Abstract
The prompt and precise identification of hemodynamically significant coronary artery lesions remains an ongoing challenge. This study investigated the diagnostic value of non-invasive global left ventricular myocardial work indices by echocardiography in functional status of coronary artery disease (CAD) patients with myocardial ischemia using fractional flow reserve (FFR) as the gold standard. A total of 77 consecutive patients with clinically suspected CAD were prospectively enrolled. All participants sequentially underwent echocardiography, invasive coronary angiography (ICA) and FFR measurement. According to the results of ICA, patients were divided into myocardial ischemia group (FFR ≤ 0.8, n = 27) and non-myocardial ischemia group (FFR > 0.8, n = 50). Myocardial work indices including global work index (GWI), global constructive work (GCW), global wasted work (GWW), global work efficiency (GWE), global positive work (GPW), global negative work (GNW), global systolic constructive work (GSCW) and global systolic wasted work (GSWW) were obtained by using the non-invasive left ventricular pressure strain loop (PSL) technique. Compared with the non-myocardial ischemia group, GWI, GCW, GPW and GSCW were significantly decreased in the myocardial ischemia group at either the 18-segment level or the 12-segment level (P < 0.001). At the 18-segment level, GWI < 1783.6 mmHg%, GCW < 1945.4 mmHg%, GPW < 1788.7 mmHg% and GSCW < 1916.5 mmHg% were optimal cut-off value to detect myocardial ischemia with an FFR ≤ 0.8. Global left ventricular myocardial work indices by echocardiography exhibited a good diagnostic value in patients with CAD and may have a good clinical significance for the screening of suspected myocardial ischemia.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
As a significant contributor to cardiovascular mortality worldwide, coronary artery disease (CAD) incurs substantial public health and economic implications [1]. The primary reliance for the clinical diagnosis of at-risk patients is either on medical imaging for providing visualization of anatomical obstruction in coronary arteries or on functional non-invasive stress testing for the detection of myocardial ischemia [2]. The prompt and precise identification of hemodynamically significant coronary artery lesions remains an ongoing challenge. As a diagnostic metric, fractional flow reserve (FFR) is established as the gold standard for assessing coronary myocardial ischemic [3]. However, in instances where patients do not require coronary intervention, the preferential adoption of FFR as a screening method becomes unsuitable due to the procedure’s invasive nature, accompanying high cost, and the potential for complications [4]. Aligning with the 2019 European Society of Cardiology (ESC) guidelines, the recommendations endorse the use of noninvasive testing as the initial diagnostic approach over invasive tests for CAD [5]. Echocardiography, as a non-invasive imaging technique for evaluating coronary artery stenosis, facilitates clinicians in diagnosing intricate coronary syndromes, thus rendering itself as a primary diagnostic tool for CAD [6]. Conventional echocardiography was implemented to scrutinize the myocardial function by visually inspecting ventricular wall motion. Yet, this qualitative method encompasses inherent limitations and is insufficient for distinguish subtle signs of myocardial ischemia [7]. Recent research posits that speckle tracking echocardiography is proficient in detecting myocardial longitudinal strain damage in patients with severe coronary artery stenosis [8,9,10]. Furthermore, it can provide a comprehensive and quantitative assessment of myocardial function, as well as differentiate between ischemic segments of dysfunctional myocardium and normal segments [11]. However, it’s pivotal to be noted that this specific method remains load-dependent and cannot accurately represent myocardial work (MW) or oxygen consumption. subsequently affecting the accuracy of assessing myocardial function [12, 13].
In recent years, the myocardial work index (MWI) premised on non-invasive pressure strain loop (PSL) technology, amalgamated with standardized left ventricular pressure and segmental strain emerges as a novel methodology to evaluate left ventricular myocardial ischemic alterations [14, 15]. This credence technology can provide incremental value for cardiac function assessment by analyzing the strain associated with dynamic left ventricular systolic pressure to account for deformation and afterload [16, 17].
The aim of this study is to explore the difference in global myocardial work among patients of suspected CAD, stratified by the presence or absence of myocardial ischemia. Additionally, the study underscores the feasibility and clinical utility of PSL in diagnosing myocardial ischemia.
Methods
Patient population and study design
This was a prospective, single-center study to investigate the diagnostic efficacy of global myocardial work in detecting myocardial ischemia (Fig. 1). Between October 2020 and September 2022, suspected CAD patients with stable chest pain in Zhongshan Hospital, Fudan University were enrolled. All patients underwent echocardiography, invasive coronary angiography (ICA) and FFR measurement (within 24 h). Inclusion criteria were as follows: (1) ≥ 18 years old; (2) Presence of sinus rhythm; (3) Clinical indication for coronary angiography; (4) Angina pectoris related symptoms or abnormal ECG examination. Exclusion criteria were as follows: (1) Left ventricular ejection fraction (LVEF) less than 55%; (2) Resting regional wall motion abnormalities; (3) Obstruction of the left ventricular outflow tract, including aortic stenosis, aortic valve replacement, hypertrophic cardiomyopathy, or other significant valvular disease; (4) Previous myocardial infarction with total occlusion or severe stenosis and documented collateral circulation; (5) Insufficient image quality for speckle tracking analysis [18]. All study procedures were approved by the Ethics Committee of Zhongshan Hospital, Fudan University, and all patients provided their informed consent for this study. All methods were performed in accordance with the applicable guidelines and regulations.
