Abstract
New protocols for coronary computed tomography angiography (CCTA) could lower the radiation dose for patients but influence the image quality. To compare image quality and radiation exposure in step-and-shoot CCTA and high-pitch spiral CCTA. Fifty-nine pairs of patients matched for weight, height, sex and heart rate were included in this study (74 m, 44 f, average age 60 years, age range 29–94 years). Step-and-shoot CCTA and high-pitch spiral CCTA was performed on a third generation dual-source CT in equally sized patient groups. The signal-to-noise ratio (SNR) in the ascending aorta and the coronary arteries were determined for each dataset. Image quality was rated using a five-point scale. We used the t-test for paired samples to compare SNR and effective dose, and the Wilcoxon test to compare image quality scores. Mean effective dose for the step-and-shoot protocol (4.15 ± 3.07 mSv) was significantly higher in comparison to the high-pitch spiral protocol (1.2 ± 0.69 mSv; p < 0.0001). Mean SNR was higher with the step-and-shoot protocol compared to the high-pitch spiral protocol in the aorta, in the left main and peripheral coronary arteries (p < 0.01), in the proximal right coronary artery (p = 0.027). Image quality scores were significantly better for the step-and-shoot protocol (p = 0.0003). Step-and-shoot CCTA has significantly better SNR and overall image quality compared to high-pitch spiral CCTA, but with a mean effective dose more than thrice as high.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Coronary heart disease has a high prevalence and is one of the leading causes of death worldwide [1,2,3]. For example, because of the high prevalence of coronary heart disease, more than one million patients undergo invasive coronary angiography (ICA) in the United States every year [3]. Although ICA is still the gold standard diagnostic test, a reliable noninvasive imaging technique would be desirable, especially as less than half of all invasive coronary angiographies showed no need of percutaneous coronary intervention [4].
Coronary computed tomography angiography (CCTA) has been introduced more than 15 years ago and is meanwhile established as a modality with high sensitivity and high negative predictive value for detecting coronary artery stenosis. In the last few years, newer generation multislice computed tomography (CT) scanners have brought a significant increase in temporal and spatial resolution whereas the radiation dose and the needed amount of contrast could be decreased significantly [5]. An important factor for radiation exposure reduction has been the use of prospective electrocardiographic (ECG) gated CT data acquisition, mostly performed in step-and-shoot mode [6, 7]. Second and third generation dual source scanners also allow for prospective high-pitch spiral CCTA, with even lower radiation exposure.
The aim of this study was to compare image quality and radiation exposure of the “state-of-the-art” step-and-shoot CCTA and the modern approach the high-pitch spiral CCTA feasible on second and third generation dual-source CT scanners.
Materials and methods
This retrospective, single center study compares step-and-shoot data acquisition to the new high-pitch spiral CCTA. The protocol of our study was approved by our local ethics committee and written informed consent was waived. All patients included in this study underwent CCTA for clinical indications with low or intermediate pre-test probability for coronary disease.
Inclusion criteria were patients with risk of coronary disease and a clinical indication for CCTA. Exclusion criteria were cardiac arrhythmia, severe coronary sclerosis within the coronary artery segments or filiform coronary arteries where it is impossible to place the normalized ROI within the vascular lumen, and incomplete documentation of patient data such as height, weight or pulse frequency during the CCTA examination.
Patient characteristics
The radiology information system (RIS) of our hospital was searched for patients who underwent a CCTA between August 2014 and August 2015. In total, 416 patients underwent a CCTA during this period; all these examinations were performed on a dual-source scanner. 197 patients underwent CCTA with retrospective triggering and were thus excluded from the study. From the remaining 219 patients, 126 were examined using step-and-shoot mode and 93 using high-pitch spiral-mode.
We included 118 patients (n = 59 in each group, 74 males and 44 females, average age 60 years, age range 29–94 years). Due to a larger amount of examination using the step-and-shoot protocol and the variety of influencing factors, we used the propensity score matching [8] to find the best comparable partners. Matching was performed separately for male and female patients because of different thoracic wall anatomy and thus possible differences in radiation dose.
Of the 118 patients, a total of 32 underwent invasive coronary angiography. The results of coronary angiography were used as a gold standard to compare stenosis assessment by CCTA.
