Abstract
Patients with rheumatoid arthritis (RA) are at higher risk for having underdiagnosed heart failure, however there are no recommendations regarding echocardiographic screening. We aimed to determine the prevalence of subclinical ventricular dysfunction in RA applying current echocardiographic guidelines, its association with patients’ characteristics, biomarkers and prognostic parameters and compare the 2016 guidelines to the recommendations from 2009. Prospective study of RA patients without known heart disease, categorized as preserved ventricular function (PVF), systolic dysfunction (SD), isolated diastolic dysfunction (DD) or indeterminate diastolic function (IDF) as per the 2016 echocardiography guidelines—or any ventricular dysfunction (AVD) comprehending the last 3. The median age was 58 years and 78% were females. The majority had PVF (73%), followed by DD (13%), IDF (11%) and SD (4%). Concordance with the 2009 echocardiographic guidelines was low. Compared with PVF, AVD patients were older (65 vs 55 years, p < 0.001), had a higher prevalence of hypertension and dyslipidaemia (56% vs 38%, p = 0.003 and 60% vs 41%, p = 0.002, respectively). In multivariable analysis, age (particularly > 57 years) was the only independent predictor of AVD or DD. AVD was significantly associated with higher NT-proBNP and lower distance in 6-min walk test. There were no significant independent associations between characteristics of RA disease and ventricular function. A total of 17% of RA patients without known cardiovascular disease presented subclinical systolic or diastolic dysfunction, which was associated with older age. The echocardiographic screening may have clinical value in identifying subclinical ventricular dysfunction, especially in older RA patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rheumatoid arthritis (RA) is a chronic inflammatory disease, involving autoimmune mechanisms, characterized by a symmetric peripheral polyarthritis; however, extra-articular involvement can occur. RA has been associated with heart disease, the pericardium being frequently affected, while coronary artery disease (CAD) and heart failure (HF) (both ischemic and non-ischemic) are also more common than in the general population [1, 2].
Aiming to better predict the cardiovascular (CV) risk in RA patients, the European League Against Rheumatism (EULAR) suggested applying a 1.5 multiplication factor to algorithms conceived for the general population [3] since patients with RA seem to have a two-fold higher incidence of HF and an increased mortality risk [4, 5]. Although HF with reduced ejection fraction is not particularly frequent, diastolic impairment and left ventricular hypertrophy seem to be more common in RA [6, 7]. Underlying HF aetiologies include atherosclerotic CAD, dilated cardiomyopathy, myocarditis and vasculitis. The role of anti-inflammatory therapies or disease-modifying anti-rheumatic drugs (DMARDs) in heart disease remains unclear [8].
Patients with RA present some specificities and the discrimination of their symptoms is often difficult because symptoms may be non-specific or conditioned by articular limitations [9]. HF may be underdiagnosed in RA patients and there are no available recommendations for HF screening specific for patients with RA. Subclinical ventricular dysfunction can be quickly identified by echocardiography, while surrogate biomarkers can be easily studied. Other studies have already suggested the prognostic utility of N-terminal prohormone of brain natriuretic peptide (NT-proBNP), C-reactive protein (CRP) and rheumatoid factor (RF), but the value of anti-cyclic citrullinated peptide (anti-CCP) antibodies, erythrocyte sedimentation rate and troponin is still more uncertain [10, 11].
An earlier diagnosis could improve treatment decisions and consequently prognosis. The non-invasive diagnosis of diastolic dysfunction—which can be linked to HF with preserved ejection fraction [12]—is particularly challenging. A change in echocardiographic guidelines in 2016 reformulated the previous algorithm, with the expectation of a better performance in clinical practice [13, 14]. Prior studies have not focused on subclinical disease following the 2016 guidelines, with a rigorous state-of-the-art homogeneous echocardiographic analysis (most used the 2009 guidelines, or only one or two parameters and did not the complete echocardiographic algorithm).
In the present study, we assess a relatively large sample of RA patients, adjust for covariates that were systematically investigated, and complement our analysis with biomarker evaluation. Our main objectives were: (1) to assess the prevalence and characterize the type of cardiac dysfunction in RA patients without known heart disease; (2) compare the characteristics of patients with RA according to their ventricular function classification, aiming to identify the predictors of ventricular dysfunction (and the patients that would benefit the most from the screening); and (3) validate the value of the identification of subclinical ventricular dysfunction by analysing associations with surrogate prognostic markers. The secondary objectives were to determine the prevalence of a possible precursor stage of HF with preserved ejection fraction (HFpEF), using a combination of echocardiographic findings and biomarkers, and compare diastolic dysfunction definitions using the actual 2016 echocardiographic guidelines [14] and the previous guidelines from 2009 [13].
