Abstract
Serum uric acid (SUA) level was shown in various studies to be related to the presence of coronary artery disease and subsequent cardiovascular events. The aim of the present study was to evaluate the association of SUA with SYNTAX score II (SSII) and the long-term prognosis of patients with stable angina pectoris who underwent percutaneous revascularization due to multivessel disease (MVD) and/or unprotected left main disease (UPLMD). Two-hundred and ninety patients with MVD and/or UPLMD who were treated consecutively with percutaneous coronary intervention (PCI) were included in the present study. The study population was divided into high SSII (n: 145; SSII > 32.9) and low SSII (n: 145; SSII ≤ 32.9) according to the median SSII value. The SUA value was significantly higher in the high SSII group than in the low SSII group (5.53 ± 1.95 vs. 6.07 ± 1.88; p = 0.001) and was found to be an independent predictor of high SSII (OR 1.306; 95% CI 1.119–1.525; p = 0,001). Twenty-eight patients (9.7%) died during the long-term follow-up, and SUA and SSII were additionally found to be independent predictors of long-term mortality (HR 1.245, 95% CI 1.046–1.482, p = 0.014; HR 1.042, 95% CI 1.007–1.079, p = 0.018, respectively). In the present study, SUA level was demonstrated to be associated with high SSII and long-term mortality in patients with MVD and/or UPLMD who were treated with PCI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Serum uric acid (SUA) is the end-product of endogenous and exogenous purine metabolism. UA appears to be a proinflammatory marker and has been shown to induce the release of IL-1β, IL-6, TNF-α, and MCP-1 [1, 2] and to stimulate oxidative stress, endothelial dysfunction, and vasoconstriction [3]. Its inflammatory role in the pathophysiology of atherosclerosis was previously shown [4]. The relationship between SUA and the presence of coronary artery disease (CAD) and subsequent cardiovascular events was also demonstrated in various studies [5,6,7]. Furthermore, SUA was shown to be associated with SYNTAX score (SS), which indicates the severity of CAD according to the number of lesions as well as their functional effects, location, and complexity [8, 9]. In addition, the association of SUA with SYNTAX score II (SSII), was reported to have a better predictive performance in terms of prognostic accuracy compared to SS, [10, 11] and the long-term prognosis of patients with multivessel disease (MVD) and/or unprotected left main disease (UPLMD) who have undergone successful percutaneous revascularization is unclear.
The purpose of this study was to investigate the relationship between SUA and SSII and to determine the effect of SUA levels on long-term prognosis in patients with complex CAD who have undergone successful percutaneous coronary artery intervention.
Methods
Study design and population
A total of 331 patients with stable angina pectoris who were evaluated by stress imaging tests and who underwent coronary angiography and subsequent percutaneous coronary intervention (PCI) from January 2014 to June 2015 in our clinics, Turkey, were retrospectively enrolled in the study. All study subjects had newly diagnosed MVD and/or UPLMD and had undergone PCI based on the decision of the heart team. In addition, all subjects enrolled in this study were completely revascularized and had a post PCI residual SS of zero. A total of 41 patients were excluded for various reasons: 5 patients died during the procedure; 12 patients referred to elective CABG were excluded because of the failure of PCI; and 24 patients had inconclusive clinical data from hospital files and computer records, so the SSII was unable to be calculated. The remaining 290 patients who were successfully treated with PCI constituted the study population. All PCIs were performed by two experienced senior interventionalists using standard practices in our Catheter Laboratory (femoral access). Interventional strategies such as stent selection and medical treatment were left to the discretion of the treating operator. Angiographic success was defined as a residual stenosis of less than 20% in the presence of TIMI 3 flow. Hospital records indicated that all patients were treated according to current guidelines and standard CAD treatment, including aspirin, clopidogrel, enoxaparin or unfractionated heparin, beta-blockers, angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, and statins. The standard drug regimen after discharge is aspirin, clopidogrel, angiotensin-converting enzyme inhibitor or angiotensin receptor blocker, B-blocker, statin therapy, and spironolactone according to the New York Heart Association functional class or left ventricular ejection fraction (LVEF). Long-term follow-up data on the patients were gathered from follow-up visits, in-hospital records, or telephone calls. To determine the current status of patients who could not be reached by telephone, records from the Birth Registration Office and Statistical Institute were thoroughly examined. The study protocol was reviewed and approved by the Local Ethics Committee of Kafkas University in accordance with the Declaration of Helsinki.