CT imaging technique
In all patients a four-channel ECG was used to monitor the heart rate. We administered an intravenous β-blocker (Beloc® i.v. 5 mg/5 ml, AstraZeneca GmbH, London, England) in recommended dosage [9, 10] via an intravenous catheter (16G) placed in the right antecubital vein to achieve a heart rate below 70 beat per minute (bpm). The initial dose of metoprolol was 2.5 mg. Depending to the response rate additional injections were made in intervals of 5 min up to a maximum dose of 15 mg. Additionally 0.4 mg of sublingual nitroglycerine spray (Nitrolingual Pumpspray; Pohl-Boskamp, Hohenlockstedt, Germany) were administered 2–4 min before cardiac CT.
50 ml of contrast (Ultravist 370, Iopromid; Bayer Healthcare, Leverkusen, Germany) were injected to all patients at a flow rate of 5 ml/s, followed by 50 ml isotonic saline at the same flow rate, using a dual head injector (Medtron Accutron CT-D, Medtron, Saarbrücken, Germany).
All examinations were performed with the same 384-slice CT scanner (Somatom Force, Siemens Medical Solutions, Erlangen, Germany) using a provided bolus tracking software by the same vendor (CareBolus, Siemens Medical Solutions, Erlangen, Germany) for CCTA acquisition [11, 12]. Therefore a single low dose scan (120 kV, 20 mAs) linked to the CT-scout at the high of the ascending aorta to place a circular region of interest (ROI) centrally in the aortic lumen. Afterwards repeated low dose scans with a delay of 1.13 s were started 10 s after contrast injection until the trigger threshold of 120 HU was reached. After reaching the trigger threshold the CT table moved to the start position and the patient was instructed to hold her/his breath.
Two different CCTA acquisition protocols were used. The first group of patients received a CCTA with the new adaptive step-and-shoot mode. The second type of CCTA was performed in adaptive high-pitch spiral mode. Both modes were performed with prospective ECG-triggering (Fig. 1). Scan parameters of both techniques were described in Table 1.
Screenshot of ECG-gating in preparation of CCTA. Prospectively ECG-gated step and shoot protocol with sequential prospective activation of the X-ray beam (columns) between the table movements at a predefined segment of the RR interval (usually 60–80% of the R–R interval). Prospectively ECG-gated high-pitch spiral protocol with a coverage speed of up to 737 mm/s and image acquisition within one heart beat (about 150 ms) with a temporal resolution of 66 ms. The image acquisition in the high-pitch spiral protocol is usually centered at 70% of the R–R interval
An experienced radiologist chose the protocol prior the examination based on individual patient characteristics. After the examination, the images were immediately viewed by a radiologist and the sufficient quality evaluated so that the decision as to whether the examination should be repeated could be made immediately afterward.
Independent of the mode all CT data were acquired in the caudocranial direction with a temporal resolution of 66 ms, a collimation of 2 × 192 × 0.6 mm, a gantry rotation time of 0.25 s. An automatic modulation of the tube current was used in all examinations (CARE Dose 4D, Siemens Medical Solutions). Tube voltage was optimized for every patient in both protocols by using automatic tube voltage adjustment called “CARE kV” by the vendor [13]. For reconstruction of the axial CCTA images a slice thickness of 0.6 mm, an increment of 0.4 mm, a field-of-view of 180 × 180 mm and a soft reconstruction kernel (Bv40) were chosen for both acquisition modes. All datasets were reconstructed using advanced modeled iterative reconstruction (ADMIRE) software (Siemens Healthcare AG). The calculation of the effective dose was made by multiplying the scanner provided dose-length product with a conversion coefficient of the chest of 17 µSv/mGy × cm [14].
Image analysis
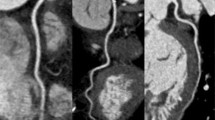
Quantitative image analysis of the axial CCTA images was made in the ascending aorta and the proximal and distal parts of both coronary arteries for each dataset by determining the signal-to-noise ratio (SNR) in each vessel. SNR was defined as a quotient of the mean density and the standard deviation of a normalized region of interest (ROI). The ROI in the ascending aorta was placed at the same height as the release of the left coronary artery and hat a standardized surface of 100 mm2, since this can be regarded as sufficiently representative. The surface of the ROI in the left main coronary artery (LM) was determined to 25 mm2 and to 15 mm2 in the right coronary artery (RCA, segment 1 and 2), in the left anterior descending artery (LAD, segment 7) as well in the ramus circumflexus (RCX, segment 13). The size of the ROI was chosen so that it is adapted as closely as possible to the standard width of the vessels. Beside the size of the ROI special attention was paid that no coronary plaques were included within the ROI position (Fig. 2).