Methods
Study design and ethics
This is a prospective study that enrolled patients followed in the outpatient clinic of Autoimmune Disorders at Centro Hospitalar Universitário do Porto, previously diagnosed with RA, between June 2016 and June 2018. Follow-up was updated in August 2019. The protocol for this study was a priori registered at ClinicalTrials.gov under the number NCT03960515.
This study was approved by the Hospital’s Ethics Committee and was conducted in accordance to the principles of the 1975 Declaration of Helsinki. All participants provided written informed consent before enrollment in the study.
Patient selection
The diagnosis of RA was made according to 2010 ACR/EULAR Classification Criteria [15]. Patients with an active neoplasm or severe comorbidity, an expected survival of less than 6 months, dementia, inability to walk or totally dependent in their daily life activities were excluded. For the present analysis, patients with previously known heart disease (HF, CAD, previous percutaneous or surgical coronary revascularization, previous cardiac surgery, at least moderate valve disease, or atrial fibrillation at the time of the echocardiogram) or those that did not perform an echocardiogram were also excluded.
Patients were divided into four categories of ventricular function, according to transthoracic echocardiogram (TTE) results: preserved ventricular function (PVF); systolic (± diastolic) dysfunction (SD); (isolated) diastolic dysfunction (DD); indeterminate diastolic function (IDF). The definition of groups was made according the 2016 European Heart Failure guidelines [12], 2016 guidelines for diastolic evaluation [14] and the 2009 recommendations of the American Society of Echocardiography [13], as depicted in Fig. 1. If half (or more) of the variables needed for each classification were missing, the diastolic classification was registered as missing. In the main analyses, the diastolic function categorization followed the 2016 guidelines. We grouped patients with IDF, DD or SD, as per the 2016 guidelines, into one category of “any ventricular dysfunction” (AVD), that was compared to PVF.
Simplified 2009 and 2016 echocardiographic guidelines for ventricular function classification. DD diastolic dysfunction, IDF indeterminate diastolic function, NVF normal ventricular function, SD systolic dysfunction. Using 2016 guidelines, if a patient had only 3 parameters available and 2 or 3 were abnormal, he/she was categorized as having DD, if 2 were normal, as having normal diastolic function. If only 2 or less variables were available, diastolic classification was recorded as missing. Using 2009 guidelines, it was mandatory that a patient had at least one e′ value and indexed LA volume; if one of those variables was missing, diastolic classification was recorded as missing
Using the 2016 HF European guidelines [12], we also analysed a category of potential subclinical heart failure with preserved ejection fraction (“HFpEF risk”), with the following characteristics: LVEF ≥ 50% and NT-proBNP > 125 pg/mL and structural echocardiographic changes (left ventricular hypertrophy or indexed LA volume or diastolic dysfunction as per 2016 echocardiographic guidelines). We use the term “risk” because the presence of signs or symptoms of HF was not necessary.
Our sample of RA patients was compared with a cohort of the general population (from the EPIPorto study [16], n = 1000) that has similar demographic characteristics and risk factors (except for the presence of RA), which was also evaluated using the 2016 European/American guidelines.
Data collection and variables
Clinical data
Biometric and clinical data was collected and included age, gender, body mass index (BMI), comorbidities, year of diagnosis of RA, Disease Activity Score 28 (DAS28) assessment—that measures disease activity by counting the number of tender or swollen joints [17], combined with the value of erythrocyte sedimentation rate (ESR)—and medication (all the medication used for RA and cardiovascular medication).
Transthoracic echocardiogram (TTE)
Echocardiographic evaluation was analysed by one cardiologist, that was blinded to the clinical information or the results of any other exams, using Philips® iE33 ultrasound machine. To certify the external validity of the echocardiographic measurements, a random sample of 25 anonymized exams was evaluated at the Institut Lorrain du Coeur et des Vaisseaux Louis Mathieu at Nancy, France, showing good correlation of the measurements (intra-class correlation coefficient > 0.75 for variables that are used in diastolic evaluation).
