Abstract
Objective
The aim of the present study was to evaluate cardiac involvement in patients with active rheumatoid arthritis (RA).
Methods
Forty patients with active RA participated. All were submitted to standard Doppler echocardiography and myocardial performance index (MPI) grading.
Results
There were left and right ventricular diastolic function abnormalities in RA patients. Left ventricular MPI was also significantly higher than in controls (P<0.05). A relationship was found between left ventricular early diastolic (E)/atrial (A) flow velocities (E/A ratio), isovolumic relaxation time (IRT), and disease duration (r=−0.47 and P=0.002, r=0.618 and P=0.000, respectively).
Conclusion
Diastolic function was impaired in both ventricles in patients with active RA. There was a direct relationship between some of the parameters of left ventricular diastolic function and disease duration as well. These findings suggest a subclinical myocardial involvement in RA patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Rheumatoid arthritis (RA) is a chronic and systemic articular inflammatory disease [1, 2], often associated with cardiac manifestations [3]. Among many other extra-articular features, several forms of cardiac involvement have been described in RA, most commonly pericarditis and pericardial effusion [4]. The rate of mortality due to cardiovascular disease and ischaemic heart disease in both sexes is higher in RA [5]. Autopsy studies have shown high incidences of pericardial, myocardial, and endocardial involvement in RA patients [6, 7]. These lesions may cause conduction defects, myocardiopathy, structural abnormalities, and cardiac dysfunction. Cardiac failure is the result of systolic or diastolic dysfunction or both [8]. Systolic dysfunction and cardiac failure are often preceded by alterations in left ventricular diastolic function, which may be clinically silent for years or even decades [9].
Doppler echocardiography is a sensitive and noninvasive method for detecting cardiac abnormalities and systolic and/or diastolic dysfunction. Although easy to use, this conventional method has several limiting factors, such as the effects of changes in preload-afterload and arrhythmia on the method.
Recently, a myocardial performance index (MPI) was suggested for evaluating ventricular function. The MPI gives information about the global function of a ventricle by assessing systolic and diastolic phases of the cardiac cycles simultaneously [10]. Since it is a ratio of time intervals, it reflects the systodiastolic rather than solely systolic or diastolic dysfunction [11]. It was also shown to be independent of changes in preload and afterload, heart rate, and tricuspid regurgitation during the assessment of ventricular myocardial performance [12].
The aim of the present study was to evaluate cardiac involvement in patients with active RA by standard pulsed-wave Doppler echocardiography and MPI.
Patients and methods
The study was carried out on 40 outpatients (eight men and 32 women) and 44 age- and sex-matched healthy controls (35 women, nine men). All of them fulfilled the 1987 revised criteria of the American College of Rheumatology for RA [13]. The disease was considered to be active if the patient had at least two of the following features [9]:
-
1.
Six or more tender joints
-
2.
Three or more swollen joints
-
3.
Morning stiffness lasting more than 45 min
-
4.
Erythrocyte sedimentation rate (ESR) higher than 25 mm
Patients with histories of rheumatic fever, systemic arterial hypertension, diabetes mellitus, primary cardiomyopathy, congenital heart disease, chronic lung disease, coronary artery disease, or arrhythmia and those with small echo window and poor image quality were excluded from the study. None of the subjects were on any pharmaceutical treatment (beta blockers, Ca channel blockers, etc.) except for antirheumatic drugs. All patients were evaluated for the numbers of tender and swollen joints and submitted to laboratory analyses including ESR, C-reactive protein (CRP), complete blood count (CBC), serum protein electrophoresis, serum creatinine, serum transaminases, and rheumatoid factor (latex agglutination test) measurement.
All patients were in stage 1–4 of the disease according to Steinbrocker's criteria [14]. The joints were scored for tenderness on a 0–3 scale according to the Ritchie Articular Index [15]. Total Ritchie Index, which is the number of tender and swollen joints, was also calculated. Each patient filled in a health assessment questionnaire (HAQ) [16] for assessment of functional impairment. All patients were treated with second-line drugs (hydroxychloroquine, methotrexate, sulphasalazine) and steroids.
