Abstract
This review surveys the findings of the International Study of Comparative Health Effectiveness with Medical and Invasive Approaches (ISCHEMIA) trial and puts them into a clinical perspective regarding its effect of the role of cardiac magnetic resonance imaging (CMR) as a well-validated gatekeeper for invasive angiography and myocardial revascularization. Noninvasive stress testing of patients with intermediate-to-high pretest likelihood for obstructive coronary artery disease (CAD) using perfusion CMR provides excellent diagnostic accuracy in detecting ischemic myocardium, and additional information from tissue characterization can guide the management of patients with stable angina toward a more individualized therapy as other non-coronary underlying causes of chest pain can be detected. Since ISCHEMIA failed to show that an invasive strategy using percutaneous coronary intervention or coronary artery bypass grafting was associated with an improved prognosis compared with initial conservative medical therapy among stable patients with moderate-to-severe ischemia, CMR as a multifaceted diagnostic imaging approach to explain patients’ symptoms should be preferred over anatomical and stress testing alone. Nevertheless, the exclusion of left main coronary artery stenosis either by coronary CT or MR angiography may be required. In conclusion, the results of the ISCHEMIA trial are in good accordance with those of the MR-INFORM trial recently published in the New England Journal of Medicine, as the noninvasive management of a large proportion of patients with CAD was shown to be noninferior to current invasive strategies. Recent outcome data from trials may therefore have an impact on future guidelines to further reduce the execution of unnecessary left heart catheterizations.
Zusammenfassung
Im vorliegenden Übersichtsartikel werden die Ergebnisse der ISCHEMIA-Studie (International Study of Comparative Health Effectiveness with Medical and Invasive Approaches) genauer betrachtet und die daraus entstehenden Konsequenzen für die Kardio-Magnetresonanztomographie (MRT) als gut validiertem Gatekeeper für die invasive Angiographie und die myokardiale Revaskularisation aus klinischer Perspektive diskutiert. Der nichtinvasive Stresstest unter Verwendung der Perfusions-MRT bietet eine ausgezeichnete diagnostische Genauigkeit zum Nachweis von ischämischem Myokard bei Patienten mit mittlerer bis hoher Vortestwahrscheinlichkeit für eine stenosierende koronare Herzkrankheit (KHK). Zusätzliche Informationen aus der Gewebecharakterisierung können bei Patienten mit stabiler Angina pectoris zu einer individualisierteren Therapie führen, da weitere zugrunde liegende Ursachen für Brustschmerzen erkannt werden können. Da sich in der ISCHEMIA-Studie nicht nachweisen ließ, dass eine invasive Strategie mit perkutaner Koronarintervention oder Bypassoperation der Koronararterien mit einer verbesserten Prognose im Vergleich zur konservativen medizinischen Therapie bei stabilen Patienten mit mittelschwerer bis schwerer Ischämie verbunden war, sollte die Kardio-MRT als vielschichtiges diagnostisches Bildgebungsverfahren gegenüber den rein anatomischen und Belastungsuntersuchungen bevorzugt werden, um die Symptome von Patienten zu erklären. Möglicherweise muss zusätzlich der Ausschluss einer Stenose im linken Hauptstamm entweder durch Koronar-CT oder MR-Angiographie durchgeführt werden. Fazit ist, dass die Ergebnisse der ISCHEMIA-Studie gut mit denen der kürzlich im New England Journal of Medicine veröffentlichten MR-INFORM-Studie übereinstimmen, da das nichtinvasive Management den derzeitigen invasiven Strategien bei einem Großteil von Patienten mit KHK nicht unterlegen war. Die aktuellen Daten aus Outcome-Studien können daher Auswirkungen auf zukünftige Richtlinien haben, um die Durchführung unnötiger Linksherzkatheteruntersuchungen weiter zu reduzieren.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
The International Study of Comparative Health Effectiveness with Medical and Invasive Approaches (ISCHEMIA) trial [1] reports on the outcomes of 5179 patients with moderate-to-severe ischemia on imaging or exercise ECG and with confirmed coronary stenosis of >50% and no left main coronary artery disease on computed tomography angiography (CTA), after a median follow-up of 3.2 years. Patients were randomized to either an initial conservative strategy of medical therapy with angiography reserved for failure of medical therapy, or an initial invasive strategy of medical therapy, coronary angiography, and revascularization of all ischemic territories.
