Abstract
Objectives
To compare radiation exposure and image quality of second-generation 128-slice dual-source CT (DSCT) coronary angiography (cCTA) protocols.
Materials and methods
We retrospectively analyzed data from four groups with 25 patients, each examined by one of the following DSCT cCTA protocols: prospectively ECG-gated high-pitch (group 1) or sequential (group 2) acquisition, retrospectively ECG-gated acquisition in dual-energy (DECT, group 3) or dual-source (group 4) mode. CT dose index volume, dose length product, estimated radiation dose, contrast-to-noise- and signal-to-noise-ratios were compared. Subjective image quality was rated by two observers blinded to the protocols.
Results
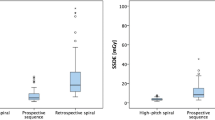
High-pitch DSCT showed a mean estimated radiation dose of 1.27 ± 0.62 mSv, significantly (p < 0.01) lower than sequential (2.04 ± 0.94 mSv), dual-energy (3.97 ± 1.29 mSv) or dual-source (8.11 ± 4.95 mSv) acquisition. Image noise showed no statistical difference (p > 0.91), ranging from 15.2 ± 4.4 (group 2) up to 24.5 ± 22.0 (group 4). Each protocol showed diagnostic image quality in at least 98.1 % of evaluated coronary segments without significant differences (p > 0.05).
Conclusions
Prospectively ECG-gated DSCT protocols enable cCTA with significant dose reduction and consistently diagnostic image quality. In patients requiring retrospectively ECG-gated DSCT for functional analysis or due to arrhythmia, dual-energy mode should be preferred over dual-source mode as it significantly decreases estimated dose without compromising image quality.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Coronary CT angiography (cCTA) has become a routinely used non-invasive examination to assess coronary artery disease (CAD) and has, therefore, been included into several guidelines for the evaluation of symptomatic patients with an intermediate risk for CAD [1, 2]. During the last decade, several electrocardiogram-gated (ECG) techniques for cCTA have been introduced to reduce the resulting radiation dose for the patient to even below 1 mSv [3, 4]. However, in clinical practice not all patients can be evaluated using the proposed protocols with very low radiation exposure due to arrhythmia, tachycardia or body habitus [5–7]. In addition, some indications for cCTA require functional analysis of the complete heart cycle which is usually performed using retrospectively ECG-gated protocols [8, 9].
Dual-source CT (DSCT) can be used to reduce examination times during cardiac CT and has also been shown to lower the resulting radiation dose [10–12]. On second-generation 128-slice DSCT, two prospectively ECG-triggered (high-pitch spiral and sequential mode) and two retrospectively ECG-gated (dual-energy and dual-source mode) protocols are available for cCTA. The prospectively ECG-gated protocols are usually used to achieve substantial radiation dose savings in patients requiring anatomical analysis of coronary artery patency [3, 5, 7]. Both retrospectively ECG-gated protocols are mainly used in patients requiring functional analysis of the myocardium during the complete heart cycle or in patients with severe arrhythmia [5, 6]. Selecting the appropriate examination protocol for each patient is crucial and depends on heart rate, body habitus and necessity of functional analysis [5]. However, to our knowledge there is no published study comparing these four protocols regarding radiation dose and image quality using the same second-generation DSCT in clinical practice.
Therefore, the purpose of the present study was to retrospectively compare the effective dose estimates, measurements of objective image quality and assessment of subjective image quality for clinically indicated cCTA examinations using the available prospectively and retrospectively ECG-triggered data acquisition protocols on the same second-generation 128-slice DSCT.
Materials and methods
Patient selection and study design
This retrospective single-institution study was approved by the local medical ethics committee with waiver of the requirement for informed consent. Data acquired from patients examined using the same second-generation 128-slice DSCT (Somatom Definition Flash, Siemens Healthcare, Forchheim, Germany) between January 2012 and February 2013 who had been referred to our department to rule out CAD were included in this study.