Echocardiography
In all subjects, two-dimensional, M-mode, pulsed Doppler, and color flow Doppler echocardiography examinations (ATL 5000, 2–4 MHz phased array transducer) were performed by the same examiner. The ejection fraction of the left ventricle was obtained using Simpson's biplane methods in two-dimensional echocardiography [17]. The left atrial and ventricular dimensions were measured with M-mode echocardiography using a parasternal window. Fractional shortening was calculated using the equation: (end diastolic diameter minus end systolic diameter)×100/end diastolic diameter. The pulsed Doppler recordings of mitral and tricuspid flow velocities were obtained from the apical 4-chamber view by placing the sample volume between the tips of the mitral and tricuspid leaflets. The peak early diastolic flow (E) and peak atrial flow (A) velocities, E wave deceleration time, time-velocity integrals of early diastolic flow velocity curve (E-VTI), time-velocity integrals of the atrial contraction velocity curve (A-VTI), and time-velocity integrals of the total diastolic velocity curve (T-VTI) were recorded. The E/A and E-VTI/A-VTI ratios and left atrial filling fractions (AFF=A-VTI/T-VTI) were calculated.
Myocardial performance index measurements:
The Doppler time intervals were measured using atrioventricular (mitral and tricuspid valves) inflow and left and right ventricular outflow tract velocities. Left ventricle outflow velocities were obtained from the apical 5-chamber view by placing the sample volume in the outflow tract below the aortic valves. Right ventricle outflow velocities were obtained from the parasternal short-axis view by placing the sample volume in the outflow tract below the pulmonary valves.
The MPI is defined as the sum of isovolumic contraction time (ICT) and isovolumic relaxation time (IRT) divided by the ventricular ejection time (ET): (ICT+IRT)/ET. To derive the sum of ICT and IRT, the ejection time was subtracted from the interval between cessation and onset of atrioventricular valve inflow. Measured intervals are depicted in Fig. 1. The interval between cessation and onset of mitral valve inflow was measured from the end of the Doppler A wave of the mitral inflow signal to the beginning of the next E wave. Similarly, the interval between cessation and onset of tricuspid valve inflow was measured from the pulsed Doppler signal of tricuspid inflow. Ejection times of the left and right ventricles were measured from the onset to the end of the ventricular outflow Doppler velocity profile. The pre-ejection period was measured from the onset of the QRS complex to the onset of ventricular ejection flow. To minimise variations due to heart rate, the average values of five consecutive beats were used for the measurement of each interval.
Diastolic dysfunction was suspected when E velocity decreased, A velocity increased, the E/A ratio was <1, and deceleration time (DT) and IRT were prolonged (>150 ms and >100 ms, respectively) [18]. The normal MPI value was formerly reported as 0.39±0.05 for the left ventricle and 0.28±0.04 for the right ventricle [19].
Statistical analysis
The independent samples t-test and Pearson's correlation analysis were used for statistical analysis. Values of P<0.05 were considered to be statistically significant.
Results
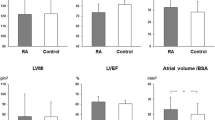
Demographic and clinical characteristics of the patients and controls are shown in Table 1. The mean ages were 48.50±11.80 years for patients and 46.1±12.7 years for the control group. There were no significant differences between age, heart rate, and systolic and diastolic blood pressure between RA patients and controls. The end systolic diameter of the left atrium, end diastolic diameter of the left ventricle, end systolic diameter of the left ventricle, ejection fraction, and fractional shortening were not statistically significantly different between the groups (Table 2).
Doppler echocardiography measurements of the left ventricle
Peak E velocity and E/A and E-VTI/A-VTI ratios were significantly lower than those of controls (P<0.05). Peak A velocity, A-VTI, and AFF were significantly higher (P<0.05). The mean IRT value was significantly longer than in controls (96.07±14.7 vs 73.72±9.5), and the IRT/ET ratio was significantly higher. We found no significant difference between the groups in other echocardiographic indices of left ventricle performance (Table 3). The mean value of left ventricular MPI was 0.52±0.12 in patients, which was also significantly higher than that of controls (0.43±0.06, P<0.05).
Doppler echocardiography measurements of the right ventricle
Mean A-VTI values were significantly higher in all patients than in healthy controls (P<0.05). The E/A and E-VTI/A-VTI ratios were also significantly lower in all the patients. In both groups, ET, ICT, and IRT intervals and ICT/ET and IRT/ET ratios did not differ (Table 4). The mean right ventricular MPI in RA patients (0.30±0.08) was not significantly different from that of controls (0.30±0.04) (P<0.05).
A significant correlation did not emerge between cardiac parameters and age, number of tender joints, Ritchie index, or HAQ score. No correlation was found between the Steinbrocker index stage and pulsed Doppler echo parameters (P>0.05). A correlation was present between the duration of illness and E/A ratio and IRT (P<0.05). There was no statistically significant correlation between other echocardiographic parameters and disease parameters (Table 5).