ICA and FFR measurements
Caffeine intake was strictly prohibited 24 h prior to invasive procedures. ICA and FFR measurements were meticulously performed according to standard guidelines [19]. FFR measurements were conducted by experienced interventional cardiologists in a blinded fashion and performed in lesions utilizing a pressure wire (Aeris, St.Jude Medical) under resting state and hyperemic state during a continuous intravenous infusion of adenosine(140 μg/kg·min). FFR was measured in coronary stenosis varying from 30 to 90% and at least one vessel with a reference diameter ≥ 2.0 mm during ICA. The FFR value was automatically calculated as the ratio of mean pressure (Pd) to mean aortic pressure (Pa) in the distal part of the stenotic vessel through the pressure guidewire and the guiding catheter, respectively. FFR value ≤ 0.8 was defined as the gold standard for diagnosing myocardial ischemia [20].
Conventional echocardiography
Transthoracic echocardiography was performed by experienced sonographers using GE Vivid E95 ultrasound device (GE Vingmed ultrasound, Horten, Norway) with an M5S 3.5 MHz transducer. The parasternal long axis view, basal, middle and apical short axis view of left ventricle, and apical 2-, 3-, and 4-chamber views were obtained. All view acquisition and parameter measurements were performed in strict accordance with the 2019 American Society of Echocardiography guidelines for adult transthoracic echocardiography [21]. The left ventricular end diastolic dimension (LVEDD), left ventricular end systolic dimension (LVESD), inter-ventricular septal thickness (IVST) and post wall thickness (PWT) was measured in the parasternal left ventricular long-axis view of conventional echocardiography. Peak early diastolic velocity (E) and peak late diastolic velocity (A) of mitral flow were obtained by pulsed Doppler in apical four-chamber view, and E/A value was calculated. In the tissue Doppler imaging (TDI) mode, the sampling volume was placed on the lateral wall of the left ventricle to obtain the early diastolic tissue velocity (e’), thus enabling the calculation of the E/e’ value. The left ventricular end diastolic volume (LVEDV), left ventricular end systolic volume (LVESV) and left ventricular ejection fraction (LVEF) were quantified using Simpson’s method in both apical four-chamber and two-chamber views.
Speckle tracking echocardiography and pressure-strain loop technique
The initial echocardiography data were imported into the EchoPAC 203 workstation for subsequent offline speckle tracking echocardiography (STE) analysis. The opening and closing time of mitral valve and aortic valve were set, and the endocardial surface was manually delineated on the four-chamber, three-chamber, and two-chamber views of the left ventricular apex, respectively. The strain curves for the corresponding segments of the left ventricle were obtained automatically. The peak left ventricular systolic pressure was assumed to be equal to the peak brachial cuff systolic pressure measured simultaneously at the time of the echocardiogram examination [18].
Systolic and diastolic blood pressure were inputted to compute the global longitudinal strain (GLS), global work index (GWI), global constructive work (GCW), global wasted work (GWW) and global work efficiency (GWE). GLS is defined as the average peak systolic longitudinal strain of three apical views [22]. GWI represents the cumulative work conducted under PSL from mitral valve closure to mitral valve opening. GCW refers to the work executed by the left ventricular myocardium during systole shortening or isovolumic diastole lengthening, which is advantageous for left ventricular ejection. GWW signifies the work expended by lengthening the myocardium during systole or shortening the myocardium during isovolumic diastole, which is detrimental to left ventricular ejection. GWE is calculated as the proportion of GCW to the sum of GCW and GWW, expressed as a percentage, quantifying the effectiveness of work achieved during a cardiac cycle.
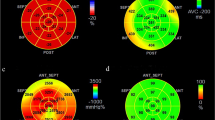
Global positive work (GPW) entails the beneficial work performed by the myocardium in each cardiac cycle, while global negative work (GNW) represents the wasted work performed by the myocardium during each cardiac cycle. Global systolic constructive work (GSCW) pertains to the energetic output generated by the myocardium of the left ventricle during the systolic phase. Global systolic wasted work (GSWW) pertains to the inefficiency of the left ventricular myocardium during the systolic phase [23,24,25] (Fig. 2).
Echocardiographic results of typical cases of myocardial ischemia and non-myocardial ischemia A.B: Non-myocardial ischemia. The area of the left ventricular PSL building module is large. The bull’s eye diagram shows that the peak systolic strain of each segment is within the normal range; C.D: Myocardial ischemia, The area of the left ventricular PSL building module is small. The bull’s eye diagram shows that the peak strain of each segment during systole decreases
The left ventricular myocardium was segmented using an 18-segment model [26], and further categorized into three distinct myocardial rings, namely, the basal ring, the intermediate ring, and the apical ring. The 18-segment level global myocardial work index is calculated as the average of the sum of the work performed by each segment in the 18-segment model. The 12-segment level global myocardial work index was obtained by excluding the 6 segments of the apical ring (Fig. 3). The analysis of speckle tracking echocardiography was conducted by sonographers who were blinded to other information. In order to ensure accuracy and precision, all parameters underwent triadic measurements by one experienced sonographer to ensure accuracy and precision, and the results were documented as the averaged data.
Repeatability test
The left ventricular work index and GLS of 22 patients were repeated. The intra-observer difference is the comparison of the results taken by the same observer more than 24 h apart, and the inter-observer difference is the comparison of the results measured by two independent observers. Both intra-observer and inter-observer differences are quantified using intraclass correlation coefficient (ICC) analysis.