At our institution, we apply the prospectively ECG-triggered high-pitch spiral in cases in which only cardiac and coronary morphology is of interest and a regular heart rate with <55 bpm can be established. We use the prospectively ECG-triggered sequential mode if the heart rate even after betablocker application remains above 55 bpm but below 70 bpm or if the heart rhythm is not completely regular. Hence, both scan modes are mostly used in outpatients. We use the retrospectively ECG-gated spiral acquisition in dual-energy mode in patients referred to us from the emergency department to evaluate wall motion and myocardial perfusion at the same time with coronary morphology. This scan mode is applied only to a heart rate of up to 70 bpm since the temporal resolution is limited to 140 ms. Above a heart rate of 70 bpm or in case of unstable heart rhythm, the conventional retrospectively ECG-gated dual-source spiral acquisition mode is used in emergency room patients as well as in patients referred to cardiac CT with the dedicated question for functional analysis.
Retrospective database analysis revealed that in this time span 25 patients had been examined using a prospectively ECG-triggered protocol in high-pitch spiral mode, thus representing the smallest group in terms of patient numbers. Hence, to improve comparability of data, 25 patients in the other three groups were randomly selected out of the total cohort.
Therefore, we included a total of 100 patients who underwent cCTA on the same second-generation DSCT between January 2012 and February 2013 at our institution to rule out CAD. There was no preselection of patients based on image quality, heart rate, body habitus or other parameters. However, we excluded patients with coronary bypasses as the included anatomic range would have been larger in these patients with a consecutively higher estimated dose. Previously implanted stents, valve prosthesis or pacemakers were not regarded as exclusion criteria. However, segments with a diameter below 1.5 mm, stented segments with an inner stent diameter <3 mm and vessel segments distal to occlusions were excluded from subjective image quality analysis.
Image acquisition
If no contraindications to β-blockers were present and the heart rate was above 65 bpm (beats per minute), Metoprolol tartrate (Beloc, AstraZeneca, Wedel, Germany) was administered intravenously in fractions of 5 mg up to a maximum dose of 20 mg prior to the examination. In addition, two sublingual pumps of glyceryl trinitrate (Nitrolingual N-Spray, G. Pohl-Boskamp GmbH, Hohenlockstedt, Germany) were administered if no contraindications were present.
During all cCTA examinations, contrast material was injected via the right cubital vein at a flow rate of 5 mL/s using the same tri-phasic contrast material injection protocol [13]. First, a 70 mL bolus of iodinated contrast material (iomeprol; Imeron® 400, Bracco Imaging, Konstanz, Germany) was injected, followed by a mixed second bolus (50 mL of a 30 % contrast and 70 % saline solution) and a final third phase (50 mL of a pure NaCl bolus). The test bolus technique (a bolus of 15 mL of contrast material and 30 mL of NaCl bolus) was used to determine the scan delay time for the angiographic phase.
Images were acquired in craniocaudal direction in inspiratory breath hold. The anatomic range was manually adjusted and confined to the heart as seen on the anterior-posterior and lateral scout images.
The data set for the angiographic visualization of the coronary arteries for group 1 and 2 was acquired using a prospectively ECG-triggered protocol in either high-pitch spiral (group 1) or sequential (group 2) mode while data for groups 3 and 4 were acquired using a retrospectively ECG-triggered spiral protocol in either dual-energy (group 3) or dual-source (group 4) mode. Collimation was set to 128 × 0.6 mm for group 1, 2 and 4 and 2 × 64 × 0.6 mm for group 3. Pitch was set to 3.4 for group 1 and to 0.17 for group 3 and 4. The tube voltage was set to 100 kV for groups 1, 2, 4 and to 100/140 kV for group 3. The tube current time product was 370 mAs for groups 1 and 2, 165/140 mAs for group 3 and 320 mAs for group 4. The resulting average scan time was ~1 s for group 1 and ~8 s for groups 2–4.
For all examination protocols, automated dose modulation (CareDose, Siemens Healthcare) and tube modulation were enabled and z-flying focal spot technique was used. No iterative reconstruction techniques were activated in the used examination protocols to improve comparability. Rotation time was 0.28 s, matrix size was set to 512 × 512, and field of view was ~18 cm.
Image reconstruction
All cCTA data were analyzed on a commercially available RIS/PACS system (Centricity, GE Healthcare, Dornstadt, Germany) using image series with a slice thickness of 0.75 mm and a reconstruction increment of 0.4 mm. A soft tissue kernel (B26f) and a dedicated CT algorithm for the selection of the phase of the cardiac cycle with the least motion artefacts (BestPhase, Siemens Healthcare) were used. Dual-energy CTA was reconstructed using the QCA hybrid algorithm combining high- and low-pass filtered data from the high- and low-energy spectra as described by Nance et al. [14] and linear blending with 60 % information of the 100 kV data set.
