Abstract
One of the foundations of the management of patients with suspected coronary artery disease (CAD) is to avoid unnecessary invasive coronary angiography (ICA) referrals. However, the diagnostic yield of ICA following abnormal conventional stress testing is low. The ability of ischemia testing to predict subsequent myocardial infarction and death is currently being challenged, and more than half of cardiac events among stable patients with suspected CAD occur in those with normal functional tests. The optimal management of patients with stable CAD remains controversial and ischemia-driven interventions, though improving anginal symptoms, have failed to reduce the risk of hard cardiovascular events. In this context, there is an ongoing debate whether the initial diagnostic test among patients with stable suspected CAD should be a functional test or coronary computed tomography angiography. Aside from considering the specific characteristics of individual patients and local availability and conditions, the choice of the initial test relates to whether the objective concerns its role as gatekeeper for ICA, prognosis, or treatment decision-making. Therefore, the aim of this review is to provide a contemporary overview of these issues and discuss the emerging role of CCTA as the upfront imaging tool for most patients with suspected CAD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Functional stress tests have been the imaging cornerstone for the assessment of patients with suspected obstructive coronary artery disease (CAD) for several decades. Nonetheless, the diagnostic yield of invasive coronary angiography (ICA) following abnormal conventional stress testing is low, with only about 40% patients showing obstructive CAD, compared to an approximate 70% of obstructive findings among patients referred from coronary computed tomography angiography (CCTA) [1, 2]. Such a suboptimal yield of ICA, derived from inaccurate risk stratification, or on occasions from misleading functional tests, affects one of the foundations of the management of patients with suspected CAD, which is to contain the number of unnecessary ICA referrals (patients without obstructive CAD who undergo ICA). The suboptimal performance of traditional functional cardiac imaging might also be attributed to the discordance between ischemia and stenosis highlighted by several clinical studies [3, 4]. Besides, the ability of ischemia testing to predict subsequent myocardial infarction (MI) and death is currently being challenged in light of recent studies that will be discussed below.
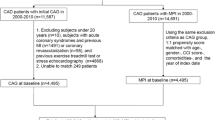
There is an ongoing debate whether the initial diagnostic test among patients with new onset stable chest pain should be a functional test or CCTA [5]. In this regard, aside from considering the specific characteristics of individual patients such as their clinical likelihood of CAD, ECG interpretability and exercise capacity (Fig. 1), a number of questions arise related to the objective of the initial test: (1) Is it the aim of the test to rule out obstructive CAD (gatekeeper role)?; (2) Is it the purpose to predict the clinical outcome (prognostic role)?; and/or (3) Is it the search for a tool that offers a more rational assessment of the potential benefits and risks of revascularization (decision-making)?. Therefore, the aim this review is to provide a contemporary overview of these issues and discuss the emerging role of CCTA as the upfront imaging tool for most patients with suspected CAD.
Diagnostic yield and prognostic value of functional vs. anatomic testing in stable patients
A large number of studies using stress-echocardiography, stress-single photon emission computed tomography (SPECT), and stress-cardiac magnetic resonance (CMR) have demonstrated the relationship between the magnitude of myocardial ischemia and major adverse cardiac events (MACE) [6,7,8,9]. In this context, the number of ordered cardiac stress tests has steadily increased in the past decades, with almost 4 million tests performed annually in the United States, a figure expected to increase given the aging population [10]. However, there is a significant decline in the number of tests that are positive for myocardial ischemia in contemporary clinical practice (< 10%) [11, 12]. Likewise, the prevalence of moderate to severe ischemia in SPECT studies has also experienced a major decline, from 20.6% in 1991 to 4.6% in 2009 [11]. Such reduction in the frequency and severity of myocardial ischemia, aside from lower threshold or higher accessibility (resulting in lower risk patients undergoing testing), can be partly attributed to the reduction in the risk factor burden and in the increasing use of statins and beta-blockers, which parallels the significant decline in the rates of MI and cardiac death in the US [13]. Furthermore, the evidence indicating that noninvasive cardiac imaging promotes a significant reduction in the risk of MI or death is conflicting [14, 15].
Regarding the diagnostic yield of non-invasive testing, in a very large registry including 661,063 patients undergoing elective catheterization, the diagnostic yield of ICA for the prediction of obstructive CAD was below 50% [1]. Indeed, among patients with a positive stress test, only 41% showed obstructive CAD, and even among patients with typical anginal symptoms and positive stress tests the diagnostic yield of ICA was below 55% [16]. Notwithstanding, it should be acknowledged though that such registry excluded a large number of patients who entered the National Cardiovascular Data Registry (NCDR) CathPCI Registry such as those with known CAD and sites without diagnostic catheterization results. In addition, the definition of non-invasive tests (NIT) as low, intermediate, and high risk was left to each site interpretation; and such risk stratification is not fully comparable between NITs. Likewise, the fact that they used a low threshold for detecting obstructive CAD (diameter stenosis ≥ 50%) might lead to further discrepancies. Also, almost 60% of the patients were asymptomatic or had atypical symptoms.
The PROMISE (PROspective Multicenter Imaging Study for Evaluation of chest pain), SCOT-HEART (Scottish COmputed Tomography of the HEART), and ISCHEMIA (International Study of Comparative Health Effectiveness With Medical and Invasive Approaches) randomized trials have provided insightful data in this regard. The PROMISE and SCOT-HEART trials compared clinical outcomes of the management of stable symptomatic patients with CCTA (anatomy) vs. standard of care (functional). The PROMISE trial randomized 10,003 symptomatic patients to a strategy of initial anatomical testing with CCTA or functional testing. Although demonstrating similar clinical outcomes compared to standard of care (SOC), CCTA enabled a significantly better diagnostic yield of ICA, by leading to more ICA but with significantly lower rates of non-significant lesions [17].