Endpoints and statistical analysis
The primary endpoint of this study was the assessment of the diagnostic efficacy of global left ventricular myocardial work indices in myocardial ischemia for suspected CAD patients. Secondary endpoints included sensitivity, specificity, and area under the receiver-operating characteristic curve (AUC) of GWI, GCW, GPW and GSCW in comparison to LVEF and GLS for the diagnostic performance. All results were analyzed at the 18 and 12 segment level.
General statistical analysis and subsequent receiver operating characteristic (ROC) analysis was meticulously conducted using IBM SPSS Statistics 20 (IBM SPSS Statistics, Chicago, IL, USA) and MedCalc statistical software, version 19.6.4 (MedCalc Software bv, Ostend, Belgium). Continuous variables were presented as mean ± standard deviation and were compared by Student t test or Student t’ test if normally distributed, were presented as median (range) if non-normally distributed and were compared by Mann-Whitney U test. Normal distribution was assessed by use of the Kolmogorov-Smirnov (K-S) test. To evaluate the diagnostic efficacy of echocardiographic parameters, ROC curve and the area under the curve (AUC) were assessed. The optimal cutoff values for each parameter were determined using the Youden’s index. Sensitivity and specificity were calculated with 95% confidence intervals (CI) as diagnostic parameters. AUC was compared using Delong’s test to evaluate the discriminatory power. A P-value of <0.05 was considered statistically significant.
Results
Patient characteristics
Between October 2020 to September 2022, a cohort of 1385 consecutive symptomatic patients were included in this study and recommended for echocardiographic examination.
104 patients underwent subsequent invasive coronary angiography and FFR measurement. It was observed that six patients exhibited a left ventricular ejection fraction (LVEF) below 55%. Additionally, abnormal left ventricular wall motion was detected in eight patients, prior myocardial infraction was documented in four patients, and poor speckle tracking image quality was experienced by nine patients. Consequently, following the exclusion of 27 patients, a total of 77 patients (62.6 ± 9.5 years, 61.0% male) were enrolled in the final analysis.
Overall, all the patients had angina pectoris, 55.8% had hypertension, 33.8% had hyperlipidemia, 26.0% had diabetes, 29.9% were previous or current smokers and 16.9% had a family history of CAD. Additional clinical and echocardiographic baseline characteristics are detailed in Table 1.
Analysis of myocardial work in the presence and absence of reduced FFR
It was observed that 27 patients (35.1%) exhibited myocardial ischemia, as indicated by an invasive FFR ≤ 0.80, while remaining 50 patients (64.9%) were not exhibit hemodynamically significant (invasive FFR > 0.80). Based on the 18-segment myocardial segmentation model, the parameters GLS, GWI, GCW, GPW and GSCW exhibited a significant decrease in patients with myocardial ischemia compared to non-ischemic patients at the 18and 12-segment levels. Further measurement results are presented in Tables 2 and 3.
The inter-operator agreement as assessed by the ICC analysis was excellent for GWI (0.855, 95% CI, 0.752–0.917), GCW (0.906, 95% CI, 0.935–0.948), GPW (0.901, 95% CI, 0.826–0.944) and GSCW (0.888, 95% CI, 0.805–0.937) and intra-operator agreement is 0.913 (95% CI, 0.848–0.951) for GWI, 0.916 (95% CI, 0.852–0.953) for GCW, 0.920 (95% CI, 0.858–0.955) for GPW and 0.912 (95% CI, 0.845–0.950) for GSCW.
Diagnostic performance of global longitudinal peak systolic strain and global myocardial work at the 18-segment level for myocardial ischemia
The diagnostic performance of global MWI and GLPSS for the detection of functionally significant coronary artery disease (CAD) at the 18-segment level is presented in Table 4. As shown in Fig. 4, the AUC for GWI, GCW, GPW and GSCW were 0.819 (95% CI: 0.724 to 0.914), 0.850 (95% CI: 0.763 to 0.936), 0.859 (95% CI: 0.775 to 0.944) and 0.850 (95% CI: 0.764 to 0.937), respectively. These values were significantly higher than the AUC for GLS (0.737; 95% CI: 0.623 to 0.852; p < 0.001).
The optimal cutoff value of GLS was determined to be -17.3%, exhibiting a sensitivity of 74.1%, specificity of 68.0%, and an accuracy of 70.1%. The optimal cutoff values for GWI, GCW, GPW and GSCW were determined to be 1783.6 mmHg% (with a sensitivity of 77.8%, specificity of 68.0%, and accuracy of 71.4%), 1945.4 mmHg% (with a sensitivity of 74.1%, specificity of 80.0%, and accuracy of 77.9%), 1788.7 mmHg% (with a sensitivity of 63.0%, specificity of 90.0%, and accuracy of 80.5%), and 1916.5 mmHg% (with a sensitivity of 81.5%, specificity of 72.0%, and accuracy of 75.3%), respectively. At the 18-segment level, the diagnostic accuracy parameters of GWI, GCW, GPW, and GSCW were found to be superior to GLS for predicting ischemia. Furthermore, the accuracy, sensitivity, and specificity of GWI, GCW, GPW, and GSCW in predicting functionally significant CAD remained consistently high across an extensive range.