Estimation of the CT radiation dose
Patient protocols of all performed cCTA examinations were assessed and dose length product (DLP) and volume computed tomography index (CTDIvol) were recorded. The effective dose [ED (mSv)] was estimated using the method proposed by the European working group for guidelines on quality criteria in CT derived from the product of the DLP and a weighting factor of 0.017 mSv/mGy/cm [15].
As the electronic chart system of the hospital did not contain current data about the patients’ body weight at the day of the cCTA examination, the two largest axial thoracic diameters [anterior-posterior (AP) and right-to-left (LAT)] were measured in each patient to allow for comparison of body habitus as previously described [16]. In addition, size-specific dose estimates (SSDE) were calculated. First, the following formula was used to calculate the effective diameter:
A conversion factor based on the effective diameter and the 32 cm diameter phantom reference numbers provided by the AAPM report no. 204 was selected for each patient and SSDE was calculated using the following formula [17]:
Assessment of objective image quality
Objective image quality of the right (RCA) and left coronary artery (LCA) were evaluated using the region-of-interest (ROI) technique. Image noise, signal attenuation, contrast, signal-to-noise-ratio (SNR) and contrast-to-noise-ratio (CNR) were measured for both vessels: the ascending aorta and the interventricular cardiac septum. To ensure data consistency, each ROI measurement was performed three times and mean values were calculated. Image noise was defined as the standard deviation (SD) measured in an ROI placed in the area in front of the sternum of the patient.
Intraluminal coronary artery signal attenuation was measured by placing ROIs centrally in the proximal segments of the left main (LM), LAD, left circumflex (LCX) and RCA. In the ascending aorta, the ROI was placed approximately 3 cm cranial of the aortic valve. ROI circles were sized as large as possible without including the vessel wall. Based on these measurements, SNR and CNR were determined according to the following formulas:
-
A: SNR = attenuation in the ascending aorta/image noise
-
B: CNR = (attenuation in the ascending aorta−attenuation of the interventricular cardiac septum)/image noise
Evaluation of subjective image quality
According to the 15-segment model proposed by the American heart association [18], each coronary artery segment was evaluated regarding subjective quality by two observers with 3 and 4 years of experience in evaluating cCTA examinations. Both observers were blinded to the used cCTA protocol and patients’ clinical data. Image quality was assessed using a four-point rating scale ranging from 1 to 4 (1: excellent image quality; 2: acceptable, not compromising diagnostic image quality; 3: poor image quality for single coronary segments; 4: non-diagnostic). Segments with a diameter below 1.5 mm, stented segments with an inner stent diameter <3 mm and vessel segments distal to occlusions were excluded from analysis similar to prior studies [16].
Statistical analysis
Statistical analysis was performed using dedicated software (BiAS 9.08, Epsilon Verlag, Frankfurt, Germany). Patient age, heart rate, measured thoracic diameters, attenuation values, SNR, CNR, CTDI, SSDE, DLP and ED are expressed as mean values ± standard deviations. To test for rejection of the null hypothesis of random distribution, comparison of these variables from all four groups was performed using the analysis of variance test (ANOVA). In the event of statistical significance of the global F test, pairwise comparison was performed with the student t test for unpaired samples. A p value of <0.05 was considered statistically significant.
The inter-rater agreement between the two observers regarding the evaluation of subjective image quality was calculated using Cohen’s kappa (κ). The kappa value was interpreted in the following way: κ < 0.20 = slight agreement, κ: 0.21–0.40 = fair agreement, κ: 0.41–0.60 = moderate agreement, κ: 0.61–0.80 = substantial agreement, κ: 0.81–1.0 = almost perfect agreement.
