Abstract
Purpose
To provide comparative prognostic information of coronary atherosclerotic plaque volume and stenosis assessment in patients with suspected coronary artery disease (CAD).
Methods
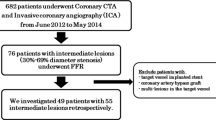
We followed 372 patients with suspected or known CAD enrolled in the CORE320 study for 2 years after baseline 320-detector row cardiac CT scanning and invasive quantitative coronary angiography (QCA). CT images were analyzed for coronary calcium scanning (CACS), semi-automatically derived total percent atheroma volume (PAV), segment stenosis score (SSS), in addition to traditional stenosis assessment (≥ 50%) by CT and QCA for (1) 30-day revascularization and (2) major adverse cardiac events (MACE). Area under the receiver operating characteristic curve (AUC) was used to compare accuracy of risk prediction.
Results
Sixty percent of patients had obstructive CAD by QCA with 23% undergoing 30-day revascularization and 9% experiencing MACE at 2 years. Most late events (20/32) were revascularization procedures. Prediction of 30-day revascularization was modest (AUC range 0.67–0.78) but improved after excluding patients with known CAD (AUC range 0.73–0.86, p < 0.05 for all). Similarly, prediction of MACE improved after excluding patients with known CAD (AUC range 0.58–0.73 vs. 0.63–0.77). CT metrics of atherosclerosis burden performed overall similarly but stenosis assessment was superior for predicting 30-day revascularization.
Conclusions
Angiographic and coronary atherosclerotic plaque metrics perform only modestly well for predicting 30-day revascularization and 2-year MACE in high risk patients but improve after excluding patients with known CAD. Atherosclerotic plaque metrics did not yield incremental value over stenosis assessment for predicting events that predominantly consisted of revascularization procedures.
Clinical Trial Registration: NCT00934037.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Coronary atherosclerotic disease burden strongly correlates with patient outcome [1]. Risk of adverse events from coronary artery disease (CAD) starts to rise with the presence of mild atherosclerotic disease and gradually increases with the extent of plaque burden [1]. Our current paradigm of grading the secerity of CAD by the number and location of stenoses is an approximate assessment of CAD burden as both correlate reasonably well [2]. With the availability of noninvasive, semi-automated coronary atherosclerotic plaque burden assessment by CT coronary angiography (CTA), there is growing interest in using total disease burden as an integrating metric for CAD risk assessment [3, 4]. Coronary calcium scanning approximates total atherosclerotic disease burden but – by design – does not account for non-calcified disease. Several studies have reported good diagnostic accuracy for coronary atherosclerotic burden to identify patients with hemodynamically significant CAD, as assessed by fractional flow reserve (FFR) or myocardial stress perfusion imaging [5, 6]. However, there are scarce data on how total coronary atherosclerotic disease burden assessment by CT compares to traditional CAD evaluation for predicting patient outcome. The purpose of this study was to directly compare the short-term and intermediate-term prognostic information of total coronary atherosclerotic plaque volume by CT angiography to established metrics of CAD risk assessment.
Methods
Study design and study population
The study design of the CORE320 multicenter study has been previously detailed [7]. The CORE320 study (coronary artery evaluation using 320-row Multidetector Computed Tomography Angiography and Myocardial Perfusion) is a prospective, multicenter, multinational, diagnostic study designed to compare the accuracy of combined CTA and myocardial computed tomography perfusion imaging (CTP) against the combination of invasive coronary angiography (ICA) and single-photon emission computed tomography myocardial perfusion imaging [8]. Patients 45 to 85 years of age who were referred for clinically indicated ICA for suspected or known CAD were enrolled. Pretest probability/risk was established by the method of Morise et al. [9].