Data collection
Baseline clinical and demographic characteristics and patients’ medical history were obtained from hospital records. Complete blood counts and blood biochemical parameters were measured in all patients on admission. Estimated glomerular filtration rate (eGFR) was determined using the Cockroft–Gault formula from blood samples obtained on admission. LVEF was assessed using a modified Simpson’s method. SUA plasma concentrations were measured using a Roche Diagnostics Cobas 8000 c502 analyzer according to manufacturer protocol.
Angiographic analysis
All patients underwent selective coronary angiography using the Judkins percutaneous transfemoral technique. Coronary angiograms were digitally recorded for quantitative analysis (Dicom-viewer; MedCom GmbH, Darmstadt, Germany). Digital angiograms were then analyzed by two independent and experienced interventional cardiologists who were blinded to all data. In case of disagreement, the final decision was made by consensus with a third independent cardiologist. Each lesion with a diameter of ≥ 1.5 mm and ≥ 50% stenosis was scored using the online SS Calculator, version 2.1 [9, 12]. SSII was calculated using an online calculator considering two anatomical variables (SS and LMCA disease) and six clinical variables (age, gender, chronic obstructive pulmonary disease [COPD], peripheral arterial disease [PAD], and creatinine clearance [LVEF]) [13].
Statistical analysis
SPSS version 22.0 (Inc, Chicago, Illinois) was used for statistical analysis. Given the data distribution characteristics and normality, means (± standard deviation) or medians (0.25–0.75 percentile) were used to express continuous variables, and t-tests or Mann–Whitney U-tests were performed for group comparisons. Categorical variables were reported as numbers (percentages) and compared to the Fisher exact or χ2 test. Pearson coefficients were calculated to assess correlations between continuous variables. The Kaplan–Meier method was used to generate event-free survival curves, and the log-rank test was used to compare the difference in survival between SSII and SUA. Univariate and multivariate Cox proportional hazards analysis was used to identify risk factors for all-cause mortality. The receiver operating curve (ROC) was utilized to derive the cut-off values of SSII and SUA for predicting all-cause mortality. A p-value of < 0.05 indicated statistical significance.
Results
The study population consisted of 290 stable angina patients who had MVD and/or UPLMD (mean age: 62 ± 11 years; 80.3% males) and had undergone PCI. The mean SUA level was 5.66 ± 1.85. The mean SS score was 31.78 ± 13.19, and the mean SSII was 34.09 ± 10.02. The SSII of the patients ranged from 12.13 to 64.74 (median 32.9). The patients were divided into two groups according to the median SSII value: (a) low SSII (145 patients; SSII ≤ 32.9) and (b) high SSII (145 patients; SSII > 32.9). SUA level was significantly higher in patients with high SSII compared to patients with lower SSII (6.07 ± 1.88 vs. 5.53 ± 1.95; p = 0.001). Patients with high SSII were older, had a more frequent history of hypertension (HT), PAD, and COPD, and also had a higher percentage of LMCA disease and MVD compared to those with low SSII. Furthermore, compared to patients with lower SSII, patients with high score had a higher body mass index, higher SS, and lower eGFR. Demographic, clinical, laboratory, and coronary angiographic characteristics of patients with high SSII, patients with low SSII, and all patients are listed in Table 1.
Multivariate logistic regression analysis was used to determine the independent predictors of high SSII. Body mass index, HT, prior usage of angiotensin-converting enzyme inhibitor or angiotensin II receptor blocker, and SUA levels were found to be independent predictors of high SSII (Table 2).
Pearson’s correlation analysis showed a positive weak correlation between SUA levels and SSII and between SUA levels and SS (p < 0.001, r = 0.340 and p < 0.001, r = 0.240, respectively). When male and female patients were evaluated separately, a positive correlation between SUA levels and SSII and between SUA levels and SS was still present (p < 0.001, r = 0.336; p < 0.001, r = 0.245 and p < 0.001, r = 0.341; p = 0.05, r = 0.255, respectively).