In an insightful sub-analysis of the PROMISE trial, Hoffmann et al. reported that CCTA provides better prognostic information than functional testing. Furthermore, when findings were stratified into mildly, moderately, or severely abnormal (Fig. 2), CCTA showed a risk continuum compared to a normal test [mild HR 2.94 (95% CI 1.64–5.26); moderate HR 7.67 (95% CI 3.83–15.37); and severe HR 10.13 (95% CI 5.15–19.92), respectively], whereas functional testing did not [mild HR 0.94 (95% CI 0.47–1.89); moderate HR 2.65 (1.46–4.83); and severe HR 3.88 (2.58–5.85)], respectively [18]. Moreover, in terms of prediction of hard events, even mildly abnormal CT exams were associated with death or MI [HR 2.73 (95% CI 1.20–6.25), p = 0.0170], whereas only severely abnormal functional tests were associated with these hard endpoints [HR 2.13 (95% CI 1.16–3.91), p = 0.0141]. It is noteworthy that such risk continuum provided by CCTA was achieved using a categorical approach considering only lesion severity, disregarding plaque characteristics with prognostic relevance that are included within specific scoring systems such as the CT Leaman score and the Leiden CT risk score.
Graphical representation of the estimated prevalence and annual rate of hard events according to the presence of normal, and mildly, moderately, and severely abnormal functional and anatomic (CCTA) tests in patients with suspected CAD [18]. *Although not clearly established, criteria for moderate-severe ischemia is generally defined as ≥ 10% ischemic myocardium at stress-SPECT, ≥ 3/16 newly dysfunctional segments at stress-echo, or ≥ 2/16 ischemic defects at perfusion CMR or ≥ 3/16 newly dysfunctional segments at dobutamine stress-CMR [94]
The SCOT-HEART trial included 4146 patients and demonstrated that using CCTA in addition to SOC in patients with stable chest pain resulted in a significantly lower rate of hard events (death from CHD or non-fatal MI) after a follow-up of 5 years compared to SOC alone. Of note, such gain did not result in significantly higher rates of ICA or revascularization, and was mostly attributed to the ability of CCTA to improve targeting of preventive (statin and antiplatelet) therapies [19, 20]. In keeping with this, a very large (n = 86705) Danish registry demonstrated that among patients with suspected CAD, initial evaluation with CCTA was associated with a 30% lower risk of myocardial infarction (MI) compared to patients who underwent initial functional testing [21]. Moreover, a recent meta-analysis including randomized CCTA trials showed that among patients with suspected CAD, CCTA was associated with a 30% reduction in the incidence of MI compared to functional stress imaging, CCTA patients were more likely to undergo ICA and revascularization than those evaluated with functional testing [22]. Taken all together, CCTA appears as the more effective first choice in this clinical scenario.
Accordingly, there is supportive evidence that compared to functional assessment CCTA is a more effective gatekeeper to ICA, providing improved clinical outcome including unsurpassed negative predictive value, and offering a risk continuum for hard cardiac events (Fig. 2), as well as enabling enhanced lifestyle modifications, eligibility, and adherence to statin therapy and aspirin [20, 22,23,24,25,26,27]. In terms of its economic impact, though this issue deserves specific and much more detailed analysis. According to the PROMISE data (US centers) CCTA and functional testing have similar costs at 3 years of follow-up. In contrast, European studies suggest that CCTA might be a more cost-effective strategy [28, 29]. Furthermore, in the recent multinational mostly Asian CONSERVE (Coronary Computed Tomographic Angiography for Selective Cardiac Catheterization) study the cumulative diagnostic test costs were 57% lower among patients randomized to selective (using CCTA as gatekeeper) ICA referral compared to those with direct ICA [2].
As a consequence of the above, the recent National Institute for Health and Care Excellences (NICE) clinical guideline recommended CCTA as the first-line investigation for patients with stable chest pain [30]. The recently released 2019 ESC guidelines for the diagnosis and management of chronic coronary syndromes recommend (class I) the use of either noninvasive functional imaging (particularly among patients with intermediate to high likelihood of CAD) or anatomical imaging using CCTA (particularly among those with low to intermediate likelihood of CAD) as the initial test for diagnosing CAD [31].
Targeting cause or effect: implications for evaluation and treatment
Until recently, the clinical relevance of myocardial ischemia was unchallenged, and most clinical decisions were closely related to the presence, extent, and distribution of inducible ischemia. Indeed, stress-induced ischemia is broadly used as a surrogate of the risk of MACE in patients with suspected and established stable CAD, and generally promotes and expedites the use of myocardial revascularization even in asymptomatic patients [32, 33]. However, the association between myocardial ischemia and CV events, though still under debate given the results of the ISCHEMIA trial, does not imply cause-effect [34]. The fundamentals of such uncertain association rely on different backbone concepts, summarized as follows. To begin with, almost 70% of acute thrombotic events arise from angiographically mild lesions and approximately half of acute MI occur in patients with no history of previous symptoms [35,36,37,38]. Indeed, several studies have documented the presence of high risk plaques as well as plaque rupture outside the culprit lesions as a relatively common finding in both stable and unstable patients [39,40,41,42]. In keeping with this, in the PROSPECT study (Prospective natural-history study of coronary atherosclerosis), half of the subsequent major coronary events were related to non-culprit lesions (with a mean baseline diameter stenosis of 32%), although it is worth mentioning that most of those events were rehospitalization for unstable angina [43]. On the other hand, among stable patients, 57% of cardiac events in the PROMISE trial occurred in patients with normal functional tests [18, 43]. Moreover, in the international CLARIFY (Prospective Observational Longitudinal Registry of Patients With Stable Coronary Artery Disease) registry, of the 469 hard events (CV death or MI), 58% occurred in patients without angina or ischemia [44]. Accordingly, it is difficult to relate ischemia with events.