In short, the primary composite outcome of cardiovascular death, myocardial infarction, cardiac hospitalization for either unstable angina or heart failure, and resuscitated sudden death was not significantly different and relatively low in both study arms with an event rate of 18.2% in the initial conservative arm versus 16.4% in the initial invasive arm at 5 years (p = 0.34). The initial invasive strategy did not lead to a reduction of events versus the initial conservative strategy. However, high-risk patients (New York Heart Association [NYHA] Class III-IV HF, unacceptable angina despite medical therapy, ejection fraction [EF] < 35%, acute coronary syndrome [ACS] within 2 months, percutaneous coronary intervention [PCI] or coronary artery bypass grafting [CABG] within 1 year) were excluded from the ISCHEMIA trial. Approximately half of the patients assigned to the initial invasive strategy were free of angina at 1 year versus approximately 20% in the conservative strategy [2]. Thus, revascularization does not improve prognosis in patients with moderate-to-severe ischemia but it improves symptoms in a large proportion of patients.
How do these results affect cardiac magnetic resonance imaging (CMR) as a gatekeeper for invasive angiography and coronary revascularization?
We will discuss several aspects:
-
1.
What is the role of CMR pre-ISCHEMIA?
-
2.
How does this differ from the guidelines?
-
3.
How is this role affected by the ISCHEMIA results?
-
4.
Anatomy or function?
ISCHEMIA findings and the role of CMR
What is the role of CMR pre-ISCHEMIA as a gatekeeper for invasive angiography?
Perfusion CMR is a well-validated gatekeeper for invasive angiography with strengths across the whole spectrum of pre-test likelihoods. In the MR-INFORM trial [3] it was shown that the subsequent management of patients with intermediate-to-high pretest likelihoods can be decided safely based on perfusion CMR and that this test is non-inferior to invasive angiography supported by fractional flow reserve (FFR). In this clinical effectiveness trial, 918 patients with typical angina despite medical management and two or more risk factors for coronary artery disease were randomized into an initial invasive arm with revascularization of stenoses >90% or positive FFR (<0.8) or an MR-INFORMED arm, with an initial perfusion CMR study and referral to invasive angiography and revascularization only if at least two adjacent segments or one transmural segment was ischemic. There was no difference between the two arms, neither for the composite event outcome (death, myocardial infarction, target vessel revascularization), nor for the presence and severity of angina after a follow up of 1 year. Only 47% of patients in the MR-INFORMED arm had invasive angiography and only 36% were revascularized versus 45% of revascularizations in the invasive arm (p < 0.005). Importantly, only 4.1% of patients in the noninvasive arm had an out-of-protocol angiography (vs. 2.6% of the invasive arm, p = ns), demonstrating that decisions based on perfusion CMR guided patients well over the subsequent year.
These results demonstrate that patients with stable chest pain and high pre-test likelihood for coronary artery disease can be safely guided by perfusion CMR, significantly reducing the numbers of invasive angiography. These data expand on previous studies demonstrating an excellent diagnostic accuracy of perfusion CMR versus invasive angiography [4] and even more so versus FFR [5, 6], which has been shown to be more accurate than other noninvasive modalities except positron emission tomography (PET; [7]) in several studies with direct comparisons [8, 9] as well as in meta-analyses [10]. Perfusion CMR has also been shown to provide strong prognostic information. The ability to prognosticate has recently been expanded by not only taking the presence of ischemia into account but using the extent and the presence of myocardial necrosis as an additional marker [11]. As known from single-photon emission computed tomography (SPECT) studies, a higher ischemic burden is related to a higher event rate [12]. For the ISCHEMIA trial a perfusion CMR cut-off of 12% ischemic myocardium during vasodilator stress was used to define “moderate to severe.” This cut-off was based on a retrospective analysis trying to define cut-off values for different imaging modalities yielding a similar event rate [13]. Most likely, the relevant ischemic threshold is higher than expected so far. Interestingly, in the MR-INFORM trial all patients with cardiovascular death had either a large ischemic burden (>50% of myocardium), triple-vessel disease on invasive angiography or delayed index angiography, and died before revascularization [3].
