Abstract
Regadenoson Stress Echocardiography (RSE) can detect myocardial ischemia, and its diagnostic accuracy should be evaluated. We sought to investigate the agreement between RSE and gated-SPECT myocardial perfusion imaging (MPI) and appraise its diagnostic accuracy. Consecutive patients (n = 202) referred for non-invasive evaluation of myocardial ischemia, with (38.6%) or without a previous coronary artery disease (CAD) diagnosis, were enrolled. Both tests were performed simultaneously. Invasive coronary angiography (CA) is considered the gold standard. The mean age was 70.9 (9.8) years, and 59.9% were male. The prevalence of cardiovascular risk factors (arterial hypertension [81.7%], diabetes mellitus [37.6%], hypercholesterolemia [71.8%], and smoking [18.8%]) was high. Forty-four patients (21.8%) had a non-interpretable electrocardiogram, 15 (34.1%) of them were a result of ventricular paced-rhythm, while 29 (65.9%) were a result of advanced left ventricular branch block. The overall agreement between both diagnostic techniques was good: Gwet’s AC1 0.66 (CI95% 0.55 to 0.76), and it was higher in patients without a previous CAD diagnosis: 0.76 (CI95% 0.65 to 0.87). In the biased sample (those who underwent CA), RSE and nuclear study sensitivity was 0.50 and 0.78 and specificity was 0.75 and 0.75, respectively. We noted a dramatic reduction in sensitivity for RSE after debiasing (debiased sensitivity of 0.16), and the negative predictive value was similar to the biased and debiased samples. RSE is in strong agreement with gated-SPECT MPI. However, its low sensitivity and negative predictive value preclude its use as a bedside test to detect myocardial ischemia.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Regadenoson is the first pharmaceutical agent to act as a selective agonist of the adenosine A2A receptors[1]. Intravenous injection induces coronary vasodilation with a rapid onset of action (time to peak myocardial hyperemia is 20–40 s) and a short effect (2–3 min), and it is given as a fixed-bolus dose. It has a very good safety profile and its side effects can be readily reversed with aminophylline. Regadenoson has been approved as a stress agent for gated-SPECT (Single Photon Emission Computed Tomography) myocardial perfusion imaging (MPI) to detect ischemia because it can induce a mismatch of blood flow in normal and under-perfused cardiac territories with a significant increase in heart rate and, as such, it is widely used in this clinical scenario.
The diagnostic information and safety of regadenoson were non-inferior to that of adenosine as a stressor agent for gated-SPECT MPI, as demonstrated in a phase 3 international clinical trial[2]. However, that trial did not use coronary angiography as the reference standard, and thus, it assumed the same diagnostic yield as regadenoson compared to the adenosine myocardial perfusion stress test. Moreover, the overall agreement between regadenoson and adenosine myocardial perfusion results (number of ischemic segments) was moderate. In a quantitative analysis of this trial, the extent of total perfusion defect size was similar between regadenoson and adenosine[3]. There are few reports on the use of regadenoson stress echocardiography (RSE), and most of them evaluated changes in myocardial perfusion during the administration of intravenous contrast echocardiographic agent [4, 5].
The idea to perform a rapid and safety stress echocardiogram to detect myocardial ischemia at a patient’s bedside is very alluring to the practitioner. RSE fulfills all the prerequisites for being a good contender for this purpose, but the accuracy of the test should be evaluated in advance in real-life patients.
We investigated the agreement between RSE regadenoson gated-SPECT with technetium-99m sestamibi or tetrofosmin and also quantitate the accuracy of the test, using coronary angiography as the gold-standard, and avoiding the verification bias with numerical methods.
Methods
Consecutive patients with chest pain because of suspected cardiac ischemic etiology who were referred to our imaging unit were included in the study. Patients were selected if they were unable to walk or run, had a left bundle branch on the surface electrocardiogram, or had a paced-ventricular rhythm. The first patient was included in May 2017 and the last in October 2019. The exclusion criteria were as follows: (1) age < 18 years; (2) no signed informed consent obtained from the patient or their legal guardian; (3) severe asthma; (4) atrioventricular conduction defects (second or third-degree block); (5) systolic blood pressure of less than 90 mmHg or uncontrolled hypertension (systolic pressure > 200 mmHg or diastolic pressure > 110 mmHg); (6) high suspicion of unstable angina based on clinical symptoms; (7) known hypersensitivity to adenosine or regadenoson; (8) history of serious uncontrolled ventricular arrhythmia; (9) caffeine intake within the previous 12 hours; (10) severe aortic stenosis or hypertrophic cardiomyopathy; or (11) pregnancy or breast-feeding. All participants or their legal guardian provided written informed consent to participate in the study. This research complied with the guidelines of our local ethics committee and was performed according to the Code Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans.