Discussion
Previous studies reported high mortality rates for RA [20, 21, 22, 23, 24, 25, 26, 27]. Researchers also noted that the rate of mortality in RA patients was dependent on concurrent heart disease [28]; however, many of these patients did not experience clinical cardiac symptoms [29]. Cardiac disease is often clinically silent in patients affected by RA.
The aim of our study was to evaluate cardiac function in patients affected by active RA but without clinical evidence of heart disease and to compare them with a control group matched for sex and age. We found diastolic dysfunction of right and left ventricles in patients with RA. In patients, we also found abnormal left ventricular MPI, which shows global ventricular function status.
Some studies report increased systolic and diastolic dysfunction in patients with RA [4, 20, 30, 31, 32, 33]. We found diastolic dysfunction in them. Abnormalities were detected in certain variables of both left ventricle diastolic dysfunctions such as E, A, E/A, A-VTI, AFF, and IRT and in right ventricle diastolic dysfunctions such as E/A, A-VTI, and E-VTI/A-VTI ratio in our study.
In accordance with the findings of previous studies [9, 31, 34], we could not find any correlation between inflammatory and functional disease parameters and variables of diastolic function. Also, no correlation was found between Steinbrocker index stage and pulsed Doppler echo parameters.
We found a statistically significant correlation between duration of disease and the alteration of left ventricle diastolic function expressed by E/A ratio and IRT. This result is in accordance with recent reports [9, 31, 34] showing a correlation between disease duration and an index of left ventricular function parameters. Other studies failed to find such a correlation [30, 32].
Until now, ventricular performance in RA has not been evaluated by measuring MPI, either. This index reflects both systolic and diastolic performance of the ventricles. The findings from this study showed that left ventricular MPI of the patients was significantly higher than that of controls. Right ventricular MPI class was preserved despite abnormal left ventricular MPI scores. We can only speculate that higher systemic pressures on the left ventricle and lower pulmonary pressures on the right ventricle might have been responsible for this observation.
A mechanistic explanation for the increase in cardiovascular disease (CVD)-related morbidity and mortality in this population remains elusive. The pathogenesis of CVD in the setting of RA is multifactorial [35]. There is increasing evidence that inflammatory mediators intrinsic to the disease represent major culprits in the development of CVD [36]. Inflammation, characteristic of active RA, likely plays a major role in CVD. Therefore, one can speculate that chronic cytokine release may lead to the deposition of connective tissue in the myocardium [9].
It has been suggested that subclinical vasculitis, speculated to be common in RA, leads to endothelial injury and accelerated atherosclerosis [37]. Myocardial fibrosis and inflammation have been reported in about 20% of the patients in autopsy studies [38, 39].
The earliest deterioration in cardiac disease is in diastolic function. Such abnormalities have been reported in a number of conditions such as arterial hypertension, coronary artery disease, and in elderly subjects. We selected patients with no evidence of hypertension or known cardiac disease. Impaired ventricular function was observed at all ages in RA patients but not in control subjects, which suggests the deterioration of diastolic function in active RA at any age.
The inflammation may accelerate the development of atherogenesis, thrombosis, and congestive heart disease [35]. Medications aimed at combatting inflammation may also adversely affect a patient's CVD risk factor profile [40, 41, 42, 43]. For instance, chloroquine has cardiotoxic side effects [44, 45]. D-penicillamine and gold salts are known to be capable of causing vasculitis, which may lead to myocardial dysfunction [46]. Sulphasalazine, methotrexate, nonsteroidal anti-inflammatory drugs, and steroids do not have known direct cardiotoxic side effects. Our patients were treated with second-line drugs (chloroquine, sulphasalazine, methotrexate) following the diagnosis of RA. None were treated with gold salts or D-penicillamine. In this study, the actual duration of antirheumatic therapy and the agents used varied in each patient. Therefore, we can not attribute our findings to the side effects of antirheumatic drug therapy. However, it is not clear whether the above mentioned parameters are effective in RA and whether they affect prognosis. We can not comment on the exact mechanism of ventricular dysfunction, because the present study was not planned to clarify its aetiopathogenesis.
In conclusion, this study showed impaired diastolic function in both ventricles of patients with active RA. The findings indicate a direct relationship between some parameters of left ventricular diastolic function (E/A ratio and IRT) and disease duration. They also suggest a subclinical myocardial involvement during the course of the disease. Being aware of unrecognised cardiac abnormalities can be very important for the correct assessment and management of RA patients. In addition to standard pulsed-wave Doppler echocardiography, MPI may be used for the evaluation of ventricular function in RA.
