular pathogenesis and targeted therapies. This review describes these molecular drivers, the development of specific targeted therapy, and the ongoing research.
A number of drivers govern the development of pancreatic ductal adenocarcinoma and act by different mechanisms: (1) activation of signal transduction leading to cell proliferation by inducing function of oncogenes or their receptors and activation of downstream pathways, (2) inducing angiogenesis, (3) inhibition of tumor suppressors, (4) inactivation of mismatch repair genes, (5) JAK/STAT pathway, (6) changes in embryonal pathways, (7) telomerase shortening, (8) an altered immune cell activity, and (9) stromal reaction. This article reviews the highlights of molecular targets and potential therapies of drivers inside the cell from cell membrane down to the nucleus.
At the cell membrane, multiple receptors play a role in PDAC including epidermal growth factor receptor (EGFR), insulin-like growth factor receptor (IGFR), vascular endothelial growth factor receptor (VEGFR), human epidermal growth factor receptor-2 (Her-2), cytokine receptor/JAK-STAT, and the embryonic pathway receptors. Each of these receptors, when activated, acts through a signal transduction pathway controlling aspects of cell function, proliferation, and survival.
Intracellular signal transduction pathways are composed of sequence of multiple proteins that transmit the signal from the cell membrane proteins down to the nucleus. These include RAS/RAF/MEK/ERK pathway, PI3K/Akt/mTOR pathway, JAK/STAT pathway, and TGF-B/SMAD4 pathway.
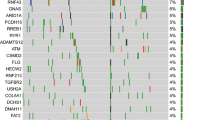
Inside the nucleus, multiple molecular drivers are identified in PDAC. Loss of function of tumor suppressor genes, such as P53 and P16, mismatch repair genes, or Fanconi anemia family DNA repair, can be molecular drivers for development of PDAC. Figure 1 shows the molecular drivers in the development pancreatic ductal adenocarcinoma.
2 At the cell membrane
2.1 Epidermal growth factor receptor
Epidermal growth factor receptor (EGFR) is a transmembrane glycoprotein with tyrosine kinase component that belongs to the ErbB family. Ligands, including EGF and transforming growth factor-alpha, activate it and trigger intracellular signaling pathways including RAS/PI3K/Akt and RAS/RAF/MAPK/ERK that regulate cell proliferation and survival [6]. EGFR-activating mutations, ligand overexpression, or increased receptor density on the cellular membrane lead to over-activation of its pathway. EGFR is encoded by c-ERBB-1 proto-oncogene located on the short arm of chromosome 7. It is overexpressed in almost 85% of PDAC and was found to correlate with aggression, metastasis, and recurrence [7,8,9,10]. Targeting the EGFR receptor and its pathway has been extensively studied.
In 2007, the FDA approved the EGFR inhibitor erlotinib as first-line treatment of locally advanced, unresectable or metastatic PDAC in combination with gemcitabine based on the results of the phase III trial that showed a prolonged overall survival (OS) with the combination of erlotinib/gemcitabine compared to gemcitabine alone. Median OS (mOS) was 6.24 months vs. 5.91 months [11]. Although statistically significant, this benefit was not clinically relevant and not practice changing. We do not use this combination in our practice. Other EGFR targeting agents were evaluated in PDAC without benefit. Table 1 demonstrates a summary of clinical trials targeting EGFR.
With receptor inhibition, feedback activation of different pathways can lead to treatment resistance. Blocking different pathways for synergism has also been studied. Possible synergy between EGFR inhibitors and inhibitors of the STAT3 pathway has been studied. Preclinical studies using Rhein, a lipophilic anthraquinone extracted from multiple herbs, suggested sensitizing the PDAC cells to EGFR inhibitors by blocking the STAT3 pathway [15]. Another study demonstrated that blocking the STAT3 pathway by simultaneous inhibition of EGFR with erlotinib and Src-kinase inhibition helps overcome resistance to gemcitabine by remodeling tumor stroma and enhancing gemcitabine delivery to the cells [16]. Most recently, a preclinical mice study confirmed this finding and demonstrated decreased stromal fibrosis and prolonged survival in mice with PDAC using the Src inhibitor dasatinib and the EGFR inhibitor erlotinib [17].
Cetuximab was extensively studied in PDAC. A recently published systematic review and meta-analysis screened 568 publications, included a total of four randomized controlled trials with 924 patients [18,19,20,21], and revealed no improvement in OS, PFS, or objective response by adding cetuximab to standard therapy of PDAC [22].
2.2 Vascular endothelial growth factor
Vascular endothelial growth factor (VEGF) belongs to the platelet-derived growth factor family. It plays a pivotal role in the regulation of pathologic vascular and endothelial cell growth and enhancing vascular permeability [33]. The goal of targeting it is to control tumor angiogenesis and progression. Multiple trials evaluated that the role of VEGF and VEGF receptor inhibitors were not successful in demonstrating a clinical benefit. Table 2 summarizes these clinical trials.
In 2005, a phase II study evaluated the use of bevacizumab, an anti-VEGF monoclonal antibody, in combination with gemcitabine in previously untreated advanced pancreatic cancer. mOS was 8.8 months, and the median progression-free survival (mPFS) was 5.4 months [34]. Unfortunately, a randomized phase III trial did not show improved survival [35].
2.3 Human epidermal receptor 2
HER2, also called erbB-2, is encoded by the ERBB2 gene [42]. It is different from other HER receptors due to lack of a specific ligand. It is activated by homo- or hetero-dimerization with other HER receptors or insulin-like growth factor receptor (IGFR) leading to auto-phosphorylation of the tyrosine kinase cytoplasmic portion. HER2 overexpression is identified variably in PDAC, detected in 21–80% of cases by IHC [43,44,45,46].
A number of attempts have been made to target HER2. Lapatinib, a small molecule inhibitor of HER2, was evaluated in a phase II trial combined with gemcitabine in the treatment of metastatic disease. No benefit was demonstrated [47]. Another phase II trial added lapatinib to capecitabine for gemcitabine-refractory metastatic PDAC in a small sample of patients. The study was not completed due to change in clinical practice and difficulty enrolling patients. However, a subset of patients responded to treatment with a median OS of 8.3 months and PFS 4 months. This was believed to be due to dual EGFR and HER2 inhibition [32]. Trastuzumab is a monoclonal antibody targeting HER2. It was added to capecitabine in metastatic PDAC in a phase II trial, but the results were disappointing [48]. The phase I/II THERAPY trial utilized the dual inhibition of EGFR and HER2 receptors with trastuzumab and cetuximab. There was no observed objective response in addition to a high toxicity profile [49].
2.4 Insulin-like growth factor receptor and axis
Insulin growth factor (IGF) axis in PDAC has been a special interest due to the association with new-onset diabetes [50]. IGF axis is a group of biomarkers consisting of ligands (IGF-1 and IGF-2), receptors (IGF1R and IGF2R), and binding proteins (6 IGFBPs and 9 IGFBP). Activation of IGF1R results in downstream activation of anti-apoptotic pathways and drug resistance, while activation of IGF2R by its ligands, IGF2 and mannose 6 phosphate (M6P), has tumor suppressor function [50]. Therefore, cell death and apoptosis are inhibited by the loss of IGF2R [50,51,52,53]. IGF-1 levels were found to be elevated in cancers like breast, colon, and prostate cancers [54,55,56]. There is no established relationship with PDAC so far, but the research is ongoing [57, 58]. The proposed association between IGF-1 level and early detection of PDAC will be revolutionary if proved true. Increased IGF-1/IGFBP-3 M ratio is thought to be a risk factor of PDAC, studied in a nested case control study of patients with prostate, lung, ovarian, and colorectal cancers who developed PDAC [59].
A phase I/II trial added the IGF1R antibody dalotuzumab (MK-0646) to gemcitabine and erlotinib in advanced PDAC. There was improved OS with the gemcitabine and MK-0646 combination but no difference in PFS, and there was no benefit in dual receptor blockade by adding erlotinib. Additionally, there was no association between IGF-1 levels and clinical outcomes [60]. Another antibody, ganitumab, was tested in the phase III GAMMA trial. In combination with gemcitabine, it failed to improve clinical outcomes [61].
2.5 JAK-STAT
The JAK-STAT pathway is a signal transduction pathway involved in cell proliferation. JAK is a transmembrane protein with intracellular tyrosine kinase portion activated by cytokines, mainly IL-6 that is produced in inflammatory conditions like pancreatitis [62, 63]. Gene expression analysis revealed increased expression of protein members of this pathway in PDAC [64].
Ruxolitinib is a JAK1/2 inhibitor that has been evaluated in PDAC. Unfortunately, combining ruxolitinib to capecitabine in gemcitabine-refractory disease did not improve outcomes [65]. Similarly, another phase III trial was terminated based on lack of efficacy (Clinical trial: NCT02119663). Trials testing other JAK inhibitor in PDAC were terminated due to a lack of efficacy as well [66, 67].
2.6 Embryonic pathways
2.6.1 Hedgehog pathway
Hedgehog signaling pathway (Hh) plays an essential role in embryonic cell growth and differentiation [68]. Anomalous activation impacts tumor progression and response to therapy [68]. It normally acts through downstream signaling initiated by binding of its three ligands: sonic hedgehog (SHH), Indian hedgehog (IHH), and desert hedgehog (DHH). Seventy-five percent of PDACs have alterations in the Hh ligand expression [69]. The most studied among the three ligands in PDAC is SHH that is highly upregulated in this disease [70,71,72,73]. Hh pathway also causes desmoplasia and stromal reaction [74, 75].
The blockade of the Hh pathway has been investigated in PDAC as a potential target [76]. Studies suggested the role of statins in inhibiting carcinogenesis of PDAC through affecting SHH signaling and post translational modification of Hh protein [77,78,79,80]. However, there is no definitive evidence yet to include statins in the treatment of PDAC.
2.6.2 Notch signaling pathway
Notch pathway affects cell growth in different ways based on the cellular context and is activated by ligands such as delta-like 4 (DLL-4). Notch can be both pro-oncogenic and tumor suppressant [81]. It is highly expressed in PDAC and has a role in chemo-resistance [82, 83]. Possible reversal of chemo-resistance was described in preclinical studies by Notch inhibition with the anti-DLL4 antibodies tarextumab and demcizumab in combination with gemcitabine [84]. However, clinical trials have so far been negative [85]. A suggested inhibition of tumor growth and invasion upon inhibition of gamma-secretase, a cleavage enzyme in notch cascade, was tested with different inhibitors [86, 87]. A phase II trial tested the gamma-secretase inhibitor RO4929097 in previously treated PDAC. Enrollment in this study was stopped, and the drug production was discontinued due to the absence of tumor response and limited activity [88]. An interesting concept that is the use of natural products such as curcumin, sulforaphane, and genistein as inhibitors of Notch-1 signaling in PDAC has been studied. Genistein suppressed cell growth, but there is no supportive clinical evidence of benefit to date [89,90,91,92].
2.6.3 Wnt/ β-catenin signaling
The Wnt pathway is involved in epithelial-mesenchymal transition, regulation of cell cycle, apoptosis, and microenvironment leading to PDAC progression, invasion, and chemo-resistance [93,94,95,96,97]. Wnt acts through a canonical pathway that is β-catenin dependent and a non-canonical pathway that is β-catenin independent [98]. Several trials highlighted this potential target for the treatment of PDAC. Attempts to inhibit the Wnt pathway focused on the various aspects of this pathway including porcupine, the enzyme involved in secretion of Wnt ligands, Wnt proteins, and the binding of Wnt ligands to their receptors [99, 100].
Table 3 summarizes several agents that reached clinical studies in PDAC. Unfortunately, however, targeting Wnt/β-Catenin signaling pathway has not demonstrated a clinically meaningful benefit.