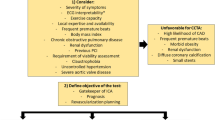
How does this differ from the guidelines?
Current European Society of Cardiology (ESC) guidelines suggest a functional test for patients with an intermediate-to-high pretest likelihood [14]. Only in patients with a high event risk is direct invasive angiography advised. The guidelines do not recommend a specific functional test, even though they acknowledge the excellent combination of positive and negative predictive values of perfusion CMR. Given the above data, we advocate that perfusion CMR be considered as the prime diagnostic modality for patients with intermediate-to-high pretest likelihoods. We would also advocate the use of perfusion CMR for patients with a very high pretest likelihood for coronary artery disease for two reasons. First, according to current ESC guidelines on revascularization, any revascularization should be based on the proof of ischemia [15] and second, MR-INFORM has shown safe clinical decision-making with perfusion CMR also in this specific patient group. Given the fact that in 2018 in Germany only 43% of left heart catheterizations resulted in a PCI, the need to use an accurate gatekeeper before diagnostic angiography remains of immense importance [16].
What is the role of CMR pre-ISCHEMIA in patients with low-to-intermediate pretest likelihoods?
Currently, CMR is less well established as a diagnostic modality in patients with a lower pretest likelihood for coronary artery disease despite some important characteristics. In these patients, current guidelines focus mainly on the exclusion of coronary artery disease [14]. Given the excellent negative predictive value of computed tomography angiography (CTA) in the literature, CTA is recommended as the prime technique for these patients. For optimal patient guidance, however, it is not only important to exclude a specific disease as the cause of the patients’ symptoms, but also to assess the underlying pathophysiology and, whenever possible, obtain a diagnosis explaining the symptoms and allowing the patient to be treated individually. Indeed, the literature on perfusion CMR demonstrated less favorable negative predictive values than published for CT. However, this can at least partially be explained by different patient populations with different prevalence of disease, as a lower prevalence in a study population will always lead to a better negative predictive value [17]. One of the major advantages of CMR is the ability to assess other pathophysiologies during the same examination. Patients with chronic chest pain or dyspnea as an angina equivalent may have microvascular disease (Fig. 1), left ventricular hypertrophy, inflammation (Fig. 2), or an underlying storage disease, all of which can be diagnosed with CMR in a standardized 30-min test including ventricular and atrial anatomy and function, valvular function, mapping, perfusion, and scar imaging [18]. The mapping techniques in particular have an excellent accuracy for the detection of cardiac pathology, allowing one to differentiate various forms of left ventricular hypertrophy [19], detecting significant myocardial inflammation [20], and providing prognostic data in ischemic [21] and nonischemic [22] heart disease. Thus, we also advocate a strong role of CMR in the work-up of patients less likely to have coronary artery disease.