The evaluated parameters included the dimensions of the cardiac chambers (left atrial and end-diastolic ventricular volumes calculated using Simpson’s rule and indexed to body surface area), left ventricular wall thickness and mass, left ventricular ejection fraction (using modified Simpson’s biplane method), valvular disease, pericardial disease and diastolic function as per the 2016 American and European guidelines [14]. The Chamber Quantification European guidelines [18] were followed for all cardiac chambers analyses.
We assessed the relationship between echocardiographic categories and surrogate prognostic markers (biomarkers, physical exercise capacity and cardiovascular events) because the echocardiographic identification of ventricular dysfunction is more relevant if it is associated with prognosis.
Biomarkers
We analysed several biomarkers in the hospital lab that included the NT-proBNP, high-sensitivity troponin T (hsTnT), CRP and erythrocyte sedimentation rate (ESR). We also checked if patients tested positive for anti-CCP antibodies or rheumatoid factor (RF) and their estimated glomerular filtration rate (eGFR).
Physical exercise capacity
Patients performed a 6-min walk test (6MWT) as recommended by the American Thoracic Society [19].
Statistical analyses
Statistical analyses were conducted using the STATA version 13 and SPSS ® version 23 software. A two-sided p-value of < 0.05 was used as statistical significance for all statistical tests. Continuous data were described as mean ± standard deviation for gaussian distribuition or median (IQR—interquartile range between the 25th and 75th quartiles) for non-gaussian distributions. The Shapiro–Wilk test was used to test the normality of distribution. Categorical data were presented as absolute frequencies (n) and percentages (%). We analysed the relationship between two categories of ventricular function and patients’ characteristics using independent-samples t test or Mann–Whitney U test for continuous variables, and Chi-squared or Fisher exact test for categorical variables, as appropriate. The four groups of LV function were compared using ANOVA, Kruskal–Wallis tests or multinomial logistic regression.
Linear regression was used to analyse the associations between continuous variables. Multivariable logistic regression, using categories of ventricular function as dependent variable (taking PVF as reference) was performed to estimate independent predictors of ventricular function (covariates with a significant association in the univariable analysis were used in the model), obtaining odds ratio (OR) and the respective 95% confidence intervals (CI). Hosmer–Lemeshow test was used to determine goodness of fit of model and area under the Receiver Operating Characteristic curve (AUC ROC) to determine its discriminative power. Logistic regression was also used to compare the prevalence of diastolic dysfunction in our sample with a cohort from the general population (EPIPorto study [16]).
We computed the Cohen’s Kappa coefficient (κ) to test the concordance between 2009 and 2016 classifications of diastolic function.
Results
Baseline characteristics
We included a total of 319 RA patients without known heart disease (Fig. 2). The median age was 58 years (IQR 19) and 78% (n = 249) were females. Patients’ characteristics are presented in Table 1.
Patients with any ventricular dysfunction (AVD)
Eighty-seven patients (27%) had AVD (Table 1). These patients were older, presented more frequently hypertension, dyslipidaemia, used corticosteroids more often, reported a lower dosage of cardiovascular medications (ACEi or ARB and statin), had increased NT-proBNP and lower eGFR concentrations, and showed poorer physical performance in the 6MWT test. In the multivariable analysis (model adjusted for age, hypertension, dyslipidaemia, corticosteroids and eGFR), age was the only independent predictor of AVD (OR 1.079; 95% CI, 1.045 to 1.114). The AUC ROC was 0.71 (95% CI, 0.65 to 0.77) with the best cut-off point (best sum of sensitivity and specificity) of 57 years old (sensitivity of 78% and specificity of 58%).
Comparison between categories of ventricular function (using 2016 echocardiographic guidelines)
Systolic dysfunction was found in 4% (n = 13), being mild (LVEF between 40 and 50%) in 11 patients and moderate (LVEF between 40 and 30%) in 2 patients.
Patients with LVEF ≥ 50%, were classified according to the 2016 guidelines. An example of a patient with diastolic dysfunction is presented in Fig. 3.