CT acquisition, image reconstruction, transfer, and analysis
A detailed description of CORE320 image acquisition and interpretation methods has been published [10]. In brief, all CT images were acquired before cardiac catheterization using a single protocol developed for a 320 × 0.5 mm-detector row CT system (Aquilion ONE, Toshiba Medical Systems, Otawara, Japan). Patient preparation included oral (75–150 mg) or IV (up to 15 mg) metoprolol and sublingual, fast-acting nitrates. Coronary calcium scanning was performed using prospective ECG triggering over a single heartbeat with a gantry rotation and x-ray exposure time of 0.35 s, 0.5-mm slice collimation, tube voltage of 120 kV, and tube current adjusted to patient body mass index. For CT angiography, 50 to 70 mL of iodinated contrast (Iopamidol 370 mg iodine/mL) was injected intravenously at 4.0–5.0 mL/s for each of the separate, axial, prospectively ECG-triggered acquisitions. For all CTA acquisitions, de-identified sinograms were reconstructed, processed, and interpreted by independent core laboratories. CT data were reconstructed to generate 0.5-mm slice thickness images with a 0.25-mm increment using both a standard (FC43) and a sharp (FC05) convolution kernel. Two level III certified investigators evaluated each CTA study for the presence and severity of CAD; disagreements were resolved by consensus. Readers examined all coronary artery segments of 1.0 mm in diameter or more for the presence of CAD using a 19-segment coronary artery model. All coronary lesions with a subjective diameter stenosis of ≥ 30% underwent quantitative evaluation on a continuous scale (0–100%) using software tools (Vitrea™ FX version 3.0 workstation, Vital Images, Minnetonka, MN, USA) at the discretion of the reader. Segment stenosis score was determined as previously described [11]. Briefly, coronary segments were scored based on the presence and severity of atherosclerotic stenoses (0–3) and scores were summed for all 19 segments (total score ranging from 0 to 57) [12]. Coronary calcium was analyzed by the Agatston method [13].
Coronary atheroma volume analysis
All reconstructed datasets were transferred to an offline workstation for quantitative coronary atheroma volume analysis using dedicated software with a semi-automated 3-dimensional (3D) contour detection algorithm (QAngio CT Research Edition version 2.0 RC4, Medis Medical Imaging Systems (MEDIS), Leiden, the Netherlands) [14,15,16]. The quantitative atheroma analysis was performed by two independent, experienced observers who were blinded to initial CTA, quantitative coronary angiography (QCA), and clinical data. On the basis of longitudinal contours, cross-sectional images at 0.5-mm intervals were obtained to create transversal lumen and vessel wall contours, using automated contour detection techniques applied to the intensity gradients in the cross sections and guided by the longitudinal contours. These cross-sectional contours were examined and, if necessary, corrected by the observer. All coronary vessels were assessed using a 19-coronary-segment model, including each epicardial vessel and side branches with at least 1.5 mm in diameter. Segments containing stents and those with poor image quality were excluded from analysis. The plaque volume was calculated by subtracting the lumen volume from the vessel volume. For each patient, the vessel, lumen, atheroma, and length values were calculated by adding all the analyzed segments. Based on prior investigations of plaque assessment, we identified percent atheroma volume as the representative metric for total coronary atherosclerotic plaque burden [6]. Percent atheroma volume (PAV) was defined as: (total atheroma volume/total vessel volume) x 100.
Invasive coronary angiography acquisition and analysis
Invasive coronary angiography was performed using standard techniques within 60 days following CTA acquisition. Quantitative coronary angiography (QCA) was performed using standard, validated analysis software (CAAS II QCA Research version 2.0.1, PIE Medical Imaging, Maastricht, The Netherlands). Coronary segments were defined using a 19-coronary-segment model, and all coronary segments 1.5 mm or more in diameter were analyzed quantitatively. Significant coronary artery stenosis (obstructive CAD) was defined as ≥ 50% diameter stenosis by QCA.