Results
Patient characteristics
A total of 100 patients were evaluated in the study. The mean heart frequency during the examination for the various study groups was as follows: group 1 = 53 ± 2 bpm; group 2 = 63 ± 5 bpm; group 3 = 64 ± 4 bpm; group 4 = 81 ± 12 bpm. Average patient age was 69 ± 13 years in group 1, 57 ± 12 years in group 2, 67 ± 8 years in group 3, and 65 ± 11 years in group 4. Groups 1 and 4 consisted of 24 % female patients (n = 6) while group 2 included eight females (32 %) and group 3 included five females (20 %). Mean thoracic diameters as a measure of body habitus showed several significant differences (anterior–posterior: group 1 = 370 ± 46 mm; group 2 = 348 ± 38 mm; group 3 = 248 ± 21 mm; group 4 = 260 ± 58 mm; p < 0.05 for group 1 vs. 3, group 1 vs. 4, group 2 vs. 3, and group 2 vs. 4; all others: n/s; right-to-left: group 1 = 345 ± 31 mm; group 2 = 354 ± 37 mm; group 3 = 265 ± 34 mm; group 4 = 264 ± 55 mm; p < 0.05 for group 1 vs. 3, group 1 vs. 4, group 2 vs. 3, and group 2 vs. 4; all others: n/s).
Comparison of objective image quality
All results from the analysis of objective image quality are summarized in Table 1. The image noise did not show any significant differences between the different study groups (group 1: 16.6 ± 5.4; group 2: 15.2 ± 4.4; group 3: 18.0 ± 9.4; group 4: 24.5 ± 22.0; p > 0.91). Statistical differences regarding the measured attenuation for the ascending aorta and both right and left coronary artery were all significant (p < 0.01). The CNR and SNR values for the coronary vessels consistently both peaked in group 2 (CNR RCA: 22.5 ± 8.8; CNR LCA: 23.6 ± 8.8; SNR RCA: 29.2 ± 10.3; SNR LCA: 30.2 ± 10.3) followed by group 1 (CNR RCA: 20.2 ± 8.3; CNR LCA: 21.0 ± 8.4; SNR RCA: 26.0 ± 9.1; SNR LCA: 26.7 ± 9.5). Differences between both groups were consistently statistically non-significant (p ≥ 0.40).
Comparison of subjective image quality
A total of 1500 coronary artery segments with a vessel diameter of at least 1.5 mm were evaluated by both observers. An overall diagnostic image quality was found in 98.67 % of all segments (1480) while 1.33 % of all segments (20) were non-evaluative. Further results from the assessment of subjective image quality are summarized in Table 2. The inter-rater agreement for subjective image quality was excellent (κ = 0.944). We observed no significant difference regarding the diagnostic image quality between the different examination protocols (p > 0.05 for all comparisons).
CT radiation dose
The resulting radiation dose parameters for the examined study groups are summarized in Table 2. The mean estimated radiation dose was 1.27 ± 0.62 mSv for group 1, 2.04 ± 0.94 mSv for group 2, 3.97 ± 1.29 mSv for group 3, and 8.11 ± 4.95 mSv for group 4. Differences in estimated dose between the different groups were all statistically significant (p < 0.01). The mean estimated radiation dose of all 100 patients examined using the same DSCT was 3.85 ± 3.70 mSv.
Discussion
In this study, we found that prospectively ECG-gated protocols for second-generation dual-source cCTA result in significantly lower radiation exposure compared to retrospectively ECG-gated protocols. Nevertheless, all evaluated protocols showed consistently high objective and subjective image quality. In patients requiring functional analysis of the complete cardiac cycle, dual-energy spiral acquisition should be preferred over dual-source spiral mode to reduce radiation exposure.
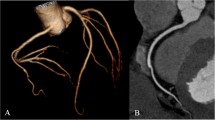
We focused on retrospectively comparing four available cCTA protocols on a second-generation DSCT in clinical routine. Due to the study design, the resulting estimated radiation doses differed significantly between the groups and protocols and were lowest in the group examined using the prospectively ECG-gated high-pitch spiral protocol with a mean dose of 1.27 mSv. Figure 1 demonstrates a patient examined using this protocol. Achenbach et al. [19] demonstrated that high-pitch spiral acquisition for cCTA may result in even lower mean radiation doses of 0.87 mSv. Several recent publications have investigated new techniques to even further reduce the resulting dose of high-pitch spiral acquisition cCTA. The combination with iterative reconstruction techniques for cCTA has been demonstrated to allow for dose reduction down to 0.58 mSv [20] or even below 0.1 mSv [21]. While these studies show that there is still potential for further dose savings, the patient groups that these protocols can be applied to are limited and not representative for clinical routine. A very low and regular heart rate remains essential for dose-saving scan techniques because otherwise motion artifacts will deteriorate image quality. For patients with moderately higher heart rates up to 70 bpm or slight arrhythmia, the prospectively ECG-gated sequential acquisition mode is a useful alternative to high-pitch spiral acquisition as it also significantly reduces radiation exposure compared to retrospectively ECG-gated protocols. We found a mean dose of 2.04 mSv using this protocol in our study. Our findings are consistent with values from prior studies investigating this technique as Kim et al. [22] reported a mean dose of 1.75 mSv and Jeong et al. [23] reported 1.94 mSv. Figure 2 demonstrates a case examined with this protocol.
