Abstract
Right ventricular (RV) free wall longitudinal strain (RVFWLS), and four-chamber longitudinal strain (RV4CLS) using speckle tracking echocardiography have demonstrated increased accuracy and discrimination to measure right ventricular function in different clinical conditions. Reproducibility data of these measures are scarce and mainly tested in small or reference populations. The main objective of this study was to investigate their reproducibility, and of other traditional RV parameters, from unselected participants of a large cohort study. RV strain reproducibility was analyzed using echocardiographic images of 50 participants from a randomly selected sample from The ELSA-Brasil Cohort. Images were acquired and analyzed following the study protocols. The mean RVFWLS was − 26.9 ± 2.6% and the mean RV4CLS was − 24.4 ± 1.9%. The intra-observer reproducibility parameters of RVFWLS demonstrated a coefficient of variation (CV) of 5.1% and an intraclass correlation coefficient (ICC [95%CI] 0.78[0.67—0.89]), and for RV4CLS were CV = 5.1% and ICC = 0.78[0.67—0.89]. Reproducibility for RV fractional area change was CV = 12.1%; ICC = 0.66 [0.50—0.81] and for RV basal diameter was CV = 6.3%; ICC = 0.82 [0.73—0.91]. The inter-observer reproducibility for RVFWLS was CV = 8.3%; ICC 0.54[0.34—0.74] and for RV4CLS, CV = 6.3%; ICC = 0.53[0.34—0.73], following the same pattern among conventional RV parameters. We found adequate reproducibility of RV longitudinal strain parameters. This information is relevant for the long-term follow-up of cohort participants and reinforces the utility of RV longitudinal strain as a tool to monitor subclinical changes in RV systolic function.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Assessment of right ventricular (RV) function is important to the management of patients with heart failure [1], pulmonary hypertension [2], and congenital heart diseases [3]. Traditional RV systolic parameters such as tricuspid lateral annular peak systolic velocity by pulsed tissue Doppler imaging (s') and tricuspid annular plane systolic excursion (TAPSE) remain the recommended measures to estimate RV systolic function [4]. However, these parameters have limitations such as angle and load dependence and inaccuracy in evaluating a global RV systolic function since they represent only the function of the basal segment [4].
Two-dimensional speckle tracking echocardiography (2DSTE) is an increasingly used technique to quantify RV global and regional myocardial function. RV longitudinal strain measurement has been demonstrated to increase the diagnostic accuracy of multiple heart conditions, such as pulmonary hypertension [5], pulmonary embolism [6], arrhythmogenic right ventricular dysplasia [7], and to further stratify the prognosis in patients with heart failure [8], acute coronary syndromes [9] and heart transplantation [10].
Previous studies evaluating the RV longitudinal strain reproducibility are scarce and were done in small or reference populations [11]. Consequently, data regarding RV longitudinal strain reproducibility in community scenarios and cohort populations are limited. Therefore, the main objective of this study was to investigate the inter- and intra-observer reproducibility of 2DSTE right ventricular longitudinal strain parameters and other traditional RV parameters from The ELSA-Brasil study participants.
Methods
Study population
The ELSA-Brasil study is a cohort study of 15,105 civil servants (men and women aged 35–75 years old) in Brazil aiming to investigate the incidence, progression, and determinants of diabetes and cardiovascular diseases, and was detailed elsewhere [12, 13]. The study protocol was approved by each institutional review board and written informed consent was obtained from all participants.
Echocardiography was performed at the study baseline (between 2008 and 2010), and 2DSTE parameters were measured in a predefined random subsample comprising 10% of the entire cohort. Exclusion criteria were inadequate echocardiography images and cardiac arrhythmias in acquired images. Fifty participants were selected from the random sample for the right ventricular global longitudinal strain reading and analysis, similar sample size to our previously published left ventricular strain reproducibility [14].
Two-Dimensional echocardiography
Transthoracic echocardiography images were acquired by trained echocardiographers following study protocols according to the North American and European Societies of Cardiology guidelines [15, 16]. All studies were performed in identical equipment (Aplio XG; Toshiba Corporation, Tokyo, Japan), using a 2.5 MHz sectorial transducer, and the frame rate for the acquisition ranged from 40 to 60 frames per second. Cine loops and static images of 3 cardiac cycles were selected in each acoustic window for posterior central reading. Cine loops and static images of 3 cardiac cycles were selected in each acoustic window for posterior central reading.