Example of a patient with diastolic dysfunction, as per the 2016 echocardiographic classification. a Apical 2-chamber view used for estimation of left atrial volume (which is complemented by an identical measurement in 4-chamber view). b Mitral inflow pattern in 4-chamber view, with measurement of E and A wave maximal velocities (marked in green E wave velocity = 88 cm/s; marked in blue A wave velocity = 87 cm/s; E/A ratio = 1). c Tissue Doppler recording, used to measure septal mitral annular e′ velocity (marked in blue). d Estimation of maximal tricuspid regurgitation systolic jet velocity using CW Doppler (suboptimal envelope in this case). This patient had preserved ejection fraction and all the parameters for having diastolic dysfunction: a left atrial volume of 44 mL/m2, septal e′ of 5.5 cm/s, lateral e′ of 6.3 cm/s; septal E/e′ of 16, lateral E/e′ of 14 (and average E/e′ of 15) and tricuspid regurgitation velocity of approximately 2.83 m/s
Isolated DD was documented in 40 patients (13%) and 34 patients (11%) had IDF. Tricuspid regurgitation (TR) velocity could be adequately determined in only 151 patients (47%).
Age, hypertension and dyslipidaemia were expressed significantly different amongst categories of ventricular function (Table 2). The RA variables, which included the RA duration, anti-CCP/RF positivity, DAS28-ESR, ESR and RA medication were not associated with TTE results, however corticosteroids were more frequently used in patients with DD and CRP was higher in SD, as compared to reference category (preserved ventricular function). In the multivariable analysis (adjusted for age, hypertension, dyslipidaemia, corticosteroids and CRP), age was the only independent factor associated with categories of ventricular function, with an OR for DD (PVF as reference) of 1.097 (95% CI 1.055 to 1.141; p < 0.001).
Comparing DD category to PVF, there were significant differences in age (66.5 (IQR 12) vs 54.5 (IQR 19); OR 5.826; 95% CI 3.704 to 7.048; p < 0.001), dyslipidaemia (65% vs 41%; OR 1.645; 95% CI 1.158 to 2.336; p = 0.005), corticosteroid use (58% vs 39%; OR 1.457; 95% CI 1.036 to 2.048; p = 0.031), eGFR (86.5 (IQR 22.2) vs 95.0 (IQR 28.0); OR 2.214; 95% CI 0.639 to 12.566; p = 0.041) and family history of ischaemic heart disease (2.5% vs 17.3%; OR 0.351; 95% CI 0.128 to 0.960; p = 0.041). In multivariable analysis, age, eGFR and family history were independently related with DD.
The prevalence of DD was significantly higher in patients with RA as compared to the general population from the EPIPorto cohort (13% vs 1.4%; p < 0.001).
“HFpEF risk”: combined strategy of echocardiographic evaluation and NT-proBNP
Excluding those with systolic dysfunction or without NT-proBNP analysis (n = 298 of 319), we identified 40 patients (13%) at “HFpEF risk” (LVEF ≥ 50% and NT-proBNP > 125 pg/mL and structural echocardiographic changes [12]). After analysis of all covariates in Table 1, age (OR 1.078; p < 0.001), CKD (OR 0.178; p = 0.013), eGFR (OR 0.977; p = 0.005) and RA duration (OR 1.031; p = 0.037) were associated with “HFpEF risk”. On multivariable analysis, age was the only independent predictor of “HFpEP risk”.
The “HFpEF risk” was significantly associated with ventricular function categories, with 82% of those without “HFpEF risk” showing preserved ventricular function (vs 35% with risk). However, patients with “HFpEF risk” were equally distributed among preserved ventricular function (14/40), indeterminate diastolic function (13/40) and diastolic dysfunction (13/40).
Comparison with 2009 guidelines for diastolic dysfunction classification
A total of 311 patients (97%) had enough data to compare the 2009 and 2016 classifications. When we applied a simplified model of the 2009 recommendations [13] to classify diastolic dysfunction, more patients would fulfil criteria for DD (23% versus 13% using the 2016 criteria)—Fig. 4 and Supplementary Table 1. The percentage of IDF would also be much higher (47% vs 11%). The concordance between both classifications was low (Cohen’s Kappa = 0.25).
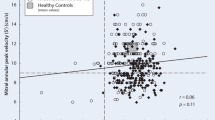
The specific echocardiographic parameters that can represent structural or functional changes related to HF were on average within normal limits (Supplementary Table 2). Most of these echocardiographic parameters were associated with several cofactors, namely age, hypertension and diabetes, and correlated with NT-proBNP and 6MWT.