A 66-year-old male outpatient with a history of hypercholesterolemia and intermittent chest pain referred for coronary CT angiography. Patient showed a stable sinus rhythm with 53 bpm after betablockers had been administered. Thus, prospectively ECG-gated high-pitch spiral protocol was chosen for coronary CT angiography. Curved multiplanar reconstructions (Aquarius iNtuition, TeraRecon, Foster City, CA, USA) show patent coronary arteries with no signs of coronary artery disease
A 58-year-old male outpatient with a history of type-2 diabetes referred for coronary CT angiography due to suspected coronary artery disease. Patient showed a stable sinus rhythm with 66 bpm after betablockers had been administered. Therefore, a prospectively ECG-synchronized sequential protocol was selected. Axial arterial (a) and curved multiplanar reconstructions (b) (Aquarius iNtuition, TeraRecon, Foster City, CA) demonstrate a high-grade stenosis of the left anterior descending artery proximal to a large intravascular calcification (big arrows). Furthermore, there is complete occlusion of the first diagonal branch (small arrows). Additional invasive coronary angiography confirmed both findings in this patient (c) with severe 3-vessel coronary artery disease who later underwent coronary artery bypass grafting
Retrospectively ECG-gated spiral acquisition protocols are still commonly used for cCTA in clinical routine [8, 9]. The results of our study demonstrate that performing the examination in dual-energy mode allows for significant dose reductions compared to the dual-source mode. This finding is in accordance with the results of a previous study by Kerl et al. [16] comparing dual-energy to dual-source cCTA with first-generation dual-source CT. The retrospectively ECG-gated dual-energy spiral mode allows for functional analysis of the left ventricle as well as the display of myocardial iodine distribution as a measure of myocardial perfusion and thus detection of myocardial ischemia [24, 25]. In addition, late enhancement dual-energy acquisition can provide auxiliary information about chronic myocardial infarction [26]. Therefore, especially in patients with a high likelihood for perfusion abnormalities or chronic ischemic changes, the use of dual-energy acquisition may be beneficial. Hence, this is our preferred examination mode in emergency room patients referred for evaluation of acute chest pain. Figure 3 demonstrates a case with acute occlusion of the left anterior descending artery and corresponding dual-energy perfusion images. However, DECT requires a low and stable heart rate since the temporal resolution with 140 ms is significantly lower than with the dual-source mode (75 ms). Therefore, we use the conventional dual-source spiral mode with retrospective ECG-gating in patients with heart rates above 70 bpm in whom functional analysis is required. Figure 4 demonstrates a case in which retrospectively gated DSCT spiral acquisition was selected due to atrial fibrillation and a coronary aneurysm was detected.