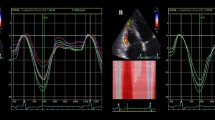
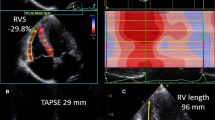
In the reading center, all studies were blindly read for clinical parameters in a dedicated workstation (ComPACS Review Station 10.5, Medimatic Solutions Srl, Italy) according to a prespecified protocol [17]. RV basal diameter was obtained from the apical four-chamber view and calculated as a mean of 3 consecutive heart cycles (Fig. 1A). RV fractional area change (FAC) was obtained from the apical four-chamber view and calculated as the difference in the end-diastolic area and the end-systolic area divided by the end-diastolic area (Fig. 1B).
Examples of right ventricular measurements: A RV basal diameter; B RV endocardial border tracing at end-diastole and end-systole to calculate the fractional area change (FAC); C observer 1 RV strain; D observer 2 RV strain. The colored lines represent strain curves of each of the six segments of the right ventricle
RV longitudinal strain
The quantitative evaluation of right ventricular global longitudinal strain followed current guidelines and recommendations [18, 19], using a previously validated and commercially available software dedicated to RV analysis (2 D Cardiac Performance Analysis©, TomTec-ArenaTM 1.2 Imaging Systems, Unterschleißheim, Germany) [20].
For deformation analysis, the software tracks speckles along the endocardial border and myocardium throughout the cardiac cycle, and unacceptable image quality was defined as a lack of a full cardiac cycle or when two or more segments could not be properly tracked. The RV strain could be obtained in all subjects of this subsample. End-diastole was manually defined as the peak of the R-wave from the QRS electrocardiogram tracing, whereas end-systole was defined as a tricuspid valve opening from the four-chamber view. The RV free wall and interventricular septum are both divided into three segments (apical, mid, and basal). RV free wall longitudinal strain (RVFWLS) is the average value from three RV free wall segments and four-chamber longitudinal strain (RV4CLS) is a measurement obtained from the average of the values from all six segments, including septal segments, and the dedicated software calculated both final values (Fig. 1C).
The strain analysis had a mean duration of 10–15 min per participant and was made by two investigators with different grades of training in RV strain measurements: investigator 1 (EGP), an echocardiographer with 500 analyses performed, and investigator 2 (GBS), echocardiographer on training with 100 analyses performed. To assess intra-observer reproducibility, each investigator repeated the analysis on the same set of images after 2 months, blinded to the first reading.
Statistical analysis
Data are presented as mean ± standard deviation (SD). For reproducibility, intra-observer and inter-observer coefficients of variation (CV) were calculated as the ratio of SD to mean, expressed in percentage. Intraclass correlation coefficient (ICC) and 95% confidence intervals (95% CI) were calculated using a two-way mixed model. [21]. Bland & Altman graphics were plotted to demonstrate the inter-observer rate of agreement and to assess the relationship between the observer’s measurements. All statistical analyses were performed using Stata® (version 13.0).
Results
The mean age of the study sample’s participants was 51.3 ± 9.7 years and 57% were female. The mean heart rate was 65 ± 6 beats per minute. Other clinical and demographic characteristics of study participants in The Brazilian Longitudinal Study of Adult Health (ELSA-Brasil) were described previously [14].
Intra- and inter-observer reproducibility
The intra-observer reproducibility of the RV global longitudinal strain was similar for free wall and four chamber analysis (Table 1). Considering RVFWLS, observer 1 had an excellent CV (6.6%) and intra-observer agreement (ICC [95%CI]: 0.77[0.65—0.86]). Considering RV4CLS, observer 1 had, also, an excellent CV (5.1%) and intra-observer agreement (ICC: 0.78 [0.67–0.89]).