3 Inside the cell
3.1 RAS
RAS is a subfamily of proteins among a large family of small GTPases [105]. They include HRAS, NRAS, and KRAS and control cell proliferation. Their genes share near-identical structures, but they harbor mutations at different frequencies in cancers. KRAS is the most frequently mutated gene [106]. It is located on chromosome 12 and is mutated in more than 90% of PDAC and early forms of pancreatic neoplasia [107,108,109]. The most characterized signaling pathway that activates the wild-type (WT) KRAS is the EGFR receptor signaling [105]. KRAS acts as an on-off switch of cell proliferation by binding to GDP/GTP through both guanine nucleotide exchange factors (GEFs) that moderate exchange of GDP for GTP and GTPase-activating proteins (GAPs) that inactivate KRAS by hydrolyzing GTP to GDP [110,111,112]. Once mutated, KRAS is in the active form sending the “on” signal which leads to continuous cellular proliferation. KRAS mutations are frequently detected at the G12 position, and G12D is the most common, which is sufficient to lead to early forms of metaplasia and pancreatic intraepithelial neoplasia that will subsequently progress to PDAC [113].
Targeting mutant KRAS has been a priority in PDAC since it is the most commonly mutated gene. However, it has so far proven to be an elusive target, partially due to its protein structure and partially due to its high affinity to GTP. Therefore, research on KRAS drug development focused on disruption of regulator/effector interaction and inhibition of downstream effectors such as PI3K/AKT and MAPK/ERK pathways, as well as membrane association, synthetic interaction, and metabolism [114]. More recently, several agents targeting G12C have shown promising results in both lung and colon cancers [115]. However, this mutation is rather uncommon in PDAC that it would be difficult to design a clinical trial evaluating its role in this subset of patients. The more common KRAS mutations in PDAC are G12D and G12V [109]. These two variants have proven to be elusive to target.
KRAC G12C is a variant of mutated KRAS that is more common in lung cancer (13%) and colon cancer (1–3%) but is present in < 2% of PDAC. Sotorasib (AMG 510) is a small molecule that binds selectively and irreversibly to KRAS G12C [116]. It was administered as single agent in a phase I trial for heavily pretreated patients with advanced solid tumors with a KRAS G12C mutation and showed encouraging antitumor activity [116]. The trial included one patient with PDAC who achieved a partial response [116].
Another promising agent for KRAC G12C is the novel pan-KRAS inhibitor BI 1701963 (add reference from next line). This is a small molecule inhibitor of protein-protein interaction that binds son of sevenless homologue 1 (SOS1), which leads to KRAS inhibition [117]. A phase I trial (ClinicalTrials.gov: NCT04111458) is currently ongoing to evaluate the maximum tolerated dose for BI 1701963 as monotherapy and in combination with the MEK inhibitor, Trametinib [117].
Since G12D and G12V variants of mutant KRAS are more common in PDAC, studies for PDAC are testing treatment by targeting these variants. Administration of peripheral blood lymphocytes transduced with murine T cell receptor to recognize these variants is being evaluated in two separate phase I/II trials (ClinicalTrials.gov: NCT03745326) (ClinicalTrials.gov: NCT03190941).
3.1.1 KRAS wild-type tumors
KRAS wild-type tumors deserve mentioning as they represent a distinct group of PDAC. Collectively, they compose ~ 6–8% of PDAC cases and are rich with molecular aberrations such as NGR1 rearrangement, NTRK fusion, as well as rearrangement of ALK and ROS [118].
Rearrangements in NRG1 confer susceptibility to targeting the ErbB family, including anti-EGFR therapy, unlike what was observed with KRAS mutant PDAC (mentioned above) [13]. For example, the combination of erlotinib and gemcitabine was associated with a survival benefit of 7.9 months compared to 5.7 months with single agent gemcitabine [12, 13]. Promising results were also observed with treatment with afatinib, a tyrosine kinase inhibitor of EGFR, Her2, and Her4 [119]. Zenocutuzumab is a bispecific Her2 and Her3 antibody that is currently subject of a phase I/II trial for advanced solid tumors with NRG1 fusions, including PDAC (ClinicalTrials.gov: NCT02912949).
Nimotuzumab is a monoclonal antibody that binds with high affinity to the extracellular region of EGFR and prevents ligand binding and receptor activation [14]. In a randomized phase IIb study, patients with wild-type KRAS also showed significantly improved OS compared to patients with mutated KRAS, when treated with a combination of nimotuzumab and gemcitabine (11.6 versus 5.6 months, P = 0.03) [14].
Fusions in the TRK-coding genes occur in < 1% of PDAC cases [120]. Larotrectinib and entrectinib are FDA approved for the treatment of advanced solid tumors with NTRK fusions, and both have activity in PDAC [121]. The original phase I/II trial included one patient with PDAC [121]. The overall response rate was 75%, and the median duration of response was not reached at the time of publication [121]. Two patients with PDAC with NTRK fusion received entrectinib on the phase 2 STARTRK-2 basket study; both had a partial response with normalization of CA 19-9 (ClinicalTrials.gov: NCT02568267) [122].
ALK rearrangements are observed in ~ 0.16% of PDAC [123]. While these gene rearrangements are more established in the management of non-small cell lung cancer, ALK inhibitors have activity in PDAC with ALK rearrangements [123]. In one case series, crizotinib was given as the first choice of ALK-targeting therapy; duration of survival from diagnosis ranged from 5 to 52 months [123]. Another case report shows a partial response with crizotinib following progression on first-line chemotherapy in a patient with locally advanced PDAC [124]. This was associated with improvement of the patient’s clinical status, and he was being evaluated for surgical resection.
3.2 BRAF
BRAF is a protein kinase that is a part of RAS/RAF/MEK/ERK signaling transduction cascade [125]. It is encoded by proto-oncogene B-Raf that acts as driver oncogene when mutated in different cancers. Somatic BRAF mutations are identified in 3% of PDAC cases [118, 126]. Targeted therapy proved benefit in cancers that harbor BRAF-specific mutations, such as melanoma [127, 128]. Oncogenic BRAF mutations are mutually exclusive with KRAS mutations. Ninety percent of BRAF driver mutations in cancer is BRAF V600E mutation, which is found in only 3% of advanced PDACs. Non-V600E BRAF aberrations are identified in 1% of PDACs [128]. In patients with identified BRAF driver mutations, BRAF targeted therapy can be considered, but responses are short lived due to development of resistance to BRAF inhibitors [129, 130]. Off-label use of MAPK inhibition in patients with in-frame BRAF insertions or deletions showed response to MAPK inhibition. However, similar to anti-BRAF therapy, responses were not sustained [131, 132], and the answer could be in combining BRAF and MEK inhibition, with combinations such as dabrafenib and trametinib [126, 133].
3.3 PI3K/AKT/mTOR pathway
Phosphoinositide 3-kinase (PI3K) is a crucial protein activated by receptor tyrosine kinases, and it in turn activates AKT which is a key signaling protein kinase involved in PI3K/AKT/mTOR and other pathways [134, 135]. There are three isoforms of Akt. Akt2, which normally plays a role in the insulin signaling pathway, is overexpressed in PDAC [136, 137]. The mammalian target of rapamycin (mTOR) is a protein kinase that belongs to a family of kinases called phosphoinositide 3-kinase-related kinases (PI3K) [138].
Rigosertib, an inhibitor of multiple signaling pathways, including PI3K, and also a RAS mimetic, did not demonstrate a clinical benefit in a phase II/III trial when added to gemcitabine compared to gemcitabine alone in previously untreated PDAC [139]. The pan-PI3K inhibitor, buparlisib (BKM120), was evaluated in advanced solid tumors alone and in combination with other agents to inhibit other protein functions like mTOR and MEK [140, 141], but no specific trials in PDAC. A phase Ib study combined buparlisib and trametinib for treatment of advanced solid tumors, including PDAC. The combination leads to minimal activity in PDAC [140]. An ongoing phase II single-arm trial (ClinicalTrials.gov: NCT01028495) is evaluating the safety and efficacy of an Akt inhibitor (RX-0201) in combination with gemcitabine in metastatic pancreatic adenocarcinoma.
Benefit of everolimus has not been established in this disease. Results of two phases II single-arm studies did not reveal a clinically relevant antitumor activity of everolimus with erlotinib in one study, and temsirolimus in another study, in PDAC [142]. The addition of everolimus to capecitabine showed moderate activity with an acceptable toxicity profile. The median overall survival was 8.9 months (95% CI 4.6–13.1) [143]. This result seemed to be promising compared to other studies of capecitabine alone.
Data from preclinical research is developing on targeting this pathway [144,145,146]. Quercetin, a flavonoid abundant in certain types of foods like apples, onions, grapes, and red raspberries is studied in the human PDAC cell line and reported to facilitate sensitivity to gemcitabine through PI3K/Akt/mTOR pathway suppression [147]. Data on metformin in the PDAC cell line demonstrated enhanced sensitivity of PDAC cells to gemcitabine with metformin through suppression of this pathway [148].
3.4 MAPK/ERK pathway
The MAPK/ERK pathway is an essential signal transduction pathway that mediates the function of Ras oncogene. Targeting proteins of this pathway causes cell cycle arrest at the G1 phase. ERK 1 and 2 also affect apoptosis by the regulation of anti-apoptotic proteins. The MEK inhibitor selumetinib was compared against gemcitabine in the second-line setting of treatment of PDAC but did not show a statistically significant difference in OS [149]. It was also evaluated in the second-line setting in a phase II trial in addition to erlotinib (add reference from next line). It showed a modest antitumor effect. A subset of patients appeared to benefit [150]. Trametinib, the MEK1/2 inhibitor, failed to improve survival when combined with gemcitabine compared to gemcitabine alone [151]. In vitro cell line studies and studies on patient-derived xenografts suggest that inhibition of MEK 1/2 affects a key regulatory axis of autophagy, LKB1→AMPK→ULK1, and combined inhibition of MEK 1/2 and autophagy creates a synergistic effect that prevents PDAC cell proliferation [152, 153]. Autophagy inhibition is also reported with hydroxychloroquine [154, 155]. The inhibitory effect of hydroxychloroquine on cell autophagy is being evaluated in clinical trials, combined with different agents (ClinicalTrials.gov: NCT04386057, ClinicalTrials.gov: NCT04132505, and ClinicalTrials.gov: NCT04145297). Studies suggest a possible synergistic effect of MEK 1/2 inhibitors and hydroxychloroquine [156]. The combination seems to promote regression of RAS/RAF/MEK/ERK-driven cancers in preclinical models and showed promising activity in patient with refractory PDAC [156]. An ongoing phase I trial is testing combination trametinib and hydroxychloroquine (ClinicalTrials.gov: NCT03825289). Another promising combination is targeting Her or PI3K and MEK [157].
3.5 TGF-B/SMAD4 pathway
SMAD4 is a protein that acts as a mediator of transforming growth factor-beta (TGF B), works as a checkpoint at G1/S, and induces cell cycle arrest and apoptosis. Therefore, it is considered a tumor suppressor pathway [158, 159]. Inactivation of SMAD4 is a common genetic aberration described in PDAC and is thought to affect patient survival and prognosis [160, 161]. The tumor suppressor function of this pathway brought an interest in research to develop targeted therapy [162, 163]. The complexity in targeting TGF-B is due to its dual effect on PDAC pathogenesis, as it also has a tumor-promoting function in other TGF B/SMAD4-independent pathways [163]. Understanding the different effects through different pathways has an impact on molecular targets that should focus on maintaining the tumor suppressor function and suppressing the tumor promotor function. Many preclinical and clinical trials focusing on targeting the TGF-B/SMAD4 pathway are ongoing, and results are pending [164,165,166,167]. Table 4 summarizes the current clinical trials targeting this pathway.
