Abstract
Malignant peripheral nerve sheath tumors are rare sarcomas of children and adolescents, and they are aggressive tumors with a high rate of local recurrence. Here we report a case of a primary cardiac malignant peripheral nerve sheath tumor without neurofibromatosis type I. A 53-year old woman presented having had cough, expectoration, and dyspnea for 20 days and was found to have a heart-involving tumor diagnosed as a malignant peripheral nerve sheath tumor, a rare cardiac sarcoma of 9 × 4.5 × 3 cm in size. The patient underwent a successful resection of the tumor but died 14 months postoperative. We report this case for its rarity and peculiar mode of morphologic and immunohistochemical presentation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Malignant peripheral nerve sheath tumor (MPNST), also known as malignant schwannoma, neurofibrosarcoma, or neurosarcoma, arises from Schwann cells, perineural cells, or fibroblasts. Primary cardiac MPNSTs are relatively rare; only 15 cases of primary cardiac MPNSTs were reported in the literature to date [1,2,3,4]. Here we report a case of primary cardiac MPNST without neurofibromatosis type I.
Clinical information
Clinical data
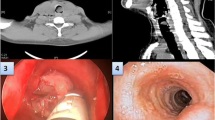
A 53-year old female patient presented having had cough, expectoration, and dyspnea for 20 days. The patient had been treated for bronchitis, but edema appeared in lower extremities, and cough and expectoration did not improve. A physical examination showed no cyanosis, no jugular venous distention, and breath sounds were clear bilaterally with no wheezes and no rales. The patient’s heart rate was 76 beats per minute, with a regular rhythm, and a diastolic murmur was heard at the apex. Further pitting edema appeared in the lower extremities. A trans-thoracic echocardiography (TTE) (Fig. 1a) showed an enlarged left atrium and a high echogenic mass of medium-intensity even echo and 77 × 38 × 33 mm in size attached to the posterior left atrial wall; the right atrium and both ventricles were normal. Furthermore, the echocardiography revealed a posterior pericardial effusion of about 7 mm in depth, with a clear echo-free space. A non-enhanced chest CT scan showed a bilateral pneumonia, pleural effusion, and pericardial effusion, but no tumor was found (Fig. 1b). A thoracic ultrasound scan showed a bilateral pleural effusion, and coronary angiography showed a normal coronary artery.
a Preoperative TTE demonstrating a giant mass inside the left atrium. b Image of non-enhanced chest CT scan. c The cut-surface of the mass was glistening and myxoid, with focal hemorrhage and necrosis. d The tumors are hyper-vascular with abundant capillaries and lots of thick vessels. The highly cellular areas neighbor less cellular one (hematoxylin and eosin, original magnification ×10). e The tumor cell proliferation is in the subendothelial zones of vessels. The nuclei of the tumor cells were enlarged and showed coarse chromatin, a thick nuclear membrane, and distinct nucleoli. (hematoxylin and eosin, original magnification ×40). f, g Immunohistochemical examination showed expressed positivity for PGP9.5 (original magnification × 10) and intense expression for Vim (original magnification ×10)
Surgical data
The tumor in the left atrium was excised in a hypothermic cardiopulmonary bypass surgery performed under general anesthesia. The right atrium and interatrial septum were incised, and the tumor, 9 × 4.5 × 3 mm in size, was located in the left atrium. The tumor appeared to have a capsule, smooth surface, tough texture, and pedicle (about 3 cm in diameter). The tumor was attached to the posterior wall of the left atrium, near the left atrial appendage, and involved the outlet of the left inferior pulmonary vein. However, the mitral valve and left ventricle were not involved. In this surgery, the tumor was completely resected at the pedicle of the tumor, together with a part of the posterior wall of the left atrium.
Pathological findings
Gross features
The tumor was a grey-white fusiform mass, 9 × 4.5 × 3 cm in size, and partly surrounded by a capsule. The mass was firm, jelly-like, fish-like, with a grey-yellow or red color on the cut surface (Fig. 1c). Hemorrhage and necrosis were seen in some areas.
Histological features
The tumor was a dense cellular tumor with alternating hypo- and hyper-cellular areas (Fig. 1d), a frequent map-like necrosis, and some areas with hyalinized stroma. The tumor mass was hyper-vascular with abundant capillaries and numerous thick vessels (Fig. 1e). Individual cells were slender with large nuclei and scanty cytoplasm. The nuclei of tumor cells were spindle-like or long oval-shaped and often had one to two small nucleoli, which were not distinct. The nuclei had irregular contours and prominent nuclear atypia, were hyperchromatic, and showed abundant mitotic activity.
Immunohistochemistry
The tumor cells expressed protein gene product 9.5 (PGP9.5) (Fig. 1f) and vimentin (Fig. 1g). The tumor cells stained negatively for S-100 protein, desmin, SMA, CD34, HMB45, CD57, and GFAP, and the MIB-1 (Ki-67) labelling index was high (30–40%).
Follow-up
The patient had a local recurrence 12 months after the surgical resection of the tumor and subsequently died in 2 months.
Discussion
MPNSTs occur more commonly in the nerve trunk of the proximal upper and lower extremities and occasionally in other sites, but they are rare in the parenchymatous viscera, and almost 50% of MPNSTs are associated with neurofibromatosis type I. As far as we know, only fifteen cases of a primary cardiac MPNST with complete pathological data have been reported to date [1,2,3,4]. As a result of the disease rarity, pathological characteristics and biological behavior of MPNSTs have not been clearly elucidated yet, and we are far from fully understanding the disease; hence, we report this case.