Cardiovascular surrogate markers
NT-proBNP
The NT-proBNP levels were associated with “any ventricular dysfunction” and with the categorization of ventricular function using either 2009 or 2016 guidelines (but were not significantly different between DD and PVF). NT-proBNP levels were also significantly associated with most echocardiographic parameters (shown in Supplementary Table 3). Overall, 87 of the 311 patients (28%) presented an NT-proBNP ≥ 125 pg/mL (cut-off generally set for chronic HF), corresponding to 34% of DD and 46% of SD patients.
hsTnT
The hsTnT levels were associated with categories of ventricular function (using 2009 or 2016 classification), but were not significantly associated with having “any ventricular dysfunction” or “HFpEF risk”. The log(hsTnT) was associated with having DD versus PVF. Overall, 25 of 311 patients (8%) had a hsTnT above normal (> 0.014 pg/mL), but only 2 patients had a value above the cut-off value considered at our laboratory for acute coronary syndrome (> 0.054 pg/mL).
6MWT
All the major echocardiographic parameters were significantly associated with 6MWT performance. The total distance walked in 6MWT was also significantly associated with ventricular function as per the 2016 or 2009 classifications (and specifically with DD versus PVF), with “any ventricular dysfunction” and “HFpEF risk”.
Cardiovascular events
During a mean follow-up time of 2.8 ± 0.6 years (54 to 1095 days), only 9 cardiovascular events (cardiovascular death, heart failure or other cardiovascular driven hospitalization) were recorded, without association with ventricular function or with “HFpEF risk”.
Discussion
The main finding of our study is that RA patients without known cardiac disease showed a 4% prevalence of subclinical systolic function and 13% of diastolic dysfunction. An increasing age was the most important independent predictor of ventricular function.
Most previous studies used the 2009 guidelines [13], but their application is complex and different authors applied distinct algorithms; in most cases the presence of one DD parameter was sufficient [20,21,22]. Our findings also support the belief that the 2009 guidelines have a poor agreement with newer 2016 classification [16, 23,24,25]. Using the 2009 guidelines instead of the 2016 recommendations, the proportion of DD would have risen from 13 to 23%, while IDF would be found in 47% of patients instead of 11%. Invasive studies suggested that the 2016 guidelines are more specific [26] and that both guidelines cannot be used interchangeably. Even when using the same 2016 guidelines, the application of those recommendations and the number of parameters taken into consideration differs amongst studies, which can result in a significant discrepancy of the reported prevalence of DD [27]. Using the latest 2016 guidelines, the diastolic function can be considered normal or abnormal if > 50% of the available variables (and not necessarily 3 out of 4) are normal or abnormal, respectively. Therefore, we considered that 3 parameters were enough to classify diastolic function, but patients with less than 3 parameters had to be excluded.
In our study, that reflects real world circumstances, the TR velocity could not be properly assessed in more than half of the patients, which played an important role in the determination of ventricular function. In such cases, other parameters can be used—such as pulmonary vein flow, S’ velocity, E/A with Valsalva, atrial longitudinal strain, global left ventricular longitudinal strain and stress echocardiography—but when applied to a large-scale screening program it is unrealistic to use a non-standardized classification. Therefore, only participants with 4 measurable parameters could be labelled with IDF (none of the patients with only 3 available parameters could be classified with IDF since it is impossible to have 50% of abnormal parameters when only 3 are considered). Patients with 3 abnormal parameters out of 3 available parameters were classified with DD and patients with only 2 abnormal parameters out of 3 were also classified with DD, since they had > 50% positive criteria (albeit in patients without significant tricuspid regurgitation it is unlikely that the pulmonary pressures are increased). If we had considered that 3 abnormal parameters were mandatory to classify DD, then the number of DD would be much lower and IDF much higher. Unfortunately, most authors using 2016 guidelines do not specify how they classified participants with missing parameters. We could also have applied a different algorithm for patients with some ventricular hypertrophy that was proposed for myocardial disease in 2016 guidelines [14], but this was not done in other studies, namely in the main study we used for comparison [16]. The normal echocardiographic parameters in the elderly are different from a younger population and both the 2009 and 2016 classifications do not contemplate the age factor.