In parallel, and as a consequence of the above, the optimal management of patients with stable CAD remains controversial, with imaging subanalysis of several trials such as COURAGE (Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation trial), BARI 2D (Bypass Angioplasty Revascularization Investigation 2 Diabetes), and FAME 2 (Fractional Flow Reserve Versus Angiography for Multivessel Evaluation 2) showing lack of benefit of revascularization in terms of reduction of MI or death compared with optimal medical therapy (OMT) [45,46,47]. Indeed, in the FAME 2 study, 16% of patients with normal fractional flow reserve (FFR > 0.80) had subsequent MACE [48]. Furthermore, in the recently published 10-year follow-up of the MASS II randomized trial, the presence of baseline myocardial ischemia was not identified as a predictor of MACE or of changes in left ventricular systolic function among patients with multiple vessel CAD [49]. In the aforementioned CLARIFY registry, that included 32,105 patients with stable CAD, anginal symptoms (with or without demonstration of ischemia) but not ischemia were related to death or MI [44]. Moreover, almost 60% of such events occurred in patients with neither angina nor ischemia, compared to 12% among patients with ischemia, 12% among those with angina alone, and 17% with both. These results are in keeping with the findings of the COURAGE study, where baseline ischemia did not predict events while anatomic extension and severity did [50]. Notwithstanding, none of the aforementioned studies were designed to compare outcomes between revascularization and OMT according to the extent of ischemia.
In turn, the ISCHEMIA trial was the first randomized comparison of a noninvasive ischemia-guided revascularization strategy (invasive vs. conservative) in patients with stable CAD. Of note, ischemia was severe in 54% of patients, moderate in 33%, and mild in only 12% of patients. The trial randomized 5,179 patients to ICA (followed by revascularization if needed) on top of OMT, or to an initial conservative strategy of OMT alone. After a median follow-up of 3.3 years, no differences were found between strategies both regarding the primary endpoint of death, MI, hospitalization for unstable angina, heart failure or resuscitated cardiac arrest [13.3% in the invasive group vs. 15.5% in the OMT group (adjusted HR 0.93; 95% CI 0.80–1.08)]; or to cardiovascular death or MI [11.7% in the invasive group vs. 13.9% in the conservative group (HR 0.90; 95% CI 0.77–1.06] [34]. This long awaited trial was conceived from the uncertainties raised by the COURAGE trial over a decade ago, reporting no benefit of revascularization over OMT in stable CAD. One of the main criticisms of the COURAGE trial, beyond the fact that it included a relatively low ischemic burden, was the outdated stent technology and the many exclusions following the initial angiogram. In contrast, the ISCHEMIA trial used state-of-the-art OMT and revascularization strategies. Also, randomization was performed without an initial ICA.
Will ischemia-driven intervention remain the cornerstone of CAD management?
Although myocardial ischemia has been the foundation of decision-making in patients with suspected CAD for several decades, the demonstration of improved clinical outcomes by means of revascularization, yet currently under debate after the ISCHEMIA trial, has only been observed in patients with large ischemic burden (more than 10% of ischemic myocardium) [51, 52]. As a matter of fact, in the COURAGE nuclear substudy, although a significant reduction of the ischemic burden lead to reduced unadjusted rates of death or MI, adjusted differences (controlling for randomized –revascularization-treatment) were comparable [53]. What might be more relevant, a post hoc analysis including SPECT and quantitative ICA identified anatomic but not ischemic burden as a predictor of death, MI, and non-ST elevation acute coronary syndromes [50].
Furthermore, in a study including 549,078 patients with suspected ischemia across 224 hospitals, centers with the higher rates of noninvasive cardiac imaging were not associated with a decrease in readmission rates for acute MI despite higher rates of ICA [15]. Finally, in a meta-analysis including 5 randomized studies evaluating PCI and OMT vs. OMT alone for stable CAD with documented ischemia, PCI was not associated with reductions in death or MI compared with OMT alone [54].
Overall, ischemia-driven interventions, though improving anginal symptoms, have failed to reduce the risk of hard cardiovascular events, thus disputing the role of ischemia as an optimal surrogate of CV risk and as a therapeutic target in stable syndromes. In contrast, statins, and more recently novel anti-inflammatory drugs and icosapent ethyl have shown a significant impact in the rates of death and MI [55,56,57,58]. Such divergent impact of ischemia-driven vs. atherosclerosis-driven interventions can be at least in part explained by understanding that the former approach targets only the later stages of the actual underlying process. However, the pathophysiology of anginal symptoms is likely more complex, and the degree of focal stenosis represents only one of multiple contributors. This concept was supported by the aforementioned CLARIFY registry, where anginal symptoms overruled ischemia as a predictor of hard events [44].
Accordingly, we are likely at the dawn of a new era, that comprises the convergence of three related developments that will shape our management of CAD in the years to come: (1) the unsatisfactory performance of functional tests as gatekeepers of ICA; (2) Degradation of the prognostic value of myocardial ischemia compared to anatomy relevant for clinical decision-making; and (3) Equipoise between PCI and an initial conservative strategy among most patients with stable CAD in terms of MACE and survival [59].
Ischemic burden or anatomic burden: Why not both?
There are several additional advantages of CCTA over functional tests as the initial strategy for most patients with suspected or established CAD. First, the identification of complete absence of coronary atherosclerosis (Fig. 3) provides an unsurpassed negative prognostic value, enabling an at least 5-year long safety window, with an annualized rate of events lower than 0.25% [60,61,62]. This is a critical discriminating aspect between anatomic and functional testing (Fig. 2), since patients with extensive but non-obstructive disease have a higher risk of events independent of the ischemic burden and clinical features [50]. Additionally, the presence of any plaque, even mild, is associated with all-cause mortality [63, 64]. Secondly, CCTA enables the identification of the presence, extent, and type of plaque (high-risk plaque characteristics, including: positive remodeling, low-attenuation, plaque burden > 70%, napkin-ring sign, and spotty calcification; Table 1), and the spatial distribution of nonobstructive plaque (Fig. 4) [65]. Such portrayal of the atherosclerotic burden has major prognostic implications that has gained clinical relevance in the past few years with the demonstration, as mentioned above, that patients with extensive but nonobstructive disease bear a similar prognosis than those with obstructive but not extensive disease [63, 64, 66,67,68,69]. Third, and of immediate clinical relevance, CCTA allows ruling out left main disease (Fig. 5), a high-risk subset of patients found in 5% of the ISCHEMIA trial population, in whom revascularization (regardless of the ischemic burden) is regarded lifesaving [70].