An analysis of the ROC curve was performed to determine the cut-off value of SUA for predicting high SSII (SSII > 32.9). A SUA value > 4.45 yielded an area under the curve (AUC) of 0.604 (95% CI 0.538–0.670; p = 0.001). Furthermore, a SUA value > 4.45 demonstrated a sensitivity of 82% and a specificity of 35% in predicting high SSII (Fig. 1).
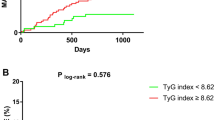
The mean follow-up time was 505 ± 13 days. Twenty-eight patients (9.7%) died during the long-term follow-up. Patients survivors and non-survivors were compared in terms of demographic, clinical, laboratory, and coronary angiographic characteristics (Table 3). Cox regression analyses were used to identify any association between the parameters and all-cause long-term mortality. SUA and SSII, which were associated with death in univariate analysis (HR 1.268, 95% CI 1.070–1.501, p = 0.006; HR 1.047, 95% CI 1.012–1.083, p = 0.008; respectively), were observed as independent predictors of long-term mortality in multivariate analysis (HR 1.245, 95% CI 1.046–1.482, p = 0.014; HR 1.042, 95% CI 1.007–1.079, p = 0.018, respectively). The optimal cut-off value for SUA was 5.7, yielding a sensitivity of 85.71% and a specificity of 40.46% (AUC: 0.650, 95% CI 0.544–0.757), and for SSII was 30.0, yielding a sensitivity of 82.14% and a specificity of 57.25% (AUC: 0.673, 95% CI 0.580–0.766) (Fig. 2).
ROC curves comparison to detect the best parameter in predicting long-term mortality. A > 5.7 cutoff value of SUA, with sensitivity of 85.71% and specificity of 40.46% (AUC: 0.650, 95% CI 0.544–0.757); SSII > 30.0, with sensitivity of 82.14% and specificity of 57.25% (AUC: 0.673, 95% CI 0.580–0.766); p = 0.771
Discussion
Our study demonstrated that SUA level was an independent predictor of high SSII in patients who underwent PCI because of multivessel and/or LMCA disease. Additionally, SUA level was associated with long-term mortality and was an independent predictor of long-term mortality.
The functional severity as well as the anatomical complexity of CAD are closely correlated with long-term outcomes [14]. This appears to apply to all patients who have been diagnosed, monitored by medical treatment, and treated with invasive therapy [15,16,17]. On this basis, several angiographic scoring systems have been devised to quantify the complexity of CAD [18,19,20,21,22,23]. The SS was recently developed angiographic scoring systems that indicate the severity of CAD according to the number of lesions as well as their localization, functional effects, and complexity [9]. Patients at highest risk of adverse events can be determined according to the SS score independently of clinical presentation; higher SS scores indicate a worse clinical prognosis [24]. The findings of the SYNTAX trial, which incorporated clinical variables (age, gender, presence of COPD and PAD, eGFR, LVEF) and anatomical variables (SS and presence of LMCA disease) using a Cox proportional hazards model, supported the creation of the SSII scoring system [13]. Campos et al. [10] investigated the predictive performance of SSII compared with SS; SSII was found to have more robust prognostic accuracy in real-world MVD and/or UPLMD cases. Consistent with the abovementioned studies, the SSII was found to be an independent predictor of 1-year mortality in our study.
Although the prognostic effect of SSII has been proven in previous studies, there is currently no common cut-off value. For this reason, our patient population was divided into two groups based on median SSII value to reveal parameters that could be related to high SSII. For the first time in the literature, elevated SUA level was significantly associated with high SSII according to univariate and multivariate analyses. This new observation could be explained by the close relationship between the parameters of SSII and those of SUA. The association of SUA with atherosclerosis and CAD was previously demonstrated [25]. However, there is conflicting information on the relationship between CAD severity (determined by different methods) and SUA [26,27,28]. Similar to the study conducted by Ekici et al. [29], SUA levels were associated with SS. Also, prior history of HT and clinical variables of SSII, including age, reduced LVEF, and presence of COPD, PAD, or impaired renal function have been associated with elevated SUA. As the present study population was divided into two groups according to the best predictive value of SSII, as consistent with previous studies, high hemoglobin level and reduced eGFR were also associated with increased SUA level [30,31,32,33,34,35]. All of the abovementioned factors may contribute to the relationship between SSII and SUA, supporting the findings of our study.