A 80-year-old male patient referred by the emergency department with acute chest pain and inconclusive electrocardiographic findings and laboratory results. Patient was clinically stable during preparation for CT imaging and showed a stable sinus rhythm of 69 bpm and was, therefore, examined using a retrospectively ECG-gated dual-energy protocol. Axial images (a) demonstrate a complete occlusion of the left anterior descending artery (big arrow) and curved multiplanar reconstructions (b) (Aquarius iNtuition, TeraRecon, Foster City, CA, USA) furthermore depict multiple intracoronary calcifications. Dual-energy perfusion images (c) reconstructed on a dedicated workstation (HeartPBV, Siemens Healthcare) show a perfusion deficit (big arrow) in the corresponding vessel territory. Invasive coronary angiography (d) confirmed the total occlusion of the left anterior descending artery (big arrow). The patient underwent invasive reperfusion and stenting in multiple coronaries due to severe 3-vessel coronary artery disease
A 66-year-old male patient referred for coronary CT angiography due to suspected coronary anomaly based on prior transthoracic echocardiographic findings. As the patient had been diagnosed with chronic atrial fibrillation and presented with a heart rate of 96 bpm, a retrospectively ECG-synchronized dual-source acquisition technique was selected. Images from CT coronary angiography show a high diagnostic image quality with no evident motion artifacts. Axial scans (a) demonstrate an aneurysm of the left circumflex artery (big arrow). Images from curved multiplanar reconstructions (b, c) and virtual rendering techniques (d) (both Aquarius iNtuition, TeraRecon, Foster City, CA, USA) improve depiction of the aneurysm (big arrows)
As cardiac DSCT can provide accurate and reproducible assessment of left and right ventricular function in comparison with magnetic resonance imaging [27, 28], retrospectively ECG-gated acquisition protocols for cCTA are still commonly used to gain information of the full cardiac cycle although the resulting dose is higher compared to prospectively ECG-gated protocols. Seneviratne et al. [29] also highlighted the importance of assessing left ventricular function as it may improve the diagnostic accuracy for acute coronary syndrome in patients with acute chest pain. Takx et al. [30] demonstrated that prospectively ECG-triggered cardiac DSCT may permit accurate quantification of left and right ventricular function and reported a mean radiation dose of 6.2 ± 1.8 mSv for this technique. In our present study, retrospectively ECG-gated dual-energy acquisition resulted in a mean radiation dose of 3.96 ± 1.16 mSv. Therefore, in our opinion, dual-energy cCTA currently remains a reliable, dose-saving protocol which allows for retrospectively ECG-gated analysis of left and right ventricular function.
The results of this study should be interpreted in the context of the study design and consequent limitations. First, the size of the examined study groups is limited. However, our results are comparable to those of similar previous studies analyzing estimated dose and objective image quality for cCTA using DSCT [3, 5, 16]. Second, patient weight was not recorded and, therefore, measured horizontal and vertical thoracic diameters were compared as described in previous studies [16]. However, the mean thoracic diameters were largest in the groups examined using prospectively ECG-gated data acquisition protocols which also resulted in the lowest estimated dose. Therefore, the dose-saving effects of prospectively ECG-gated protocols might be even more distinct in a more diversified study population. Third, severity of CAD was neither documented nor compared as it was not aim of this study and did not interfere with any measurement of objective image quality in this study determined by the observers. Fourth, iterative reconstruction techniques were not used, as this was not goal of the study and differences between the various iterative reconstruction techniques may have compromised the comparability of image quality. However, prior studies have demonstrated that iterative reconstruction allows for noise reduction and hence improvement of image quality and potentially reduction of radiation dose [20, 31].
In conclusion, our results demonstrate that prospectively ECG-gated cCTA protocols result in significantly less radiation dose exposure than retrospectively ECG-gated DSCT protocols in a clinical routine setting. All assessed second-generation DSCT protocols showed consistently high objective and subjective image quality. If data of the full cardiac cycle are required, e.g., for functional analysis, the dual-energy spiral acquisition mode should be preferred in patients with low and regular heart rate over the dual-source mode as it results in significant dose reduction without compromising diagnostic image quality.