The heart receives a wealth of innervation, with the cardiac branch of the vagus nerve and the cardiac branch of the sympathetic nerve. The nerves that enter the heart are intertwined into a cardiac plexus. The cardiac plexus is divided into an atrial plexus and a left and right coronary plexus. Furthermore, there is a wide range of nerve fiber connections in intracardiac ganglion cells, and it is difficult to distinguish between the nerve fibers in the myocardial fiber bundles and the myocardial membrane unless special staining is used. The nerve fibers are composed of axons and dendrites with Schwann cells wrapped around their surface. The Schwann cell membrane wraps the axons and dendrites to form a myelin sheath. The MPNSTs originate from these Schwann cells, which make up the myelin sheath.
Primary cardiac MPNSTs occur predominantly in adults. Out of 16 patients, 9 were male and 7 were female (M:F = 9:7). The age ranged from 23 months to 66 years, with a median age of 32 years and an average age of 36 years. The left atria were the commonest site of involvement (6/16), followed by the pericardium (5/16), right ventricle (2/16), right atrium (2/16), and left ventricle (1/16).
The cardiac tumors can give rise to multiple cardiovascular and constitutional symptoms, which are non-specific and differ depending on the tumor site. Patients may present with constitutional symptoms like emaciation, fever, and edema of lower extremities, and with cardiovascular symptoms such as chest pain, fainting, bilateral cardiac failure, valvular disease-like symptoms, pericarditis symptoms, retention of pericardial effusion, cardiac tamponade, arrhythmia, and conductive disorders. Chest distress, shortness of breath, and chest pain are likewise common complaints. Tumors of the pericardium can give rise to pericarditis symptoms, mostly chest pain. MPNSTs present no specific signs that could be detected by an imaging examination, and they are hard to distinguish from other cardiac tumors like cardiac myxomas The diagnosis of primary cardiac MPNSTs depends on a pathological examination. Previous study noted intraoperative frozen sections can be used to define the character of the tumor and the surgical margins.
There are no significant differences between primary cardiac MPNSTs and other soft tissue sarcomas, generally speaking. The MPNST is usually large; the maximum size ranges from 4.1 to 18 cm, with 7.97 cm on average. The MPNST, which can be smooth on the surface and partially surrounded by a capsule, can have mostly solid sections with an occasional cystic section and the cut surface can be grey-yellow or white, fish-like, and with hemorrhage and necrosis.
Histological features are complicated; the tumors are composed of ovoid and short spindle cells arranged closely in fascicles, palisades, sheets, swirls, scattered, or with alternating hypo- and hyper-cellular areas and frequent map-like necrosis. The tumor is highly vascularized, with thick vessel walls surrounded by dense wavy tumor cells and with internal thrombosis. The nuclei are hyperchromatic, with marked pleomorphism and abundant mitotic activity, while the cytoplasm is eosinophilic or biophilic. Immunohistochemical staining is an important technique for the diagnosis as well as the differential diagnosis; MPNSTs show immunohistochemical expression of neuronal differentiation markers, e.g. S-100 protein, PGP9.5, CD57, CD56, and GFAP.
16 patients with the MPNST diagnosis underwent a radical or a partial surgical resection. It has been reported that the radical resection may improve the survival and the partial resection may improve the symptoms. 6 patients accepted a postoperative radiotherapy and chemotherapy, but the effects of radiotherapy and chemotherapy on the MPNSTs are not clear. Primary cardiac MPNSTs are easy to recur even after the radical resection, with a recurrence rate around 15% (2 patients). 13 cases have clear follow-up data, 5 patients died within half a year (the half-year fatality rate is high to 38%), 6 patients died within 2 years (the 2-year fatality rate is high to 46%), and 6 patients survived. At the follow-up evaluation, metastasis records were available for 10 patients. Metastasis occurred in 3 out of 10 patients (the metastasis rate is 30%), 2 to the lungs, 1 to both the small intestine and the brain.
In conclusion, the MPNST is a highly malignant tumor with a high short-term mortality rate. At present, there are no unified and effective treatment protocols, and a heart transplantation is considered an effective treatment option despite immunosuppression.
References
Sun J, Chen S, Fan R (2014) Primary cardiac malignant peripheral nerve sheath tumor in a 23-month-old infant. Cardiovasc Pathol 23(4):248–250
Ursell PC, Albala A, Fenoglio JJ Jr (1982) Malignant neurogenic tumor of the heart. Hum Pathol 13(7):640–645
Machado I, Arana E, Cruz J, Brotons S, Vendrell J, Escriba I, Chust ML, Martinez-Banaclocha N, Lavernia J, Llombart-Bosch A (2016) Malignant peripheral nerve sheath tumor with osseous heterologous differentiation in uncommon locations (heart and retropharynx). Int J Surg Pathol 24(5):456–462
Eindhoven JA, Loonstra EEG, Kik C, van den Bos EJ, Kofflard MJM (2018) Atypical presentation of a primary cardiac malignant peripheral nerve sheath tumor. Int J Cardiovasc Imaging 34(6):903–904
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Informed consent
Written informed consent was obtained from all patients for publication of data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, X., Liu, C. & Zhang, R. Primary cardiac malignant peripheral nerve sheath tumor: a case report. Int J Cardiovasc Imaging 35, 1615–1618 (2019). https://doi.org/10.1007/s10554-019-01608-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-019-01608-7