Qualitative image analysis for both study groups was independently performed by two board-certified radiologists with 10 respectively 6 years of experience in cardiac imaging. Both readers were blinded for the mode of CT data acquisition and for the patient’s clinical information. The readers evaluated the images independently at different times on a workstation equipped with PACS software (IMPAX EE R 20, Agfa Healthcare, Mortsel, Belgium).
The qualitative assessment of the image quality was performed for the segments of the main coronary arteries according to the 17-segment model provided by the American Heart Association guidelines [15]. A Likert-scale point score system with a 5-point ranking scale was used to classify the image quality (Table 2).
In addition, the degree of stenosis in each coronary segment was also evaluated. Reconstructions of the coronary arteries were performed using the Syngo.Via reconstruction software (Siemens Syngo.Via Multimodality Workplace; Version VB30A_HF01, Siemens, Germany). A distinction was made between stenoses less than 50% and greater than or equal to 50%.
Statistical analysis
The Wilcoxon test was used to compare image quality scores between the two patient groups. Interrater agreement was assessed using weighted κ. κ values were interpreted according to thresholds proposed by Landis and Koch [16] (with κ ≤ 0 being poor agreement; 0.01–0.2, slight agreement; 0.21–0.4, fair agreement; 0.41–0.6, moderate agreement; 0.61–0.8, substantial agreement; and 0.81–1, almost perfect agreement).
The propensity score matching was performed with the R software environment for statistical computing [17] using the “MatchIt” package [18]. The matching method was “nearest neighbor” that matches the closest control unit for each treated unit. Conditional on the covariates a distance measure utilizing a logistic regression model is used to estimate the propensity score. For each treated unit matches are chosen one at a time. Therefore each control unit that is not yet matched but is closest to the treated unit on the distance measure is chosen at each matching step.
The t-test for paired samples was used to compare SNR between the step-and-shoot protocol and the high-pitch protocol. In this case, the Bonferroni correction [19, 20] was used to avoid the effect of multiple comparisons (as SNR from three vessels are compared). Due to the Bonferroni correction a p value of 0.0167 or less was considered statistically significant for SNR comparison.
Otherwise, a p value of 0.05 or less was considered statistically significant. Statistical analysis was performed with MedCalc 16.4.2 (MedCalc Software, Ostend, Belgium).
Sensitivity and specificity were calculated with regard to the comparison of the stenosis degree between ICA and CCTA.
Results
Both patient groups of the step-and-shoot and the high-pitch spiral protocol did not differ significantly after the matching process in regard to heart rate, height and weight (Table 3).
The two readers had identical image quality scores in 88/118 patients (74.6%) and differing results in 30/118 patients (25.4%). The resulting weighted kappa was κ = 0.69, consistent with substantial interrater agreement.
Overall image quality scores were significantly higher for patients examined with the step-and-shoot protocol when compared to the high-pitch spiral (p = 0.0003).
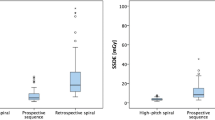
Mean SNR was higher with the step-and-shoot protocol compared to the high-pitch spiral protocol in the ascending aorta (16.31 ± 4.66 vs. 12.24 ± 3.67, p < 0.0001), the LM (20.15 ± 11.03 vs. 12.91 ± 4.69, p < 0.0001), the LAD (26.91 ± 11.13 vs. 14.04 ± 8.08, p < 0.0018), the CX (22.17 ± 12.15 vs. 13.64 ± 5.62, p < 0.0081) and the RCA in segment 2 (36.7 ± 26.87 vs. 14.95 ± 6.06, p < 0.0047). In the proximal RCA, the mean SNR did not differ significantly between the two protocols (17.00 ± 6.57 vs. 15.73 ± 8.94, p = 0.027).