4 Inside the nucleus
4.1 Tumor suppressor genes
4.1.1 CKDN2A
CDKN2A is a tumor suppressor gene encoding P16/INK4A protein. It inhibits cyclin D-CDK4 and cyclin D-CDK6 complexes which eventually inhibits G1/S transition and arrest of the cell cycle in the G1 phase [168, 169]. CKDN2A mutation or promoter hypermethylation is found in 90% of PDAC, which leads to uncontrolled cell proliferation and tumor growth [170]. Targeting CDK4 and CDK6 is established in the treatment of hormone-sensitive breast cancer [171,172,173]. Inhibition of these proteins would compensate for the loss of p16 tumor suppressor function observed in some cancers including PDAC. Preclinical evidence showed a promising effect of the CDK4/6 inhibitor abemaciclib in PDAC [174], and there is an ongoing phase I trial (ClinicalTrials.gov: NCT03454035) evaluating the combination of the ERK inhibitor ulixertinib (BVD-523) with the CDK4/6 inhibitor palbociclib in patients with PDAC among other solid tumors. Another ongoing phase I trial is evaluating the role of the CDK4/6 inhibitor palbociclib in combination with the PI3K/mTOR inhibitor gedatolisib (ClinicalTrials.gov: NCT03065062).
4.1.2 P53
P53 is a protein encoded by the TP53 gene and acts as a tumor suppressor by regulating the cell cycle progression, apoptosis, and response to DNA damage and oxidative stress. More than 50% of cancers in general and 70% of PDAC harbor mutations in TP53 [175]. Replacing the loss of p53 will be revolutionary if successful. However, it is currently still in the preclinical realm. In vitro studies have achieved a stable expression of wild-type TP53 by retroviral-mediated gene transduction in human cancer cells including pancreatic cancer. Introduction of wild-type TP53 into PDAC cells increased cell sensitivity to therapy [175]. In vivo studies have also shown inhibition of cancer cell line growth by viral-mediated delivery of wild-type TP53 [176,177,178]. Dihydrosanguinarine mediated cell cycle arrest by downregulation of mutant TP53 in PDAC cell line, which is a promising concept in molecular research [179]. Inhibition of class I histone deacetylases HDAC1 and HDAC2 is another mechanism of inhibition of the mutant TP53 protein. Preclinical data led to clinical studies that evaluated many of the HDAC inhibitors in different cancers, including PDAC [180,181,182]. The HDAC inhibitor CI-994 showed antitumor activity combined with paclitaxel and carboplatin in a phase I trial in patients with advanced solid tumors [183]. In a phase II trial, CI-994 added to gemcitabine offered no benefit compared to gemcitabine alone in PDAC [184]. Vorinostat is another HDAC inhibitor studied in a phase I trial combined with chemoradiation with capecitabine in PDAC and showed tolerability and median OS of 1.1 years [185]. Table 5 demonstrates the active clinical trials of HDAC inhibitors in PDAC. Other studies have been terminated early due to either slow accrual or loss of funding.
4.2 Mismatch repair proteins
Deficiency in mismatch repair (dMMR) or loss of function of the mismatch repair proteins MLH1, MSH2, MSH6, or PMS2 increases mutation burden and microsatellite instability (MSI), which promotes tumor immunogenicity by activating T cells and production of pro-inflammatory cytokines [186, 187]. Deficiency in mismatch repair and microsatellite instability are rarely seen in PDAC (occur in < 1% of cases), and most cases are associated with Lynch syndrome [188,189,190]. The use of the checkpoint inhibitor pembrolizumab in patients with microsatellite instability or mismatch repair deficiency is associated with improved survival [191], but we emphasize on the fact that such a presentation is rare [192, 193]. A few studies specifically evaluated the role of immunotherapy in PDAC treatment outside of dMMR or MSI and failed to improve outcomes. A phase I trial used nivolumab in combination with vaccine therapy for the treatment of patients with advanced PDAC [194]. It resulted in two partial responses and possible benefits of PDL-1 inhibition with the dendritic cell vaccine [194]. A phase Ib/II trial combined gemcitabine, nab-paclitaxel, and pembrolizumab for metastatic PDAC. There was a slight improvement in efficacy, but the primary endpoint of more than 15% complete response was not met [195].
4.3 Fanconi anemia DNA repair pathway
Normally, DNA damage activates the Fanconi anemia (FA) repair pathway, which contains multiple proteins including BRCA1, BRCA2, and PALB2 [196]. Mutations in this pathway are mostly sporadic but can be associated with hereditary cancer syndromes in 5–10% of PDAC [197, 198]. The hereditary breast cancer pathway is one example, associated with mutations of BRCA1 and BRCA2 [199]. To date, there are promising results of PARP inhibitor use in patients with BRCA mutations [200]. Olaparib is now FDA approved as maintenance treatment of patients with metastatic PDAC with a germline BRCA1/2 or PALB2 mutations who did not experience disease progression for at least 16 weeks of platinum-based chemotherapy [201]. The approval came after results of the POLO phase III trial that showed 7.4-month mPFS in patients who received olaparib maintenance compared to 3.8 months in patients who received placebo [202]. The drawback of this trial is that olaparib was compared against placebo and not a form of active maintenance treatment such as capecitabine. However, we would still consider olaparib in our practice for this subset of patients. Rucaparib, another PARP inhibitor, was recently studied in a phase 2 trial as maintenance therapy in patients with BRCA1/2 or PALB2 mutations whose disease did not progress on platinum-based chemotherapy, similar to the olaparib study [203]. However, this trial included patients with both germline and somatic mutations in the affected genes. Results from the interim analysis show a mPFS of 9.1 months, with a disease-control rate of 89.5% for at least 8 weeks [203]. While these data are preliminary, they are very promising. This is in comparison to the negative RUCAPANC study, a phase 2 trial that evaluated the role of rucaparib after progression on 1 or 2 lines of chemotherapy in patients with PDAC with germline and somatic BRCA 1/2 mutations [204]. Although the majority (78.9%) of patients was exposed to platinum-based chemotherapy, the trial was terminated due to lack of response in the first 15 patients evaluated on the trial, per specifications of the trial protocol. Those results are in line with the results of prior and following studies, and this perhaps speaks to the study design and also to the need of better patient selection and treatment sequencing.
The PARP 1/2 inhibitor veliparib showed a potential OS benefit in patients with PARP3 and RBX1 transcripts when given with radiotherapy [205]. It was also evaluated in patients with locally advanced and metastatic PDAC after progression on one or more lines of prior therapy, but there was no confirmed response [206]. An active phase II clinical trial is currently comparing gemcitabine and cisplatin with and without veliparib to veliparib alone in previously treated BRCA1/2- or PALB2-mutant PDAC (ClinicalTrials.gov: NCT01585805). Veliparib is also being evaluated as second-line therapy with FOLFIRI in metastatic PDAC, regardless of BRCA status (ClinicalTrials.gov: NCT02890355). Interesting future applications of PARP inhibitors in PDAC include combinations with immune checkpoint inhibitors (ClinicalTrials.gov: NCT03404960) as well as with anti-VEGF therapy (Clinical Trials: NCT02498613).
Data from the Know Your Tumor Program highlights that the survival benefit observed in patients with mutations in the homologous recombination DNA damage response pathway (HR-DDR) occurs in the setting of exposure to platinum-based chemotherapy, irrespective of whether those mutations involve BRCA1/2 or PALB2 versus others, such as ATM, CHEK1/2, and RAD50/51 [207]. However, the question that begs itself is whether the same holds true for treatment with PARP inhibitors, and more studies are needed to answer this question. In our practice, we reserve treatment with a PARP inhibitor to those patients with germline mutations in BRCA1/2 or PALB2, with a consideration to those with somatic mutations as well. The other important issue to note is the methods used to identify such genomic derangements. While comprehensive measures such as whole genome sequencing are definitely more laborious, simpler means such as simple gene sequencing and/or methylation assays are sure to miss a subset of patients who have functional deficiencies in their HR-DDR pathway in ways yet to be discovered [208, 209].
4.4 Cancer stem cell and telomerase as targets for PDAC treatment
The human cell genome contains multiple nucleotide sequence repeats that protect the end of chromosomes from DNA breaks, damage, and fusions, called telomeres [210, 211]. Telomerase is the enzyme that protects telomeres. It is normally produced early in human body development and is later repressed [212]. Telomerase was found to be highly expressed in multiple human cancers, including PDAC, which contributes to cancer cell immortality and survival, a feature all cancer research is trying to target [213, 214]. Finding agents that alter telomerase activity can cause a dramatic change in cancer therapeutics in general and in the treatment of PDAC that still carries a poor prognosis among cancers. However, the obstacle with this approach is the expected delay in effect due to the time needed for sufficient loss of telomeres that leads to cancer cell death [215, 216].
Inhibition of telomerase is based on the two main subunits of the enzyme: the human telomerase reverse transcriptase (hTERT) and human telomerase RNA (hTR) [217]. Studies that attempted to target hTR used oligonucleotide inhibitors of telomerase [218,219,220]. Imetelstat (GRN163L) leads to rapid shortening of telomerase in PDAC cell lines and maintained extremely short but stable telomeres. Continuous exposure to Imetelstat leads to complete loss of cell viability [201]. Another target is the shelterin complex that regulates telomerase activity and protects telomere by capping [221, 222]. Shelterin complex is composed of six subunits: TRF1, TRF2, RAP1, TIN2, TPP1, and POT1, of which TRF1 and TRF2 are regulated by poly (ADP-ribose) polymerases (PARPs) [223,224,225,226]. This also makes PARP inhibitors a potential treatment targeting this aspect of PDAC. Preclinical studies reported telomere shortening with prolonged PARP inhibition [227,228,229]. There is possible synergy between telomerase inhibition with Imetelstat (GRN163L) and PARP inhibition to limit the life span of cancer cells when evaluated in the pancreatic cancer cell line [230]. However, further studied are needed to confirm this.
5 Conclusion
Understanding the molecular drivers of PDAC has been the focus of researchers for the development of more efficacious therapies. Recent advances introduced a role for targeted therapy in the management of PDAC. The biggest challenges that clinicians continue to face (and patients) in regard to better utility of targeted therapy include (1) timely molecular profiling that delivers crucial information without delays in patient care, (2) comprehensive molecular profiling to encompass the wide range of molecular signatures, and (3) effective use of data from molecular profiling for improved access of patients to clinical trials and improved selection of patient enrollment on those trials. Multiple other molecular targeted therapies for the treatment of pancreatic cancer are under development, including miRNA, tumor vaccines, targets of the extracellular matrix, and immunotherapy. A discussion of these topics is beyond the scope of this review article that mainly focuses on pancreatic cancer cell drivers with their targets.
References
Hezel, A. F., Kimmelman, A. C., Stanger, B. Z., Bardeesy, N., & DePinho, R. A. (2006). Genetics and biology of pancreatic ductal adenocarcinoma. Genes and Development. https://doi.org/10.1101/gad.1415606.
Distler, M., Aust, D., Weitz, J., Pilarsky, C., & Grützmann, R. (2014). Precursor lesions for sporadic pancreatic cancer: PanIN, IPMN, and MCN. BioMed Research International. https://doi.org/10.1155/2014/474905.
Weissmueller, S., et al. (2014). Mutant p53 drives pancreatic cancer metastasis through cell-autonomous PDGF receptor β signaling. Cell. https://doi.org/10.1016/j.cell.2014.01.066.
Makohon-Moore, A., & Iacobuzio-Donahue, C. A. (2016). Pancreatic cancer biology and genetics from an evolutionary perspective. Nature Reviews Cancer. https://doi.org/10.1038/nrc.2016.66.
Khan, S., Ansarullah, D., Kumar, M. J., & Chauhan, S. C. (2013). Targeting microRNAs in pancreatic cancer: Microplayers in the big game. Cancer Research. https://doi.org/10.1158/0008-5472.CAN-13-1288.
Troiani, T., et al. (2012). Targeting EGFR in pancreatic cancer treatment. Current Drug Targets. https://doi.org/10.2174/138945012800564158.