Diagnostic performance of global longitudinal peak systolic strain and global myocardial work at the 12-segment level for myocardial ischemia
The diagnostic performance of global GWI and GLS for the detection of functionally significant CAD at the 12-segment level is presented in Table 5. As illustrated in Fig. 5,
the AUC for GWI, GCW, GPW and GSCW were 0.860 (95% CI: 0.774 to 0.946; p < 0.001), 0.855 (95% CI: 0.767 to 0.943; p < 0.001), 0.876 (95% CI: 0.793 to 0.959; p < 0.001) and 0.870 (95% CI: 0.787 to 0.953; p < 0.001), respectively. These values were significantly higher than the AUC for GLS (0.711; 95% CI: 0.591 to 0.832; p < 0.001).
The optimal cutoff value of GLS was determined to be -14.5%, exhibiting a sensitivity of 65.2%, specificity of 68.3%, and an accuracy of 72.7%. The optimal cutoff values for GWI, GCW, GPW and GSCW were determined to be 1515.3 mmHg% (with a sensitivity of 74.1%, specificity of 84.0%, and accuracy of 80.5%), 1739.3 mmHg% (with a sensitivity of 70.4%, specificity of 86.0%, and accuracy of 80.5%), 1610.8 mmHg% (with a sensitivity of 66.7%, specificity of 96.0%, and accuracy of 85.7%), and 1668.2 mmHg% (with a sensitivity of 77.8%, specificity of 82.0%, and accuracy of 80.5%), respectively. At the 12-segment level, the diagnostic accuracy parameters of GWI, GCW, GPW, and GSCW were found to be superior to GLS in predicting ischemia. Compared to the data at the 18-segment level, the diagnostic performance of GWI, GCW, GPW and GSCW in detecting functionally significant CAD showed improvement at the 12-segment level.
Discussion
Our study represented the initial exploration of the diagnostic efficacy of global GWI and GLS in detecting myocardial ischemia among symptomatic suspected CAD patients, through a head-to-head comparative analysis. The key findings of this study revealed a significant decrease in GWI, GCW, GPW and GSCW among patients with myocardial ischemia (FFR ≤ 0.8) as opposed to those without myocardial ischemia (FFR > 0.8). The diagnostic performance of global GWI was found to be excellent and demonstrated superiority over GLS in detecting myocardial ischemia. Furthermore, a trend of enhancement in diagnostic performance was observed for the global GWI as the count of apical ring segments was reduced. Additionally, the insights derived from our study lend credence to adopting, in clinically applicable scenarios, the noninvasive STE procedure as a strategy for identifying substantial myocardial ischemia.
The clinical significance of implementing FFR as a standard to evaluate the severity of lesions in coronary artery disease has been widely recognized [27, 28], and FFR ≤ 0.80 has validated as a reliable indicator to distinguish the presence or absence of significant hemodynamic lesions [29]. Therefore, FFR was employed as the gold standard for the assessment of the functional condition of coronary artery lesions in the current study.
Despite the notable benefits of FFR in identifying ischemia-related coronary artery lesions, its invasive nature, potential side effects, and high costs remain significant factors constraining its clinical application [4, 30, 31]. In recent years, advancements in echocardiography technology, which is a noninvasive and user-friendly imaging method, have led to increased diagnostic accuracy in coronary artery disease (CAD), thus making it a promising tool for early detection of complex coronary syndrome [6]. Conventional echocardiography requires particularly experienced clinicians to detect abnormal ventricular wall motion, thus rough qualitative detection of myocardial function. Obviously, this method may ignore the subtle manifestation of myocardial ischemia [7]. LVEF may occasionally reflect myocardial function in CAD patients presenting with severe left ventricular dysfunction, yet its correlation and consistency with CAD severity are often inadequate [32,33,34]. Consistent with these observations, our findings also indicated no significant difference in LVEF between patients with and without myocardial ischemia.
STE empowers the quantitative analysis of regional ventricular wall movement via a detailed examination of myocardial velocity and strain. This technique provides comprehensive insights into cardiac functionality and risk stratification [35], ultimately benefitting the identification of subtle myocardial deformations, the magnitude of which may pose considerable difficulty using traditional methodologies. GLS derived from STE, has been extensively demonstrated as a highly sensitive indicator of myocardial ischemia [36, 37]. It has been found to outperform conventional parameters like wall thickening in the detection of myocardial ischemia [38,39,40]. This was consistent in our study, with a sensitivity of 74.1%, specificity of 68.0%, accuracy of 70.1% and an AUC of 0.737 in detecting myocardial ischemia by GLS at 18-segment level. This is because regional asynchronous myocardial contraction can occur in ischemic heart disease, leading to significant variability in the duration and amplitude of GLS [41]. This variability, while presenting potential advantages, also has its drawbacks. Importantly, the diagnostic capability of GLS when it comes to identifying myocardial ischemia might be restricted due to the inherent dependency on stress [12, 13].
PSL is an emerging technique that eschews the inherent stress dependence. This technique, when combined with strain, allows for estimation of the left ventricular pressure curve, essentially facilitating the analysis of the left ventricular pressure-strain loop area to quantitatively reflect regional myocardial metabolism [15]. The global GWI, derived from PSL with standardized left ventricular pressure and segmental strain, holds considerable potential value for myocardial ischemia [17]. Previous studies have revealed that MW exposes superior sensitivity and accuracy than LVEF and GLS in detecting CAD patients [42]. Furthermore, among all MW indices, GWI and GCW are more important predictive parameters for detecting ischemia [17, 41]. Our findings not only corroborated the enhanced diagnostic efficacy of GWI and GCW, but also revealed that GPW and GSCW exhibited comparable functionalities. Notably, the diagnostic performance of GWI, GCW, GPW and GSCW in detecting myocardial ischemia was found to supersede that of GLS at the 18-segment level and 12-segment level. Specifically, the sensitivity, specificity, and accuracy of GWI, GCW, GPW, and GSCW emerged superior when juxtaposed with GLS.