Abbreviations
- CAD:
-
Coronary artery disease
- cCTA:
-
Coronary computed tomography angiography
- CNR:
-
Contrast-to-noise-ratio
- CTDIvol :
-
Volume computed tomography index
- DECT:
-
Dual-energy computed tomography
- DLP:
-
Dose length product
- DSCT:
-
Dual-source computed tomography
- ECG:
-
Electrocardiogram
- LCA:
-
Left coronary artery
- RCA:
-
Right coronary artery
- ROI:
-
Region of interest
- SD:
-
Standard deviation
- SNR:
-
Signal-to-noise-ratio
References
Budoff MJ, Achenbach S, Blumenthal RS, Carr JJ, Goldin JG, Greenland P et al (2006) Assessment of coronary artery disease by cardiac computed tomography: a scientific statement from the American heart association committee on cardiovascular imaging and intervention, council on cardiovascular radiology and intervention, and committee on cardiac imaging, council on clinical cardiology. Circulation 114:1761–1791
Hendel RC, Patel MR, Kramer CM, Poon M, Hendel RC, Carr JC et al (2006) ACCF/ACR/SCCT/SCMR/ASNC/NASCI/SCAI/SIR 2006 appropriateness criteria for cardiac computed tomography and cardiac magnetic resonance imaging: a report of the American College of Cardiology Foundation Quality Strategic Directions Committee Appropriateness Criteria Working Group, American College of Radiology, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, American Society of Nuclear Cardiology, North American Society for Cardiac Imaging, Society for Cardiovascular Angiography and Interventions, and Society of Interventional Radiology. J Am Coll Cardiol 48:1475–1497
Leschka S, Stolzmann P, Desbiolles L, Baumueller S, Goetti R, Schertler T et al (2009) Diagnostic accuracy of high-pitch dual-source CT for the assessment of coronary stenoses: first experience. Eur Radiol 19:2896–2903
Paul J-F, Abada HT (2007) Strategies for reduction of radiation dose in cardiac multislice CT. Eur Radiol 17:2028–2037
Alkadhi H, Stolzmann P, Scheffel H, Desbiolles L, Baumüller S, Plass A et al (2008) Radiation dose of cardiac dual-source CT: the effect of tailoring the protocol to patient-specific parameters. Eur J Radiol 68:385–391
Rist C, Johnson TR, Müller-Starck J, Arnoldi E, Saam T, Becker A et al (2009) Noninvasive coronary angiography using dual-source computed tomography in patients with atrial fibrillation. Invest Radiol 44:159–167
Alkadhi H, Scheffel H, Desbiolles L, Gaemperli O, Stolzmann P, Plass A et al (2008) Dual-source computed tomography coronary angiography: influence of obesity, calcium load, and heart rate on diagnostic accuracy. Eur Heart J 29:766–776
Woodard PK (2005) Science to practice: can multi-detector row spiral CT be used to assess left ventricular function? Radiology 236:1–2
Juergens KU, Fischbach R (2006) Left ventricular function studied with MDCT. Eur Radiol 16:342–357
Flohr TG, McCollough CH, Bruder H, Petersilka M, Gruber K, Süss C et al (2006) First performance evaluation of a dual-source CT (DSCT) system. Eur Radiol 16:256–268
Stolzmann P, Scheffel H, Schertler T, Frauenfelder T, Leschka S, Husmann L et al (2008) Radiation dose estimates in dual-source computed tomography coronary angiography. Eur Radiol 18:592–599
Chen H, Fang X, Hu X, Bao J, Hu C, Chen Y et al (2010) Efficacy of dual-source CT coronary angiography in evaluating coronary stenosis: initial experience. Clin Imaging 34:165–171
Kerl JM, Ravenel JG, Nguyen SA, Suranyi P, Thilo C, Costello P et al (2008) Right heart: split-bolus injection of diluted contrast medium for visualization at coronary CT angiography. Radiology 247:356–364
Nance JW Jr, Bastarrika G, Kang DK, Ruzsics B, Vogt S, Schmidt B et al (2011) High-temporal resolution dual-energy computed tomography of the heart using a novel hybrid image reconstruction algorithm: initial experience. J Comput Assist Tomogr 35:119–125
Huda W, Ogden KM, Khorasani MR (2008) Converting dose-length product to effective dose at CT. Radiology 248:995–1003
Kerl JM, Bauer RW, Maurer TB, Aschenbach R, Korkusuz H, Lehnert T et al (2011) Dose levels at coronary CT angiography—a comparison of dual Energy-, dual Source- and 16-slice CT. Eur Radiol 21:530–537
Boone J, Strauss K, Cody D, McCollough CH, McNitt-Gray MF, Toth TL, et al. (2011) Size-specific dose estimates (SSDE) in pediatric and adult body CT examinations. Report of Am. Assoc. Phys. Med. AAPM Task Group 204. College Park, Md: American Association of Physicists in Medicine
Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK et al (2002) Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 105:539–542
Achenbach S, Marwan M, Ropers D, Schepis T, Pflederer T, Anders K et al (2010) Coronary computed tomography angiography with a consistent dose below 1 mSv using prospectively electrocardiogram-triggered high-pitch spiral acquisition. Eur Heart J 31:340–346
Yin W-H, Lu B, Hou Z-H, Li N, Han L, Wu Y-J et al (2013) Detection of coronary artery stenosis with sub-milliSievert radiation dose by prospectively ECG-triggered high-pitch spiral CT angiography and iterative reconstruction. Eur Radiol 23:2927–2933
Schuhbaeck A, Achenbach S, Layritz C, Eisentopf J, Hecker F, Pflederer T et al (2013) Image quality of ultra-low radiation exposure coronary CT angiography with an effective dose <0.1 mSv using high-pitch spiral acquisition and raw data-based iterative reconstruction. Eur Radiol 23:597–606
Kim JS, Choo KS, Jeong DW, Chun KJ, Park YH, Song SG et al (2011) Step-and-shoot prospectively ECG-gated vs. retrospectively ECG-gated with tube current modulation coronary CT angiography using 128-slice MDCT patients with chest pain: diagnostic performance and radiation dose. Acta Radiol 52:860–865
Jeong DW, Choo KS, Baik SK, Kim YW, Jeon UB, Kim JS et al (2011) Step-and-shoot prospectively ECG-gated versus retrospectively ECG-gated with tube current modulation coronary CT angiography using the 128-slice MDCT: comparison of image quality and radiation dose. Acta Radiol 52:155–160
Ruzsics B, Lee H, Zwerner PL, Gebregziabher M, Costello P, Schoepf UJ (2008) Dual-energy CT of the heart for diagnosing coronary artery stenosis and myocardial ischemia-initial experience. Eur Radiol 18:2414–2424
Meinel FG, De Cecco CN, Schoepf UJ, Nance JW Jr, Silverman JR, Flowers BA et al (2014) First-arterial-pass dual-energy CT for assessment of myocardial blood supply: do we need rest, stress, and delayed acquisition? comparison with SPECT. Radiology 270:708–716
Wichmann JL, Bauer RW, Doss M, Stock W, Lehnert T, Bodelle B et al (2013) Diagnostic accuracy of late iodine-enhancement dual-energy computed tomography for the detection of chronic myocardial infarction compared with late gadolinium-enhancement 3-T magnetic resonance imaging. Invest Radiol 48:851–856
Maffei E, Messalli G, Martini C, Nieman K, Catalano O, Rossi A et al (2012) Left and right ventricle assessment with cardiac CT: validation study vs. cardiac MR. Eur Radiol 22:1041–1049
Arraiza M, Azcárate PM, De Cecco CN, Viteri G, Simón-Yarza I, Hernández-Estefanía R et al (2012) Assessment of left ventricular parameters in orthotopic heart transplant recipients using dual-source CT and contrast-enhanced echocardiography: comparison with MRI. Eur J Radiol 81:3282–3288
Seneviratne SK, Truong QA, Bamberg F, Rogers IS, Shapiro MD, Schlett CL et al (2010) Incremental diagnostic value of regional left ventricular function over coronary assessment by cardiac computed tomography for the detection of acute coronary syndrome in patients with acute chest pain: from the ROMICAT trial. Circ Cardiovasc Imaging 3:375–383
Takx RAP, Moscariello A, Schoepf UJ, Barraza JM Jr, Nance JW Jr, Bastarrika G et al (2012) Quantification of left and right ventricular function and myocardial mass: comparison of low-radiation dose 2nd generation dual-source CT and cardiac MRI. Eur J Radiol 81:e598–e604
Renker M, Nance JW Jr, Schoepf UJ, O’Brien TX, Zwerner PL, Meyer M et al (2011) Evaluation of heavily calcified vessels with coronary CT angiography: comparison of iterative and filtered back projection image reconstruction. Radiology 260:390–399
Conflict of interest
Ralf W. Bauer and J. Matthias Kerl are on the speakers’ bureau of Siemens Healthcare, Computed Tomography division. However, both co-authors did not analyze or control any data in this study. All other authors have nothing to disclose.
Ethical standards
This retrospective study was approved with waiver of the requirement for informed consent.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wichmann, J.L., Hu, X., Engler, A. et al. Dose levels and image quality of second-generation 128-slice dual-source coronary CT angiography in clinical routine. Radiol med 120, 1112–1121 (2015). https://doi.org/10.1007/s11547-015-0546-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-015-0546-9