One of the most important findings of the present study was that SUA level was associated with long-term mortality in PCI-treated patients. Previous studies have shown that SUA is associated with cardiovascular and all-cause mortality in patients with stable CAD [5, 36, 37]. However, in this study, SUA was shown to be associated for the first time with all-cause long-term mortality in patients with MVD and/or UPLMD treated with PCI. This result might stem from the close relationship between SUA and SII variables, including SS, age, reduced LVEF, and presence of COPD, PAD, and impaired renal function, which are associated with a worse prognosis.
Conclusion
The present study is the first to comprehensively evaluate the relationship between SUA levels and CAD severity using SSII. SSII was previously associated with a worse prognosis. In this study, we show that high SUA levels are significantly related to high SSII, and patients with high SUA levels had a worse prognosis in the long-term follow-up. Although our findings indicate that SUA levels can provide important prognostic information for patients with MVD and/or UPLMD who have undergone PCI, these findings must be validated in larger population studies.
Limitations
The limitations of this clinical study are its small number of patients and its retrospective observational nature. Additional data are needed to better understand the results and apply them in future treatments.
References
Kanellis J et al (2003) Uric acid stimulates monocyte chemoattractant protein-1 production in vascular smooth muscle cells via mitogen-activated protein kinase and cyclooxygenase-2. Hypertension 41(6):1287–1293
Johnson RJ et al (2005) A unifying pathway for essential hypertension. Am J Hypertens 18(3):431–440
Johnson RJ (2015) Why focus on uric acid? Curr Med Res Opin 31(suppl 2):3–7
Libby P. Ridker PM. Maseri A (2002) Inflammation and atherosclerosis. Circulation 105(9):1135
Fang J, Alderman MH (2000) Serum uric acid and cardiovascular mortality: the NHANES I epidemiologic follow-up study, 1971–1992. JAMA 283(18):2404–2410
Bos MJ et al (2006) Uric acid is a risk factor for myocardial infarction and stroke. Stroke 37(6):1503–1507
Zhu Y et al (2015) Serum cystatin C level is associated with carotid intima-media thickening and plaque. Scand J Clin Lab Invest 75(3):265–272
Yu J et al (2014) Association between serum uric acid level and the severity of coronary artery disease in patients with obstructive coronary artery disease. Chin Med J 127(6):1039–1045
Sianos G et al (2005) The SYNTAX Score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention 1(2):219–227
Campos CM et al (2014) Predictive performance of SYNTAX Score II in patients with left main and multivessel coronary artery disease. Circ J 78(8):1942–1949
Hayiroglu MI et al (2018) Predictive value of SYNTAX score II for clinical outcomes in cardiogenic shock underwent primary percutaneous coronary intervention; a pilot study. Int J Cardiovasc Imaging 34(3):329–336
SYNTAX Score calculator (2016) http://www.syntaxscore.com. SYNTAX working-group. Accessed December 2016
Farooq V et al (2013) Anatomical and clinical characteristics to guide decision making between coronary artery bypass surgery and percutaneous coronary intervention for individual patients: development and validation of SYNTAX score II. Lancet 381(9867):639–650
Piccolo R et al (2015) Stable coronary artery disease: revascularisation and invasive strategies. Lancet 386(9994):702–713
Emond M et al (1994) Long-term survival of medically treated patients in the Coronary Artery Surgery Study (CASS) Registry. Circulation 90(6):2645–2657
Min JK et al (2007) Prognostic value of multidetector coronary computed tomographic angiography for prediction of all-cause mortality. J Am Coll Cardiol 50(12):1161–1170
Vranckx P et al (2015) Clinical outcome of patients with stable ischaemic heart disease as compared to those with acute coronary syndromes after percutaneous coronary intervention. EuroIntervention 11(2):171–179
Iwakura K et al (2003) Association between hyperglycemia and the no-reflow phenomenon inpatients with acute myocardial infarction. J Am Coll Cardiol 41(1):1–7