Fifty-two year-old female, with hypertension. She had two episodes of typical chest pain associated with palpitations, with normal ECG and enzyme levels. She underwent a stress-echocardiogram, showing inferior-wall ischemia. CCTA demonstrated absence of calcifications and normal LAD (a) and LCX (b) arteries. The RCA (c) showed two non-significant lesions at the mid portion (white asterisk, and d) and at the distal/posterolateral branch ostia (yellow asterisk, and panel e). Albeit mild, both lesions had high-risk characteristics including positive remodeling, a low attenuation core, and napkin-ring sign; as portrayed in cross-sectional views (d and e)
Seventy-eight year-old male, with obesity (body mass index 31 kg/m2). He has anginal chest pain and dyspnea. He underwent a rest-stress myocardial perfusion imaging SPECT (90% maximum heart rate, 7 METS), showing normal relative myocardial perfusion (a), preserved post-stress left ventricular function (b) and absence of ST-T changes (c); although ventricular premature beats and non-limiting chest pain were documented at maximal stress. Given the discordant results between SPECT images and the symptom referred by the patient during the treadmill test, an anatomic evaluation was recommended. CCTA revealed complex multi-vessel disease, including severe stenoses of the LMCA (arrows in panels d and e), proximal LAD (d) *, and distal RCA (asterisks in f), including a bifurcation lesion with significant positive remodeling (f, white asterisk). The LCX had moderate proximal stenosis (e, *)
In other words, if a stress test shows moderate or severe ischemia one would certainly want to rule out left main disease. Fourth, CCTA has the advantage of identifying alternative causes of exertional and non-exertional chest discomfort such as coronary anomalies (including fistulae), pericardial, aortic, valve, and pulmonary disease, or a hiatal hernia. In this regard, the presence of exertional angina and nonobstructive CAD (INOCA) may have other underlying mechanisms such as microvascular dysfunction or coronary spasm that cannot be defined by CCTA and deserve advanced functional imaging or, in some instances, invasive techniques. In addition, the CT scan allows for the measurement of epicardial fat and the detection of occult (subendocardial) myocardial infarcts, both with independent prognostic value [71,72,73,74].
Nonetheless, despite its very high sensitivity and negative predictive value, CCTA has a relatively lower specificity, particularly in the presence of diffuse calcification. Stress myocardial CT perfusion (CTP) has emerged as a possible solution in this regard, and several studies have demonstrated that CTP might offer a significant incremental value over CCTA, though it demands an additional acquisition thus substantially higher radiation and contrast dose [75, 76]. In contrast, the non-invasive assessment of FFR through computational fluid dynamics obtained from conventional CCTA datasets (FFR-CT, Fig. 6), enables the assessment of the hemodynamic significance of coronary lesions from the same CT angiogram. A number of multicenter clinical studies have demonstrated that FFR-CT provides incremental value over CCTA, particularly by increasing the specificity and reducing the number of unnecessary referrals to ICA [77,78,79,80]. Indeed, in two recent head-to-head comparison studies, the accuracy of FFR-CT was at least comparable to functional tests for the assessment of the hemodynamic significance of lesions [76, 81]. In addition, computational fluid dynamics applied to CT angiograms can elucidate the mechanical forces onto individual plaques, including endothelial shear stress and axial plaque stress, which are associated with adverse outcome (Fig. 6) [82]. Non-invasive assessment of the hemodynamic stress on plaques may identify lesion-specific precursor of an acute coronary event, and improve the modest positive predictive value (< 20%) of the currently available high-risk (anatomic) plaque characteristics [43, 69, 83]. In this regard, the recently published EMERALD (Exploring the Mechanism of plaque Rupture in Acute coronary syndrome using coronary CT Angiography and computationaL fluid Dynamics) trial demonstrated improved identification of culprit lesions of future acute coronary syndromes through the integration of anatomic (including lesion severity and length, and adverse plaque characteristics) and non-invasive hemodynamic parameters (ΔFFR-CT, wall shear stress, and axial plaque stress) [84]. Hence, CCTA (with selective FFR-CT) has the potential for comprehensive and integral evaluation of the anatomic burden, tissue composition, spatial distribution, and hemodynamic impact both on a patient and lesion-specific basis, within a single exam and without the need of additional contrast, radiation, or vasodilatory stress agents [65].
Seventy-two year-old female, with hypercholesterolemia and atypical chest pain. She underwent stress-SPECT, showing normal myocardial perfusion and unspecific ST-T changes. CCTA showed mild calcification of the proximal left anterior descending (LAD) artery, and a moderate non-calcified lesion at the mid LAD (a) *. The left circumflex and right coronary arteries were normal. Non-invasive computational flow dynamics analyses were performed to rule out lesion-specific ischemia, displaying a normal FFR (b) but adverse hemodynamic characteristics including high wall shear stress (≥ 154.7 dyn/cm2, c) and axial plaque stress (≥ 1606.6 dyn/cm2, d)
Final considerations and future perspectives
It should be emphasized that the decision for the initial diagnostic strategy depends of many factors (Fig. 1), as well as regional or institutional conditions that determine the preferred initial diagnostic test for patients with suspected or new-onset stable CAD. Indeed, the selection of the initial diagnostic test remains closely linked to individual patient characteristics, and in some situations a simple exercise ECG may be sufficient to guide patient management [85].