Table 2 shows inter-observer reproducibility for RVFWLS and RV4CLS. Both longitudinal strain parameters had a fair inter-observer agreement (RVFWLS ICC: 0.54 [0.34–0.74]), (RV4CLS ICC: 0.53 [0.34–0.73]), and CV of 8.3% and 6.3%, respectively. An inter-observer Bland & Altman analysis shows a mean difference of 0.17 ± 1.55 for RVFWLS (Fig. 2A) and 0.54 ± 2.2 for RV4CLS (Fig. 2B).
Bland & Altman plot of inter-observer for RVFWLS (A) and RV4CLS (B). The red solid lines indicate the mean difference, and the green solid lines indicate the 95% limits of agreement (LOA). RVFWLS right ventricular free wall longitudinal strain, RV4CLS right ventricular four chamber longitudinal strain
The reproducibility of more common RV parameters demonstrated that FAC had worse intra-observer (ICC: 0.66 [0.50–0.81], CV: 12.1%) and inter-observer agreement (ICC: 0.22 [0–0.51], CV: 17.6%) (Tables 1 and 2), while RV basal diameter had an excellent intra-observer agreement (ICC: 0.82 [0.73–0.91], CV: 6.3%).
Comparison of the first 25 readings to the last 25 in the less experienced observer demonstrated improved intra-observer agreement in the last measurements for RVFWLS (ICC: 0.28 [0–0.64], vs. 0.55 [0.27–0.82]; CV: 14.5% vs 10.4%) and RV4CLS (ICC: 0.2 [0–0.58] vs. 0.56 [0.29–0.83]; CV: 12.5% vs. 6.5%) (Table 3).
Discussion
In this sample from a multicentric Brazilian free-dwelling middle-aged individuals, there was adequate reproducibility and level of agreement in right ventricular longitudinal strain measurements. The more traditional FAC appeared to show worse reproducibility while RV basal diameter, a dimension parameter, had excellent intra-observer reproducibility.
In a previous study, Mirea et al. prospectively selected 200 subjects who underwent echocardiography examination, and they found excellent intra-observer agreement in RVFWLS and RV4CLS (ICC > 0.75) with the worse inter-observer agreement [11], similar to our study. Another study that included 35 subjects (5 healthy controls and 30 subjects with pulmonary hypertension), found an inter-reader RV4CLS CV of 9.6% and intra-reader CV of 8.5% [22], and this degree of variability was consistent with our sample, using a not selected sample based on a disease condition and in a clinical research context. RV longitudinal strain by cardiovascular magnetic resonance feature tracking also demonstrated excellent reproducibility [23]. However, Erley et al. studied the agreement in RV longitudinal strain measurement between cardiovascular magnetic resonance (CMR) and echocardiography, and found only moderate inter-modality agreement, concluding that different modalities and techniques should not be used interchangeably to determine and monitor RV strain. [24]
Regarding traditional RV function parameters, Ruotsalainen et al. analyzed FAC in 51 hypoplastic left heart syndrome children and found an inter-observer ICC of 0.774 [0.427–0.922] and an intra-observer ICC of 0.205 [0.498—0.269], similarly to our numbers [25]. In addition, Genovese et al. compared RV size and function parameters obtained from RV-focused and apical four-chamber views, and the test–retest variability between these two views in 50 patients undergoing clinically indicated transthoracic echocardiography. Their intra-operator RV basal diameter test-rest had an excellent agreement (ICC: 0.92 [0.87–0.96]), comparable to our study. In contrast, they found better intra-operator agreement than our study for FAC (ICC: 0.89 [0.81–0.93]), RVFWLS (ICC: 0.97 [0.94–0.98]), and RV4CLS (ICC: 0.90 [0.84–0.94]) [26]. These discrepancies could be explained by better image quality obtained in RV-focused views, allowing better visualization of endocardial borders to calculate FAC and longitudinal strain. Furthermore, Srinivasan et al. evaluated the correlation of 2D echocardiographic assessment of RV size and function with CMR imaging in 23 patients with repaired Tetralogy of Fallot and 13 controls. In contrast to the left ventricle, 2D echocardiographic indices of RV size and function did not correlate with CMR data and qualitative assessment of the RV showed poor interobserver agreement. [27] The lack of accuracy in assessing RV function by 2D echocardiography is likely due to the complex geometry of the RV and dynamic volumetric measures as those derived from 3D echocardiographic images [28] or cardiac resonance, which has been considered the gold standard, may be more accurate and reliable, however, these modalities require more advanced and less available resources, which limits its wider use in most conditions. Nevertheless, RV strain 2D-parameters had been shown a better correlation with RV ejection fraction using magnetic resonance imaging than conventional RV measures [29] and seemed to detect subtle RV longitudinal systolic abnormalities despite preserved RV conventional measurements [30].
