Abstract
Prosthesis-patient mismatch (PPM) occurs when the effective orifice area of the prosthesis is too small in relation to the patient's body surface area. There are few data available on the frequency and prognostic impact of PPM after transcatheter aortic valve implantation (TAVI). Our aim was to determine the prevalence of PPM and to investigate its association with medium-term clinical course of patients undergoing TAVI. We included 185 patients undergoing TAVI (79 ± 5 years, 49% male, 98% CoreValve) between April-2008 and December-2014. The effective orifice area (EOA) was determined by transthoracic echocardiography prior and after the procedure. We defined PPM as indexed EOA ≤ 0.85 cm2/m2 (severe PPM if ≤ 0.65 cm2/m2). All cause death, stroke and hospitalization for heart failure were considered as major clinical events. 45 patients (24%) showed PPM (severe 11 patients, 6%). PPM was associated with a higher EuroSCORE (OR 1.06, IC 95% 1.01–1.12, p = 0.03), body surface area ≥ 1.72 m2 (OR 3.58, IC 95% 1.30–9.87, p = 0.01) and small aortic annulus (OR 0.73, IC 95% 0.55–0.92, p = 0.03); and severe PPM with small prostheses size (OR 17.79, IC 95% 1.87–169.78, p = 0.012). The mean event-free survival was 34 ± 26 months. Patients with severe PPM showed lower rates of event free survival than the rest of the series (52% vs. 84%, p = 0.04) at 34 months follow up. In our series, PPM was present in a quarter of the patients after TAVI. Higher EuroSCORE, smaller prosthesis size, larger body surface area and smaller aortic annulus diameter were associated with PPM. Severe PPM was an independent factor associated with major events at medium-term follow up.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Transcatheter aortic valve implantation (TAVI) is today an indisputable alternative to surgery in severe aortic stenosis patients with high or intermediate surgical risk, with initial success rates of 75–88% [1,2,3,4] and a good short- and long-term clinical course [5,6,7,8].
A potential complication of this procedure is prosthesis-patient mismatch (PPM), which is defined as the presence of a reduced effective prosthetic valve area in relation to patient’s body surface area, measuring significantly high transprosthetic gradients too. Recent consensus of experts have already approached the issue of mismatch and the most appropriate definition of it [9, 10].
Frecuency of PPM after surgical aortic prosthesis implantation is relatively high (20–70%), with lower incidence for severe PPM (2–20%) [11, 12], and it increases mortality for any reason by 31% [13, 14].
But PPM after TAVI is less studied and published results are less consistent. Recent studies [14], including Edwards [15] and CoreValve [16, 17] prosthesis, showed a lower PPM incidence comparing with surgical prostheses (24–48%; 8–18% for severe PPM) [14,15,16,17,18]. Moreover, severe PPM prognostic impact after TAVI is still under discussion, with conflicting results between studies showing lower survival [15, 16] and those which have not established significant differences in relation to PPM-free patients [14, 17]. Regarding the occurrence of major clinical events such as stroke or heart failure hospitalization after TAVI, no previous studies have reported PPM impact on them.
Therefore, our aim was to study the prevalence of PPM, to describe possible factors associated with PPM occurrence, as well as to investigate its relation with mid-term clinical course of patients undergoing TAVI.
Materials and methods
Design and population
This study is a retrospective analysis of a consecutive patient registry, in which the echocardiographic and clinical variables were prospectively collected in all patients. The inclusion period was from April 2008 to December 2014, made up of consecutive patients with symptomatic severe aortic stenosis and high surgical risk undergoing TAVI, in most cases using the CoreValve self-expandable system (Medtronic Inc, Irvine, California, USA).
All patients were studied with transthoracic echocardiogram (TTE) prior to prosthesis implantation, and 72 h after the procedure. Furthermore, basal clinical and demographic data were collected. Patients who didn´t undergo one or both studies were excluded.
Three study groups were established: mismatch-free, moderate mismatch, and severe mismatch. PPM was defined as an indexed effective orifice area (EOA) ≤ 0.85 cm2/m2, distinguishing between severe PPM for indexed EOA ≤ 0.65 cm2/m2 and moderate PPM for indexed EOA > 0.65 and ≤ 0.85 cm2/m2, according to previous consensus [11, 19]. Although some expert consensus has recommended different cut-off points for obese patients [9, 10], most of the previous PPM studies have not used them [11,12,13]. In our protocol, we decided not to use different cut points to standardize the comparison with the previous scientific literature.