Patients were divided into two groups. Group A included patients with a previous CAD diagnosis with or without revascularization, and group B included patients who were referred for the first diagnosis of ischemic heart disease. The diagnostic yield of the RSE was evaluated in the entire cohort and agreement between both non-invasive techniques in both groups was evaluated separately.
With the patient lying in the left lateral position, a resting echocardiogram was obtained in the parasternal (long and short axis) and apical (four and two chambers) views and the images were digitally stored. The blood pressure and the 12-lead electrocardiogram were recorded throughout the test. Regadenoson (400 µg) was administered as a bolus in a peripheral vein, followed immediately by a 5-mL saline flush. 60 to 90 s later, the stress echocardiogram was performed using the same echocardiographic views to compare side to side rest and stress images. Using the same venous access and 15–20 s after the administration of regadenoson, 555 MBq (15 mCi) of the radiotracer (either technetium-99m sestamibi or tetrofosmin) was injected coinciding with the increase in heart rate. A gated-SPECT scan was performed 60±10 min after the radiotracer injection, and, in the case of a positive result, a new set of images was obtained at rest 1 day later. A cardiologist and a nuclear medicine specialist interpreted the results of the gated-SPECT MPI, and both were blinded to the result of the stress echocardiogram.
RSE was considered to be positive if at least two adjacent segments showed worsening contractility using the following grading scheme: normal, hypokinesia, akinesia, and dyskinesia (a shift from akinesia to dyskinesia was not considered to indicate ischemia). The stress echocardiograms were evaluated by two experienced observers each of whom had performed more than 300 tests each year. If there was a discrepancy, a third observer broke the tie by consensus with the other two.
All gated-SPECT MPI scans (General Electric Discovery NM/CT 870DR) were performed according to the American Society of Nuclear Cardiology guidelines [6]. Briefly, patients were imaged in the supine position and acquisition was performed over 180 degrees of rotation obtaining 60 projection data sets. The projections were acquired into a 64 × 64 matrix with a zoom of 1.33 and a 20% symmetrical energy window around 140 keV. Reconstruction was performed using filtered back projection techniques, with a Butterworth filter with a cutoff frequency of 0.45 and a power of 5. Possible perfusion defects were qualitatively analyzed. Wall motion and thickening were scored using standard nomenclature that was based on the guidelines. An unequivocal perfusion score defect that was greater than or equal to 1 with reduced regional wall motion and thickening was deemed to be ischemic when a perfusion defect was detected in only one basal segment of the left ventricle. A segment was considered to be necrotic, either transmural or not, if there was no change in the perfusion defect between the rest and stress images, otherwise was considered to be ischemic. We used attenuation correction based on map from CT. Both corrected and uncorrected images were interpreted to obtain a conclusion.
For the purpose of this study the results of both tests were categorized as positive (indicative of inducible ischemia) or negative.
Coronary angiography, if indicated by the attending physician, was performed using standard techniques within a period that was not greater than 6 months. Significant CAD was defined as the presence of more than 70% reduction in the lumen of at least one epicardial artery or a reduction between 50% and 70%, with a fractional flow reserve of < 0.85. For a patient who was surgically revascularized, only those with stenosis in one of the grafts or stenosis beyond the distal anastomosis using the same cutoff values were considered to be significant.
Statistical analysis
Continuous variables with normal distribution are presented as the mean and standard deviation between parenthesis. Variables with non-normal distribution are presented as the median (interquartile range [IQR]). Discrete variables are presented as n (%) and compared using the Chi-square or Fisher’s exact test, as necessary.