Outcome variables
Outcome variables were (1) 30-day revascularization and (2) major adverse cardiac events after 2 years follow up. Major adverse cardiac events (MACE) included cardiac death, myocardial infarction, hospitalization for acute chest pain or heart failure, arrhythmia, and late revascularization (beyond 6 months of index cardiac catheterization). Assessment of follow-up data was performed at 30 days, 6 months, 12 months, and 24 months after conventional coronary angiography. Data was obtained on office visits, telephone interviews, or mailing of a standardized questionnaire. The follow-up questionnaire assessed death, myocardial infarction, hospitalization, new or unstable angina, congestive heart failure, percutaneous intervention, and coronary artery bypass surgery. All events were adjudicated by a committee of nine cardiologists and radiologists.
Statistical analysis
Descriptive statistics of metrics were compared by Wilcoxon rank-sum test. Area under the receiver operating characteristic (ROC) curve (AUC) was used as a measure of diagnostic power. AUCs were calculated for the full group as well as the subset of patients without known CAD. Each graph includes a calibration curve (dotted line); to identify the corresponding cut point, extend a vertical line from a point on the ROC curve to the calibration curve, then a horizontal line to the right-hand ordinate, which gives the cut point. Kaplan-Meier survival curves were computed using standard methodology. All analyses were carried out in SAS 9.4 (SAS Institute, Cary, NC) and graphics were created using S-Plus 8.0 (TIBCO Spotfire, Palo Alto, ca.).
Results
Clinical characteristics
Of 391 patients included in the final CORE320 study sample, nineteen patients were excluded from this analysis because of loss to follow up or technical problems, resulting in a final study population of 372 patients. Of the 372, 86 (23%) underwent coronary artery revascularization within 30 days of invasive coronary angiography and 32 (8.6%) experienced MACE after 30 days: 20 revascularization procedures, 6 hospitalizations for chest pain, 4 myocardial infarctions, one hospitalization for heart failure and one occurrence of a new arrhythmia. Table 1 displays the clinical data and baseline characteristics for the entire study population and according to occurrence of MACE. The median age of all patients was 62 years (range 56 to 68 years): 67% were male, 33% were Asian, 11% were African-American, and 56% were Caucasian. Patients had a high prevalence of risk factors (hypertension 78%, diabetes 34%, dyslipidemia 68%, current smoker 17%, and previous percutaneous coronary intervention 30%). Patients who experienced MACE were more likely to experience angina and have high grade stenoses on coronary angiography.
Coronary artery disease evaluation
Results for the tested metrics of CAD evaluation are presented in Table 2, including a break down for subjects who experienced MACE and who did not. Notably, values for percent atheroma volume (p = 0.05), coronary artery stenosis by both CTA (p = 0.0006) and QCA (p < 0.0001), and calcium score (p = 0.051) were greater among patients with MACE compared to those without. Table 3 presents the same data after excluding patients with known CAD. The same metrics (percent atheroma volume, percent stenosis, and calcium score) showed a strong association with MACE in this context (Table 3).
Accuracy for identifying patients who required 30-day revascularization
Table 4 presents the performances of the tested metrics for identifying patients at baseline who underwent coronary artery revascularization within 30 days, including results after excluding patients with known CAD. Coronary stenosis assessment by CTA and QCA achieved greatest AUC wheras other metrics performed only modestly. Performances for all metrics improved after excluding patients with known CAD (Table 4). ROC curves are presented in Fig. 1.
Accuracy of Predicting 30-Day Revascularization. Shown are the receiver operating characteristic (ROC) curves along with their respective calibration curves for identifying patients who required coronary artery revascularization within 30 days of coronary angiography for percent atheroma volume (PAV), CT angiography (CTA), quantitative coronary angiography (QCA), coronary calcium scanning (CACS), segment stenosis score (SSS), and Clinical Risk Score by Morise. Each graph includes a calibration curve (dotted line); to identify the corresponding cut point, extend a vertical line from a point on the ROC curve to the calibration curve, then a horizontal line to the right-hand ordinate, which gives the cut point
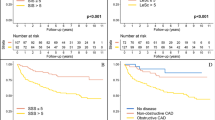
Accuracy for identifying patients who experienced MACE after 30 days
Table 5 presents the performances of the tested metrics for identifying patients at baseline who experienced MACE, including results after excluding patients with known CAD. Overall, metrics performed only modestly, particularly in patients with history of CAD. Coronary stenosis assessment by CTA and QCA achieved the greatest AUC. Performances for all metrics improved after excluding patients with known CAD, though statistically significantly only for PAV (p = 0.02). ROC curves are presented in Fig. 2.