Both methods of CCTA were compared with ICA results in terms of sensitivity and specificity. Of a total of 59 patient pairs, 32 patients underwent ICA. The step-and-shoot CCTA showed a significantly better sensitivity compared to the high-pitch spiral CCTA protocol (80% vs. 50%). The specificity values hardly differed (97.8% vs. 97.3%). The results of the coronary segments are summarized in Table 4. Due to motion artifacts or blooming artifacts caused by pronounced coronary sclerosis, the degree of stenosis in individual segments could not be reliably assessed. For this reason, 4 segments were not evaluated for the step-and-shoot protocol and 23 segments for the high-pitch spiral protocol. These were not included in the calculation of sensitivity and specificity.
A total of five examinations had to be repeated due to larger artifacts (one from the group of step-and-shoot protocol and four from the group of high-pitch spiral protocol). The repetition of the examination was done in the case of the step-and-shoot protocol with a retrospectively gated spiral protocol and in the case of the four high-pitch protocols, the repetition by step-and-shoot protocol was sufficient.
The mean radiation dose was significantly lower for the patients examined with the high-pitch spiral protocol in both for the actual (28.92%) as well as the normalized (12 cm) z-axis length (25.86%).
The mean radiation dose for the patients undergoing the step-and-shoot protocol was 4.15 ± 3.07 mSv (range 17.12–0.97 mSv) and for the high-pitch spiral protocol 1.20 ± 0.69 mSv (range 3.86–0.35 mSv). The mean tube voltage did not differ significantly (86.95 kV ± 17.54) for the step-and-shoot protocol and (84.75 kV ± 10.88) for the high-pitch spiral protocol.
Discussion
In this study, we compared two prospectively gated cardiac CT protocols, the step-and-shoot CCTA and a modern approach the high-pitch spiral CCTA protocol.
Our data showed a significantly higher SNR within the measured region of interests and a better overall image quality when using the step-and-shoot protocol but the mean radiation dose is more than thrice as high compared to the high-pitch protocol.
To our knowledge, this is the first study to assess image quality and radiation exposure for the before mentioned CCTA protocols in comparable patient cohorts.
Comparing CCTA acquisition protocols is difficult, as repeated CCTA in the same patients would not be permissible on ethical reasons. To achieve comparable patient cohorts for both CCTA protocols either very large patient cohorts or preselection are necessary.
Previous studies have not sufficiently addressed the issue of cohort comparability. For example, Smettei et al. [21] compared fast pitch CCTA and step-and-shoot CCTA, but did not select the patients in the two groups to assure better comparability (81 patients in each group).
In regard to radiation exposure, the results of our study are similar to earlier studies on related topics.
For example, Ghadri et al. [22] have shown a lower radiation exposure in high-pitch CCTA compared to step-and-shoot CCTA; however, different scanner types were used for each type of CCTA. Similarly, Wang et al. [23] were also able to show lower radiation doses in high-pitch CCTA, but this was achieved at lower tube voltage than the step-and-shoot CCTA.
Previous results on image quality however differ from our findings. Smettei et al. did not find significant differences in image quality between high-pitch CCTA and step-and-shoot CCTA. But, as mentioned above, the patients were not matched in this study.
Although a number of solutions have contributed to dose reduction in computed tomography in the past, especially the usage of prospective vs. retrospective gated CCTA, further reduction would be desirable to reduce the life risk of cancer due to CCTA [24, 25]. Newer generation CT scanner are using the dual-source technology with two X-ray tubes and two corresponding detector arrays to enable a z-axis-coverage of the entire heart within one heartbeat for further dose reduction.
For best comparability we subdivided the two groups of patients undergoing the two different protocols of CCTA in male and female patients and a propensity score matching was used to find the nearest partners of both groups. The propensity score matching is a very useful method to minimize the difference in the multiple covariates like heart rate, weight and height which has a leading influence on image quality and radiation dose. Apart from that it was guaranteed that the length of the z-axis and the tube voltage did not differ significantly in both groups to minimize the factors influencing the dose of radiation. We found out that the radiation dose in high-pitch spiral CCTA was about one-fourth compared to the step-and-shoot CCTA protocol. Therefore the high-pitch spiral CCTA seems to be a preferable method of choice in the light of radiation hygiene and reduction of patients risk on radiation exposure.