Agreement between both tests was assessed using Gwet’s first order agreement coefficient (Gwet’s AC1). Because a high prevalence of negative results in both tests was anticipated, we chose this statistic instead of the most commonly used Cohen’s kappa (κ) index because it is more sensitive to the prevalence of the different categories [7]. McNemar’s χ2 statistic was used to assess if disagreement was distributed evenly, and a significant p-value indicated an uneven agreement distribution. This index was applied to the results of the studies that were categorized as positive or negative depending if myocardial ischemia was detected and depending on the territories where the ischemia was detected, which were categorized into the following three groups: anterior/lateral, posterior/inferior, and multiple segments. We considered a Gwet’s AC1 value between 0 and 0.20 as slight, 0.21 to 0.40 as fair, 0.41 to 0.60 as moderate, 0.61 to 0.80 as substantial, and > 0.80 as an almost perfect agreement.
Sensitivity, specificity, and positive and negative predictive values were calculated in the group of patients who had an invasive coronary angiogram performed. The method described by Begg and Greenes was used to prevent the expected verification bias [8], by which a patient with a positive test has a higher probability of undergoing an invasive coronary angiogram. This method assumes that the positive and negative predicted values are the same for patients who were and were not verified using the gold-standard procedure, which, in this case, was a coronary angiogram.
The positive likelihood ratio (LR) (LR+) and negative LR (LR−) were calculated as follows: LR + = sensitivity/(1 − specificity) and LR− = specificity/(1 − sensitivity).
No data in this study were missing. Analyses were performed using R software, version 3.6.2 (R Project for Statistical Computing). We set a p-value of < 0.05 as statistically significant.
All authors contributed to the study conception and design. The first draft of the manuscript was written by the first author and all the contributors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Results
Two hundred two patients were included in the study. The baseline characteristics of the entire group are shown in Table 1. Overall, 78 patients (38.6%) had a diagnosis of ischemic heart disease before the stress tests. The pre-test probability of CAD in group B was low (< 15%) in 22.6%, intermediate (15–85%) in 76.6%, and high (> 85%) in 0.8% of the patients. Forty-four patients (21.8%) had a non-interpretable electrocardiogram, and 15 (34.1%) of them were a result of ventricular paced-rhythm, while 29 (65.9%) were a result of advanced left ventricular branch block.
Regadenoson induced a significant decrease in systolic arterial pressure: 134.4 (19.5) mmHg before and 129.3 (23.5) mmHg 60–90 s after administration, with a mean difference of 2.1 mmHg (95% confidence interval [CI] 0.01 to 4.22, p = 0.048). It also caused a significant decrease in diastolic blood pressure: 74.0 (11.2) mmHg vs. 71.4 (11.7) mmHg, with a mean difference of 2.6 mmHg (95%CI 1.4 to 3.8, p < 0.001) and a significant increase in heart rate from 65.3 (11.8) bpm to 88.7 (15.4) bpm, with a mean difference of 23.4 bpm (22.1 to 24.7 bpm, p < 0.001). The most common side effects were shortness of breath (n = 110, 54,5%), facial flushing (n = 47, 23,3%) and dizziness (n = 32, 15,8%).
Five RSE results were discarded because of inadequate image quality. Interobserver and intraobserver agreement for myocardial perfusion studies were 92% an 95% and for stress echocardiograms 85% and 88% respectively. The results of the agreement analysis are depicted in Table 2. Overall, there is strong agreement between both techniques, and the agreement was even better in group B, patients without a previous CAD diagnosis; this result was markedly lower than Gwet’s AC1 value in group A. Moreover, in the small subgroup of patients who had positive results with both tests, the agreement in the area where ischemia was detected was also strong. McNemar’s statistic, albeit only significant in the whole group, indicates that there was some degree of uneven distribution in the agreement because most of it came from the negative results; overall, there were 130 patients with both results that were negative, 23 patients with both results that were positive, and 44 patients with discordant results. Among the group of patients with a positive gated – SPECT MPI, those with a positive RSE exhibited more segments with inducible ischemia, although the difference was not statistically significant: 3.8 (2.7) vs. 2.8 (1.9), p = 0.173.
Only three (1.9%) patients with interpretable electrocardiograms had ischemic changes in repolarization with regadenoson.
During the 6-month follow-up, 31 coronary angiograms were performed, 23 (74.2%) with significant coronary or graft stenosis and 11 (35.5%) with left main or three-vessel disease. Eight angiograms (6.2%) were performed in patients with both negative tests and 23 (33.3%) in patients with at least one positive test (p < 0.001), demonstrating the presence of verification bias. Eighteen (22.8%) patients in group A and 13 (10.6%) patients in group B had a coronary angiogram performed (p = 0.032). The diagnostic accuracy in the biased and debiased sample is shown in Table 3.