Accuracy of Predicting MACE. Shown are the receiver operating characteristic (ROC) curves along with their respective calibration curves for identifying patients who experienced major adverse cardiovascular events (MACE) for percent atheroma volume (PAV), CT angiography (CTA), quantitative coronary angiography (QCA), coronary calcium scanning (CACS), segment stenosis score (SSS), and Clinical Risk Score by Morise. Each graph includes a calibration curve (dotted line); to identify the corresponding cut point, extend a vertical line from a point on the ROC curve to the calibration curve, then a horizontal line to the right-hand ordinate, which gives the cut point
Incremental value of metrics beyond CTA stenosis
Table 6 presents the performances of the tested metrics for identifying patients at baseline who experienced 30-day revascularization and MACE using a stepwise model to assess the incremental value of metrics beyond CTA stenosis assessment. Only QCA stenosis assement yielded statistically significant increase in diagnostic performance for both outcomes.
Discussion
We compared the effectiveness of frequently used cardiac CT metrics for predicting short and long term coronary artery revascularization and MACE. We found overall similar performance for PAV, coronary calcium scanning, and SSS while CTA and QCA stenosis assessment fared slightly better, particularly, for predicting short term revascularization. The favorable performance by both CTA and QCA stenosis assessment is not surprising given that most of the events were related to coronary artery revascularization procedures which were triggered by the degree of observed diameter stenosis. Indeed, it is remarkable that the metrics based on atherosclerotic disease burden assessment performed relatively well in this context.
The question of whether stenosis severity confers risk of adverse outcome through its association with disease burden or if there is independent risk associated with high grade stenoses has not been conclusively settled. While lesion stenosis severity at baseline is clearly associated with greater risk of subsequent revascularization, it appears less strongly linked with the risk of myocardial infarction and death [17]. The presence of coronary artery stenoses correlates with coronary atherosclerotic disease burden, which explains its strong association with patient outcome [18]. Given the strong correlation of coronary atherosclerotic disease burden and occurrence of myocardial infarction and death at follow up, it is conceivable that metrics capturing total disease volume yield an advantage over CAD evaluation—which only approximates such assessment.However, our data did not allow to confirm this hypothesis because of the few observed events of myocardial infarction or death.
All metrics performed better after excluding patients with known CAD which is of clinical significance since cardiac CT is predominantly used in patients without prior CAD history. The reason for the rather modest predictive value in patients with history of CAD remains speculative at this time. It is likely that the more homogeneous group of high-risk individuals allows less risk discrimination.
While PAV did not perform superiorly to standard stenosis evaluation by CTA or QCA, a semi-automated assessment of plaque burden provides conceptual advantages over categorical determination of disease presence, including the reduction of observer bias. While not tested in this study, historical data suggest greater reproducibility of plaque volume analysis compared to user depedent stenosis evaluation [19, 20].
We noted with interest that coronary calcium scanning performed less well than standard stenosis assessment and also trended inferiorly to total atherosclerotic disease burden evaluation in our study. In the CONFIRM registry, stenosis assessment by CTA provided incremental risk prediction over calcium scanning in symptomatic but not in most low risk patients [21, 22]. It is likely that the performance of calcium scanning was affected by the predominance of coronary revascularization among outcome measures. On the other hand, evaluation of total atherosclerotic disease burden by PAV still performed well, which may indicate that assessment of noncalcified coronary artery disease is relevant in the context of testing intermediate-high risk populations.