Case example of a 52-year-old male human immunodeficiency virus-positive patient with dyspnea on exertion and no history of cardiovascular disease. Acquired immunodeficiency syndrome was clinically manifested in 1999 due to cytomegalovirus retinitis; however, the infection is currently well controlled with a viral load below the detection limit and normal CD4 cell counts under antiretroviral therapy. Cardiac magnetic resonance imaging with vasodilator stress revealed subendocardial circular hypoperfusion (arrowheads) of the myocardium, defined as a pattern of microvascular disease. The patient also had diffuse myocardial fibrosis with native T1 values ≥2 SD above the mean of the sequence- and scanner-specific normal ranges. Further abnormalities were not present. Additional coronary computed tomography angiography excluded the presence of any coronary plaque, stenosis, or congenital anomaly. Anti-remodeling drugs were recommended subsequently, whereas sole anatomical testing of the coronary arteries would not have resulted in further consequences
a–c Case example of a 43-year-old male with a 3-week history of atypical chest pain. High-sensitivity troponin T 78 ng/ml. Normal invasive angiography findings. Cardiac magnetic resonance imaging 7 days after the acute event shows an intramyocardial stria in late gadolinium enhancement (a, white arrows), an increased native T1 (b, 1171 ms, >4 SD above normal), and an increased native T2 signal (c, 42 ms, >3 SD above normal), allowing for a diagnosis of acute myocarditis with high confidence
How does this differ from the guidelines?
Numerous ESC guidelines recommend CMR to establish the underlying pathophysiology. They refrain from recommending it as a first-line technique, however, mainly due to lack of availability. Nevertheless, they acknowledge its ability to establish the etiology in more difficult cases, such as myocardial infarction with non-obstructed coronary arteries (MINOCA) [23], heart failure with preserved ejection fraction (HFpEF; [24]), and heart failure or cancer toxicity [25]. Again, we advocate that CMR be used earlier in the work-up of many patients if access to the technique is available (Fig. 3). Such access can be facilitated by short and standardized examinations, focusing on the core questions.
How is this role affected by the ISCHEMIA results?
The ISCHEMIA trial will require us to rethink many aspects of our work. Certain elements will remain unchanged, such as: Ischemia remains an important risk factor, risk reduction with guideline-directed medical therapy and lifestyle changes remain an important pillar of patient management, revascularization should not be performed without the proof of ischemia.
However, other parts of the diagnostic/therapeutic chain need to be reassessed.
Some have brought forward the extreme argument that no gatekeeper would be required at all as it has no consequence on the subsequent management. This argument would only hold if we would (a) not revascularize any patient with stable chest pain, (b) accept to not establish a diagnosis in patients with chest pain, (c) forfeit any individualized medical therapy. None of these would be adequate reactions to the new data.
To optimally guide patient management with efficient use of resources, the following thoughts should dominate our decision processes.
-
1.
Focus on explaining the patients’ symptoms rather than establishing or excluding the presence of coronary artery disease.
Based on the ISCHEMIA results, the main reason for coronary revascularization in chronic stable angina should be symptomatic relief, rather than improving prognosis. Consequently, the focus of any diagnostic test should be to understand the cause of the patients’ symptoms and advise the optimal direction for therapeutic intervention. In patients with myocardial ischemia, antianginal therapy should be maximized. If patients remain symptomatic and have ischemic myocardium at stress, revascularization is a safe and efficient method for symptom relief and should be focused on the ischemic territories. Patients who have no significant areas of ischemia or suffer from microvascular disease should not be revascularized but treated with guideline-directed medical therapy and lifestyle changes. Patients with inflammation may benefit from immunomodulation or -suppression. Here, CMR is well suited to guide the majority of these questions.
-
2.
Use stress testing only for patients with intractable symptoms, not responding to medical therapy or for risk assessment.
The use of stress testing can be reduced. In our clinical practice we see a considerable number of patients referred for stress testing based on risk factors but without having symptoms. This is due to the wish “to be on the safe side” and not miss “significant” coronary artery disease. This defensive strategy can be safely abandoned, risk management can focus on established risk factors without the proof of ischemia. Performing coronary angiography for defensive reasons should be fully eliminated. If symptomatic, a stress test is the more adequate solution, if there are no symptoms, conservative risk reduction should suffice.
Anatomy versus function?