Acknowledging all these precautions needed when comparing studies, we compared our results to the EPIPorto cohort [16], that used the same classification for DD and was conducted in the general population of the same city, sharing similar biometric and sociodemographic features and that excluded patients with systolic dysfunction [16]. The study comprised a sample of 1,000 individuals and presented a 1.4% prevalence of DD, which is substantially smaller than in our cohort with RA patients (13%). Similarly, the STANLISLAS cohort [23] included a sample of 1,485 participants and also found a smaller overall prevalence of DD (1.3%)—even when comparing to their cohort with over 60 years of age, the prevalence of DD was only 3.1%. In opposition to other studies, we focused on subclinical ventricular dysfunction in patients RA—older studies [6, 28] have reported a DD prevalence of 30–50% in RA patients versus 25–30% in the general population, but these studies have considered patients who already had cardiovascular events and used different definitions of DD.
The terms DD and HFpEF are often used as interchangeable terms, but in fact their overlap is limited. We found that 13% of the patients had HFpEF features according to the 2016 HF European criteria [12], but interestingly the correspondence with ventricular dysfunction categories was weak. The echocardiographic parameters most frequently used to assess diastolic function or structural changes that are related to HFpEF were associated with traditional cardiovascular risk factors and showed a generally good correlation with prognostic surrogate markers, such as 6MWT, NT-proBNP and even hsTnT.
Given the short follow-up and small number of cardiovascular events, and albeit the association between ventricular function and surrogate prognostic markers such as 6MWT, NT-proBNP and hsTnT, our sample was probably underpowered to detect an association between echocardiographic classification and events. Most patients with ventricular dysfunction presented NT-proBNP and hsTnT levels that were within the normal range, and it is therefore difficult to use these biomarkers in clinical practice to detect subclinical ventricular impairment. The NT-proBNP and hsTnT levels were also changed in IDF and not specifically in DD or SD.
Overall, we did not find significant associations between characteristics of RA disease and echocardiographic parameters. Nonetheless, inflammatory markers, particularly ESR, showed a significant association with most echocardiographic findings (and also with other outcomes), suggesting that the inflammatory pathways may play a role in the development of cardiovascular diseases in patients with RA.
Compared to the general population, the prevalence of DD was significantly higher in our cohort of RA patients, particularly in older patients, who can benefit the most from echocardiographic screening. An early diagnosis would allow for a close follow-up and can improve effectiveness of treatment strategies to decrease the risk of HF. Even though RA and other autoimmune diseases have been identified as increasing the HF risk, there are no recommendations to date on how to follow-up and diagnose these patients.
Limitations
We acknowledge that our study has some limitations in addition to those inherent to the definition of DD that are previously discussed. Despite being a prospective study, the follow-up duration was short. Due to its observational nature, we cannot infer causality, but only associations. Considering the relatively low prevalence of systolic and diastolic dysfunction, our sample size was probably underpowered to detect other independent predictors of SD and DD.
We did not explore different grades of diastolic dysfunction, given the reduced group size. We used the most common operational definition for systolic impairment, but it is possible that patients with LVEF > 50% may also have some systolic dysfunction. We did not evaluate other echocardiographic parameters, such as global longitudinal strain, that can detect early systolic ventricular dysfunction—however, this would make screening much more cumbersome and there are no recommendations on how to manage changes in ventricular mechanics in the absence of systolic or diastolic dysfunction.
When analyzing NT-proBNP levels and particularly for the classification of “HFpEF risk”, one should be aware that age-stratified cut-offs may be more appropriate. Moreover, this biomarker is affected by renal function and weight. Our goal was to assess current guidelines, but we believe that future guidelines may take stratified thresholds into consideration.
In future studies, our intention is to continue the follow-up of these patients, particularly those with indeterminate diastolic function, to ascertain what is their evolution and prognosis. We believe that our ongoing search of the optimal echocardiographic identification of diastolic dysfunction must be guided by clinical outcomes.
Conclusion
Patients with RA without any known cardiac disease showed a 4% prevalence of subclinical systolic function and 13% of diastolic dysfunction. The prevalence of diastolic dysfunction was higher than a comparable general population. Older age (particularly > 57 years) stood out as the most important independent predictor of ventricular dysfunction in patients with RA. A screening strategy using TTE may therefore be useful in older RA patients.