On the other side high-pitch spiral CCTA showed a significantly lower image quality for the aorta and coronary arteries within the subjective scoring using a Likert scale by two blinded radiologists as well in the objective measurement of the signal to noise ratio for the Aorta, the left main and the peripheral coronary arteries (RCA in segment 2, LAD in segment 7 and CX in segment 13). Only the first segment of the right coronary artery shows a notable but not significant difference for the measurement of the signal to noise ratio. We can only speculate about this result. Maybe one reason could be found in the coronary dominance pattern that shows a dominance of the RCA in more than 80% [26] and the higher blood flow within a dominant RCA [27] compared to the LM.
Another reason for better image quality of the step-and-shoot protocol, apart from the higher radiation dose, could be the absences of table movement during the scan time. In respective of the acquired images there are more possibilities of reconstruction in the step-and-shoot CCTA protocol due to the higher amount of R–R interval reconstruction percentages, which could also be an important reason for better image quality, compared to high-pitch spiral CCTA.
A limitation of our study is the retrospective design and therefore the capabilities of including patients. Due to ethical reasons we had to use two different groups of patients and could not justify using both protocols for the same patient. Therefore the comparability is not ideal but it was optimized by using the propensity score for matching two groups of patients fitting the most in biometric data witch influence the radiation dose and image quality the most. The patients included in this study were examined for clinical reasons and had an intermediate risk of coronary disease. Due to the need to place a ROI within the coronary vessels, no patients with severe coronary plaques which made it impossible to place the standardized ROI in the coronary arteries could be included. Therefore, this study could give only a limited statement for patients with excessive arteriosclerosis.
A further limitation of the study results from the protocols for image acquisition, since the methodology can only be applied to the latest generation of Siemens scanners and is not directly transferable to other device manufacturers.
In conclusion, our study showed a significant reduction of radiation dose but also lower image quality for high-pitch CCTA when compared to step-and-shoot CCTA which leads to lower sensitivity in the determination of the stenosis degree of coronary plaques. Due to this conflict, the usage of high-pitch spiral CCTA should be used deliberately and only for a selected patient population like young individuals with a low pre-test probability could benefit from the high-pitch spiral protocol.
References
Roth GA, Huffman MD, Moran AE, Feigin V, Mensah GA, Naghavi M et al (2015) Global and regional patterns in cardiovascular mortality from 1990 to 2013. Circulation 132:1667–1678
Bhatnagar P, Wickramasinghe K, Williams J, Rayner M, Townsend N (2015) The epidemiology of cardiovascular disease in the UK 2014. Heart 101:1182–1189
Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ et al (2014) Heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation 129:e28–e292
Patel MR, Peterson ED, Dai D, Brennan JM, Redberg RF, Anderson HV et al (2010) Low diagnostic yield of elective coronary angiography. N Engl J Med 362:886–895
Dewey M, Zimmermann E, Deissenrieder F, Laule M, Dübel H-P, Schlattmann P et al (2009) Noninvasive coronary angiography by 320-row computed tomography with lower radiation exposure and maintained diagnostic accuracy: comparison of results with cardiac catheterization in a head-to-head pilot investigation. Circulation 120:867–875
Hsieh J, Londt J, Vass M, Li J, Tang X, Okerlund D (2006) Step-and-shoot data acquisition and reconstruction for cardiac X-ray computed tomography. Med Phys 33:4236–4248
Earls JP (2009) How to use a prospective gated technique for cardiac CT. J Cardiovasc Comput Tomogr 3:45–51
Baek S, Park SH, Won E, Park YR, Kim HJ (2015) Propensity score matching: a conceptual review for radiology researchers. Korean J Radiol 16:286–296
Pannu HK, Alvarez W, Fishman EK (2006) Beta-blockers for cardiac CT: a primer for the radiologist. Am J Roentgenol 186:S341–S345