In addition, it has been reported that both GWE and GWW have the capability to detect significant CAD under hyperemic state [43]. Nevertheless, our analysis did not reveal any noticeable differentiation in the two parameters between patients with and without myocardial ischemia. The primary factor contributing to this is likely the measurement method employed during the resting state of patients, where the alteration in workload isn’t inherently discernible from GWW. GCW significantly surpasses that of GWW, and GWE is determined by dividing GCW by the sum of GCW and GWW. This calculation further diminishes the impact of GWW on GWE and reduces the variability in GWE.
The cardiac apex plays a crucial role in maintaining the entire contractile functionality of the myocardium [44, 45]. According to Laplace Law, it is observed that the basal region has a larger radius of curvature compared to the apical region and experiences higher wall stress [46]. Therefore, during the early stages of CAD, an accentuated wall stress or stiffness is prominent within the basal myocardium region, leading to initial damage therein. Conversely, the apical myocardium remains unscathed or endures minimal damage. The apical myocardium exhibits an increased work contribution in response to damage in the basal myocardium, thereby ensuring the preservation of normal overall myocardial function [47]. If the persistent imbalance surpasses the regulatory capacity of the apical myocardium, it may cause serious and widespread myocardial injury, resulting in a reduction in GWI, GCW and an elevation in MWW across all segments [48].
In our study, we employed the 18-segment level model to investigate the impact of reducing the apical myocardial segment. This reduction allowed us to assess the global myocardial work at the 12-segment level, thereby enhancing the visibility of myocardial ischemia indicators. The findings indicate that there has been a gradual improvement in the overall myocardial work parameters GWI, GCW, GPW, and GSCW for diagnosing myocardial ischemia at the 18 to 12 segment level. This improvement has correspondingly led to enhancements in sensitivity, specificity, and accuracy.
In this study, the measurement of echocardiographic myocardial work parameters was conducted during resting conditions to alleviate the cardiac stress. Our findings revealed a significant discrepancy in myocardial work between patients with and without myocardial ischemia. From the level of 18 to 12 segments, GWI, GCW, GPW and GSCW in myocardial ischemia patients exhibited a gradual decrease. This denotes a potential initial reduction in myocardial work at rest, which precedes the tangible functional alterations of the heart. Moreover, the myocardial base displayed heightened damage levels, a finding that aligns with our previous discussions.
We have also established 1783.6 mmHg%, 1945.4 mmHg%, 1788.7 mmHg% and 1916.5 mmHg% as the optimal threshold values for GWI, GCW, GPW and GSCW, respectively, in diagnosing myocardial ischemia (FFR ≤ 0.8). The results demonstrated favorable sensitivity (ranging from 63.0 to 81.5%), specificity (ranging from 68.0% to 90.0) and accuracy (ranging from 71.4 to 80.5%). A meta-analysis has indicated that there exists a normal range for the global left ventricular myocardial performance index in adults. The reported normal mean values for GWI and GCW are 2010 mm Hg% (95% CI, 1,907-2,113 mmHg%) and 2278 mm Hg% (95% CI, 2,186-2,369 mmHg%), respectively [49]. The global myocardial work index of our patients without myocardial ischemia (FFR > 0.8) fell within the expected range. Conversely, the global MWI of patients with myocardial ischemia was significantly lower than this range, thus validating the rationality of the results.
Despite the study’s valuable contributions, it is crucial to recognize certain limitations inherent to this research. First, the cohort was recruited exclusively from a single tertiary center, which may limit the generalizability of the findings. Second, the study utilized a relatively modest sample size, which may compromise statistical reliability and result precision. Third, the established cut-off values for global myocardial work parameters, specifically GWI, GCW, GPW, and GSCW in the diagnosis of myocardial ischemia, need further validation with a larger sample size to certify their accuracy and dependability. Lastly, while the potential clinical application of PSL in the early detection of resting-state CAD without necessitating stress imaging looks promising, additional prospective studies should be conducted.
Conclusion
In conclusion, the current study has provided evidence to support the clinical potential of echocardiography-derived myocardial work parameters as novel non-invasive functional indicators for diagnosing myocardial ischemia. At the 18 and 12 segment level, the GWI, GCW, GPW and GSCW are significantly lower in patients with myocardial ischemia compared to those without myocardial ischemia. These parameters demonstrate excellent diagnostic efficacy in identifying functional myocardial ischemia.
Data availability
No datasets were generated or analysed during the current study.