The question of whether an anatomical or a functional test is better for assessing patients with suspected coronary artery disease has been hotly debated. The PROMISE study [26] of 10,003 patients has not provided a conclusive answer also due to the low rate of only approx. 11% of patients with a positive index test in the recruited cohort. The results of the ISCHEMIA trial further reduce the need for anatomical imaging, as the majority of the arguments set forth above, such as proof of ischemia in patients with high pretest likelihood and understanding non-coronary reasons for chest pain in patients with low pretest likelihood, favor functional imaging. On the other hand, the proof of the presence of plaques and especially high-risk plaques by CT has resulted in favorable outcomes due to intensified risk modification [27]. Whether coronary plaque or myocardial ischemia is the stronger risk factor is less important. Both are important and require systematic reduction of risk factors. An additional argument, which could be used to suggest CT coronary angiography for the majority of patients with stable chest pain, is the exclusion of left main coronary artery stenosis before randomization in the ISCHEMIA trial. Transferring these results to clinical practice would support the need to visualize the proximal coronary arteries, thus advocating for an anatomical test as the primary imaging modality. Alternatively to CT coronary angiography, MR coronary angiography may be a viable option with good diagnostic accuracy for large and proximal segments even with well-established techniques available on most of today’s MR scanners [28]. A combination of CMR coronary angiography and stress perfusion imaging has been used in the CE-MARC study yielding excellent accuracy [29]. The contribution of MR coronary angiography at that time was limited; however, the endpoint was based on diagnostic accuracy versus invasive angiography rather than outcome. In a more recent study, the addition of MR coronary angiography to stress perfusion imaging improved overall accuracy [30], again, however, versus invasive angiography as the reference standard. In patients with severely reduced ejection fraction, MR coronary angiography has been used to exclude coronary artery disease as the underlying cause [31]. In the MR-INFORM trial patients with left main coronary artery stenosis were not excluded from randomization. However, all patients with moderate-to-severe ischemia were revascularized, thus also not leaving significant left main coronary artery disease untreated.
Limitations
The discussion of the ISCHEMIA results needs to take certain limitations of the trial into account. A large group of patients was included with positive exercise ECG but no imaging and only about 5% had a perfusion CMR. Perfusion CMR with its higher accuracy may have yielded a different outcome. In ISCHEMIA, 28% of patients in the medical arm were revascularized within the first 4 years demonstrating the remaining importance of invasive procedures with revascularization.
Conclusion
The role of cardiac magnetic resonance imaging (CMR) as a well-validated gatekeeper for invasive angiography and myocardial revascularization has been revisited in light of the findings of the International Study of Comparative Health Effectiveness with Medical and Invasive Approaches (ISCHEMIA) trial. Noninvasive stress testing of patients with intermediate-to-high pretest likelihood for obstructive coronary artery disease using perfusion CMR provides excellent diagnostic accuracy in detecting ischemic myocardium. The ISCHEMIA trial failed to show that an invasive strategy using percutaneous coronary intervention or coronary artery bypass grafting was associated with an improved prognosis compared with initial conservative medical therapy among stable patients with moderate-to-severe ischemia; therefore, CMR as a multifaceted diagnostic imaging approach to explain patients’ symptoms should be preferred over anatomical and stress testing alone. Recent outcome data from trials may have an impact on future guidelines to further reduce unnecessary left heart catheterizations.
Change history
01 July 2020
In the above mentioned article, the family name of the second author was not given correctly: it is Carerj instead of Careri.
The authors apologize for this mistake.