References
Wilder RL (1993) Rheumatoid arthritis, epidemiology, pathology and pathogenesis. In: Schumacher RH (eds) Primer on the rheumatic diseases. Arthritis Foundation, Atlanta, pp 86–89
Isomaki H (1992) Long-term outcome of rheumatoid arthritis. Scand J Rheumatol Suppl 95:3–8
Bacon PA (1993) Extra-articular rheumatoid arthritis. In: McCarty DJ, Koopman WJ (eds) Arthritis and allied conditions. Lea and Febiger, Philadelphia, pp 811–840
Corrao S, Salli L, Arnone S, Scaglione R, Amato V, Cecala M, Licata A, Licata G (1995) Cardiac involvement in rheumatoid arthritis: evidence of silent heart disease. Eur Heart J 16:253–256
Wallberg-Jonsson S, Öhman ML, Dahlqvist SR (1997) Cardiovascular morbidity and mortality in patients with seropositive rheumatoid arthritis in northern Sweden. J Rheumatol 24:445–451
Lebowitz WB (1963) The heart in rheumatoid arthritis. A clinical and pathological study of 62 cases. Ann Intern Med. 58:102–123
Bonfiglio T, Atwater EC (1969) Heart disease in patients with seropositive rheumatoid arthritis. Arch Intern Med 124:714–719
Apstein CS, Eberly FR (1998) Diastolic function and dysfunction with exercise, hypertrophy, ischemia, and heart failure. Cardiologia 43:1269–1279
Montecucco C, Gobbi G, Perlini S, Rossi S, Grandi AM, Caporali R, Finardi G (1999) Impaired diastolic function in active rheumatoid arthritis. Relationship with disease duration. Clin Exp Rheumatol 17:407–412
Tei C (1995) New non-invasive index for combined systolic and diastolic ventricular function. J Cardiol:26:396–404
Lax JA, Bermann AM, Cianciulli TF et al (2000) Estimation of the ejection fraction in patients with myocardial infarction obtained from the combined index of systolic and diastolic left ventricular function: a new method. J Am Soc Echocardiogr 13:116–123
Eidem BW, O'Leary PW, Tei C, Seward JB (2000) Usefulness of the myocardial performance index for assessing right ventricular function in congenital heart disease. Am J Cardiol; 86:654–658
Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS (1988) The American Rheumatism Association 1987 criteria for the classification of rheumatoid arthritis. Arthritis Rheum 31:315–324
Steinbrocker O, Treger H, Cornelius H (1949) Therapeutic criteria in rheumatoid arthritis. JAMA 140:659–662
Ritchie DM, Boyle JA, McInnes JM, Jasani MK, Dalakos TG, Grieveson P, Buchanan WW (1968) Clinical studies with an articular index for the assessment of joint tenderness in patients with rheumatoid arthritis. Q J Med 147:393–406
Wade DT (1992) Measurement in neurological rehabilitation. Oxford University Press, New York, pp 189–191
Schiller NB, Shah PM, Crawford M et al (1989) Recommendations for quantification of the left ventricle by two-dimensional echocardiography. J Am Soc Echocardiogr 2:358–367
Appleton CP, Hatle LK, Popp RL (1988) Relation of transmitral flow velocity patterns to left ventricular diastolic function: new insights from a combined hemodynamic and Doppler echocardiographic study. J Am Coll Cardiol 12:426–440
Oh JK, Seward JB, Tajik AJ (1999) The echo manual, 2nd edn. Lippincott Williams and Wilkins, Philadelphia, p 55
Wislowska M, Sypula S, Kowalik I (1999) Echo cardiographic findings and 24-h electrocardiographic Holter monitoring in patients with nodular and non-nodular rheumatoid arthritis. Rheumatol Int 18:163–169
Allebeck P (1982) Increased mortality in rheumatoid arthritis. Scand J Rheumatol 11:81–86
Martinez MS, Garcia-Monforte A, Rivera J (2001) Survival study of rheumatoid arthritis patients in Madrid (Spain). A 9-year prospective follow-up. Scand J Rheumatol 30:195–198
Mutru O, Laakso M, Isomaki H, Koota K (1989) Cardiovascular mortality in patients with rheumatoid arthritis. Cardiology 76:71–77
Myllykangas-Luosujarvi RA, Aho K, Kautianinen H, Isomaki H (1995) Cardiovascular mortality in females with rheumatoid arthritis. J Rheumatol 22:1065–1067