The role of coronary artery calcium score (CACS) among symptomatic patients with suspected CAD also merits consideration as it might potentially act as a gatekeeper for functional tests, or refine risk stratification particularly among patients with mildly abnormal or equivocal functional tests. In this regard, a number of studies have shown that the absence of calcifications (CACS 0) among symptomatic patients with low to intermediate pre-test likelihood of CAD, which is found in approximately half of these patients, is related to very low rates of obstructive CAD (< 4%) and of MACE (annual rate ~ < 0.5%) [86,87,88,89] [90].
As for the future perspectives, there are emerging approaches to plan revascularization strategies without the use of ICA. The CT-SYNTAX score, which may be calculated automatically using machine learning algorithms in the near future, offers information regarding the extent, location, length, calcification degree, and tortuosity of lesions, among other features, aiding the selection of the revascularization strategy and providing additional prognostic value in patients with complex CAD [91, 92]. This was recently shown in the SYNTAX III Revolution trial, a randomized multinational trial where in patients with complex or extensive CAD, treatment decision-making based on CCTA was found to be similar to the decision derived from conventional ICA, with a 93% agreement in the decision-making and planning [93].
Overall, in view of the better diagnostic performance and prognostic value, an (at least) similar economic burden at follow-up, the promotion of a more rational use of ICA, the aforementioned relevant additional characteristics provided (Table 1) including ruling out left main disease, and the possibility of evaluating lesion-specific ischemia from the same scan; we believe that CCTA might become frontline, comprehensive imaging tool for the majority of patients with suspected CAD.
References
Patel MR, Dai D, Hernandez AF et al (2014) Prevalence and predictors of nonobstructive coronary artery disease identified with coronary angiography in contemporary clinical practice. Am Heart J 167(6):846–852
Chang HJ, Lin FY, Gebow D et al (2019) Selective referral using CCTA versus direct referral for individuals referred to invasive coronary angiography for suspected CAD: a randomized, controlled Open-Label Trial. JACC Cardiovasc Imaging 12(7 Pt 2):1303–1312
Park SJ, Kang SJ, Ahn JM et al (2012) Visual-functional mismatch between coronary angiography and fractional flow reserve. JACC Cardiovasc Interv 5(10):1029–1036
Park HB, Heo R, OH B et al (2015) Atherosclerotic plaque characteristics by CT angiography identify coronary lesions that cause ischemia: a direct comparison to fractional flow reserve. JACC Cardiovasc Imaging 8(1):1–10
Saraste A, Barbato E, Capodanno D et al (2019) Imaging in ESC clinical guidelines: chronic coronary syndromes. Eur Heart J Cardiovasc Imaging 20(11):1187–1197
Wang EY, Dixson J, Schiller NB, Whooley MA (2017) Causes and predictors of death in patients with coronary heart disease (from the Heart and soul study). Am J Cardiol 119(1):27–34
Hachamovitch R, Berman DS, Shaw LJ et al (1998) Incremental prognostic value of myocardial perfusion single photon emission computed tomography for the prediction of cardiac death: differential stratification for risk of cardiac death and myocardial infarction. Circulation 97(6):535–543
Kral BG, Becker DM, Vaidya D, Yanek LR, Becker LC (2012) Severity of inducible myocardial ischemia predicts incident acute coronary syndromes in asymptomatic individuals with a family history of premature coronary artery disease. J Nucl Cardiol 19(1):28–36
Lipinski MJ, McVey CM, Berger JS, Kramer CM, Salerno M (2013) Prognostic value of stress cardiac magnetic resonance imaging in patients with known or suspected coronary artery disease: a systematic review and meta-analysis. J Am Coll Cardiol 62(9):826–838
Ladapo JA, Blecker S, Douglas PS (2014) Physician decision making and trends in the use of cardiac stress testing in the United States: an analysis of repeated cross-sectional data. Ann Intern Med 161(7):482–490
Rozanski A, Gransar H, Hayes SW et al (2013) Temporal trends in the frequency of inducible myocardial ischemia during cardiac stress testing: 1991 to 2009. J Am Coll Cardiol 61(10):1054–1065
Barbieri A, Mantovani F, Bursi F et al (2018) 12-year temporal trend in referral pattern and test results of stress echocardiography in a tertiary care referral center with moderate volume activities and cath-lab facility. J Cardiovasc Echogr 28(1):32–38
Benjamin EJ, Muntner P, Alonso A et al (2019) Heart disease and stroke statistics-2019 update: a report from the American heart association. Circulation 139(10):e56–e528
Shah BR, McCoy LA, Federspiel JJ et al (2013) Use of stress testing and diagnostic catheterization after coronary stenting: association of site-level patterns with patient characteristics and outcomes in 247,052 Medicare beneficiaries. J Am Coll Cardiol 62(5):439–446
Safavi KC, Li SX, Dharmarajan K et al (2014) Hospital variation in the use of noninvasive cardiac imaging and its association with downstream testing, interventions, and outcomes. JAMA Intern Med 174(4):546–553
Patel MR, Peterson ED, Dai D et al (2010) Low diagnostic yield of elective coronary angiography. New Engl J Med 362(10):886–895
Douglas PS, Hoffmann U, Patel MR et al (2015) Outcomes of anatomical versus functional testing for coronary artery disease. New Engl J Med 372(14):1291–1300
Hoffmann U, Ferencik M, Udelson JE et al (2017) Prognostic value of noninvasive cardiovascular testing in patients with stable chest pain: insights from the promise trial (prospective multicenter imaging study for evaluation of chest pain). Circulation 135(24):2320–2332