Discussion
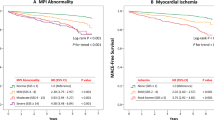
In patients who were referred for evaluation of chest pain, a substantial agreement between RSE and gated-SPECT MPI was detected. If the patient had a previous CAD diagnosis, the agreement between both techniques was lower. However, the sensitivity and negative predictive values for the RSE seemed to be low enough to apply this technique in everyday clinical practice to a heterogeneous population of patients with intermediate pretest probability or a previous CAD diagnosis (Fig. 1).
Appraisal of the agreement between two diagnostic tests is not an easy task. Clinical practice shows that sometimes, the agreement is readily achieved while in other situations, agreement occurs almost at random. The Gwet’s AC1 statistic, instead of the most commonly used Cohen’ Kappa index, considers this and is a more reliable measure of agreement when there is an uneven disagreement distribution. Overall, the agreement between both tests was substantial, between 0.6 and 0.8, which was lower when the subgroup of patients with a previous CAD diagnosis was analyzed.
We detected an uneven agreement distribution, with most of the agreement established in negative results (130 of 143 concordant results) and a higher rate of discrepancy when one of the tests was positive. This is not surprising because myocardial ischemia often precedes regional diastolic and systolic dysfunction in the ischemic cascade [9]. This may explain the higher sensitivity and the larger ischemic area that was detected with nuclear studies. Some myocardial segments (apical segments of the interventricular septum and lateral wall) can be perfused either by the right or left coronary artery, and scintigraphic studies detect a larger ischemic area; thus, some disagreement could be anticipated. This disagreement is higher if the patient has a previous CAD diagnosis, probably reflecting the uncertainties in detecting ischemia if necrotic areas with systolic dysfunction are found. Because nuclear studies are more sensitive in the overall population, it is compelling that RSE has a high rate of false-negative tests in this clinical scenario and, therefore, this reduces the agreement between both techniques. Given this unbalanced disagreement distribution, it would be tempting to use both tests simultaneously to increase the chance of detecting myocardial ischemia. The cardiologist should take into consideration that the simultaneous interpretation of both tests, when one or both indicates ischemia, could lead to a false increase in the positivity rate, thereby increasing the sensitivity and decreasing the specificity.
The low sensitivity of RSE that was found in this study deserves special consideration. The recently published guidelines for performance, interpretation, and application of stress echocardiography in ischemic heart disease [10] report an average sensitivity of 0.88 and specificity of 0.83 for ischemia detection, while the sensitivity is comparable to and the specificity is higher than nuclear myocardial perfusion studies. Remarkably, most recent studies performed coronary angiography in all patients, trying to avoid the referral/verification bias [11,12,13,14,15]. When only patients with positive results were referred for coronary angiography, the reported sensitivity is strikingly lower [16]. Although sensitivity is mostly independent of the disease prevalence, it is linked to the extent of CAD, increasing as the severity of the disease increases [17]. In our study, patients were referred for coronary angiography if it was indicated by the attending cardiologist. As expected, more patients with positive results had the coronary angiogram performed, inducing a referral bias and, therefore, increasing the estimation of sensitivity and reducing the specificity. Thus, we used a numerical method to correct for this bias, obtaining a very low value for sensitivity in the debiased sample. The true value likely lies between the biased and debiased sensitivity, but in any case, it was lower enough to consider the test to be unreliable for detecting myocardial ischemia. Although it is well recognized that left bundle brand block or ventricular-paced rhythm increase the false positive rate of exercise myocardial perfusion studies, this is not the case with pharmacological stress studies [18] and, thus, the inclusion of almost 22% of patients with these specific abnormalities in ventricular activation probably did not impact evaluation of the test accuracy.
There is little information in the literature on the accuracy of RSE to detect myocardial ischemia and most of the published papers focused on myocardial perfusion echocardiography. Porter et al. (5) provide the diagnostic utility of the test in 100 patients who were referred for coronary angiography and who had a high prevalence of significant CAD and multivessel disease. They reported a sensitivity and specificity for detection of myocardial ischemia (angiographic cutoff value of 70% and wall motion abnormalities analysis) of 0.61 and 0.84, respectively, which is close to the metrics found in the biased analysis of our sample. However, our data came from a consecutive series of patients who were referred for evaluation of chest pain, and not necessarily for invasive angiography. Thus, the results are from a common scenario in everyday clinical practice, but with the limitation of verification bias.