The learning curve was defined as the initial patients treated in our institution with the presence of an external “proctor”, in order to acquire enough experience. Obesity was defined as the presence of a Body Mass Index (BMI) ≥ 30 kg/m2.
All patients gave their informed consent. The study protocol was approved by the Ethics Committee from Hospital Universitario Reina Sofía.
Echocardiographic study
Echocardiograms were performed with a Philips iE33 equipment (Philips Electronics, Eindhoven, The Netherlands). In all cases the assessment was performed by the same level III echocardiographist [20, 21]. Enough quality was ensured in all studies in order to perform reliable and reproducible measurements.
Valve annulus, aortic root, and ascending aorta diameters were determined in long-axis parasternal view in the same plane, in meso-systole for valve annulus and in diastole for the rest of parameters [19, 22]. The aortic annulus was measured from the non-coronary valve point of attachment to the right coronary valve point of attachment [22]. The aortic valve area was calculated using the continuity equation.
The EOA of implanted aortic prosthesis was calculated according to scientific guidelines [19]. The resulting area was indexed by body surface area, determined by Dubois formula [23, 25].
The following parameters were also evaluated: ejection fraction and left ventricle volumes using biplane Simpson formula; left ventricle telesystolic and telediastolic diameters, and septal and posterior wall thickness, in M mode; maximum and mean prosthesis gradient; possible mitral valve disease; and prosthetic regurgitation assessment.
Prosthesis size choice and implantation procedure
The candidate selection´s protocol and the implantation procedure were previously described by our group [24, 25].
The prosthesis size choice was based on aortic annulus measurement by transesophageal echocardiography, cardiac tomography (CT), and aortography [25]. In case of doubts and/or complications [26] an intraprocedure transesophageal echocardiography was performed.
Implantation was carried out through femoral arterial access, under general anesthesia [27].
Follow-up
Follow-up after hospital discharge was based on three complementary methods: visits to the cardiology outpatient clinic, information from regional healthcare databases, and phone calls to the patients, their relatives or primary care physicians.
Global and event-free survival were determined. Major clinical events included all cause death, stroke, and heart failure hospitalization.
Statistical analysis
Quantitative variables, after normality checked by means of Kolmogorov–Smirnov test, are expressed as mean ± standard deviation, while qualitative variables are expressed as a percentage.
Comparisons were made at three levels: PPM patients versus PPM-free patients, severe PPM patients versus the rest of the series, and comparison of the three groups among each other (PPM-free, moderate PPM, and severe PPM).
Chi square, t-student, and one-way ANOVA tests were used for group comparisons; and Kaplan–Meier curves and log-rank test for survival assessment. A multivariate analysis using binary logistic regression was performed to determine those factors independently associated with PPM and severe PPM. And, finally, a multivariate analysis using Cox proportional hazards model was carried out to determine independent factors associated with event-free survival.
Results
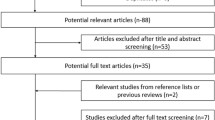
During the inclusion period, 212 prostheses were implanted. A total of 27 cases were excluded from the study: 18 due to hospital death and 9 because of incomplete TTE data. Finally, 185 patients were included.
Baseline characteristics of patients are shown in Table 1.
A 29 mm prosthesis was implanted in 61 patients; a 26 mm one in 119; a 23 mm one in 4; and a 25 mm was placed in 1. The most frequent prosthesis (181, 97.8%) was classic CoreValve. There was also one CoreValve Evolut, one Portico, and two Lotus.
PPM was present in 45 patients (24%), severe PPM in 11 patients (6%), and moderate PPM in 34 (18%). Table 2 shows three groups comparisons.
PPM was significantly associated with more than mild baseline aortic regurgitation (82.5% of PPM patients versus 59.7% of PPM-free patients, p = 0.008). Significance was kept when comparing severe PPM, moderate PPM, and PPM-free patients (75%, 84.4%, and 59.7%, respectively, p = 0.02). However, differences were not significant when comparing severe PPM patients with the rest of the series (75% of severe PPM patients versus 64.7%, p = 0.72).
PPM was significantly more frequent in smaller prostheses (100% incidence in 23 mm prostheses, 0% in the 25 mm model, 22% in 26 mm ones, and 23% in 29 mm ones; p = 0.004). Severe PPM was noted in 50% of 23 mm prostheses, 0% in the 25 mm one, in 3.4% of 26 mm ones, and in 6.6% of 29 mm ones; p = 0.002, Fig. 1.