Korc, M., Meltzer, P., & Trent, J. (1986). Enhanced expression of epidermal growth factor receptor correlates with alterations of chromosome 7 in human pancreatic cancer. Proceedings of the National Academy of Sciences of the United States of America. https://doi.org/10.1073/pnas.83.14.5141.
Shimizu, N., Kondo, I., Gamou, S., Behzadian, M. A., & Shimizu, Y. (1984). Genetic analysis of hyperproduction of epidermal growth factor receptors in human epidermoid carcinoma A431 cells. Somatic Cell and Molecular Genetics. https://doi.org/10.1007/BF01534472.
Barton, C. M., Hall, P. A., Hughes, C. M., Gullick, W. J., & Lemoine, N. R. (1991). Transforming growth factor alpha and epidermal growth factor in human pancreatic cancer. The Journal of Pathology. https://doi.org/10.1002/path.1711630206.
Tobita, K., et al. (2003). Epidermal growth factor receptor expression in human pancreatic cancer: Significance for liver metastasis. International Journal of Molecular Medicine. https://doi.org/10.3892/ijmm.11.3.305.
Moore, M. J., et al. (2007). Erlotinib plus gemcitabine compared with gemcitabine alone in patients with advanced pancreatic cancer: A phase III trial of the National Cancer Institute of Canada clinical trials group. Journal of Clinical Oncology. https://doi.org/10.1200/JCO.2006.07.9525.
Da Cunha Santos, G., et al. (2010). Molecular predictors of outcome in a phase 3 study of gemcitabine and erlotinib therapy in patients with advanced pancreatic cancer: National Cancer Institute of Canada clinical trials group study PA.3. Cancer. https://doi.org/10.1002/cncr.25393.
Boeck, S., et al. (2013). EGFR pathway biomarkers in erlotinib-treated patients with advanced pancreatic cancer: Translational results from the randomised, crossover phase 3 trial AIO-PK0104. British Journal of Cancer. https://doi.org/10.1038/bjc.2012.495.
Schultheis, B., et al. (2017). Gemcitabine combined with the monoclonal antibody nimotuzumab is an active first-line regimen in KRAS wildtype patients with locally advanced or metastatic pancreatic cancer: A multicenter, randomized phase IIb study. Annals of Oncology. https://doi.org/10.1093/annonc/mdx343.
Yang, L., et al. (2019). Rhein sensitizes human pancreatic cancer cells to EGFR inhibitors by inhibiting STAT3 pathway. Journal of Experimental & Clinical Cancer Research. https://doi.org/10.1186/s13046-018-1015-9.
Nagaraj, N. S., Washington, M. K., & Merchant, N. B. (2011). Combined blockade of Src kinase and epidermal growth factor receptor with gemcitabine overcomes STAT3-mediated resistance of inhibition of pancreatic tumor growth. Clinical Cancer Research. https://doi.org/10.1158/1078-0432.CCR-10-1670.
Dosch, A. R., et al. (2020). Combined Src/EGFR inhibition targets STAT3 signaling and induces stromal remodeling to improve survival in pancreatic cancer. Molecular Cancer Research. https://doi.org/10.1158/1541-7786.MCR-19-0741.
Cascinu, S., et al. (2008). Cetuximab plus gemcitabine and cisplatin compared with gemcitabine and cisplatin alone in patients with advanced pancreatic cancer: A randomised, multicentre, phase II trial. The Lancet Oncology. https://doi.org/10.1016/S1470-2045(07)70383-2.
Philip, P. A., et al. (2010). Phase III study comparing gemcitabine plus cetuximab versus gemcitabine in patients with advanced pancreatic adenocarcinoma: Southwest oncology group-directed intergroup trial S0205. Journal of Clinical Oncology. https://doi.org/10.1200/JCO.2009.25.7550.
Khan, K., et al. (2016). miR-21 expression and clinical outcome in locally advanced pancreatic cancer: Exploratory analysis of the pancreatic cancer Erbitux, radiotherapy and UFT (PERU) trial. Oncotarget. https://doi.org/10.18632/oncotarget.7208.
Burtness, B., Powell, M., Catalano, P., Berlin, J., Liles, D. K., Chapman, A. E., Mitchell, E., & Benson, A. B. (2016). Randomized phase ii trial of irinotecan/docetaxel or irinotecan/docetaxel plus cetuximab for metastatic pancreatic cancer: An eastern cooperative oncology group study. American Journal of Clinical Oncology CANCER CLINICAL TRIALS, 39, 340–345. https://doi.org/10.1097/COC.0000000000000068.
Forster, T., et al. (2020). Cetuximab in pancreatic cancer therapy: A systematic review and meta-analysis. Oncol. https://doi.org/10.1159/000502844.
Philip, P. A., et al. (2014). Dual blockade of epidermal growth factor receptor and insulin-like growth factor receptor-1 signaling in metastatic pancreatic cancer: Phase Ib and randomized phase II trial of gemcitabine, erlotinib, and cixutumumab versus gemcitabine plus erlotinib (SWO). Cancer. https://doi.org/10.1002/cncr.28744.
Sinn, M., et al. (2017). CONKO-005: Adjuvant chemotherapy with gemcitabine plus erlotinib versus gemcitabine alone in patients after r0 resection of pancreatic cancer: A multicenter randomized phase III trial. Journal of Clinical Oncology. https://doi.org/10.1200/JCO.2017.72.6463.
Cardin, D. B., et al. (2014). Phase II trial of sorafenib and erlotinib in advanced pancreatic cancer. Cancer Medicine. https://doi.org/10.1002/cam4.208.
Ko, A. H., et al. (2016). A multicenter, open-label phase II clinical trial of combined MEK plus EGFR inhibition for chemotherapy-refractory advanced pancreatic adenocarcinoma. Clinical Cancer Research. https://doi.org/10.1158/1078-0432.CCR-15-0979.
Javle, M. M., et al. (2011). Randomized phase II study of gemcitabine (G) plus anti-IGF-1R antibody MK-0646, G plus erlotinib (E) plus MK-0646 and G plus E for advanced pancreatic cancer. Journal of Clinical Oncology. https://doi.org/10.1200/jco.2011.29.15_suppl.4026.
Middleton, G., et al. (2017). Vandetanib plus gemcitabine versus placebo plus gemcitabine in locally advanced or metastatic pancreatic carcinoma (ViP): A prospective, randomised, double-blind, multicentre phase 2 trial. The Lancet Oncology. https://doi.org/10.1016/S1470-2045(17)30084-0.
T. R. Halfdanarson et al., “A phase II randomized trial of panitumumab, erlotinib, and gemcitabine versus erlotinib and gemcitabine in patients with untreated, metastatic pancreatic adenocarcinoma: North Central Cancer Treatment Group Trial N064B (Alliance),” Oncologist, 2019, doi: https://doi.org/10.1634/theoncologist.2018-0878.
Fountzilas, G., et al. (2008). Gemcitabine combined with gefitinib in patients with inoperable or metastatic pancreatic cancer: A phase II study of the Hellenic Cooperative Oncology Group with biomarker evaluation. Cancer Investigation. https://doi.org/10.1080/07357900801918611.
Brell, J. M., et al. (2009). Phase II study of docetaxel and gefitinib as second-line therapy in gemcitabine pretreated patients with advanced pancreatic cancer. Oncology. https://doi.org/10.1159/000206141.
Wu, Z., et al. (2015). Phase II study of lapatinib and capecitabine in second-line treatment for metastatic pancreatic cancer. Cancer Chemotherapy and Pharmacology. https://doi.org/10.1007/s00280-015-2855-z.
Veikkola, T., Karkkainen, M., Claesson-Welsh, L., & Alitalo, K. (2000). Regulation of angiogenesis via vascular endothelial growth factor receptors. Cancer Research.
Kindler, H. L., et al. (2005). Phase II trial of bevacizumab plus gemcitabine in patients with advanced pancreatic cancer. Journal of Clinical Oncology. https://doi.org/10.1200/JCO.2005.01.9661.
Kindler, H. L., et al. (2010). Gemcitabine plus bevacizumab compared with gemcitabine plus placebo in patients with advanced pancreatic cancer: Phase III trial of the Cancer and Leukemia Group B (CALGB 80303). Journal of Clinical Oncology. https://doi.org/10.1200/JCO.2010.28.1386.
Ko, A. H., et al. (2010). A phase II study of bevacizumab plus erlotinib for gemcitabine-refractory metastatic pancreatic cancer. Cancer Chemotherapy and Pharmacology. https://doi.org/10.1007/s00280-010-1257-5.
Watkins, D. J., et al. (2014). The combination of a chemotherapy doublet (gemcitabine and capecitabine) with a biological doublet (bevacizumab and erlotinib) in patients with advanced pancreatic adenocarcinoma. The results of a phase I/II study. European Journal of Cancer. https://doi.org/10.1016/j.ejca.2014.02.003.
Spano, J. P., et al. (2008). Efficacy of gemcitabine plus axitinib compared with gemcitabine alone in patients with advanced pancreatic cancer: An open-label randomised phase II study. Lancet. https://doi.org/10.1016/S0140-6736(08)60661-3.
Kindler, H. L., et al. (2011). Axitinib plus gemcitabine versus placebo plus gemcitabine in patients with advanced pancreatic adenocarcinoma: A double-blind randomised phase 3 study. The Lancet Oncology. https://doi.org/10.1016/S1470-2045(11)70004-3.
Kindler, H. L., et al. (2012). Gemcitabine plus sorafenib in patients with advanced pancreatic cancer: A phase II trial of the University of Chicago Phase II Consortium. Investigational New Drugs. https://doi.org/10.1007/s10637-010-9526-z.
Dragovich, T., et al. (2014). Phase II trial of vatalanib in patients with advanced or metastatic pancreatic adenocarcinoma after first-line gemcitabine therapy (PCRT O4-001). Cancer Chemotherapy and Pharmacology. https://doi.org/10.1007/s00280-014-2499-4.
Brandt-Rauf, P. W., Pincus, M. R., & Carney, W. P. (1994). The c-erbB-2 protein in oncogenesis: Molecular structure to molecular epidemiology. Critical Reviews in Oncogenesis. https://doi.org/10.1615/CritRevOncog.v5.i2-3.100.
Komoto, M., et al. (2010). In vitro and in vivo evidence that a combination of lapatinib plus S-1 is a promising treatment for pancreatic cancer. Cancer Science. https://doi.org/10.1111/j.1349-7006.2009.01405.x.
Safran, H., et al. (2001). Overexpression of the HER-2/neu oncogene in pancreatic adenocarcinoma. American Journal of Clinical Oncology Cancer Clinical Trials. https://doi.org/10.1097/00000421-200110000-00016.
Yamanaka, Y., et al. (1993). Overexpression of HER2/neu oncogene in human pancreatic carcinoma. Human Pathology. https://doi.org/10.1016/0046-8177(93)90194-L.
J. D. Day et al., “Immunohistochemical evaluation of HER-2/neu expression in pancreatic adenocarcinoma and pancreatic intraepithelial neoplasms,” Human Pathology, 1996, doi: https://doi.org/10.1016/S0046-8177(96)90364-0.
Safran, H., et al. (2011). Lapatinib and gemcitabine for metastatic pancreatic cancer: A phase II study. American Journal of Clinical Oncology Cancer Clinical Trials. https://doi.org/10.1097/COC.0b013e3181d26b01.
Harder, J., Ihorst, G., Heinemann, V., Hofheinz, R., Moehler, M., Buechler, P., Kloeppel, G., Röcken, C., Bitzer, M., Boeck, S., Endlicher, E., Reinacher-Schick, A., Schmoor, C., & Geissler, M. (2012). Multicentre phase II trial of trastuzumab and capecitabine in patients with HER2 overexpressing metastatic pancreatic cancer. British Journal of Cancer, 106, 1033–1038. https://doi.org/10.1038/bjc.2012.18.