Additionally, we observed an improvement in RV intra-observer reproducibility in the last exams compared to the first exams analyzed by the less experienced observer, suggesting a quick learning curve for this method, reinforcing its potential utility in less specialized scenarios. Chamberlain et al. demonstrated that a minimum of 100 studies was required to achieve an expert level of competency (intraclass correlation coefficient > 0.90) among all novice observers, whereas left ventricular longitudinal strain required only 50 studies to achieve level III competency [31]. Possible explanations for these findings include difficulty to visualize the true RV apex because of foreshortening during image acquisition, increased prevalence of apical trabeculation and moderator bands, and the placement of the markers too close to the tricuspid annulus which can also affect strain analysis results.
Some limitations of RV strain 2D analyses should be considered. RV echocardiographic strain is influenced by image quality, reverberation, and artifacts and the thin RV free wall may make it difficult to limit the myocardium. The global analyses of RV function are from a single view (4-chamber) and may not represent a global assessment of RV function.
Conclusion
This study showed that measurements of right ventricular global longitudinal strain by speckle tracking echocardiography are reproducible in a clinical research context. This information is crucial for the long-term follow-up of cohort participants and reinforces the utility of RV longitudinal strain as a tool to monitor subclinical changes in RV systolic function.
References
Meyer P, Filippatos GS, Ahmed MI, Iskandrian AE, Bittner V, Perry GJ, White M, Aban IB, Mujib M, Dell’Italia LJ, Ahmed A (2010) Effects of right ventricular ejection fraction on outcomes in chronic systolic heart failure. Circulation 121(2):252–258
Van de Veerdonk MC, Kind T, Marcus JT, Mauritz GJ, Heymans MW, Bogaard HJ, Boonstra A, Marques KM, Westerhof N, Vonk-Noordegraaf A (2011) Progressive right ventricular dysfunction in patients with pulmonary arterial hypertension responding to therapy. J Am Coll Cardiol 58(24):2511–2519
Gatzoulis MA, Balaji S, Webber SA, Siu SC, Hokanson JS, Poile C, Rosenthal M, Nakazawa M, Moller JH, Gillette PC, Webb GD (2000) Risk factors for arrhythmia and sudden cardiac death late after repair of tetralogy of Fallot: a multicentre study. The Lancet 356(9234):975–981
Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, Solomon SD, Louie EK, Schiller NB (2010) Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography: endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr 23(7):685–713
Hekimsoy V, Kaya EB, Akdogan A, Sahiner L, Evranos B, Canpolat U, Aytemir K, Özer N, Tokgozoglu L (2018) Echocardiographic assessment of regional right ventricular systolic function using two-dimensional strain echocardiography and evaluation of the predictive ability of longitudinal 2D-strain imaging for pulmonary arterial hypertension in systemic sclerosis patients. Int J Cardiovasc Imaging 34(6):883–892
Wright L, Dwyer N, Power J, Kritharides L, Celermajer D, Marwick TH (2016) Right ventricular systolic function responses to acute and chronic pulmonary hypertension: assessment with myocardial deformation. J Am Soc Echocardiogr 29(3):259–266
Prakasa KR, Wang J, Tandri H, Dalal D, Bomma C, Chojnowski R, James C, Tichnell C, Russell S, Judge D, Corretti M (2007) Utility of tissue Doppler and strain echocardiography in arrhythmogenic right ventricular dysplasia/cardiomyopathy. Am J Cardiol 100(3):507–512