Raju VM, Gosling OE, Morgan-Hughes G, Colliver RJ, Iyengar S, Dissanayake P et al (2014) High-dose intravenous metoprolol usage for reducing heart rate at CT coronary angiography: efficacy and safety. Clin Radiol 69:739–744
Cademartiri F, Nieman K, van der Lugt A, Raaijmakers RH, Mollet N, Pattynama PMT et al (2004) Intravenous contrast material administration at 16-detector row helical CT coronary angiography: test bolus versus bolus-tracking technique. Radiology 233:817–823
Sun K, Liu G-R, Li Y-C, Han R-J, Cui L-F, Ma L-J et al (2013) Intravenous contrast material administration at high-pitch dual-source CT coronary angiography: bolus-tracking technique with shortened time of respiratory instruction versus test bolus technique. Chin Med Sci J 27:225–231
Ulzheimer S, Endt H, Leidecker C (2011) CARE kV—How to optimize individualized dose. Siemens Med. Solut. USA, Inc. http://health.siemens.com/ct_applications/somatomsessions/index.php/care-kv-how-to-optimize-individualized-dose. Accessed 8 Mar 2016
Bongartz G, Golding SJ, Jurik AG, Leonardi M, van Meerten EP, Geleijns JM fl. EUR 16262 EN. http://www.drs.dk/guidelines/ct/quality/index.htm. Accessed 15 Feb 2019
Cerqueira MD (2002) Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart: a statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 105:539–542
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biom Int Biom Soc 33:159
R Core Team (2017) R: a language and environment for statistical computing. http://www.r-project.org/. Accessed 23 July 2018
Randolph JJ, Falbe K, Manuel AK, Balloun JL (2014) A step-by-step guide to propensity score matching in R. Pract Assess Res Eval 19. http://eric.ed.gov/?id=EJ1046892. Accessed 2 May 2016
Armstrong RA (2014) When to use the Bonferroni correction. Ophthalmic Physiol Opt 34:502–508
Curtin F, Schulz P (1998) Multiple correlations and Bonferroni’s correction. Biol Psychiatry 44:775–777
Smettei OA, Sayed S, Al Habib MA, Alharbi F, Abazid RM (2018) Ultra-fast, low dose high-pitch (FLASH) versus prospectively-gated coronary computed tomography angiography: comparison of image quality and patient radiation exposure. J Saudi Heart Assoc 30:165–171
Ghadri JR, Küest SM, Goetti R, Fiechter M, Pazhenkottil AP, Nkoulou RN et al (2012) Image quality and radiation dose comparison of prospectively triggered low-dose CCTA: 128-slice dual-source high-pitch spiral versus 64-slice single-source sequential acquisition. Int J Cardiovasc Imaging 28:1217–1225. https://doi.org/10.1007/s10554-011-9921-3
Wang W, Zhao YE, Qi L, Li X, Zhou CS, Zhang LJ et al (2017) Prospectively ECG-triggered high-pitch coronary CT angiography at 70 kVp with 30 mL contrast agent: an intraindividual comparison with sequential scanning at 120 kVp with 60 mL contrast agent. Eur J Radiol 90:97–105
Zanzonico P, Dauer L, Strauss HW (2016) Radiobiology in cardiovascular imaging. JACC Cardiovasc Imaging 9:1446–1461
Huang B, Li J, Law MW-M, Zhang J, Shen Y, Khong PL (2010) Radiation dose and cancer risk in retrospectively and prospectively ECG-gated coronary angiography using 64-slice multidetector CT. Br J Radiol 83:152–158. https://doi.org/10.1259/bjr/29879495
Gebhard C, Fuchs TA, Stehli J, Gransar H, Berman DS, Budoff MJ et al (2015) Coronary dominance and prognosis in patients undergoing coronary computed tomographic angiography: results from the CONFIRM (COronary CT Angiography EvaluatioN For Clinical Outcomes: an international multicenter) registry. Eur Heart J Cardiovasc Imaging 16:853–862
Sakamoto S, Takahashi S, Coskun AU, Papafaklis MI, Takahashi A, Saito S et al (2013) Relation of distribution of coronary blood flow volume to coronary artery dominance. Am J Cardiol 111:1420–1424
Funding
This study was not supported by any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Consent for publication
Consent for publication was obtained for every individual person’s data included in the study.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Seppelt, D., Kolb, C., Kühn, J.P. et al. Comparison of sequential and high-pitch-spiral coronary CT-angiography: image quality and radiation exposure. Int J Cardiovasc Imaging 35, 1379–1386 (2019). https://doi.org/10.1007/s10554-019-01568-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-019-01568-y