References
Solomon DH, Karlson EW, Rimm EB, Cannuscio CC, Mandl LA, Manson JE, Stampfer MJ, Curhan GC (2003) Cardiovascular morbidity and mortality in women diagnosed with rheumatoid arthritis. Circulation 107(9):1303–1307
Giles JT, Fernandes V, Lima JA, Bathon JM (2005) Myocardial dysfunction in rheumatoid arthritis: epidemiology and pathogenesis. Arthritis Res Ther 7(5):195–207
Agca R, Heslinga SC, Rollefstad S, Heslinga M, McInnes IB, Peters MJ, Kvien TK, Dougados M, Radner H, Atzeni F, Primdahl J, Södergren A, Wallberg Jonsson S, van Rompay J, Zabalan C, Pedersen TR, Jacobsson L, de Vlam K, Gonzalez-Gay MA, Semb AG, Kitas GD, Smulders YM, Szekanecz Z, Sattar N, Symmons DP, Nurmohamed MT (2017) EULAR recommendations for cardiovascular disease risk management in patients with rheumatoid arthritis and other forms of inflammatory joint disorders: 2015/2016 update. Ann Rheum Dis 76(1):17–28
Pujades-Rodriguez M, Duyx B, Thomas SL, Stogiannis D, Rahman A, Smeeth L, Hemingway H (2016) rheumatoid arthritis and incidence of twelve initial presentations of cardiovascular disease: a population record-linkage cohort study in England. PLoS ONE 11(3):e0151245
Khalid U, Egeberg A, Ahlehoff O, Lane D, Gislason GH, Lip GYH, Hansen PR (2018) Incident heart failure in patients with rheumatoid arthritis: a nationwide cohort study. J Am Heart Assoc 7(2):e007227
Sharma A, Kaushik R, Kaushik RM, Kakkar R (2015) Echocardiographic evaluation of diastolic dysfunction in rheumatoid arthritis—a case-control study. Mod Rheumatol 25(4):552–557
Myasoedova E, Davis JM 3rd, Crowson CS, Roger VL, Karon BL, Borgeson DD, Therneau TM, Matteson EL, Rodeheffer RJ, Gabriel SE (2013) Brief report: rheumatoid arthritis is associated with left ventricular concentric remodeling: results of a population-based cross-sectional study. Arthritis Rheum 65(7):1713–1718
Roubille C, Richer V, Starnino T, McCourt C, McFarlane A, Fleming P, Siu S, Kraft J, Lynde C, Pope J, Gulliver W, Keeling S, Dutz J, Bessette L, Bissonnette R, Haraoui B (2015) The effects of tumour necrosis factor inhibitors, methotrexate, non-steroidal anti-inflammatory drugs and corticosteroids on cardiovascular events in rheumatoid arthritis, psoriasis and psoriatic arthritis: a systematic review and meta-analysis. Ann Rheum Dis 74(3):480–489
Davis JM 3rd, Roger VL, Crowson CS, Kremers HM, Therneau TM, Gabriel SE (2008) The presentation and outcome of heart failure in patients with rheumatoid arthritis differs from that in the general population. Arthritis Rheum 58(9):2603–2611
Bradham WS, Bian A, Oeser A, Gebretsadik T, Shintani A, Solus J, Estis J, Lu QA, Todd J, Raggi P, Stein CM (2012) High-sensitivity cardiac troponin-I is elevated in patients with rheumatoid arthritis, independent of cardiovascular risk factors and inflammation. PLoS ONE 7(6):e38930
Provan S, Angel K, Semb AG, Atar D, Kvien TK (2010) NT-proBNP predicts mortality in patients with rheumatoid arthritis: results from 10-year follow-up of the EURIDISS study. Ann Rheum Dis 69(11):1946–1950
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, González-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P, Authors/Task Force Members; Document Reviewers (2016) 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail 18(8):891–975
Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, Waggoner AD, Flachskampf FA, Pellikka PA, Evangelista A (2009) Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr 22(2):107–133
Nagueh SF, Smiseth OA, Appleton CP, Byrd BF 3rd, Dokainish H, Edvardsen T, Flachskampf FA, Gillebert TC, Klein AL, Lancellotti P, Marino P, Oh JK, Popescu BA, Waggoner AD (2016) Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 29(4):277–314
Villeneuve E, Nam J, Emery P (2010) 2010 ACR-EULAR classification criteria for rheumatoid arthritis. Rev Bras Reumatol 50(5):481–483