References
Malakar AK, Choudhury D, Halder B, Paul P, Uddin A, Chakraborty S (2019) A review on coronary artery disease, its risk factors, and therapeutics. J Cell Physiol 234:16812–16823. https://doi.org/10.1002/jcp.28350
Rakisheva A, Marwan M, Achenbach S (2020) The ISCHEMIA trial: implications for non-invasive imaging. Anatol J Cardiol 24:2–6. https://doi.org/10.14744/AnatolJCardiol.2020.82428
Raja J, Seitz MP, Yedlapati N, Khouzam RN (2021) Can computed fractional flow reserve coronary CT angiography (FFRCT) offer an accurate noninvasive comparison to invasive coronary angiography (ICA)? The noninvasive CATH. A comprehensive review. Curr Probl Cardiol 46:100642. https://doi.org/10.1016/j.cpcardiol.2020.100642
Zhuang B, Wang S, Zhao S, Lu M (2020) Computed tomography angiography-derived fractional flow reserve (CT-FFR) for the detection of myocardial ischemia with invasive fractional flow reserve as reference: systematic review and meta-analysis. Eur Radiol 30:712–725. https://doi.org/10.1007/s00330-019-06470-8
Saraste A, Knuuti J (2020) ESC 2019 guidelines for the diagnosis and management of chronic coronary syndromes: recommendations for cardiovascular imaging. Herz 45:409–420. https://doi.org/10.1007/s00059-020-04935-x
Pastore MC, Mandoli GE, Contorni F, Cavigli L, Focardi M, D’Ascenzi F, Patti G, Mondillo S, Cameli M (2021) Speckle tracking echocardiography: early predictor of diagnosis and prognosis in coronary artery disease. Biomed Res Int 2021:6685378. https://doi.org/10.1155/2021/6685378
Kvitting JP, Wigström L, Strotmann JM, Sutherland GR (1999) How accurate is visual assessment of synchronicity in myocardial motion? An in vitro study with computer-simulated regional delay in myocardial motion: clinical implications for rest and stress echocardiography studies. J Am Soc Echocardiogr 12:698–705. https://doi.org/10.1016/s0894-7317(99)70019-2
Liel-Cohen N, Tsadok Y, Beeri R, Lysyansky P, Agmon Y, Feinberg MS, Fehske W, Gilon D, Hay I, Kuperstein R et al (2010) A new tool for automatic assessment of segmental wall motion based on longitudinal 2D strain: a multicenter study by the Israeli echocardiography research group. Circ Cardiovasc Imaging 3:47–53. https://doi.org/10.1161/circimaging.108.841874
Dahlslett T, Karlsen S, Grenne B, Eek C, Sjøli B, Skulstad H, Smiseth OA, Edvardsen T, Brunvand H (2014) Early assessment of strain echocardiography can accurately exclude significant coronary artery stenosis in suspected non-ST-segment elevation acute coronary syndrome. J Am Soc Echocardiogr 27:512–519. https://doi.org/10.1016/j.echo.2014.01.019
Mazzitelli M, Torti C, Sabatino J, D’Ascoli GL, Costa C, Pisani V, Raffetti E, De Rosa S, Strazzulla A, Focà A et al (2018) Evaluation of cardiac function by global longitudinal strain before and after treatment with sofosbuvir-based regimens in HCV infected patients. BMC Infect Dis 18:518. https://doi.org/10.1186/s12879-018-3426-9
Kukulski T, Jamal F, Herbots L, D’Hooge J, Bijnens B, Hatle L, De Scheerder I, Sutherland GR (2003) Identification of acutely ischemic myocardium using ultrasonic strain measurements. A clinical study in patients undergoing coronary angioplasty. J Am Coll Cardiol 41:810–819. https://doi.org/10.1016/s0735-1097(02)02934-0
Gao L, Wang Y, Gao M, Chen L (2023) Clinical research progress of myocardial work in assessment and prediction of coronary artery disease in noninvasive pressure-strain loop technique. J Clin Ultrasound 51:38–45. https://doi.org/10.1002/jcu.23326
Hubert A, Le Rolle V, Leclercq C, Galli E, Samset E, Casset C, Mabo P, Hernandez A, Donal E (2018) Estimation of myocardial work from pressure-strain loops analysis: an experimental evaluation. Eur Heart J Cardiovasc Imaging 19:1372–1379. https://doi.org/10.1093/ehjci/jey024
Chan J, Edwards NFA, Khandheria BK, Shiino K, Sabapathy S, Anderson B, Chamberlain R, Scalia GM (2019) A new approach to assess myocardial work by non-invasive left ventricular pressure-strain relations in hypertension and dilated cardiomyopathy. Eur Heart J Cardiovasc Imaging 20:31–39. https://doi.org/10.1093/ehjci/jey131
Russell K, Eriksen M, Aaberge L, Wilhelmsen N, Skulstad H, Remme EW, Haugaa KH, Opdahl A, Fjeld JG, Gjesdal O et al (2012) A novel clinical method for quantification of regional left ventricular pressure-strain loop area: a non-invasive index of myocardial work. Eur Heart J 33:724–733. https://doi.org/10.1093/eurheartj/ehs016
Russell K, Eriksen M, Aaberge L, Wilhelmsen N, Skulstad H, Gjesdal O, Edvardsen T, Smiseth OA (2013) Assessment of wasted myocardial work: a novel method to quantify energy loss due to uncoordinated left ventricular contractions. Am J Physiol Heart Circ Physiol 305:H996–1003. https://doi.org/10.1152/ajpheart.00191.2013
Boe E, Russell K, Eek C, Eriksen M, Remme EW, Smiseth OA, Skulstad H (2015) Non-invasive myocardial work index identifies acute coronary occlusion in patients with non-ST-segment elevation-acute coronary syndrome. Eur Heart J Cardiovasc Imaging 16:1247–1255. https://doi.org/10.1093/ehjci/jev078