Carluccio E, Biagioli P, Alunni G, Murrone A, Zuchi C, Coiro S, Riccini C, Mengoni A, D’Antonio A, Ambrosio G (2018) Prognostic value of right ventricular dysfunction in heart failure with reduced ejection fraction: superiority of longitudinal strain over tricuspid annular plane systolic excursion. Circ Cardiovasc Imaging 11(1):e006894
Kanar BG, Tigen MK, Sunbul M, Cincin A, Atas H, Kepez A, Ozben B (2018) The impact of right ventricular function assessed by 2-dimensional speckle tracking echocardiography on early mortality in patients with inferior myocardial infarction. Clin Cardiol 41(3):413–418
Barakat AF, Sperry BW, Starling RC, Mentias A, Popovic ZB, Griffin BP, Desai MY (2017) Prognostic utility of right ventricular free wall strain in low risk patients after orthotopic heart transplantation. Am J Cardiol 119(11):1890–1896
Mirea O, Berceanu M, Donoiu I, Militaru C, Săftoiu A, Istrătoaie O (2019) Variability of right ventricular global and segmental longitudinal strain measurements. Echocardiography 36(1):102–109
Aquino EM, Barreto SM, Bensenor IM, Carvalho MS, Chor D, Duncan BB, Lotufo PA, Mill JG, Molina MD, Mota EL, Azeredo Passos VM (2012) Brazilian longitudinal study of adult health (ELSA-Brasil): objectives and design. Am J Epidemiol 175(4):315–324
Schmidt MI, Duncan BB, Mill JG, Lotufo PA, Chor D, Barreto SM, Aquino EM, Passos VM, Matos SM, Molina MD, Carvalho MS (2015) Cohort profile: longitudinal study of adult health (ELSA-Brasil). Int J Epidemiol 44(1):68–75
Cañon-Montañez W, Santos A, do Amaral MV, Nunes LA, Duncan BB, Schmidt MI, Foppa M (2017) Reproducibility of left ventricular global longitudinal strain using two-dimensional ultrasound speckle tracking: Longitudinal Study of Adult Health (ELSA-Brasil). Revista Colombiana de Cardiología 24(6):559–566
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise J, Solomon S (2006) Recommendations for chamber quantification. Eur J Echocardiogr 7(2):79–108
Negishi K, Negishi T, Kurosawa K, Hristova K, Popescu BA, Vinereanu D, Yuda S, Marwick TH (2015) Practical guidance in echocardiographic assessment of global longitudinal strain. JACC Cardiovasc Imaging. 8(4):489–92
Mill JG, Pinto K, Griep RH, Goulart A, Foppa M, Lotufo PA, Maestri MK, Ribeiro AL, Andreão RV, Dantas EM, Oliveira I (2013) Aferições e exames clínicos realizados nos participantes do ELSA-Brasil. Rev Saude Publica 47:54–62
Muraru D, Haugaa K, Donal E, Stankovic I, Voigt JU, Petersen SE, Popescu BA, Marwick T (2022) Right ventricular longitudinal strain in the clinical routine: a state-of-the-art review. Eur Heart J-Cardiovasc Imaging 23(7):898–912
Badano LP, Kolias TJ, Muraru D, Abraham TP, Aurigemma G, Edvardsen T, D’Hooge J, Donal E, Fraser AG, Marwick T, Mertens L (2018) Standardization of left atrial, right ventricular, and right atrial deformation imaging using two-dimensional speckle tracking echocardiography: a consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. Eur Heart J-Cardiovasc Imaging 19(6):591–600
Muraru D, Spadotto V, Cecchetto A, Romeo G, Aruta P, Ermacora D, Jenei C, Cucchini U, Iliceto S, Badano LP (2015) New speckle-tracking algorithm for right ventricular volume analysis from three-dimensional echocardiographic data sets: validation with cardiac magnetic resonance and comparison with the previous analysis tool. Eur J Echocardiogr 17(11):1279–1289
Cicchetti DV (1994) Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess 6(4):284
Il’Giovine ZJ, Mulder H, Chiswell K, Arges K, Tomfohr J, Hashmi A, Velazquez EJ, Kisslo JA, Samad Z, Rajagopal S (2018) Right ventricular longitudinal strain reproducibility using vendor-dependent and vendor-independent software. J Am Soc Echocardiogr 31(6):721–32