Almeida JG, Fontes-Carvalho R, Sampaio F, Ribeiro J, Bettencourt P, Flachskampf FA, Leite-Moreira A, Azevedo A (2018) Impact of the 2016 ASE/EACVI recommendations on the prevalence of diastolic dysfunction in the general population. Eur Heart J Cardiovasc Imaging 19(4):380–386
Prevoo ML, van’t Hof MA, Kuper HH, van Leeuwen MA, van de Putte LB, van Riel PL (1995) Modified disease activity scores that include twenty-eight-joint counts. Development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum 38(1):44–48
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, Lancellotti P, Muraru D, Picard MH, Rietzschel ER, Rudski L, Spencer KT, Tsang W, Voigt JU (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 16(3):233–270
ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories (2002) ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 166(1):111–117
Levendoglu F, Temizhan A, Ugurlu H, Ozdemir A, Yazici M (2004) Ventricular function abnormalities in active rheumatoid arthritis: a Doppler echocardiographic study. Rheumatol Int 24(3):141–146
Gonzalez-Juanatey C, Testa A, Garcia-Castelo A, Garcia-Porrua C, Llorca J, Ollier WE, Gonzalez-Gay MA (2004) Echocardiographic and Doppler findings in long-term treated rheumatoid arthritis patients without clinically evident cardiovascular disease. Semin Arthritis Rheum 33(4):231–238
Liang KP, Myasoedova E, Crowson CS, Davis JM, Roger VL, Karon BL, Borgeson DD, Therneau TM, Rodeheffer RJ, Gabriel SE (2010) Increased prevalence of diastolic dysfunction in rheumatoid arthritis. Ann Rheum Dis 69(9):1665–1670
Huttin O, Fraser AG, Coiro S, Bozec E, Selton-Suty C, Lamiral Z, Frikha Z, Rossignol P, Zannad F, Girerd N (2017) Impact of changes in consensus diagnostic recommendations on the echocardiographic prevalence of diastolic dysfunction. J Am Coll Cardiol 69(25):3119–3121
Wan SH, Pumerantz AS, Dong F, Ochoa C, Chen HH (2019) Comparing the influence of 2009 versus 2016 ASE/EACVI diastolic function guidelines on the prevalence and echocardiographic characteristics of preclinical diastolic dysfunction (stage B heart failure) in a Hispanic population with type 2 diabetes mellitus. J Diabetes Complicat 33(8):579–584
Mokotedi L, Gunter S, Robinson C, Norton GR, Woodiwiss AJ, Tsang L, Dessein PH, Millen AME (2017) The impact of different classification criteria sets on the estimated prevalence and associated risk factors of diastolic dysfunction in rheumatoid arthritis. Int J Rheumatol 2017:2323410
Balaney B, Medvedofsky D, Mediratta A, Singh A, Ciszek B, Kruse E, Shah AP, Addetia K, Lang RM, Mor-Avi V (2018) Invasive validation of the echocardiographic assessment of left ventricular filling pressures using the 2016 diastolic guidelines: head-to-head comparison with the 2009 guidelines. J Am Soc Echocardiogr 31(1):79–88
Selmeryd J, Henriksen E, Leppert J, Hedberg P (2016) Interstudy heterogeneity of definitions of diastolic dysfunction severely affects reported prevalence. Eur Heart J Cardiovasc Imaging 17(8):892–899
Aslam F, Bandeali SJ, Khan NA, Alam M (2013) Diastolic dysfunction in rheumatoid arthritis: a meta-analysis and systematic review. Arthritis Care Res (Hoboken) 65(4):534–543
Funding
F. A. Saraiva is supported by Universidade do Porto/FMUP and FSE-Fundo Social Europeu, NORTE 2020-Programa Operacional Regional do Norte, NORTE-08-5369-FSE-000024-Programas Doutorais.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
This study was approved by the Ethics Committee of Centro Hospitalar Universitário do Porto (number 2016-023; 020-DEFI/020-CES).
Informed consent
All participants gave written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rodrigues, P., Ferreira, B., Fonseca, T. et al. Subclinical ventricular dysfunction in rheumatoid arthritis. Int J Cardiovasc Imaging 37, 847–859 (2021). https://doi.org/10.1007/s10554-020-02057-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-020-02057-3