Investigators S-H, Newby DE, Adamson PD et al (2018) Coronary CT angiography and 5-year risk of myocardial infarction. New Engl J Med 379(10):924–933
Adamson PD, Williams MC, Dweck MR et al (2019) Guiding therapy by coronary CT angiography improves outcomes in patients with stable chest pain. J Am Coll Cardiol 74(16):2058–2070
Jorgensen ME, Andersson C, Norgaard BL et al (2017) Functional testing or coronary computed tomography angiography in patients with stable coronary artery disease. J Am Coll Cardiol 69(14):1761–1770
Foy AJ, Dhruva SS, Peterson B, Mandrola JM, Morgan DJ, Redberg RF (2017) Coronary computed tomography angiography vs functional stress testing for patients with suspected coronary artery disease: a systematic review and meta-analysis. JAMA Intern Med 177(11):1623–1631
Nasir K, Bittencourt MS, Blaha MJ et al (2015) Implications of coronary artery calcium testing among statin candidates according to american college of Cardiology/American Heart Association Cholesterol Management Guidelines: MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol 66(15):1657–1668
Martin SS, Blaha MJ, Blankstein R et al (2014) Dyslipidemia, coronary artery calcium, and incident atherosclerotic cardiovascular disease: implications for statin therapy from the multi-ethnic study of atherosclerosis. Circulation 129(1):77–86
Kalia NK, Cespedes L, Youssef G, Li D, Budoff MJ (2015) Motivational effects of coronary artery calcium scores on statin adherence and weight loss. Coron Artery Dis 26(3):225–230
Miedema MD, Duprez DA, Misialek JR et al (2014) Use of coronary artery calcium testing to guide aspirin utilization for primary prevention: estimates from the multi-ethnic study of atherosclerosis. Circ Cardiovasc Qual Outcomes 7(3):453–460
Smulders MW, Jaarsma C, Nelemans PJ et al (2017) Comparison of the prognostic value of negative non-invasive cardiac investigations in patients with suspected or known coronary artery disease-a meta-analysis. Eur Heart J Cardiovasc Imaging 18(9):980–987
Mark DB, Federspiel JJ, Cowper PA et al (2016) Economic outcomes with anatomical versus functional diagnostic testing for coronary artery disease. Ann Intern Med 165(2):94–102
Lorenzoni V, Bellelli S, Caselli C et al (2019) Cost-effectiveness analysis of stand-alone or combined non-invasive imaging tests for the diagnosis of stable coronary artery disease: results from the EVINCI study. Eur J Health Econ 20(9):1437–1449
Moss AJ, Williams MC, Newby DE, Nicol ED (2017) The updated NICE guidelines: cardiac CT as the first-line test for coronary artery disease. Curr Cardiovasc Imaging Rep 10(5):15
Knuuti J, Wijns W, Saraste A et al (2020) 2019 ESC guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J 41(3):407–477
Montalescot G, Sechtem U, Achenbach S et al (2013) 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J 34(38):2949–3003
Fihn SD, Gardin JM, Abrams J et al (2012) 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol 60(24):e44–e164
Hochman JS. International study of comparative health effectiveness with medical and invasive approaches: primary report of clinical outcomes. AHA scientific sessions 2019, Philadelphia, PA
Ambrose JA, Tannenbaum MA, Alexopoulos D et al (1988) Angiographic progression of coronary artery disease and the development of myocardial infarction. J Am Coll Cardiol 12(1):56–62
Nobuyoshi M, Tanaka M, Nosaka H et al (1991) Progression of coronary atherosclerosis: is coronary spasm related to progression? J Am Coll Cardiol 18(4):904–910
Little WC, Constantinescu M, Applegate RJ et al (1988) Can coronary angiography predict the site of a subsequent myocardial infarction in patients with mild-to-moderate coronary artery disease? Circulation 78(5 Pt 1):1157–1166
Tunstall-Pedoe H, Morrison C, Woodward M, Fitzpatrick B, Watt G (1996) Sex differences in myocardial infarction and coronary deaths in the Scottish MONICA population of Glasgow 1985 to 1991. Presentation, diagnosis, treatment, and 28-day case fatality of 3991 events in men and 1551 events in women. Circulation 93(11):1981–1992
Tian J, Ren X, Vergallo R et al (2014) Distinct morphological features of ruptured culprit plaque for acute coronary events compared to those with silent rupture and thin-cap fibroatheroma: a combined optical coherence tomography and intravascular ultrasound study. J Am Coll Cardiol 63(21):2209–2216
Rioufol G, Finet G, Ginon I et al (2002) Multiple atherosclerotic plaque rupture in acute coronary syndrome: a three-vessel intravascular ultrasound study. Circulation 106(7):804–808
Rodriguez-Granillo GA, Garcia-Garcia HM, Valgimigli M et al (2006) Global characterization of coronary plaque rupture phenotype using three-vessel intravascular ultrasound radiofrequency data analysis. Eur Heart J 27(16):1921–1927
Maehara A, Mintz GS, Bui AB et al (2002) Morphologic and angiographic features of coronary plaque rupture detected by intravascular ultrasound. J Am Coll Cardiol 40(5):904–910
Stone GW, Maehara A, Lansky AJ et al (2011) A prospective natural-history study of coronary atherosclerosis. New Engl J Med 364(3):226–235
Steg PG, Greenlaw N, Tendera M et al (2014) Prevalence of anginal symptoms and myocardial ischemia and their effect on clinical outcomes in outpatients with stable coronary artery disease: data from the International Observational CLARIFY Registry. JAMA Intern Med 174(10):1651–1659
Boden WE, O'Rourke RA, Teo KK et al (2007) Optimal medical therapy with or without PCI for stable coronary disease. New Engl J Med 356(15):1503–1516
Group BDS, Frye RL, August P et al (2009) A randomized trial of therapies for type 2 diabetes and coronary artery disease. N Engl J Med 360(24):2503–2515