Guo Y, Yang C, Wang X, Pei Z, Zhu H, Meng X, Zhou Z, Lang X, Ning S, Zhang R et al (2022) Regional myocardial work measured by echocardiography for the detection of myocardial ischemic segments: a comparative study with invasive fractional flow reserve. Front Cardiovasc Med 9:813710. https://doi.org/10.3389/fcvm.2022.813710
Toth GG, Johnson NP, Jeremias A, Pellicano M, Vranckx P, Fearon WF, Barbato E, Kern MJ, Pijls NH, De Bruyne B (2016) Standardization of fractional flow reserve measurements. J Am Coll Cardiol 68:742–753. https://doi.org/10.1016/j.jacc.2016.05.067
Tonino PA, De Bruyne B, Pijls NH, Siebert U, Ikeno F, van’ t Veer M, Klauss V, Manoharan G, Engstrøm T, Oldroyd KG et al (2009) Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med 360:213–224. https://doi.org/10.1056/NEJMoa0807611
Mitchell C, Rahko PS, Blauwet LA, Canaday B, Finstuen JA, Foster MC, Horton K, Ogunyankin KO, Palma RA, Velazquez EJ (2019) Guidelines for performing a comprehensive transthoracic echocardiographic examination in adults: recommendations from the American Society of Echocardiography. J Am Soc Echocardiogr 32:1–64. https://doi.org/10.1016/j.echo.2018.06.004
Yadav K, Prajapati J, Singh G, Patel I, Karre A, Bansal PK, Garhwal V (2022) The correlation between speckle-tracking echocardiography and coronary angiography in suspected coronary artery disease with normal left ventricular function. J Cardiovasc Thorac Res 14:234–239. https://doi.org/10.34172/jcvtr.2022.30520
Olsen FJ, Skaarup KG, Lassen MCH, Johansen ND, Sengeløv M, Jensen GB, Schnohr P, Marott JL, Søgaard P, Gislason G et al (2022) Normal values for myocardial work indices derived from pressure-strain loop analyses: from the CCHS. Circ Cardiovasc Imaging 15:e013712. https://doi.org/10.1161/circimaging.121.013712
Taconne M, Le Rolle V, Panis V, Hubert A, Auffret V, Galli E, Hernandez A, Donal E (2022) How myocardial work could be relevant in patients with an aortic valve stenosis? Eur Heart J Cardiovasc Imaging 24:119–129. https://doi.org/10.1093/ehjci/jeac046
Sahiti F, Morbach C, Henneges C, Stefenelli U, Scholz N, Cejka V, Albert J, Heuschmann PU, Ertl G, Frantz S et al (2021) Dynamics of left ventricular myocardial work in patients hospitalized for acute heart failure. J Card Fail 27:1393–1403. https://doi.org/10.1016/j.cardfail.2021.07.004
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28:1–39e14. https://doi.org/10.1016/j.echo.2014.10.003
Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, Byrne RA, Collet JP, Falk V, Head SJ et al (2019) 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J 40:87–165. https://doi.org/10.1093/eurheartj/ehy394
Douglas PS, Pontone G, Hlatky MA, Patel MR, Norgaard BL, Byrne RA, Curzen N, Purcell I, Gutberlet M, Rioufol G et al (2015) Clinical outcomes of fractional flow reserve by computed tomographic angiography-guided diagnostic strategies vs. usual care in patients with suspected coronary artery disease: the prospective longitudinal trial of FFR(CT): outcome and resource impacts study. Eur Heart J 36:3359–3367. https://doi.org/10.1093/eurheartj/ehv444
Barbato E, Toth GG, Johnson NP, Pijls NH, Fearon WF, Tonino PA, Curzen N, Piroth Z, Rioufol G, Jüni P et al (2016) A prospective natural history study of coronary atherosclerosis using fractional flow reserve. J Am Coll Cardiol 68:2247–2255. https://doi.org/10.1016/j.jacc.2016.08.055
Dong M, Li C, Yang G, Gou Q, Zhao Q, Liu Y, Shou X (2022) Diagnostic performance of coronary computed tomography angiography-derived fractional flow reverse in lesion-specific ischemia patients with different Gensini score levels. Ann Transl Med 10:412. https://doi.org/10.21037/atm-22-881
Tao Y, Gao Y, Wu X, Cheng Y, Yan X, Gao Y, Liu Y, Tang Y, Li Z (2022) Diagnostic performance of coronary computed tomography (CT) angiography derived fractional flow reserve (CTFFR) in patients with coronary artery calcification: insights from multi-center experiments in China. Ann Transl Med 10:788. https://doi.org/10.21037/atm-22-3180
Lopes RD, Alexander KP, Stevens SR, Reynolds HR, Stone GW, Piña IL, Rockhold FW, Elghamaz A, Lopez-Sendon JL, Farsky PS et al (2020) Initial invasive versus conservative management of stable ischemic heart disease in patients with a history of heart failure or left ventricular dysfunction: insights from the ISCHEMIA trial. Circulation 142:1725–1735. https://doi.org/10.1161/circulationaha.120.050304
Raja S, Mittal BR, Santhosh S, Bhattacharya A, Rohit MK (2014) Comparison of LVEF assessed by 2D echocardiography, gated blood pool SPECT, 99mTc tetrofosmin gated SPECT, and 18F-FDG gated PET with ERNV in patients with CAD and severe LV dysfunction. Nucl Med Commun 35:1156–1161. https://doi.org/10.1097/mnm.0000000000000182
Liu Y, Song J, Wang W, Zhang K, Qi Y, Yang J, Wen J, Meng X, Gao J, Shao C et al (2022) Association of ejection fraction with mortality and cardiovascular events in patients with coronary artery disease. ESC Heart Fail 9:3461–3468. https://doi.org/10.1002/ehf2.14063