Assenat, E., et al. (2015). Dual targeting of HER1/EGFR and HER2 with cetuximab and trastuzumab in patients with metastatic pancreatic cancer after gemcitabine failure: Results of the ‘THERAPY’ phase 1–2 trial. Oncotarget. https://doi.org/10.18632/oncotarget.3473.
Hwa, V., Oh, Y., & Rosenfeld, R. G. (1999). The insulin-like growth factor-binding protein (IGFBP) superfamily 1. Endocrine Reviews. https://doi.org/10.1210/edrv.20.6.0382.
Bauer, T. W., et al. (2006). Regulatory role of c-Met in insulin-like growth factor-I receptor - mediated migration and invasion of human pancreatic carcinoma cells. Molecular Cancer Therapeutics. https://doi.org/10.1158/1535-7163.MCT-05-0175.
Pollak, M. (2008). Insulin and insulin-like growth factor signalling in neoplasia. Nature Reviews Cancer. https://doi.org/10.1038/nrc2536.
Schiller, H. B., Szekeres, A., Binder, B. R., Stockinger, H., & Leksa, V. (2009). Mannose 6-phosphate/insulin-like growth factor 2 receptor limits cell invasion by controlling αVβ3 integrin expression and proteolytic processing of urokinase-type plasminogen activator receptor. Molecular Biology of the Cell. https://doi.org/10.1091/mbc.E08-06-0569.
Peyrat, J. P., Louchez, M. M., Lefebvre, J., Bonneterre, J., Vennin, P., Demaille, A., Helquet, B., & Fournier, C. (1993). Plasma insulin-like growth factor-1 (IGF-1) concentrations in human breast cancer. European Journal of Cancer, 29, 492–497. https://doi.org/10.1016/S0959-8049(05)80137-6.
Dowling, C. M., et al. (2016). Protein kinase C beta II suppresses colorectal cancer by regulating IGF-1 mediated cell survival. Oncotarget. https://doi.org/10.18632/oncotarget.8062.
Miles, F. L., et al. (2017). Interactions of the insulin-like growth factor axis and vitamin D in prostate cancer risk in the prostate cancer prevention trial. Nutrients. https://doi.org/10.3390/nu9040378.
El-Mesallamy, H. O., Hamdy, N. M., Zaghloul, A. S., & Sallam, A. M. (2013). Clinical value of circulating lipocalins and insulin-like growth factor axis in pancreatic cancer diagnosis. Pancreas. https://doi.org/10.1097/MPA.0b013e3182550d9d.
Wlodarczyk, B., Gasiorowska, A., Borkowska, A., & Malecka-Panas, E. (2017). Evaluation of insulin-like growth factor (IGF-1) and retinol binding protein (RBP-4) levels in patients with newly diagnosed pancreatic adenocarcinoma (PDAC). Pancreatology. https://doi.org/10.1016/j.pan.2017.04.001.
Douglas, J. B., Silverman, D. T., Pollak, M. N., Tao, Y., Soliman, A. S., & Stolzenberg-Solomon, R. Z. (2010). Serum IGF-I, IGF-II, IGFBP-3, and IGF-I/IGFBP-3 molar ratio and risk of pancreatic cancer in the prostate, lung, colorectal, and ovarian cancer screening trial. Cancer Epidemiology, Biomarkers & Prevention, 19(9), 2298–2306. https://doi.org/10.1158/1055-9965.EPI-10-0400.
Abdel-Wahab, R., et al. (2018). Randomized, phase I/II study of gemcitabine plus IGF-1R antagonist (MK-0646) versus gemcitabine plus erlotinib with and without MK-0646 for advanced pancreatic adenocarcinoma. Journal of Hematology & Oncology. https://doi.org/10.1186/s13045-018-0616-2.
Fuchs, C. S., et al. (2015). A phase 3 randomized, double-blind, placebo-controlled trial of ganitumab or placebo in combination with gemcitabine as first-line therapy for metastatic adenocarcinoma of the pancreas: The GAMMA trial. Annals of Oncology. https://doi.org/10.1093/annonc/mdv027.
Jatiani, S. S., Baker, S. J., Silverman, L. R., & Premkumar Reddy, E. (2010). JAK/STAT pathways in cytokine signaling and myeloproliferative disorders: Approaches for targeted therapies. Genes & Cancer. https://doi.org/10.1177/1947601910397187.
Bunt, S. K., Yang, L., Sinha, P., Clements, V. K., Leips, J., & Ostrand-Rosenberg, S. (2007). Reduced inflammation in the tumor microenvironment delays the accumulation of myeloid-derived suppressor cells and limits tumor progression. Cancer Research. https://doi.org/10.1158/0008-5472.CAN-07-2354.
Lili, L. N., Matyunina, L. V., Walker, L. D., Daneker, G. W., & McDonald, J. F. (2014). Evidence for the importance of personalized molecular profiling in pancreatic cancer. Pancreas. https://doi.org/10.1097/MPA.0000000000000020.
Hurwitz, H. I., et al. (2015). Randomized, double-blind, phase II study of ruxolitinib or placebo in combination with capecitabine in patients with metastatic pancreatic cancer for whom therapy with gemcitabine has failed. Journal of Clinical Oncology. https://doi.org/10.1200/JCO.2015.61.4578.
Cardin, D. B., Thota, R., Goff, L. W., Berlin, J. D., Jones, C. M., Ayers, G. D., Whisenant, J. G., & Chan, E. (2018). A phase II study of ganetespib as second-line or third-line therapy for metastatic pancreatic cancer. American Journal of Clinical Oncology Cancer Clinical Trials, 41, 772–776. https://doi.org/10.1097/COC.0000000000000377.
Beatty, G. L., et al. (2019). A phase Ib/II study of the JAK1 inhibitor, itacitinib, plus nab -paclitaxel and gemcitabine in advanced solid tumors. Oncologist. https://doi.org/10.1634/theoncologist.2017-0665.
Hebrok, M., Kim, S. K., St-Jacques, B., McMahon, A. P., & Melton, D. A. (2000). Regulation of pancreas development by hedgehog signaling. Development.
Thayer, S. P., et al. (2003). Hedgehog is an early and late mediator of pancreatic cancer tumorigenesis. Nature. https://doi.org/10.1038/nature02009.
Li, C., et al. (2007). Identification of pancreatic cancer stem cells. Cancer Research. https://doi.org/10.1158/0008-5472.CAN-06-2030.
Pak, E., & Segal, R. A. (2016). Hedgehog signal transduction: Key players, oncogenic drivers, and cancer therapy. Developmental Cell. https://doi.org/10.1016/j.devcel.2016.07.026.
Rosow, D. E., et al. (2012). Sonic Hedgehog in pancreatic cancer: From bench to bedside, then back to the bench. Surgery. (United States). https://doi.org/10.1016/j.surg.2012.05.030.
Strobel, O., et al. (2010). Pancreatic duct glands are distinct ductal compartments that react to chronic injury and mediate Shh-induced metaplasia. Gastroenterology. https://doi.org/10.1053/j.gastro.2009.12.005.
Di Magliano, M. P., Sekine, S., Ermilov, A., Ferris, J., Dlugosz, A. A., & Hebrok, M. (2006). Hedgehog/Ras interactions regulate early stages of pancreatic cancer. Genes & Development. https://doi.org/10.1101/gad.1470806.
Bailey, J. M., et al. (2008). Sonic hedgehog promotes desmoplasia in pancreatic cancer. Clinical Cancer Research. https://doi.org/10.1158/1078-0432.CCR-08-0291.
Feldmann, G., et al. (2007). Blockade of hedgehog signaling inhibits pancreatic cancer invasion and metastases: A new paradigm for combination therapy in solid cancers. Cancer Research. https://doi.org/10.1158/0008-5472.CAN-06-3281.
Zhong, S., Zhang, X., Chen, L., Ma, T., Tang, J., & Zhao, J. (2015). Statin use and mortality in cancer patients: Systematic review and meta-analysis of observational studies. Cancer Treatment Reviews. https://doi.org/10.1016/j.ctrv.2015.04.005.
Archibugi, L., et al. (2017). Exclusive and combined use of statins and aspirin and the risk of pancreatic Cancer: A case-control study. Scientific Reports. https://doi.org/10.1038/s41598-017-13430-z.
Lee, H. S., et al. (2016). Statin use and its impact on survival in pancreatic cancer patients. Medicine (United States). https://doi.org/10.1097/MD.0000000000003607.
Yin, Y., et al. (2018). Simvastatin inhibits sonic hedgehog signaling and stemness features of pancreatic cancer. Cancer Letters. https://doi.org/10.1016/j.canlet.2018.04.001.
Avila, J. L., & Kissil, J. L. (2013). Notch signaling in pancreatic cancer: Oncogene or tumor suppressor? Trends in Molecular Medicine. https://doi.org/10.1016/j.molmed.2013.03.003.
Wang, Z., et al. (2009). Acquisition of epithelial-mesenchymal transition phenotype of gemcitabine-resistant pancreatic cancer cells is linked with activation of the notch signaling pathway. Cancer Research. https://doi.org/10.1158/0008-5472.CAN-08-4312.
Mullendore, M. E., et al. (2009). Ligand-dependent notch signaling is involved in tumor initiation and tumor maintenance in pancreatic cancer. Clinical Cancer Research. https://doi.org/10.1158/1078-0432.CCR-08-2004.
Yen, W. C., et al. (2012). Anti-DLL4 has broad spectrum activity in pancreatic cancer dependent on targeting DLL4-notch signaling in both tumor and vasculature cells. Clinical Cancer Research. https://doi.org/10.1158/1078-0432.CCR-12-0736.
Cubillo Gracian, A., et al. (2017). YOSEMITE: A 3 arm double-blind randomized phase 2 study of gemcitabine, paclitaxel protein-bound particles for injectable suspension, and placebo (GAP) versus gemcitabine, paclitaxel protein-bound particles for injectable suspension and either 1 or 2 trun. Annals of Oncology. https://doi.org/10.1093/annonc/mdx369.004.
Artavanis-Tsakonas, S., Matsuno, K., & Fortini, M. E. (1995). Notch signaling. Science (80-.). https://doi.org/10.1126/science.7716513.
Gangopadhyay, S., Nandy, A., Hor, P., & Mukhopadhyay, A. (2013). Breast cancer stem cells: A novel therapeutic target. Clinical Breast Cancer. https://doi.org/10.1016/j.clbc.2012.09.017.
De Jesus-Acosta, A., et al. (2014). A phase II study of the gamma secretase inhibitor RO4929097 in patients with previously treated metastatic pancreatic adenocarcinoma. Investigational New Drugs, 32, 739, 745. https://doi.org/10.1007/s10637-014-0083-8.
Bao, B., et al. (2011). Notch-1 induces epithelial-mesenchymal transition consistent with cancer stem cell phenotype in pancreatic cancer cells. Cancer Letters. https://doi.org/10.1016/j.canlet.2011.03.012.
Xia, J., Duan, Q., Ahmad, A., Bao, B., Banerjee, S., Shi, Y., Ma, J., Geng, J., Chen, Z., Wahidur Rahman, K. M., Miele, L., H Sarkar, F., & Wang, Z. (2012). Genistein inhibits cell growth and induces apoptosis through up-regulation of miR-34a in pancreatic cancer cells. Current Drug Targets, 13, 1750–1756. https://doi.org/10.2174/138945012804545597.
Kallifatidis, G., et al. (2011). Sulforaphane increases drug-mediated cytotoxicity toward cancer stem-like cells of pancreas and prostate. Molecular Therapy. https://doi.org/10.1038/mt.2010.216.
Rausch, V., et al. (2010). Synergistic activity of sorafenib and sulforaphane abolishes pancreatic cancer stem cell characteristics. Cancer Research. https://doi.org/10.1158/0008-5472.CAN-10-0066.