De Bruyne B, Fearon WF, Pijls NH et al (2014) Fractional flow reserve-guided PCI for stable coronary artery disease. New Engl J Med 371(13):1208–1217
Xaplanteris P, Fournier S, Pijls NHJ et al (2018) Five-Year outcomes with PCI guided by fractional flow reserve. New Engl J Med 379(3):250–259
Garzillo CL, Hueb W, Gersh B et al (2019) Association between stress testing-induced myocardial ischemia and clinical events in patients with multivessel coronary artery disease. JAMA Intern Med. https://doi.org/10.1001/jamainternmed.2019.2227
Mancini GBJ, Hartigan PM, Shaw LJ et al (2014) Predicting outcome in the COURAGE trial (Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation): coronary anatomy versus ischemia. JACC Cardiovasc Interv 7(2):195–201
Hachamovitch R, Hayes SW, Friedman JD, Cohen I, Berman DS (2003) Comparison of the short-term survival benefit associated with revascularization compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation 107(23):2900–2907
Shaw LJ, Cerqueira MD, Brooks MM et al (2012) Impact of left ventricular function and the extent of ischemia and scar by stress myocardial perfusion imaging on prognosis and therapeutic risk reduction in diabetic patients with coronary artery disease: results from the Bypass Angioplasty Revascularization Investigation 2 Diabetes (BARI 2D) trial. J Nucl Cardiol 19(4):658–669
Shaw LJ, Berman DS, Maron DJ et al (2008) Optimal medical therapy with or without percutaneous coronary intervention to reduce ischemic burden: results from the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial nuclear substudy. Circulation 117(10):1283–1291
Stergiopoulos K, Boden WE, Hartigan P et al (2014) Percutaneous coronary intervention outcomes in patients with stable obstructive coronary artery disease and myocardial ischemia: a collaborative meta-analysis of contemporary randomized clinical trials. JAMA Intern Med 174(2):232–240
Baigent C, Keech A, Kearney PM et al (2005) Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet 366(9493):1267–1278
Ridker PM, Everett BM, Thuren T et al (2017) Antiinflammatory therapy with canakinumab for atherosclerotic disease. New Engl J Med 377(12):1119–1131
Sabatine MS, Giugliano RP, Keech AC et al (2017) Evolocumab and clinical outcomes in patients with cardiovascular disease. New Engl J Med 376(18):1713–1722
Bhatt DL, Steg PG, Miller M et al (2019) Cardiovascular risk reduction with icosapent ethyl for hypertriglyceridemia. New Engl J Med 380(1):11–22
Podrid PJ, Graboys TB, Lown B (1981) Prognosis of medically treated patients with coronary-artery disease with profound ST-segment depression during exercise testing. New Engl J Med 305(19):1111–1116
Chow BJ, Small G, Yam Y et al (2015) Prognostic and therapeutic implications of statin and aspirin therapy in individuals with nonobstructive coronary artery disease: results from the CONFIRM (COronary CT angiography evaluation for clinical outcomes: an international multicenter registry). Arterioscler Thromb Vasc Biol 35(4):981–989
Ostrom MP, Gopal A, Ahmadi N et al (2008) Mortality incidence and the severity of coronary atherosclerosis assessed by computed tomography angiography. J Am Coll Cardiol 52(16):1335–1343
Finck T, Hardenberg J, Will A et al (2019) 10-Year follow-up after coronary computed tomography angiography in patients with suspected coronary artery disease. JACC Cardiovasc Imaging 12(7 Pt 2):1330–1338
Min JK, Dunning A, Lin FY et al (2011) Age- and sex-related differences in all-cause mortality risk based on coronary computed tomography angiography findings results from the International Multicenter CONFIRM (Coronary CT Angiography Evaluation for Clinical Outcomes: An International Multicenter Registry) of 23,854 patients without known coronary artery disease. J Am Coll Cardiol 58(8):849–860
Lin FY, Shaw LJ, Dunning AM et al (2011) Mortality risk in symptomatic patients with nonobstructive coronary artery disease: a prospective 2-center study of 2,583 patients undergoing 64-detector row coronary computed tomographic angiography. J Am Coll Cardiol 58(5):510–519
Lee JM, Choi KH, Koo BK et al (2019) Prognostic implications of plaque characteristics and stenosis severity in patients with coronary artery disease. J Am Coll Cardiol 73(19):2413–2424
Maddox TM, Stanislawski MA, Grunwald GK et al (2014) Nonobstructive coronary artery disease and risk of myocardial infarction. JAMA 312(17):1754–1763
Nicholls SJ, Hsu A, Wolski K et al (2010) Intravascular ultrasound-derived measures of coronary atherosclerotic plaque burden and clinical outcome. J Am Coll Cardiol 55(21):2399–2407
Bittencourt MS, Hulten E, Ghoshhajra B et al (2014) Prognostic value of nonobstructive and obstructive coronary artery disease detected by coronary computed tomography angiography to identify cardiovascular events. Circ Cardiovasc Imaging 7(2):282–291
Rodriguez-Granillo GA, Carrascosa P, Bruining N et al (2016) Defining the non-vulnerable and vulnerable patients with computed tomography coronary angiography: evaluation of atherosclerotic plaque burden and composition. Eur Heart J Cardiovasc Imaging 17(5):481–491
Collet C, Capodanno D, Onuma Y et al (2018) Left main coronary artery disease: pathophysiology, diagnosis, and treatment. Nat Rev Cardiol 15(6):321–331
Elliott MD, Heitner JF, Kim H et al (2019) Prevalence and prognosis of unrecognized myocardial infarction in asymptomatic patients with diabetes: a two-center study with up to 5 years of follow-up. Diabetes Care 42(7):1290–1296
Oikonomou EK, Marwan M, Desai MY et al (2018) Non-invasive detection of coronary inflammation using computed tomography and prediction of residual cardiovascular risk (the CRISP CT study): a post-hoc analysis of prospective outcome data. Lancet 392(10151):929–939