A larger body surface area was also significantly associated with a higher PPM incidence. PPM patients showed a mean body surface area of 1.77 ± 0.16 m2, and PPM-free patients 1.70 ± 0.17 m2, p = 0.02. This relation was consistent when analyzing severe PPM patients versus the rest of the series (1.84 ± 0.10 m2 versus 1.72 ± 0.17 m2, respectively, p = 0.02) and when comparing the three groups (1.84 ± 0.10 m2 versus 1.75 ± 0.17 m2 versus 1.7 ± 0.17 m2 for severe PPM, moderate PPM, and PPM-free patients, p = 0.03).
A smaller aortic annulus was associated with PPM, when comparing the three groups (20.6 ± 1.9 mm versus 20.5 ± 1.9 mm versus 21.6 ± 2.1 mm, for severe PPM, moderate PPM, and PPM-free patients, respectively, p = 0.02), and when comparing PPM patients versus PPM-free patients (20,5 ± 1.9 mm versus 21.6 ± 2.1 mm, p = 0.004). However, this difference was not statistically significant when comparing severe PPM patients versus the rest of the series (20.6 ± 1.8 mm versus 21.4 ± 2.1 mm, p = 0.27).
There were no significant differences in other parameters as potential PPM predictors (Tables 1, 2).
Intraprocedure overexpansion with balloon was performed in 75 patients: 21.3% of them presented PPM versus 26.6% of the rest of series (p = 0.49). The frequency of severe PPM was also similar in both groups (4% vs. 7.3%, p = 0.53).
The learning curve included 24 patients: 4.2% presented PPM versus 27.3% in the remaining 161 patients (p = 0.01). However, the frequency of severe PPM was similar in both groups (0% vs. 6.8%, p = 0.36).
Obesity percentage among PPM patients was 46.7% versus 30.7% in PPM-free patients, p = 0.05. A 54.5% of severe PPM patients presented obesity versus 33.3% from the rest of the series, p = 0.15. There were no significant differences among severe PPM, moderate PPM and PPM-free groups (54.5% vs. 44.1% vs. 30.7%, p = 0.12). In general, results were consistent when analyzing BMI as a continuous variable (Tables 1, 2).
Mean logistic EuroSCORE in PPM patients was 15 ± 9.2% versus 10.5 ± 7.5% in PPM-free patients, p = 0.009. Significant differences were also noticed when analyzing the three groups (10.5 ± 7.5% vs. 15.6 ± 9.4% vs. 11.4 ± 8%, for PPM-free, moderate PPM, and severe PPM, respectively, p = 0.02). However, differences were not significant between severe PPM group and the rest of the series (11.4 ± 8.1% vs. 11.3 ± 8%, p = 0.99).
Multivariate analysis showed an independent association of PPM with higher logistic EuroSCORE (OR 1.06, CI 95% 1.01–1.12, p = 0.03), a body surface area ≥ 1.72 m2 (OR 3.58, CI 95% 1.30–9.87, p = 0.01), and smaller aortic annuli (OR 0.73, CI 95% 0.55–0.92, p = 0.03). The 23 mm prosthesis was found to be an independent factor associated with severe PPM (OR 17.79, CI 95% 1.87–179.78, p = 0.012). This was also the case for a ≥ 1.72 m2 body surface area (OR 8.62, CI 95% 1.03–72.05, p = 0.047) Table 3.
In a mean follow-up of 43 ± 23 months, 77 patients suffered a major event (45 deaths, 19 strokes, and 39 heart failure hospitalizations). The mean event-free survival was 34 ± 26 months.
Severe PPM patients showed a lower event-free survival than the rest of the series (52% vs. 84% after 34 months, p = 0.04). There were neither significant differences between PPM patients and PPM-free patients (55% vs. 71%, respectively, p = 0.12), nor when comparing severe PPM, moderate PPM, and PPM-free patients (52%, 58%, and 71% respectively, p = 0.08) Fig. 2.
Event-free survival curves (including all cause death, stroke, or heart failure hospitalization) according to presence and degree of prosthesis patient mismatch (PPM). Left: probability of survival for PPM-free patients versus PPM. Centre: probability of survival for severe PPM patients versus the rest of the series. Right: PPM-free patient survival curves, versus moderate PPM and severe PPM
When analyzing major events individually, PPM patients showed a trend, with borderline statistical significance, to lower stroke-free survival versus PPM-free patients (81% vs. 94% after 34 months, p = 0.05). There were no differences neither among severe PPM patients versus the rest of the series (80% vs. 91%, p = 0.11), nor when comparing the three groups (severe PPM, moderate PPM, and PPM-free: 80% vs. 82% vs. 94%, p = 0.10) Fig. 3.