Gonzalez, D. M., & Medici, D. (2014). Signaling mechanisms of the epithelial-mesenchymal transition. Science Signaling. https://doi.org/10.1126/scisignal.2005189.
Lee, J. M., Dedhar, S., Kalluri, R., & Thompson, E. W. (2006). The epithelial-mesenchymal transition: New insights in signaling, development, and disease. The Journal of Cell Biology. https://doi.org/10.1083/jcb.200601018.
Modi, S., Kir, D., Banerjee, S., & Saluja, A. (2016). Control of apoptosis in treatment and biology of pancreatic cancer. Journal of Cellular Biochemistry. https://doi.org/10.1002/jcb.25284.
Van den broeck, A., et al. (2013). Human pancreatic cancer contains a side population expressing cancer stem cell-associated and prognostic genes. PLoS One. https://doi.org/10.1371/journal.pone.0073968.
Chikazawa, N., et al. (2010). Inhibition of Wnt signaling pathway decreases chemotherapy-resistant side-population colon cancer cells. Anticancer Research.
Kikuchi, A., Yamamoto, H., Sato, A., & Matsumoto, S. (2011). New insights into the mechanism of Wnt signaling pathway activation. In International review of cell and molecular biology.
Krishnamurthy, N., & Kurzrock, R. (2018). Targeting the Wnt/beta-catenin pathway in cancer: Update on effectors and inhibitors. Cancer Treatment Reviews. https://doi.org/10.1016/j.ctrv.2017.11.002.
Makena, M. R., Gatla, H., Verlekar, D., Sukhavasi, S., Pandey, M. K., & Pramanik, K. C. (2019). Wnt/β-catenin signaling: The culprit in pancreatic carcinogenesis and therapeutic resistance. International Journal of Molecular Sciences. https://doi.org/10.3390/ijms20174242.
Messersmith, W., et al. (2016). Phase 1b study of WNT inhibitor vantictumab (VAN, human monoclonal antibody) with nab-paclitaxel (nab-P) and gemcitabine (G) in patients (pts) with previously untreated stage IV pancreatic cancer (PC). Annals of Oncology. https://doi.org/10.1093/annonc/mdw371.69.
Weekes, C., et al. (2016). Phase 1b study of WNT inhibitor ipafricept (IPA, decoy receptor for WNT ligands) with nab-paclitaxel (nab-P) and gemcitabine (G) in patients (pts) with previously untreated stage IV pancreatic cancer (PC). Annals of Oncology. https://doi.org/10.1093/annonc/mdw368.10.
Dotan, E., et al. (2019). Phase Ib study of WNT inhibitor ipafricept (IPA) with nab-paclitaxel (nab-P) and gemcitabine (G) in patients (pts) with previously untreated stage IV pancreatic cancer (mPC). Journal of Clinical Oncology. https://doi.org/10.1200/jco.2019.37.4_suppl.369.
McWilliams, R. R., et al. (2015). A phase Ib dose-escalation study of PRI-724, a CBP/beta-catenin modulator, plus gemcitabine (GEM) in patients with advanced pancreatic adenocarcinoma (APC) as second-line therapy after FOLFIRINOX or FOLFOX. Journal of Clinical Oncology. https://doi.org/10.1200/jco.2015.33.15_suppl.e15270.
Repasky, G. A., Chenette, E. J., & Der, C. J. (2004). Renewing the conspiracy theory debate: Does Raf function alone to mediate Ras oncogenesis? Trends in Cell Biology. https://doi.org/10.1016/j.tcb.2004.09.014.
Prior, I. A., Lewis, P. D., & Mattos, C. (2012). A comprehensive survey of Ras mutations in cancer. Cancer Research. https://doi.org/10.1158/0008-5472.CAN-11-2612.
Jones, S., et al. (2008). Core signaling pathways in human pancreatic cancers revealed by global genomic analyses. Science (80-. ). https://doi.org/10.1126/science.1164368.
Raphael, B. J., et al. (2017). Integrated genomic characterization of pancreatic ductal adenocarcinoma. Cancer Cell. https://doi.org/10.1016/j.ccell.2017.07.007.
Biankin, A. V., et al. (2012). Pancreatic cancer genomes reveal aberrations in axon guidance pathway genes. Nature. https://doi.org/10.1038/nature11547.
Kraulis, P. J. (1991). MOLSCRIPT. A program to produce both detailed and schematic plots of protein structures. Journal of Applied Crystallography. https://doi.org/10.1107/s0021889891004399.
Vigil, D., Cherfils, J., Rossman, K. L., & Der, C. J. (2010). Ras superfamily GEFs and GAPs: Validated and tractable targets for cancer therapy? Nature Reviews Cancer. https://doi.org/10.1038/nrc2960.
Downward, J. (2003). Targeting RAS signalling pathways in cancer therapy. Nature Reviews Cancer. https://doi.org/10.1038/nrc969.
Herreros-Villanueva, M., Hijona, E., Cosme, A., & Bujanda, L. (2012). Mouse models of pancreatic cancer. World Journal of Gastroenterology. https://doi.org/10.3748/wjg.v18.i12.1286.
Papke, B., & Der, C. J. (2017). Drugging RAS: Know the enemy. Science. https://doi.org/10.1126/science.aam7622.
Canon, J., et al. (2019). The clinical KRAS(G12C) inhibitor AMG 510 drives anti-tumour immunity. Nature. https://doi.org/10.1038/s41586-019-1694-1.
D. S. Hong et al., “ KRAS G12C inhibition with sotorasib in advanced solid tumors ,” N. Engl. J. Med., 2020, doi: https://doi.org/10.1056/nejmoa1917239.
Gort, E., et al. (2020). A phase I, open-label, dose-escalation trial of BI 1701963 as monotherapy and in combination with trametinib in patients with KRAS mutated advanced or metastatic solid tumors. Journal of Clinical Oncology. https://doi.org/10.1200/jco.2020.38.15_suppl.tps3651.
The Cancer Genome Atlas Research Network, & Raphael, B. J. (2017). Integrated genomic characterization of pancreatic ductal adenocarcinoma The Cancer Genome Atlas Research Network*. Cancer Cell.
Jones, M. R., et al. (2019). NRG1 gene fusions are recurrent, clinically actionable gene rearrangements in KRAS wild-type pancreatic ductal adenocarcinoma. Clinical Cancer Research. https://doi.org/10.1158/1078-0432.CCR-19-0191.
Nevala-Plagemann, C., Hidalgo, M., & Garrido-Laguna, I. (2020). From state-of-the-art treatments to novel therapies for advanced-stage pancreatic cancer. Nature Reviews. Clinical Oncology. https://doi.org/10.1038/s41571-019-0281-6.
Drilon, A., et al. (2018). Efficacy of Larotrectinib in TRK fusion–positive cancers in adults and children. The New England Journal of Medicine. https://doi.org/10.1056/nejmoa1714448.
Pishvaian, M. J., Rolfo, C. D., Liu, S. V., Multani, P. S., Chow Maneval, E., & Garrido-Laguna, I. (2018). Clinical benefit of entrectinib for patients with metastatic pancreatic cancer who harbor NTRK and ROS1 fusions. Journal of Clinical Oncology. https://doi.org/10.1200/jco.2018.36.4_suppl.521.
Singhi, A. D., et al. (2017). Identification of targetable ALK rearrangements in pancreatic ductal adenocarcinoma. Journal of the National Comprehensive Cancer Network. https://doi.org/10.6004/jnccn.2017.0058.
Tuli, R., et al. (2017). Anaplastic lymphoma kinase rearrangement and response to crizotinib in pancreatic ductal adenocarcinoma. JCO Precision Oncology. https://doi.org/10.1200/po.17.00016.
Roskoski, R. (2010). RAF protein-serine/threonine kinases: Structure and regulation. Biochemical and Biophysical Research Communications. https://doi.org/10.1016/j.bbrc.2010.07.092.
Guan, M., et al. (2018). Molecular and clinical characterization of BRAF mutations in pancreatic ductal adenocarcinomas (PDACs). Journal of Clinical Oncology. https://doi.org/10.1200/jco.2018.36.4_suppl.214.
Sala, E., Mologni, L., Truffa, S., Gaetano, C., Bollag, G. E., & Gambacorti-Passerini, C. (2008). BRAF silencing by short hairpin RNA or chemical blockade by PLX4032 leads to different responses in melanoma and thyroid carcinoma cells. Molecular Cancer Research. https://doi.org/10.1158/1541-7786.MCR-07-2001.
Halaban, R., et al. (2010). PLX4032, a selective BRAFV600E kinase inhibitor, activates the ERK pathway and enhances cell migration and proliferation of BRAFWT melanoma cells. Pigment Cell & Melanoma Research. https://doi.org/10.1111/j.1755-148X.2010.00685.x.
Sullivan, R. J., & Flaherty, K. T. (2011). BRAF in melanoma: Pathogenesis, diagnosis, inhibition, and resistance. Journal of Skin Cancer. https://doi.org/10.1155/2011/423239.
Gowrishankar, K., Snoyman, S., Pupo, G. M., Becker, T. M., Kefford, R. F., & Rizos, H. (2012). Acquired resistance to BRAF inhibition can confer cross-resistance to combined BRAF/MEK inhibition. The Journal of Investigative Dermatology. https://doi.org/10.1038/jid.2012.63.
Aguirre, A. J., et al. (2018). Real-time genomic characterization of advanced pancreatic cancer to enable precision medicine. Cancer Discovery. https://doi.org/10.1158/2159-8290.CD-18-0275.
Wrzeszczynski, K. O., et al. (2019). Identification of targetable BRAF Δn486_P490 variant by whole-genome sequencing leading to dabrafenib induced remission of a BRAF-mutant pancreatic adenocarcinoma. Cold Spring Harbor Molecular Case Studies. https://doi.org/10.1101/mcs.a004424.
Busch, E., et al. (2020). Successful BRAF/MEK inhibition in a patient with BRAFV600E-mutated extrapancreatic acinar cell carcinoma. Cold Spring Harbor Molecular Case Studies. https://doi.org/10.1101/MCS.A005553.
Falasca, M., Selvaggi, F., Buus, R., Sulpizio, S., & Edling, C. E. (2012). Targeting phosphoinositide 3-kinase pathways in pancreatic cancer – From molecular signalling to clinical trials. Anti-Cancer Agents in Medicinal Chemistry. https://doi.org/10.2174/187152011795677382.
King, D., Yeomanson, D., & Bryant, H. E. (2015). PI3King the lock: Targeting the PI3K/Akt/mTOR pathway as a novel therapeutic strategy in neuroblastoma. Journal of Pediatric Hematology/Oncology. https://doi.org/10.1097/MPH.0000000000000329.
Mitsiades, C., Mitsiades, N., & Koutsilieris, M. (2005). The Akt pathway: Molecular targets for anti-cancer drug development. Current Cancer Drug Targets, 4, 235–256. https://doi.org/10.2174/1568009043333032.
Garofalo, R. S., et al. (2003). Severe diabetes, age-dependent loss of adipose tissue, and mild growth deficiency in mice lacking Akt2/PKBβ. The Journal of Clinical Investigation. https://doi.org/10.1172/JCI16885.
Mitra, A., et al. (2015). Dual mTOR inhibition is required to prevent TGF-β-mediated fibrosis: Implications for scleroderma. Journal of Investigative Dermatology. https://doi.org/10.1038/jid.2015.252.
O’Neil, B. H., et al. (2015). A phase II/III randomized study to compare the efficacy and safety of rigosertib plus gemcitabine versus gemcitabine alone in patients with previously untreated metastatic pancreatic cancer. Annals of Oncology. https://doi.org/10.1093/annonc/mdv264.
Bedard, P. L., et al. (2015). A phase Ib dose-escalation study of the oral pan-PI3K inhibitor buparlisib (BKM120) in combination with the oral MEK1/2 inhibitor trametinib (GSK1120212) in patients with selected advanced solid tumors. Clinical Cancer Research. https://doi.org/10.1158/1078-0432.CCR-14-1814.