Rodriguez-Granillo GA, Reynoso E, Capunay C, Carpio J, Carrascosa P (2018) Pericardial and visceral, but not total body fat, are related to global coronary and extra-coronary atherosclerotic plaque burden. Int J Cardiol 260:204–210
Rodriguez-Granillo GA, Reynoso E, Capunay C, Antoniades C, Shaw LJ, Carrascosa P (2019) Prognostic value of vascular calcifications and regional fat depots derived from conventional chest computed tomography. J Thorac Imaging 34(1):33–40
Goncalves Pde A, Rodriguez-Granillo GA, Spitzer E et al (2015) Functional evaluation of coronary disease by CT angiography. JACC Cardiovasc Imaging 8(11):1322–1335
Pontone G, Baggiano A, Andreini D et al (2019) Stress computed tomography perfusion versus fractional flow reserve CT derived in suspected coronary artery disease: the perfection study. JACC Cardiovasc Imaging 12(8 Pt 1):1487–1497
Koo BK, Erglis A, Doh JH et al (2011) Diagnosis of ischemia-causing coronary stenoses by noninvasive fractional flow reserve computed from coronary computed tomographic angiograms. Results from the prospective multicenter DISCOVER-FLOW (Diagnosis of Ischemia-Causing Stenoses Obtained Via Noninvasive Fractional Flow Reserve) study. J Am Coll Cardiol 58(19):1989–1997
Min JK, Leipsic J, Pencina MJ et al (2012) Diagnostic accuracy of fractional flow reserve from anatomic CT angiography. JAMA 308(12):1237–1245
Norgaard BL, Leipsic J, Gaur S et al (2014) Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: the NXT trial (analysis of coronary blood flow using CT angiography: next steps). J Am Coll Cardiol 63(12):1145–1155
Hlatky MA, De Bruyne B, Pontone G et al (2015) Quality-of-Life and economic outcomes of assessing fractional flow reserve with computed tomography angiography: PLATFORM. J Am Coll Cardiol 66(21):2315–2323
Driessen RS, Danad I, Stuijfzand WJ et al (2019) Comparison of coronary computed tomography angiography, fractional flow reserve, and perfusion imaging for ischemia diagnosis. J Am Coll Cardiol 73(2):161–173
Gijsen F, Katagiri Y, Barlis P et al (2019) Expert recommendations on the assessment of wall shear stress in human coronary arteries: existing methodologies, technical considerations, and clinical applications. Eur Heart J 40(41):3421–3433
Cheng JM, Garcia-Garcia HM, de Boer SP et al (2014) In vivo detection of high-risk coronary plaques by radiofrequency intravascular ultrasound and cardiovascular outcome: results of the ATHEROREMO-IVUS study. Eur Heart J 35(10):639–647
Lee JM, Choi G, Koo BK et al (2019) Identification of high-risk plaques destined to cause acute coronary syndrome using coronary computed tomographic angiography and computational fluid dynamics. JACC Cardiovasc Imaging 12(6):1032–1043
Shaw LJ, Mieres JH, Hendel RH et al (2011) Comparative effectiveness of exercise electrocardiography with or without myocardial perfusion single photon emission computed tomography in women with suspected coronary artery disease: results from the What Is the Optimal Method for Ischemia Evaluation in Women (WOMEN) trial. Circulation 124(11):1239–1249
Chaikriangkrai K, Velankar P, Schutt R et al (2015) Additive prognostic value of coronary artery calcium score over coronary computed tomographic angiography stenosis assessment in symptomatic patients without known coronary artery disease. Am J Cardiol 115(6):738–744
Hulten E, Bittencourt MS, Ghoshhajra B et al (2014) Incremental prognostic value of coronary artery calcium score versus CT angiography among symptomatic patients without known coronary artery disease. Atherosclerosis 233(1):190–195
Mouden M, Timmer JR, Reiffers S et al (2013) Coronary artery calcium scoring to exclude flow-limiting coronary artery disease in symptomatic stable patients at low or intermediate risk. Radiology 269(1):77–83
Villines TC, Hulten EA, Shaw LJ et al (2011) Prevalence and severity of coronary artery disease and adverse events among symptomatic patients with coronary artery calcification scores of zero undergoing coronary computed tomography angiography: results from the CONFIRM (Coronary CT Angiography Evaluation for Clinical Outcomes: An International Multicenter) registry. J Am Coll Cardiol 58(24):2533–2540
Engbers EM, Timmer JR, Ottervanger JP et al (2016) Prognostic value of coronary artery calcium scoring in addition to single-photon emission computed tomographic myocardial perfusion imaging in symptomatic patients. Circ Cardiovasc Imaging 9(5):e003966
Lee SE, Han K, Hur J et al (2018) Accuracy of computed tomography for selecting the revascularization method based on SYNTAX score II. Eur Radiol 28(5):2151–2158
Suh YJ, Han K, Chang S et al (2017) SYNTAX score based on coronary computed tomography angiography may have a prognostic value in patients with complex coronary artery disease: an observational study from a retrospective cohort. Medicine (Baltimore) 96(37):e7999
Collet C, Onuma Y, Andreini D et al (2018) Coronary computed tomography angiography for heart team decision-making in multivessel coronary artery disease. Eur Heart J 39(41):3689–3698
Shaw LJ, Berman DS, Picard MH et al (2014) Comparative definitions for moderate-severe ischemia in stress nuclear, echocardiography, and magnetic resonance imaging. JACC Cardiovasc Imaging 7(6):593–604
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We declare that Patricia Carrascosa is Consultant of GE Healthcare. None of the other authors has conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rodriguez-Granillo, G.A., Nieman, K., Carrascosa, P. et al. Anatomic or functional testing in stable patients with suspected CAD: contemporary role of cardiac CT in the ISCHEMIA trial era. Int J Cardiovasc Imaging 36, 1351–1362 (2020). https://doi.org/10.1007/s10554-020-01815-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-020-01815-7