Limitations
We acknowledge several study limitations. First, the CORE320 study was not designed to address the present particular research question and thus we may not have had sufficient statistical power to conclusively demonstrate differences between groups. As power calculations would not be appropriate as a post hoc measure, we provide 95% confidence intervals for our analyses. Second, the CORE320 study population contains patients who are at higher risk than typically seen with the application of CTA. Thus, results may not be applicable to low risk populations. Third, prospectively total atheroma assessment was limited to non-stented segments. Fourth, the contour detection algorithm was upgraded and improved since our analysis and thus its current performance may exceed that of our study. It is conceivable that further software upgrades may allow including smaller segments and stented lesions and perform better with poor image quality or extensive calcification. Lastly, it should be noted that the contour detection software is for research purposes only at this time and not yet validated for clinical use.
Conclusions
Coronary atherosclerosis and stenosis assessment by CTA and QCA predict only modestly well major adverse cardiac events, consistent of predominantly revascularization procedures, in high risk patients presenting with stable symptoms. Predictive performance increases after excluding patients with prior coronary heart disease history. Stenosis assessment by CTA and QCA performed marginally better than atherosclerotic plaque burden evaluation for predicting revascularization procedures.
Availabilityof data and material
Data belongs to the sponsor and may be provided on request at the discretion of the sponsor.
References
Arbab-Zadeh A, Fuster V (2016) The risk continuum of atherosclerosis and its implications for defining CHD by coronary angiography. J Am Coll Cardiol 68:2467–2478
Nakagomi A, Celermajer DS, Lumley T, Freedman SB (1996) Angiographic severity of coronary narrowing is a surrogate marker for the extent of coronary atherosclerosis. Am J Cardiol 78:516–519
Kalra DK, Heo R, Valenti V, Nakazato R, Min JK (2014) Role of computed tomography for diagnosis and risk stratification of patients with suspected or known coronary artery disease. Arterioscler Thromb Vasc Biol 34:1144–1154
Boogers MJ, Broersen A, van Velzen JE et al (2012) Automated quantification of coronary plaque with computed tomography: comparison with intravascular ultrasound using a dedicated registration algorithm for fusion-based quantification. Eur Heart J 33:1007–1016
Nakazato R, Shalev A, Doh JH et al (2013) Aggregate plaque volume by coronary computed tomography angiography is superior and incremental to luminal narrowing for diagnosis of ischemic lesions of intermediate stenosis severity. J Am Coll Cardiol 62:460–467
Kishi S, Magalhaes TA, Cerci RJ et al (2016) Total coronary atherosclerotic plaque burden assessment by CT angiography for detecting obstructive coronary artery disease associated with myocardial perfusion abnormalities. J Cardiovasc Comput Tomogr 10:121–127
Vavere AL, Simon GG, George RT et al (2011) Diagnostic performance of combined noninvasive coronary angiography and myocardial perfusion imaging using 320 row detector computed tomography: design and implementation of the CORE320 multicenter, multinational diagnostic study. J Cardiovasc Comput Tomogr 5:370–381
Rochitte CE, George RT, Chen MY et al (2014) Computed tomography angiography and perfusion to assess coronary artery stenosis causing perfusion defects by single photon emission computed tomography: the CORE320 study. Eur Heart J 35:1120–1130
Morise AP, Haddad WJ, Beckner D (1997) Development and validation of a clinical score to estimate the probability of coronary artery disease in men and women presenting with suspected coronary disease. Am J Med 102:350–356
George RT, Arbab-Zadeh A, Cerci RJ et al (2011) Diagnostic performance of combined noninvasive coronary angiography and myocardial perfusion imaging using 320-MDCT: the CT angiography and perfusion methods of the CORE320 multicenter multinational diagnostic study. AJR Am J Roentgenol 197:829–837