Coronary angiography is the usual diagnostic tool to establish the accuracy of a non-invasive method to detect myocardial ischemia. Although considered to be the gold-standard for the diagnosis of ischemic heart disease, coronary angiography has some important shortcomings. First, it is an anatomic evaluation and not a functional test of the coronary tree. Second, some patients can have myocardial ischemia even in the absence of epicardial stenoses (i.e. microvascular angina). Third, some patients with epicardial stenoses do not have inducible myocardial ischemia. Thus, coronary angiography is a “tarnished” gold-standard with some flaws that should be considered. We took special care to avoid these limitations, including functional invasive validation of epicardial coronary stenosis when we evaluated the Fractional Flow Reserve in case of intermediate epicardial lesions. However, we included a high percentage of patients with known CAD, and most of them had revascularization and multivessel disease. These patients are more prone to be catheterized, making the interpretation of the coronary anatomy more difficult, influencing the calculation of the accuracy of the non-invasive tests, and suggesting a selection bias. The expected consequence would be an increase in sensitivity and even in this situation, the calculated sensitivity is low, reinforcing the findings of a low sensitivity for the stress echo. The small number of patients without a previous CAD diagnosis who were catheterized precludes a distinct analysis.
The interpretation of RSE is challenging. It requires a high level of expertise because the response to myocardial ischemia is usually seen as a change from normal contractility to mild-to-moderate hypokinesia, sometimes with post-systolic contraction. Minor changes in contractility after the administration of regadenoson could be overlooked by cardiologists. Moreover, Porter et al. (5) reported that the highest sensitivity with RSE when wall motion abnormalities were appraised was 4 to 6 min after the bolus of regadenoson. We acquired the stress images earlier based on the study design (60 to 90 s after the bolus). These two facts could have also influenced the low sensitivity that was found in our study. Whether quantitative methods to assess myocardial contractility, i.e. tissue Doppler imaging, or strain analysis could increase the sensitivity of the test has not been evaluated in this study. Further investigation in this direction is required. The relationship between the increase in heart rate induced by regadenoson and the sensitivity for the detection of myocardial ischemia was not specifically analyzed. Nonetheless, the positive rate did not rise in parallel with the increase in heart rate and was even lower for gated-SPECT studies (data not shown).
In conclusion, RSE results are in strong agreement with those of regadenoson gated-SPECT MPI. However, its low sensitivity to detect myocardial ischemia makes this test unreliable as a bedside rapid test in clinical practice. Determining if different RSE protocols are more useful to detect myocardial ischemia merits further clinical research.
Data availability
The dataset used in this study can be retrieved in: Iglesias-Garriz, Ignacio (2020), “Regadenoson stress echo and gated-SPECT, phase 2.”, Mendeley Data, V2, https://doi.org/10.17632/8vkpcz8wxd.2.
References
Al Jaroudi W, Iskandrian AE (2009) Regadenoson: a new myocardial stress agent. J Am Coll Cardiol 54:1123–1130. https://doi.org/10.1016/j.jacc.2009.04.089
Iskandrian AE, Bateman TM, Belardinelli L et al (2007) Adenosine versus regadenoson comparative evaluation in myocardial perfusion imaging: Results of the ADVANCE phase 3 multicenter international trial. J Nucl Cardiol 14:645–658. https://doi.org/10.1016/j.nuclcard.2007.06.114
Mahmarian JJ, Cerqueira MD, Iskandrian AE et al (2009) Regadenoson induces comparable left ventricular perfusion defects as adenosine. JACC Cardiovasc Imaging 2:959–968. https://doi.org/10.1016/j.jcmg.2009.04.011
Le DE, Bragadeesh T, Zhao Y et al (2011) Detection of coronary stenosis with myocardial contrast echocardiography using regadenoson, a selective adenosine A2A receptor agonist. Eur Hear J 13:298–308. https://doi.org/10.1093/ejechocard/jer232