Event-free survival curves and prosthesis-patient mismatch degree. Upper row: comparative curves of mortality-for-any-reason-free survival. Central row: comparative curves of stroke-free survival. Lower row: comparative curves of heart failure hospitalization-free survival. Left column: comparison of mismatch-free group (solid line) versus global mismatch group (thick dotted line). Central column: comparison of severe mismatch group (thin dotted line) versus the rest of the series (solid line). Right column: comparison among the three groups; mismatch-free (solid line) versus moderate mismatch (thick dotted line) versus severe mismatch (thin dotted line). No statistical significance is achieved in any case
There were no significant differences in heart failure admission-free survival in any comparison: PPM versus PPM-free (66% vs. 83%, p = 0.32), severe PPM versus the rest of the series (52% vs. 81%, p = 0.12), or severe PPM versus moderate PPM versus PPM-free (52%, 71%, and 83%, respectively, p = 0.28) Fig. 3.
There were no differences in global survival (all cause death) in follow-up: neither in the comparison between PPM-free with PPM patients (81% vs. 82%, after 34 months, p = 0.73), nor when comparing severe PPM patients versus the rest of the series (70% vs. 82% after 34 months, p = 0.29), nor when comparing the three groups (70% severe PPM, 85% moderate PPM, and 81% PPM-free, p = 0.41) Fig. 3.
In the multivariate analysis (Table 4), severe PPM remained as an independent factor associated with lower event-free survival (HR 2.91, CI 95% 1.14–7.43, p = 0.03), as well as high pulmonary artery systolic pressure (HR 1.04, CI 95% 1.02–1.06, p < 0.0005), and chronic obstructive pulmonary disease (COPD) (HR 2.54, CI 95% 1.34–4.82, p = 0.004).
Discussion
The main findings of our study are a low incidence of PPM after TAVI, the association of PPM with some key clinical and echocardiographic variables and the adverse prognostic impact of severe PPM in follow up regarding some major clinical events not previously reported.
PPM prevalence after TAVI, especially severe, is relatively low in our series. It is lower than surgical prostheses [12] and even slightly lower than other transcatheter valve series (severe PPM prevalence of nearly 20% in the TAVI group from PARTNER [15] study). In studies with CoreValve prosthesis predominance [16, 17], average severe PPM prevalence is 6–9%, similar to this study. A possible explanation for the differences between prostheses could be the fact that the CoreValve valve stent is less thick than Edwards and surgical prostheses´ supports, representing hemodynamics advantages. However, it could also be due to methodological issues such as differences in the way of determining the effective prosthetic area, or differences in terms of population and technical device features.
We found several conditions associated with severe PPM appearance. Those factors have not been completely defined in current literature. Up to now, a smaller native aortic annulus and/or a smaller left ventricular outflow tract (LVOT) diameter, as well as a larger body surface area and presence of COPD with home oxygen therapy, have been highlighted [14, 17]. The relationship between PPM and a larger body surface area has already been reported in other series [15, 16], which has been confirmed by our results. It makes sense that larger patients are associated with greater tissue oxygenation requirements and, consequently, greater effective aortic areas. Likewise, our analysis also found a relationship between obesity and PPM, but it was not confirmed for severe PPM or when comparing the three groups, probably due to the lack of statistical power owing to severe PPM’s low prevalence in our series.
As a result of this, PPM occurrence is more likely in small aortic annulus patients, confirmed by our results, consistent with those published by other authors [15, 28, 29]. However, TAVI has been suggested to be preferable to surgery, especially in small aortic annulus patients [15], in order to reduce mismatch, since there seems to be a better hemodynamic profile and better reverse remodeling in PPM patients’ follow up after TAVI versus conventional prosthesis [14, 15]. The explanation relies on the fact that transcatheter prostheses are on a thinner stent than the ring of surgical prostheses, and they are not emplaced in annular position, which would cause more obstruction to blood flow. This difference is proportionally increased when the prosthesis is placed in a smaller aortic annulus [28].
Additionally, our analysis relates PPM occurrence with small prostheses size, which had never been established by literature until now. This crucial finding leads us to think that, in annuli close to the limits for prosthesis size selection, we should choose slightly over dimensioned prostheses to achieve the double effect of leak reduction, as proposed by different authors [28,29,30,31], and mismatch minimization.
Regarding that point, method used for measuring aortic annulus is important. Two-dimensional transesophageal echocardiography determines lower annulus values than the three-dimensional one, which may lead to place smaller prostheses, provoking entailing higher rates [18] of severe PPM. In our study, we believe that this factor is minimized by a multi-image study protocol including multi-slice CT measurements [24].