Owonikoko, T. K., et al. (2020). A phase I study of safety, pharmacokinetics, and pharmacodynamics of concurrent everolimus and buparlisib treatment in advanced solid tumors. Clinical Cancer Research. https://doi.org/10.1158/1078-0432.ccr-19-2697.
Javle, M. M., et al. (2010). Inhibition of the mammalian target of rapamycin (mTOR) in advanced pancreatic cancer: Results of two phase II studies. BMC Cancer. https://doi.org/10.1186/1471-2407-10-368.
Kordes, S., Klümpen, H. J., Weterman, M. J., Schellens, J. H. M., Richel, D. J., & Wilmink, J. W. (2015). Phase II study of capecitabine and the oral mTOR inhibitor everolimus in patients with advanced pancreatic cancer. Cancer Chemotherapy and Pharmacology. https://doi.org/10.1007/s00280-015-2730-y.
Ichimaru, Y., et al. (2019). Indirubin 3′-oxime inhibits migration, invasion, and metastasis in vivo in mice bearing spontaneously occurring pancreatic cancer via blocking the RAF/ERK, AKT, and SAPK/JNK pathways. Translational Oncology. https://doi.org/10.1016/j.tranon.2019.08.010.
Zhou, L., Jiao, X., Peng, X., Yao, X., Liu, L., & Zhang, L. (2020). MicroRNA-628-5p inhibits invasion and migration of human pancreatic ductal adenocarcinoma via suppression of the AKT/NF-kappa B pathway. Journal of Cellular Physiology. https://doi.org/10.1002/jcp.29468.
Elaskalani, O., Domenchini, A., Razak, N. B. A., Dye, D. E., Falasca, M., & Metharom, P. (2020). Antiplatelet drug ticagrelor enhances chemotherapeutic efficacy by targeting the novel P2Y12-AKT pathway in pancreatic cancer cells. Cancers (Basel). https://doi.org/10.3390/cancers12010250.
Lan, C. Y., Chen, S. Y., Kuo, C. W., Lu, C. C., & Yen, G. C. (2019). Quercetin facilitates cell death and chemosensitivity through RAGE/PI3K/AKT/mTOR axis in human pancreatic cancer cells. Journal of Food and Drug Analysis. https://doi.org/10.1016/j.jfda.2019.07.001.
Zhou, H. Y., Yao, X. M., Chen, X. D., Tang, J. M., Qiao, Z. G., & Wu, X. Y. (2019). Mechanism of metformin enhancing the sensitivity of human pancreatic cancer cells to gem-citabine by regulating the PI3K/Akt/mTOR signaling pathway. European Review for Medical and Pharmacological Sciences. https://doi.org/10.26355/eurrev_201912_19666.
Bodoky, G., Timcheva, C., Spigel, D. R., la Stella, P. J., Ciuleanu, T. E., Pover, G., & Tebbutt, N. C. (2012). A phase II open-label randomized study to assess the efficacy and safety of selumetinib (AZD6244 [ARRY-142886]) versus capecitabine in patients with advanced or metastatic pancreatic cancer who have failed first-line gemcitabine therapy. Investigational New Drugs, 30, 1216–1223. https://doi.org/10.1007/s10637-011-9687-4.
Ko, A. H., et al. (2013). Dual MEK/EGFR inhibition for advanced, chemotherapy-refractory pancreatic cancer: A multicenter phase II trial of selumetinib (AZD6244; ARRY-142886) plus erlotinib. Journal of Clinical Oncology. https://doi.org/10.1200/jco.2013.31.15_suppl.4014.
Infante, J. R., Somer, B. G., Park, J. O., Li, C. P., Scheulen, M. E., Kasubhai, S. M., Oh, D. Y., Liu, Y., Redhu, S., Steplewski, K., & le, N. (2014). A randomised, double-blind, placebo-controlled trial of trametinib, an oral MEK inhibitor, in combination with gemcitabine for patients with untreated metastatic adenocarcinoma of the pancreas. European Journal of Cancer, 50, 2072–2081. https://doi.org/10.1016/j.ejca.2014.04.024.
Mihaylova, M. M., & Shaw, R. J. (2011). The AMPK signalling pathway coordinates cell growth, autophagy and metabolism. Nature Cell Biology. https://doi.org/10.1038/ncb2329.
Egan, D. F., et al. (2011). Phosphorylation of ULK1 (hATG1) by AMP-activated protein kinase connects energy sensing to mitophagy. Science (80-.). https://doi.org/10.1126/science.1196371.
Vessoni, A. T., et al. (2016). Chloroquine-induced glioma cells death is associated with mitochondrial membrane potential loss, but not oxidative stress. Free Radical Biology & Medicine. https://doi.org/10.1016/j.freeradbiomed.2015.11.008.
Boya, P., et al. (2003). Mitochondrial membrane permeabilization is a critical step of lysosome-initiated apoptosis induced by hydroxychloroquine. Oncogene. https://doi.org/10.1038/sj.onc.1206622.
Kinsey, C. G., et al. (2019). Protective autophagy elicited by RAF→MEK→ERK inhibition suggests a treatment strategy for RAS-driven cancers. Nature Medicine. https://doi.org/10.1038/s41591-019-0367-9.
Jiang, H., et al. (2018). Concurrent HER or PI3K inhibition potentiates the antitumor effect of the ERK inhibitor ulixertinib in preclinical pancreatic cancer models. Molecular Cancer Therapeutics. https://doi.org/10.1158/1535-7163.MCT-17-1142.
Souchelnytskyi, S., Rönnstrand, L., Heldin, C. H., & ten Dijke, P. (2001). Phosphorylation of Smad signaling proteins by receptor serine/threonine kinases. Methods in Molecular Biology. https://doi.org/10.1385/1-59259-059-4:107.
Massagué, J., Blain, S. W., & Lo, R. S. (2000). TGFβ signaling in growth control, cancer, and heritable disorders. Cell. https://doi.org/10.1016/S0092-8674(00)00121-5.
Wilentz, R. E., et al. (2000). Immunohistochemical labeling for Dpc4 mirrors genetic status in pancreatic adenocarcinomas: A new marker of DPC4 inactivation. The American Journal of Pathology. https://doi.org/10.1016/S0002-9440(10)64703-7.
Singh, P., Srinivasan, R., & Wig, J. D. (2012). SMAD4 genetic alterations predict a worse prognosis in patients with pancreatic ductal adenocarcinoma. Pancreas. https://doi.org/10.1097/MPA.0b013e318247d6af.
Sánchez-Elsner, T., Botella, L. M., Velasco, B., Corbí, A., Attisano, L., & Bernabéu, C. (2001). Synergistic cooperation between hypoxia and transforming growth factor-β pathways on human vascular endothelial growth factor gene expression. The Journal of Biological Chemistry. https://doi.org/10.1074/jbc.M104536200.
Massagué, J. (2008). TGFβ in Cancer. Cell. https://doi.org/10.1016/j.cell.2008.07.001.
Nemunaitis, J., et al. (2006). Phase 1/2 trial of autologous tumor mixed with an allogeneic GVAX® vaccine in advanced-stage non-small-cell lung cancer. Cancer Gene Therapy. https://doi.org/10.1038/sj.cgt.7700922.
Trotta, R., et al. (2008). TGF-β utilizes SMAD3 to inhibit CD16-mediated IFN-γ production and antibody-dependent cellular cytotoxicity in human NK cells. Journal of Immunology. https://doi.org/10.4049/jimmunol.181.6.3784.
Thomas, D. A., & Massagué, J. (2005). TGF-β directly targets cytotoxic T cell functions during tumor evasion of immune surveillance. Cancer Cell. https://doi.org/10.1016/j.ccr.2005.10.012.
Wilson, E. B., et al. (2011). Human tumour immune evasion via TGF-β blocks NK cell activation but not survival allowing therapeutic restoration of anti-tumour activity. PLoS One. https://doi.org/10.1371/journal.pone.0022842.
Hussussian, C. J., et al. (1994). Germline p16 mutations in familial melanoma. Nature Genetics. https://doi.org/10.1038/ng0994-15.
Vasen, H. F. A., Gruis, N. A., Frants, R. R., Van Der Velden, P. A., Hille, E. T. M., & Bergman, W. (2000). Risk of developing pancreatic cancer in families with familial atypical multiple mole melanoma associated with a specific 19 deletion of p16 (p16-Leiden). International Journal of Cancer, 87, 809–811. https://doi.org/10.1002/1097-0215(20000915)87:6<809::AID-IJC8>3.0.CO;2-U.
Tang, B., et al. (2015). Clinicopathological significance of CDKN2A promoter hypermethylation frequency with pancreatic cancer. Scientific Reports, (1), 1. https://doi.org/10.1038/srep13563.
Finn, R. S., et al. (2016). Palbociclib and letrozole in advanced breast cancer. The New England Journal of Medicine, 1(1). https://doi.org/10.1056/NEJMoa1607303.
Hortobagyi, G. N., et al. (2016). Ribociclib as first-line therapy for HR-positive, advanced breast cancer. The New England Journal of Medicine, 1(1). https://doi.org/10.1056/NEJMoa1609709.
Sledge, G. W., et al. (2017). MONARCH 2: Abemaciclib in combination with fulvestrant in women with HR+/HER2-advanced breast cancer who had progressed while receiving endocrine therapy. Journal of Clinical Oncology, 1(1). https://doi.org/10.1200/JCO.2017.73.7585.
Dhir, T., et al. (2019). Abemaciclib is effective against pancreatic cancer cells and synergizes with HuR and YAP1 inhibition. Molecular Cancer Research, 1, 1. https://doi.org/10.1158/1541-7786.MCR-19-0589.
Abrams, S. L., et al. (2018). Introduction of WT-TP53 into pancreatic cancer cells alters sensitivity to chemotherapeutic drugs, targeted therapeutics and nutraceuticals. Advances in Biological Regulation, 1, 1. https://doi.org/10.1016/j.jbior.2018.06.002.
Clayman, G. L., et al. (1995). In vivo molecular therapy with p53 adenovirus for microscopic residual head and neck squamous carcinoma. Cancer Research.
Eastham, J. A., et al. (1995). In vivo gene therapy with p53 or p21 adenovirus for prostate cancer. Cancer Research, 1(1).
Lesoon Wood, L. A., Kim, W., Kleinman, H. K., Weintraub, B. D., & Mixson, A. J. (1995). Systemic gene therapy with p53 reduces growth and metastases of a malignant human breast cancer in nude mice. Human Gene Therapy, 1, 1. https://doi.org/10.1089/hum.1995.6.4-395.
zhi Wu, S., et al. (2019). Dihydrosanguinarine suppresses pancreatic cancer cells via regulation of mut-p53/WT-p53 and the Ras/Raf/Mek/Erk pathway. Phytomedicine, 1, 1. https://doi.org/10.1016/j.phymed.2019.152895.
Stojanovic, N., et al. (2017). HDAC1 and HDAC2 integrate the expression of p53 mutants in pancreatic cancer. Oncogene, 1, 1. https://doi.org/10.1038/onc.2016.344.
Münster, P., et al. (2007). Phase I trial of histone deacetylase inhibition by valproic acid followed by the topoisomerase II inhibitor epirubicin in advanced solid tumors: A clinical and translational study. Journal of Clinical Oncology, 1, 1. https://doi.org/10.1200/JCO.2006.08.6165.
Pili, R., et al. (2012). Phase i study of the histone deacetylase inhibitor entinostat in combination with 13-cis retinoic acid in patients with solid tumours. British Journal of Cancer. https://doi.org/10.1038/bjc.2011.527.
Pauer, L. R., et al. (2004). Phase I study of oral CI-994 in combination with carboplatin and paclitaxel in the treatment of patients with advanced solid tumors. Cancer Investigation. https://doi.org/10.1081/CNV-200039852.