Hamburger JN et al (1997) Recanalization of total coronary occlusions using a laser guidewire (the European TOTAL Surveillance Study). Am J Cardiol 80(11):1419–1423
Ellis SG et al (1990) Coronary morphologic and clinical determinants of procedural outcome with angioplasty for multivessel coronary disease. Implications for patient selection. Multivessel Angioplasty Prognosis Study Group. Circulation 82(4):1193–1202
Gensini GG (1983) A more meaningful scoring system for determining the severity of coronary heart disease. Am J Cardiol 51(3):606
Leaman DM et al (1981) Coronary artery atherosclerosis. Circulation 63(2):285–292
Brkovic V et al (2013) Additive prognostic value of the SYNTAX score over GRACE, TIMI, ZWOLLE, CADILLAC and PAMI risk scores in patients with acute ST-segment elevation myocardial infarction treated by primary percutaneous coronary intervention. Int J Cardiovasc Imaging 29(6):1215–1228
van Gaal WJ et al (2009) The Syntax score predicts peri-procedural myocardial necrosis during percutaneous coronary intervention. Int J Cardiol 135(1):60–65
Ishizaka N et al (2007) Higher serum uric acid is associated with increased arterial stiffness in Japanese individuals. Atherosclerosis 192(1):131–137
Qureshi AE, Hameed S, Noeman A (2013) Relationship of serum uric acid level and angiographic severity of coronary artery disease in male patients with acute coronary syndrome. Pak J Med Sci 29(5):1137
Gur M et al (2008) Relation of serum uric acid levels with the presence and severity of angiographic coronary artery disease. Angiology 59(2):166–171
Wheeler JG et al (2005) Serum uric acid and coronary heart disease in 9,458 incident cases and 155,084 controls: prospective study and meta-analysis. PLoS Med 2(3):e76
Ekici B et al (2015) The relationship between serum uric acid levels and angiographic severity of coronary heart disease. Kardiologia Polska (Polish Heart J) 73(7):533–538
Wang B, Lin L, Zhao C (2016) Related factors of serum uric acid in patients with primary hypertension and hyperhomocysteinemia. Clin Exp Hypertens 38(3):312–316
Miyaoka T et al (2014) Serum uric acid levels and long-term outcomes in chronic kidney disease. Heart Vessel 29(4):504–512
Kocak ND et al (2016) Serum uric acid levels and uric acid/creatinine ratios in stable chronic obstructive pulmonary disease (COPD) patients: are these parameters efficient predictors of patients at risk for exacerbation and/or severity of disease? Med Sci Monit 22:4169
Sotoda Y et al (2017) Association of serum uric acid levels with leg ischemia in patients with peripheral arterial disease after treatment. J Atheroscler Thromb 24:725–734
Gonzales GF, Tapia V (2015) Increased levels of serum γ-glutamyltransferase and uric acid on metabolic, hepatic and kidney parameters in subjects at high altitudes. J Basic Clin Physiol Pharmacol 26(1):81–87
Yamauchi Y et al (2017) Is serum uric acid independently associated with left ventricular mass index, ejection fraction, and B-type natriuretic peptide among female and male cardiac patients? Int Heart J 58(4):562–569
Niskanen LK et al (2004) Uric acid level as a risk factor for cardiovascular and all-cause mortality in middle-aged men: a prospective cohort study. Archives of internal medicine 164(14):1546–1551
Liese AD et al (1999) Association of serum uric acid with all-cause and cardiovascular disease mortality and incident myocardial infarction in the MONICA Augsburg cohort. Epidemiology 10:391–397
Acknowledgements
The authors thank http://www.metastata.com for their contributions to the statistical analysis and trial design.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Rights and permissions
About this article
Cite this article
Karabağ, Y., Rencuzogullari, I., Çağdaş, M. et al. Association of serum uric acid levels with SYNTAX score II and long term mortality in the patients with stable angina pectoris who undergo percutaneous coronary interventions due to multivessel and/or unprotected left main disease. Int J Cardiovasc Imaging 35, 1–7 (2019). https://doi.org/10.1007/s10554-018-1446-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-018-1446-6