Schmidt B, Dick A, Treutlein M, Schiller P, Bunck AC, Maintz D, Baeßler B (2017) Intra-and inter-observer reproducibility of global and regional magnetic resonance feature tracking derived strain parameters of the left and right ventricle. Eur J Radiol 1(89):97–105
Erley J, Tanacli R, Genovese D, Tapaskar N, Rashedi N, Bucius P, Kawaji K, Karagodin I, Lang RM, Kelle S, Mor-Avi V (2020) Myocardial strain analysis of the right ventricle: comparison of different cardiovascular magnetic resonance and echocardiographic techniques. J Cardiovasc Magn Reson 22(1):1–2
Ruotsalainen HK, Bellsham-Revell HR, Bell AJ, Pihkala JI, Ojala TH, Simpson JM (2017) Right ventricular systolic function in hypoplastic left heart syndrome: a comparison of manual and automated software to measure fractional area change. Echocardiography 34(4):587–593
Genovese D, Mor-Avi V, Palermo C, Muraru D, Volpato V, Kruse E, Yamat M, Aruta P, Addetia K, Badano LP, Lang RM (2019) Comparison between four-chamber and right ventricular–focused views for the quantitative evaluation of right ventricular size and function. J Am Soc Echocardiogr 32(4):484–494
Srinivasan C, Sachdeva R, Morrow WR, Greenberg SB, Vyas HV (2011) Limitations of standard echocardiographic methods for quantification of right ventricular size and function in children and young adults. J Ultrasound Med 30(4):487–493
Vitarelli A, Mangieri E, Terzano C, Gaudio C, Salsano F, Rosato E, Capotosto L, D’Orazio S, Azzano A, Truscelli G, Cocco N (2015) Three-dimensional echocardiography and 2D–3D speckle-tracking imaging in chronic pulmonary hypertension: diagnostic accuracy in detecting hemodynamic signs of right ventricular (RV) failure. J Am Heart Assoc 4(3):e001584
Park JH, Negishi K, Kwon DH, Popovic ZB, Grimm RA, Marwick TH (2014) Validation of global longitudinal strain and strain rate as reliable markers of right ventricular dysfunction: comparison with cardiac magnetic resonance and outcome. J Cardiovasc Ultrasound 22(3):113–120
Morris DA, Krisper M, Nakatani S, Köhncke C, Otsuji Y, Belyavskiy E, Radha Krishnan AK, Kropf M, Osmanoglou E, Boldt LH, Blaschke F (2017) Normal range and usefulness of right ventricular systolic strain to detect subtle right ventricular systolic abnormalities in patients with heart failure: a multicentre study. Eur Heart J-Cardiovasc Imaging 18(2):212–223
Chamberlain R, Scalia GM, Wee Y, Hlaing S, Lee A, Hotham I, Page-Taylor E, Sabapathy S, Chan J (2020) The learning curve for competency in right ventricular longitudinal strain analysis. J Am Soc Echocardiogr 33(4):512–514
Funding
This work was supported by the Brazilian Ministry of Health (Science and Technology Department), the Brazilian Ministry of Science, Technology and Innovation (Financiadora de Estudos e Projetos-grants 01 06 0010.00, 01 10 0643.00 RS, 01 06 0212.00 BA, 01 06 0300.00 ES, 01 06 0278.00 MG, 01 06 0115.00 SP, 01 06 0071.00 RJ), CNPq (the Brazilian National Council for Scientific and Technological Development).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Data collection was performed by EGP and GBS. Material preparation and data analysis were performed by EGP. The first draft of the manuscript was written by EGP and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Because it is a multicenter study, ELSA-Brasil’s research protocol was approved not only by the ethics committee of each institution but also by the National Research Ethics Committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pianca, E.G., Schmitz, G.B., Duncan, B.B. et al. Reproducibility of right ventricular function by longitudinal strain and other echocardiographic parameters in the ELSA-Brasil study. Int J Cardiovasc Imaging 39, 1865–1870 (2023). https://doi.org/10.1007/s10554-023-02899-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-023-02899-7