Min JK, Shaw LJ, Devereux RB et al (2007) Prognostic value of multidetector coronary computed tomographic angiography for prediction of all-cause mortality. J Am Coll Cardiol 50:1161–1170
Miller JM, Dewey M, Vavere AL et al (2009) Coronary CT angiography using 64 detector rows: methods and design of the multi-centre trial CORE-64. Eur Radiol 19:816–828
Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R (1990) Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 15:827–832
de Graaf MA, Broersen A, Kitslaar PH et al (2013) Automatic quantification and characterization of coronary atherosclerosis with computed tomography coronary angiography: cross-correlation with intravascular ultrasound virtual histology. Int J Cardiovasc Imaging 29:1177–1190
Boogers MJ, Schuijf JD, Kitslaar PH et al (2010) Automated quantification of stenosis severity on 64-slice CT: a comparison with quantitative coronary angiography. JACC Cardiovasc Imaging 3:699–709
de Graaf MA, Broersen A, Ahmed W et al (2014) Feasibility of an automated quantitative computed tomography angiography-derived risk score for risk stratification of patients with suspected coronary artery disease. Am J Cardiol 113:1947–1955
Chang HJ, Lin FY, Lee SE et al (2018) Coronary atherosclerotic precursors of acute coronary syndromes. J Am Coll Cardiol 71:2511–2522
Arbab-Zadeh A, Fuster V (2015) The myth of the vulnerable plaque - transitioning from a focus on individual lesions to atherosclerotic disease burden for coronary artery disease risk assessment. J Am Coll Cardiol JACC 65:846–855
Herzog C, Kerl JM, De Rosa S et al (2013) Influence of observer experience and training on proficiency in coronary CT angiography interpretation. Eur J Radiol 82:1240–1247
Papadopoulou SL, Garcia-Garcia H, Rossi A et al (2013) Reproducibility of computed tomography angiography data analysis using semiautomated plaque quantification software: implications for the design of longitudinal studies. Int J Cardiovasc Imaging 29:1095–1104
Cho I, Chang HJ, Sung JM et al (2012) Coronary computed tomographic angiography and risk of all-cause mortality and nonfatal myocardial infarction in subjects without chest pain syndrome from the CONFIRM registry (coronary CT angiography evaluation for clinical outcomes: an international multicenter registry). Circulation 126:304–313
Al-Mallah MH, Qureshi W, Lin FY et al (2014) Does coronary CT angiography improve risk stratification over coronary calcium scoring in symptomatic patients with suspected coronary artery disease? Results from the prospective multicenter international CONFIRM registry. Eur Heart J Cardiovasc Imaging 15:267–274
Funding
The sponsor of the CORE320 study, Canon (formerly Toshiba) Medical Systems Corporation, was not involved during any stage of the planning, design, data acquisition, data analysis, or manuscript preparation of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. J.H.C. Reiber has a part-time appointment as Professor of Medical Imaging at the Leiden University Medical Center (LUMC) and is the CEO of Medis medical imaging systems, Leiden, the Netherlands. Dr. P. Kitslaar has a research appointment at the LUMC, Division of Image Processing (LKEB), Department of Radiology and is an employee of Medis, Leiden, the Netherlands. Drs. F. Rybicki and A. Arbab-Zadeh disclose their membership of the CORE320 steering committee. The CORE320 study was sponsored by Canon (formerlyToshiba) Medical Systems. Dr. George and Mrs. Vavere have joined AstraZeneca as employees since completion of this research but disclose no conflicts to this topic.
Ethical approval
Approval for all research activities were obtained from local and central institutional review boards.
Informed consent
All patients signed written consent to participate. Permission was obtained to publish the presented data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kishi, S., Magalhães, T.A., Cerci, R.J. et al. Comparative effectiveness of coronary artery stenosis and atherosclerotic plaque burden assessment for predicting 30-day revascularization and 2-year major adverse cardiac events. Int J Cardiovasc Imaging 36, 2365–2375 (2020). https://doi.org/10.1007/s10554-020-01851-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-020-01851-3