The original article has been …
References
Maron DJ, Hochman JS, Reynolds HR et al (2020) Initial invasive or conservative strategy for stable coronary disease. N Engl J Med 382:1395–1407. https://doi.org/10.1056/NEJMoa1915922
Spertus JA, Jones PG, Maron DJ et al (2020) Health-status outcomes with invasive or conservative care in coronary disease. N Engl J Med 382:1408–1419. https://doi.org/10.1056/NEJMoa1916370
Nagel E, Greenwood JP, McCann GP et al (2019) Magnetic resonance perfusion or fractional flow reserve in coronary disease. N Engl J Med 380:2418–2428. https://doi.org/10.1056/NEJMoa1716734
Nagel E, Klein C, Paetsch I et al (2003) Magnetic resonance perfusion measurements for the noninvasive detection of coronary artery disease. Circulation 108:432–437. https://doi.org/10.1161/01.CIR.0000080915.35024.A9
Lockie T, Ishida M, Perera D et al (2011) High-resolution magnetic resonance myocardial perfusion imaging at 3.0-Tesla to detect hemodynamically significant coronary stenoses as determined by fractional flow reserve. J Am Coll Cardiol 57:70–75. https://doi.org/10.1016/j.jacc.2010.09.019
Watkins S, McGeoch R, Lyne J et al (2009) Validation of magnetic resonance myocardial perfusion imaging with fractional flow reserve for the detection of significant coronary heart disease. Circulation 120:2207–2213. https://doi.org/10.1161/CIRCULATIONAHA.109.872358
Morton G, Chiribiri A, Ishida M et al (2012) Quantification of absolute myocardial perfusion in patients with coronary artery disease: comparison between cardiovascular magnetic resonance and positron emission tomography. J Am Coll Cardiol 60:1546–1555. https://doi.org/10.1016/j.jacc.2012.05.052
Schwitter J, Wacker CM, Wilke N et al (2013) MR-IMPACT II: Magnetic Resonance Imaging for Myocardial Perfusion Assessment in Coronary artery disease Trial: perfusion-cardiac magnetic resonance vs. single-photon emission computed tomography for the detection of coronary artery disease: a comparative multicentre, multivendor trial. Eur Heart J 34:775–781. https://doi.org/10.1093/eurheartj/ehs022
Greenwood JP, Herzog BA, Brown JM et al (2016) Cardiovascular magnetic resonance and single-photon emission computed tomography in suspected coronary heart disease. Ann Intern Med 165:830–831. https://doi.org/10.7326/L16-0480
Takx RAP, Blomberg BA, Aidi HE et al (2014) Diagnostic accuracy of stress myocardial perfusion imaging compared to invasive coronary angiography with fractional flow reserve meta-analysis. Circ Cardiovasc Imaging 8:e2666. https://doi.org/10.1161/CIRCIMAGING.114.002666
Kwong RY, Ge Y, Steel K et al (2019) Cardiac magnetic resonance stress perfusion imaging for evaluation of patients with chest pain. J Am Coll Cardiol 74:1741–1755. https://doi.org/10.1016/j.jacc.2019.07.074
Hachamovitch R, Hayes SW, Friedman JD et al (2003) Comparison of the short-term survival benefit associated with revascularization compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation 107:2900–2907. https://doi.org/10.1161/01.CIR.0000072790.23090.41
Shaw LJ, Berman DS, Picard MH et al (2014) Comparative definitions for moderate-severe ischemia in stress nuclear, echocardiography, and magnetic resonance imaging. JACC Cardiovasc Imaging 7:593–604. https://doi.org/10.1016/j.jcmg.2013.10.021
Knuuti J, Wijns W, Saraste A et al (2019) 2019 ESC guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J 41:407–477. https://doi.org/10.1093/eurheartj/ehz425
Neumann F‑J, Sousa-Uva M, Ahlsson A et al (2019) 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J 40:87–165. https://doi.org/10.1093/eurheartj/ehy394
Andresen D (2018) Deutscher Herzbericht 2018. Deutsche Herzstiftung, Frankfurt am Main
Nagel E (2010) Magnetic resonance coronary angiography: the condemned live longer. J Am Coll Cardiol 56:992–994. https://doi.org/10.1016/j.jacc.2010.02.069
Hendel RC, Friedrich MG, Schulz-Menger J et al (2016) CMR first-pass perfusion for suspected inducible myocardial ischemia. JACC Cardiovasc Imaging 9:1338–1348. https://doi.org/10.1016/j.jcmg.2016.09.010