Richards, D. A., et al. (2006). Gemcitabine plus CI-994 offers no advantage over gemcitabine alone in the treatment of patients with advanced pancreatic cancer: Results of a phase II randomized, double-blind, placebo-controlled, multicenter study. Annals of Oncology. https://doi.org/10.1093/annonc/mdl081.
Chan, E., et al. (2016). Phase i trial of vorinostat added to chemoradiation with capecitabine in pancreatic cancer. Radiotherapy and Oncology. https://doi.org/10.1016/j.radonc.2016.04.013.
Hewish, M., Lord, C. J., Martin, S. A., Cunningham, D., & Ashworth, A. (2010). Mismatch repair deficient colorectal cancer in the era of personalized treatment. Nature Reviews. Clinical Oncology. https://doi.org/10.1038/nrclinonc.2010.18.
Le, D. T., et al. (2017). Mismatch repair deficiency predicts response of solid tumors to PD-1 blockade. Science (80-.). https://doi.org/10.1126/science.aan6733.
Hu, Z. I., et al. (2018). Evaluating mismatch repair deficiency in pancreatic adenocarcinoma: Challenges and recommendations. Clinical Cancer Research. https://doi.org/10.1158/1078-0432.CCR-17-3099.
Humphris, J. L., et al. (2017). Hypermutation in pancreatic cancer. Gastroenterology. https://doi.org/10.1053/j.gastro.2016.09.060.
Lupinacci, R. M., et al. (2018). Prevalence of microsatellite instability in intraductal papillary mucinous neoplasms of the pancreas. Gastroenterology. https://doi.org/10.1053/j.gastro.2017.11.009.
(2017). FDA grants accelerated approval to pembrolizumab for first tissue/site agnostic indication. Journal of Medical Case Reports. https://doi.org/10.31525/fda1-ucm560040.htm.
Nakata, B., et al. (2002). Prognostic value of microsatellite instability in resectable pancreatic cancer. Clinical Cancer Research.
Yamamoto, H., et al. (2001). Genetic and clinical features of human pancreatic ductal adenocarcinomas with widespread microsatellite instability. Cancer Research.
Nesselhut, J., et al. (2016). Systemic treatment with anti-PD-1 antibody nivolumab in combination with vaccine therapy in advanced pancreatic cancer. Journal of Clinical Oncology. https://doi.org/10.1200/jco.2016.34.15_suppl.3092.
Weiss, G. J., Blaydorn, L., Beck, J., Bornemann-Kolatzki, K., Urnovitz, H., Schütz, E., & Khemka, V. (2018). Phase Ib/II study of gemcitabine, nab-paclitaxel, and pembrolizumab in metastatic pancreatic adenocarcinoma. Investigational New Drugs, 36, 96–102. https://doi.org/10.1007/s10637-017-0525-1.
Zhang, J., & Walter, J. C. (2014). Mechanism and regulation of incisions during DNA interstrand cross-link repair. DNA Repair (Amst). https://doi.org/10.1016/j.dnarep.2014.03.018.
Klein, A. P. (2012). Genetic susceptibility to pancreatic cancer. Molecular Carcinogenesis. https://doi.org/10.1002/mc.20855.
Holter, S., Borgida, A., Dodd, A., Grant, R., Semotiuk, K., Hedley, D., Dhani, N., Narod, S., Akbari, M., Moore, M., & Gallinger, S. (2015). Germline BRCA mutations in a large clinic-based cohort of patients with pancreatic adenocarcinoma. Journal of Clinical Oncology, 33, 3124–3129. https://doi.org/10.1200/JCO.2014.59.7401.
Venkitaraman, A. R. (2009). Linking the cellular functions of BRCA genes to cancer pathogenesis and treatment. Annual Review of Pathology: Mechanisms of Disease. https://doi.org/10.1146/annurev.pathol.3.121806.151422.
Lowery, M. A., et al. (2011). An emerging entity: Pancreatic adenocarcinoma associated with a known BRCA mutation: Clinical descriptors, treatment implications, and future directions. Oncologist. https://doi.org/10.1634/theoncologist.2011-0185.
(2019). FDA approves olaparib for gBRCAm metastatic pancreatic adenocarcinoma. Journal of Medical Case Reports. https://doi.org/10.31525/cmr-2590075.
Oh, D.-Y., et al. (2019). Olaparib as maintenance treatment following first-line platinum-based chemotherapy (PBC) in patients (pts) with a germline BRCA mutation and metastatic pancreatic cancer (mPC): Phase III POLO trial. Annals of Oncology. https://doi.org/10.1093/annonc/mdz422.004.
Binder KAR et al., “ Abstract CT234: A phase II, single arm study of maintenance rucaparib in patients with platinum-sensitive advanced pancreatic cancer and a pathogenic germline or somatic mutation in BRCA1, BRCA2 or PALB2 ,” 2019, https://doi.org/10.1158/1538-7445.am2019-ct234.
Shroff, R. T., et al. (2018). Rucaparib monotherapy in patients with pancreatic cancer and a known deleterious BRCA mutation. JCO Precision Oncology. https://doi.org/10.1200/po.17.00316.
Tuli, R., et al. (2019). A phase 1 study of veliparib, a PARP-1/2 inhibitor, with gemcitabine and radiotherapy in locally advanced pancreatic cancer. EBioMedicine. https://doi.org/10.1016/j.ebiom.2018.12.060.
Lowery, M. A., et al. (2018). Phase II trial of veliparib in patients with previously treated BRCA-mutated pancreas ductal adenocarcinoma. European Journal of Cancer. https://doi.org/10.1016/j.ejca.2017.11.004.
Pishvaian, M. J., et al. (2019). Outcomes in patients with pancreatic adenocarcinoma with genetic mutations in DNA damage response pathways: Results from the know your tumor program. JCO Precision Oncology. https://doi.org/10.1200/po.19.00115.
O’Kane, G. M., et al. (2020). Homologous recombination deficiency (HRD) scoring in pancreatic ductal adenocarcinoma (PDAC) and response to chemotherapy. Journal of Clinical Oncology. https://doi.org/10.1200/jco.2020.38.4_suppl.741.
O’Kane, G. M., et al. (2020). Outcomes and immunogenicity of pancreatic cancer stratified by the HRDetect score. Journal of Clinical Oncology. https://doi.org/10.1200/jco.2020.38.15_suppl.4630.
Blackburn, E. H. (1994). Telomeres: No end in sight. Cell., 1, 1. https://doi.org/10.1016/0092-8674(94)90046-9.
De Lange, T. (2002). Protection of mammalian telomeres. Oncogene., 1(1). https://doi.org/10.1038/sj/onc/1205080.
Wright, W. E., Piatyszek, M. A., Rainey, W. E., Byrd, W., & Shay, J. W. (1996). Telomerase activity in human germline and embryonic tissues and cells. Developmental Genetics, 1, 1. https://doi.org/10.1002/(SICI)1520-6408(1996)18:2<173::AID-DVG10>3.0.CO;2-3.
Shay, J. W., & Bacchetti, S. (1997). A survey of telomerase activity in human cancer. European Journal of Cancer Part A, 1, 1. https://doi.org/10.1016/S0959-8049(97)00062-2.
Hiyama, E., et al. (1997). Telomerase activity is detected in pancreatic cancer but not in benign tumors. Cancer Research, 1, 1.
Harley, C. B. (2008). Telomerase and cancer therapeutics. Nature Reviews. Cancer, 1(1). https://doi.org/10.1038/nrc2275.
Ouellette, M. M., Wright, W. E., & Shay, J. W. (2011). Targeting telomerase-expressing cancer cells. Journal of Cellular and Molecular Medicine, 1, 1. https://doi.org/10.1111/j.1582-4934.2011.01279.x.
Blackburn, E. H., & Collins, K. (2011). Telomerase: An RNP enzyme synthesizes DNA. Cold Spring Harbor Perspectives in Biology, 1, 1. https://doi.org/10.1101/cshperspect.a003558.
White, L. K., Wright, W. E., & Shay, J. W. (2001). Telomerase inhibitors. Trends in Biotechnology, 1, 1. https://doi.org/10.1016/S0167-7799(00)01541-9.
Herbert, B. S., et al. (2005). Lipid modification of GRN163, an N3′→P5′ thio-phosphoramidate oligonucleotide, enhances the potency of telomerase inhibition. Oncogene, 1, 1. https://doi.org/10.1038/sj.onc.1208760.
Burchett, K. M., Yan, Y., & Ouellette, M. M. (2014). Telomerase inhibitor Imetelstat (GRN163L) limits the lifespan of human pancreatic cancer cells. PLoS One, (1), 1. https://doi.org/10.1371/journal.pone.0085155.
Choi, K. H., Farrell, A. S., Lakamp, A. S., & Ouellette, M. M. (2011). Characterization of the DNA binding specificity of Shelterin complexes. Nucleic Acids Research, 1, 1. https://doi.org/10.1093/nar/gkr665.
Palm, W., & de Lange, T. (2008). How shelterin protects mammalian telomeres. Annual Review of Genetics, (1), 1. https://doi.org/10.1146/annurev.genet.41.110306.130350.
Schreiber, V., Dantzer, F., Amé, J. C., & De Murcia, G. (2006). Poly(ADP-ribose): Novel functions for an old molecule. Nature Reviews. Molecular Cell Biology, 1, 1. https://doi.org/10.1038/nrm1963.
Smith, S., Giriat, I., Schmitt, A., & De Lange, T. (1998). Tankyrase, a poly(ADP-ribose) polymerase at human telomeres. Science (80-.). https://doi.org/10.1126/science.282.5393.1484.
Dantzer, F., et al. (2004). Functional interaction between poly(ADP-ribose) polymerase 2 (PARP-2) and TRF2: PARP activity negatively regulates TRF2. Molecular and Cellular Biology, 1, 1. https://doi.org/10.1128/mcb.24.4.1595-1607.2004.
Gomez, M., Wu, J., Schreiber, V., Dunlap, J., Dantzer, F., Wang, Y., & Liu, Y. (2006). PARP1 is a TRF2-associated poly(ADP-ribose)polymerase and protects eroded telomeres. Molecular Biology of the Cell, 17, 1686–1696. https://doi.org/10.1091/mbc.E05-07-0672.
Beneke, S., Cohausz, O., Malanga, M., Boukamp, P., Althaus, F., & Bürkle, A. (2008). Rapid regulation of telomere length is mediated by poly(ADP-ribose) polymerase-1. Nucleic Acids Research. https://doi.org/10.1093/nar/gkn615.
Donà, F., et al. (2013). Poly(ADP-ribosylation) and neoplastic transformation: Effect of PARP inhibitors. Current Pharmaceutical Biotechnology. https://doi.org/10.2174/138920101405131111104642.
Seimiya, H., Muramatsu, Y., Ohishi, T., & Tsuruo, T. (2005). Tankyrase 1 as a target for telomere-directed molecular cancer therapeutics. Cancer Cell. https://doi.org/10.1016/j.ccr.2004.11.021.
Burchett, K. M., Etekpo, A., Batra, S. K., Yan, Y., & Ouellette, M. M. (2017). Inhibitors of telomerase and poly(ADP-ribose) polymerases synergize to limit the lifespan of pancreatic cancer cells. Oncotarget. https://doi.org/10.18632/oncotarget.19410.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Areas covered
This review covers the molecular drivers in the cell and the cell membrane involved in the development and progression of PDAC and novel therapeutic agents targeting them.
Rights and permissions
About this article
Cite this article
Al-Share, B., Hammad, N. & Diab, M. Pancreatic adenocarcinoma: molecular drivers and the role of targeted therapy. Cancer Metastasis Rev 40, 355–371 (2021). https://doi.org/10.1007/s10555-020-09948-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10555-020-09948-w