Myllykangas-Luosujarvi R, Aho K, Kautiainen H, Isomaki H (1995) Shortening of life span and causes of excess mortality in a population-based series of subjects with rheumatoid arthritis. Clin Exp Rheumatol 13:149–153
Allebeck P, Ahlbom A, Allander E (1981) Increased mortality among patients with rheumatoid arthritis, but where RA doesn't appear on the death certificate. Eleven-year follow-up of an epidemiological study. Scand J Rheumatol 10:301–306
Vandenbroucke JP, Hazevoet HM, Cats A (1984) Survival and cause of death in rheumatoid arthritis: a 25 year prospective follow-up. J Rheumatol 11:158–161
Pincus T, Callahan LF, Vaughn WK (1987) Questionnaire, walking time and button test measures of functional capacity as predictive markers for mortality in rheumatoid arthritis. J Rheumatol 14:240–251
Mody GM, Stevens JE, Meyers OL (1987) The heart in rheumatoid arthritis: a clinical and echocardiographic study. Q J Med 65:921–928
Mustonen J, Laakso M, Hirvonen T, Mutru O, Pirnes M, Vainio P, Kuikka JT, Rautio P, Lansimies E (1993) Abnormalities in left ventricular diastolic function in male patients with rheumatoid arthritis without clinically evident cardiovascular disease. Eur J Clin Invest 23:246–253
Di Franco M, Paradiso M, Mammarella A, Paoletti V, Labbadia G, Coppotelli L, Taccari E, Musca A (2000) Diastolic function abnormalities in rheumatoid arthritis. Evaluation by echo Doppler transmitral flow and pulmonary venous flow: relation with duration of disease. Ann Rheum Dis 59:227–229
Rowe IF, Gibson DG, Keat ACS, Breverton DA (1991) Echocardiographic diastolic abnormalities of the left ventricle in inflammatory joint disease. Ann Rheum Dis 50:227–230
Maione S, Valentini G, Giunta A, Tirri R, Giacummo A, Lippolis C, Arnese M, De Paulis A, Marone G, Tirri G (1993) Cardiac involvement in rheumatoid arthritis: an echocardiographic study. Cardiology 83:234–239
Cindas A, Gokce-Kutsal Y, Tokgözoglu L, Karanfil A (2002) QT dispersion and cardiac involvement in patients with rheumatoid arthritis. Scand J Rheumatol 31:22–26
Mikuls TR, Saag KG (2001) Rheumatoid arthritis: comorbidity in rheumatoid arthritis. Rheum Dis Clin North Am 27:283–303
Pasceri V, Yeh E (1999) A tale of two diseases: atherosclerosis and rheumatoid arthritis. Circulation 100:122–126
Bacon P, Kitas G (1994) The significance of vascular inflammation in rheumatoid arthritis. Ann Rheum Dis 53:621–623
Schwartz S (1977) Rheumatoid carditis. JAMA 201:556–558
Sweezy RL (1967) Myocardial infarction due to rheumatoid arteritis. JAMA 199:855–857
Page J, Henry D (2000) Consumption of NSAIDs and the development of congestive heart failure in elderly patients. Arch Intern Med 160:777–784
Nashel D (1986) Is atherosclerosis a complication of long-term corticosteroid treatment? Am J Med 80:925–929
Landewe R, van den Borne B, Breedveld F et al (2000) Methotrexate effects in patients with rheumatoid arthritis with cardiovascular comorbidity. Lancet 355:1616–1617
Haagsma C, Blom H, van Riel PL et al (1999) Influence of sulfasalazine, methotrexate and combination of both on plasma homocysteine concentrations in patients with rheumatoid arthritis. Ann Rheum Dis 58:79–84
Iglesias Cubero G, Rodriguez Reguero JJ, Rojo Ortega JM (1993) Restrictive cardiomyopathy caused by chloroquine. Br Heart J 69:451–452
Ratliff NB, Estes ML, Myles JL, Shirey EK, McMahon JT (1987) Diagnosis of chloroquine cardiomyopathy by endomyocardial biopsy. N Engl J Med 316:191–193
Qasim FJ, Thiru S, Gillespie K (1997) Gold and D-penicillamine induce vasculitis and up-regulate m RBA for IL-4 in the Brown Norway rat: support for a role of Th2 cell activity. Clin Exp Immunol 108:438–445
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Levendoglu, F., Temizhan, A., Ugurlu, H. et al. Ventricular function abnormalities in active rheumatoid arthritis: a Doppler echocardiographic study. Rheumatol Int 24, 141–146 (2004). https://doi.org/10.1007/s00296-003-0342-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-003-0342-z