Hsiao JF, Pan KL, Chu CM, Chang ST, Chung CM, Hsu JT (2020) Usefulness of serial post-systolic shortening by speckle tracking echocardiography to predict major adverse cardiovascular events and segmental function improvement after acute myocardial infarction. PLoS ONE 15:e0244589. https://doi.org/10.1371/journal.pone.0244589
Moustafa S, Elrabat K, Swailem F, Galal A (2018) The correlation between speckle tracking echocardiography and coronary artery disease in patients with suspected stable angina pectoris. Indian Heart J 70:379–386. https://doi.org/10.1016/j.ihj.2017.09.220
Liou K, Negishi K, Ho S, Russell EA, Cranney G, Ooi SY (2016) Detection of obstructive coronary artery disease using peak systolic global longitudinal strain derived by two-dimensional speckle-tracking: a systematic review and meta-analysis. J Am Soc Echocardiogr 29:724–735e724. https://doi.org/10.1016/j.echo.2016.03.002
Rumbinaite E, Karuzas A, Verikas D, Jonauskiene I, Gustiene O, Mamedov A, Jankauskiene L, Benetis R, Zaliunas R, Vaskelyte JJ (2022) Value of myocardial deformation parameters for detecting significant coronary artery disease. J Cardiovasc Thorac Res 14:180–190. https://doi.org/10.34172/jcvtr.2022.30
Montgomery DE, Puthumana JJ, Fox JM, Ogunyankin KO (2012) Global longitudinal strain aids the detection of non-obstructive coronary artery disease in the resting echocardiogram. Eur Heart J Cardiovasc Imaging 13:579–587. https://doi.org/10.1093/ejechocard/jer282
Bajracharya P, Acharya KP, Banerjee SK, Ahmed CM, Alam MM, Arzu J, Sheikh N, Osmany D, Ahsan SA (2020) Correlation between myocardial strain by 2-D speckle-tracking echocardiography and angiographic findings by coronary angiogram in stable angina. Maedica (Bucur) 15:365–372. https://doi.org/10.26574/maedica.2020.15.3.365
Edwards NFA, Scalia GM, Shiino K, Sabapathy S, Anderson B, Chamberlain R, Khandheria BK, Chan J (2019) Global myocardial work is superior to global longitudinal strain to predict significant coronary artery disease in patients with normal left ventricular function and wall motion. J Am Soc Echocardiogr 32:947–957. https://doi.org/10.1016/j.echo.2019.02.014
Papadopoulos K, Özden Tok Ö, Mitrousi K, Ikonomidis I (2021) Myocardial work: methodology and clinical applications. Diagnostics (Basel) 11. https://doi.org/10.3390/diagnostics11030573
Lin J, Wu W, Gao L, He J, Zhu Z, Pang K, Wang J, Liu M, Wang H (2022) Global myocardial work combined with treadmill exercise stress to detect significant coronary artery disease. J Am Soc Echocardiogr 35:247–257. https://doi.org/10.1016/j.echo.2021.10.009
Ding J, Sun HG, Liu J, Wu D (2022) Assessment of left ventricular myocardial work done by noninvasive pressure-strain loop technique in patients with essential hypertension. Ann Noninvasive Electrocardiol 27:e12983. https://doi.org/10.1111/anec.12983
Gaudron PD, Liu D, Scholz F, Hu K, Florescu C, Herrmann S, Bijnens B, Ertl G, Störk S, Weidemann F (2016) The septal bulge–an early echocardiographic sign in hypertensive heart disease. J Am Soc Hypertens 10:70–80. https://doi.org/10.1016/j.jash.2015.11.006
Slivnick J, Lampert BC (2019) Hypertension and heart failure. Heart Fail Clin 15:531–541. https://doi.org/10.1016/j.hfc.2019.06.007
Loncaric F, Marciniak M, Nunno L, Mimbrero M, Fernandes JF, Fabijanovic D, Sanchis L, Doltra A, Montserrat S, Cikes M et al (2021) Distribution of myocardial work in arterial hypertension: insights from non-invasive left ventricular pressure-strain relations. Int J Cardiovasc Imaging 37:145–154. https://doi.org/10.1007/s10554-020-01969-4
Huang H, Ruan Q, You Z, Fu L (2023) Segmental and global myocardial work in hypertensive patients with different left ventricular ejection fraction: what’s the role of the apex played? Int J Cardiovasc Imaging 39:1505–1514. https://doi.org/10.1007/s10554-023-02874-2
Truong VT, Vo HQ, Ngo TNM, Mazur J, Nguyen TTH, Pham TTM, Le TK, Phan H, Palmer C, Nagueh SF et al (2022) Normal ranges of global left ventricular myocardial work indices in adults: a meta-analysis. J Am Soc Echocardiogr 35:369–377e368. https://doi.org/10.1016/j.echo.2021.11.010
Funding
Shanghai Science and Technology Commission(202140291); Shanghai Municipal Key Clinical Specialty(shslczdzk03501).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, searching, data collection were performed by YZ, WG, YL, GQ, YZ, HZ, HL, SZ. The datas were analyzed by YG, YJ. ZG, ZG, JL, WH, CP, XS contributed with critical review of the whole work. The first draft of the manuscript was written by YZ and FH and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhao, Y., He, F., Guo, W. et al. The clinical value of noninvasive left ventricular myocardial work in the diagnosis of myocardial ischemia in coronary heart disease: a comparative study with coronary flow reserve fraction. Int J Cardiovasc Imaging (2024). https://doi.org/10.1007/s10554-024-03208-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10554-024-03208-6