Hinojar R, Varma N, Child N et al (2015) T1 mapping in discrimination of hypertrophic phenotypes: hypertensive heart disease and hypertrophic cardiomyopathy. Circ Cardiovasc Imaging 8:e3285. https://doi.org/10.1161/CIRCIMAGING.115.003285
Hinojar R, Foote L, Ucar E et al (2014) Myocardial T2 mapping for improved detection of inflammatory myocardial involvement in acute and chronic myocarditis. J Cardiovasc Magn Reson 16:O63. https://doi.org/10.1186/1532-429X-16-S1-O63
Puntmann VO, Carr-White G, Jabbour A et al (2018) Native T1 and ECV of noninfarcted myocardium and outcome in patients with coronary artery disease. J Am Coll Cardiol 71:766–778. https://doi.org/10.1016/j.jacc.2017.12.020
Puntmann VO, Carr-White G, Jabbour A et al (2016) T1-mapping and outcome in nonischemic cardiomyopathy. JACC Cardiovasc Imaging 9:40–50. https://doi.org/10.1016/j.jcmg.2015.12.001
Thygesen K, Alpert JS, Jaffe AS et al (2019) Fourth universal definition of myocardial infarction. Eur Heart J 40:237–269. https://doi.org/10.1093/eurheartj/ehy462
Pieske B, Tschöpe C, de Boer RA et al (2019) How to diagnose heart failure with preserved ejection fraction: the HFA-PEFF diagnostic algorithm: a consensus recommendation from the Heart Failure Association (HFA) of the European Society of Cardiology (ESC). Eur Heart J 40:3297–3317. https://doi.org/10.1093/eurheartj/ehz641
Zamorano JL, Lancellotti P, Rodriguez Muñoz D et al (2016) 2016 ESC position paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC Committee for Practice Guidelines. Eur Heart J 37:2768–2801. https://doi.org/10.1093/eurheartj/ehw211
Douglas PS, Hoffmann U, Patel MR et al (2015) Outcomes of anatomical versus functional testing for coronary artery disease. N Engl J Med 372:1291–1300. https://doi.org/10.1056/NEJMoa1415516
SCOT-HEART Investigators, Newby DE, Adamson PD et al (2018) Coronary CT angiography and 5‑year risk of myocardial infarction. N Engl J Med 379:924–933. https://doi.org/10.1056/NEJMoa1805971
Kim WY, Danias PG, Stuber M et al (2001) Coronary magnetic resonance angiography for the detection of coronary stenoses. N Engl J Med 345:1863–1869. https://doi.org/10.1056/NEJMoa010866
Greenwood JP, Maredia N, Younger JF et al (2012) Cardiovascular magnetic resonance and single-photon emission computed tomography for diagnosis of coronary heart disease (CE-MARC): a prospective trial. Lancet 379:453–460. https://doi.org/10.1016/S0140-6736(11)61335-4
Zhang L, Song X, Dong L et al (2018) Additive value of 3T cardiovascular magnetic resonance coronary angiography for detecting coronary artery disease. J Cardiovasc Magn Reson 20:29. https://doi.org/10.1186/s12968-018-0450-2
Assomull RG, Shakespeare C, Kalra PR et al (2011) Role of cardiovascular magnetic resonance as a gatekeeper to invasive coronary angiography in patients presenting with heart failure of unknown etiology. Circulation 124:1351–1360. https://doi.org/10.1161/CIRCULATIONAHA.110.011346
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
E. Nagel received grant support from Bayer AG and speaker fees from Bayer AG. C.T. Arendt received a “Rotation Grant” from the DZHK. L. Careri and V.O. Puntmann declare that they have no competing interests.
For this article no studies with human participants or animals were performed by any of the authors. All studies performed were in accordance with the ethical standards indicated in each case.
Additional information
The original version of this article was revised: In this article, the family name of the second author was not given correctly: it is Carerj instead of Careri. The authors apologize for this mistake.
Rights and permissions
About this article
Cite this article
Nagel, E., Carerj, M.L., Arendt, C.T. et al. After ISCHEMIA: Is cardiac MRI a reliable gatekeeper for invasive angiography and myocardial revascularization?. Herz 45, 446–452 (2020). https://doi.org/10.1007/s00059-020-04936-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-020-04936-w