Mary RPT, HR AR et al (2011) Rapid detection of coronary artery stenoses with real-time perfusion echocardiography during regadenoson stress. Circ Cardiovasc Imaging 4:628–635. https://doi.org/10.1161/CIRCIMAGING.111.966341
Holly TA, Abbott BG, Al-Mallah M et al (2010) Single photon-emission computed tomography. J Nucl Cardiol 17:941–973. https://doi.org/10.1007/s12350-010-9246-y
Wongpakaran N, Wongpakaran T, Wedding D, Gwet KL (2013) A comparison of Cohen’s Kappa and Gwet’s AC1 when calculating inter-rater reliability coefficients: a study conducted with personality disorder samples. BMC Med Res Methodol 13:61. https://doi.org/10.1186/1471-2288-13-61
Begg CB, Greenes RA (1983) Assessment of diagnostic tests when disease verification is subject to selection bias. Biometrics 39:207–215. https://doi.org/10.2307/2530820
Stillman AE, Oudkerk M, Bluemke DA et al (2018) Imaging the myocardial ischemic cascade. Int J Cardiovasc Imaging 34:1249–1263. https://doi.org/10.1007/s10554-018-1330-4
Pellikka PA, Arruda-Olson A, Chaudhry FA et al (2020) Guidelines for performance, interpretation, and application of stress echocardiography in ischemic heart disease: from the American Society of Echocardiography. J Am Soc Echocardiogr 33:1-41.e8. https://doi.org/10.1016/j.echo.2019.07.001
Kim M-N, Kim S-A, Kim Y-H et al (2016) Head to head comparison of stress echocardiography with exercise electrocardiography for the detection of coronary artery stenosis in women. J Cardiovasc Ultrasound 24:135–143
Abdelmoneim SS, Mulvagh SL, Xie F et al (2015) Regadenoson stress real-time myocardial perfusion echocardiography for detection of coronary artery disease: feasibility and accuracy of two different ultrasound contrast agents. J Am Soc Echocardiogr 28:1393–1400. https://doi.org/10.1016/j.echo.2015.08.011
Shaikh K, Wang DD, Saad H et al (2014) Feasibility, safety and accuracy of regadenoson–atropine (REGAT) stress echocardiography for the diagnosis of coronary artery disease: an angiographic correlative study. Int J Cardiovasc Imaging 30:515–522. https://doi.org/10.1007/s10554-014-0363-6
Caiati C, Lepera ME, Carretta D et al (2013) Head-to-head comparison of peak upright bicycle and post-treadmill echocardiography in detecting coronary artery disease: a randomized, single-blind crossover study. J Am Soc Echocardiogr 26:1434–1443. https://doi.org/10.1016/j.echo.2013.08.007
Peteiro J, Bouzas-Mosquera A, Estevez R et al (2012) Head-to-head comparison of peak supine bicycle exercise echocardiography and treadmill exercise echocardiography at peak and at post-exercise for the detection of coronary artery disease. J Am Soc Echocardiogr 25:319–326. https://doi.org/10.1016/j.echo.2011.11.002
Danilo N, Daniele R, Chiara C et al (2015) Detection of significant coronary artery disease by noninvasive anatomical and functional imaging. Circ Cardiovasc Imaging 8:e002179. https://doi.org/10.1161/CIRCIMAGING.114.002179
van Stralen KJ, Stel VS, Reitsma JB et al (2009) Diagnostic methods I: sensitivity, specificity, and other measures of accuracy. Kidney Int 75:1257–1263. https://doi.org/10.1038/ki.2009.92
Jazmati B, Sadaniantz A, Emaus SP, Heller GV (1991) Exercise thallium-201 imaging in complete left bundle branch block and the prevalence of septal perfusion defects. Am J Cardiol 67:46–49. https://doi.org/10.1016/0002-9149(91)90097-5
Acknowledgements
We are indebted to Concepción Gonzalez-Anton, Silvia Marcos-Rey, and Monica Dominguez-Barriales for their excellent nursing care of the patients during the stress studies.
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. The first draft of the manuscript was written by the first author and all the contributors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors do not declare any conflict of interest related to this research.
Ethical approval
Approval was obtained from the ethics committee of our institution. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Iglesias-Garriz, I., Vara-Manso, J., Sevilla, A. et al. Diagnostic accuracy of regadenoson stress echocardiography: concordance with gated-spect myocardial perfusion imaging. Int J Cardiovasc Imaging 37, 509–515 (2021). https://doi.org/10.1007/s10554-020-02033-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-020-02033-x