In a study by Takagi et al. with the CoreValve prosthesis [14], significant native aortic regurgitation was suggested as a PPM predictor. This factor was associated with PPM in our univariate analysis but not in multivariate one.
On the other hand, a PARTNER [15] subanalysis demonstrated a lower PPM incidence among patients who underwent intraprocedure post-dilation. We did not observe significant differences regarding this point, even though 41% of our patients received postdilatation. Different technical and hemodynamic characteristics of the device placed (98% CoreValve versus 100% Edwards) could be an explanation, but it could also rely on the sample’s size.
Like ours, previous observational studies with surgical prostheses had shown a relationship between a higher basal risk profile (EuroSCORE) and the occurrence of PPM [32]. However, we did not found any prognostic impact of this variable on the medium term follow up in the multivariate analysis.
The lower appearance of PPM during the “learning stage” could be due to the fact that patient selection and process were made under the supervision of a “proctor” team, so the cases with less probability of complications was chosen. In addition, during that period, smaller native aortic annulus were rejected for TAVI due to the lack of a 23 mm prosthesis.
In the TTE performed 72 h after implantation, 38% of our patients presented at least moderate periprosthetic regurgitation, without significant associations with PPM occurrence nor prognostic implication. This lack of association seems to be related to the low statistical power due to the sample’s size and our relatively low mortality rate during the follow-up.
The most remarkable results from our study are those related to follow-up and PPM’s prognostic impact after TAVI. Surgical series [12, 13] demonstrated lower global survival in severe mismatch, and in mismatch of any degree accompanied by left ventricular systolic dysfunction, which did not happen in our series. However, there is great discrepancy in the literature regarding to TAVI and its negative impact of PPM on mortality [14,15,16,17, 33]. Furthermore, no previous studies had focused on analyzing major clinical events such as stroke or heart failure.
Like other studies published [16], the results from our series demonstrate an adverse prognostic impact in the mid-term follow up in severe PPM patients. This may be explained by the fact that high ventricular afterload persistence and lower left ventricular hypertrophy regression, because of severe PPM, may have a negative impact on coronary flow normalization. In addition, sustained tissue perfusion deficit could partially explain an increase in major clinical events.
Given the clinical significance of severe PPM in patient´s follow-up, the main practical application of our data is that PPM occurrence after TAVI should be minimized. Potential strategies could include a careful annulus measurement, trying to avoid infraestimations and choosing a larger prosthesis size for annuli close to the limits for prosthesis size selection, and insisting on weight loss in selected patients (nearly half of PPM patients in our series were obese). On the other hand, since PPM patients present higher stroke incidence, the antiaggregating/anticoagulant strategy could be reconsidered in this group of patients. According to this, in their latest update of clinical practice guidelines, ACC/AHA American societies [34] recommend antivitamin K anticoagulation during three months after TAVI in low bleeding risk patients with a IIb level of evidence.
Limitations
The main limitation of our study is the relatively low sample size of a single-center observational study. Even though the total number is not insignificant, the low incidence of PPM and events limit statistical significance. This also explains the fact that our study shows conclusive results for major events as a combined endpoint but not on an individual basis.
Although echocardiography measures were carried out following current guidelines, there are still discrepancies regarding the correct determination of EOA in TAVI.
Bias might have been introduced because of exclusion of patients without two TTE and those patients deceased in hospital.
The percentage of patients who completed echocardiographic follow-up was insufficient to draw solid conclusions regarding lower left ventricular hypertrophy regression as a possible cause of worse prognosis of PPM.
Conclusions
In our series, PPM is present in a quarter of the patients undergoing TAVI, with a lower frequency for severe PPM (6%). A higher EuroSCORE, a smaller prosthesis size, a greater body surface area, and a smaller aortic annulus size were independently associated with PPM. Severe PPM has an independent association with major events in mid-term follow up.
References
Grube E, Schuler G, Buellesfeld L, Gerckens U, Linke A, Zickmann B et al (2007) Percutaneous aortic valve replacement for severe aortic stenosis in high-risk patients using the second- and current third-generation self-expanding Core-Valve Prosthesis. J Am Coll Cardiol 50:69–76
Tamburino C, Capodanno D, Ramondo A, Petronio AS, Ettori F, Santoro G et al (2011) Incidence and predictors of early and late mortality after transcatheter aortic valve implantation in 663 patients. Circulation 123:299–308
Leon MB, Smith CR, Mack M, Miller DC, Moses JW, Svensson LG et al (2010) Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med 363:1597–1607
Smith C, Leon M, Mack M, Miller D, Moses J, Svensson L et al (2011) Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med 364(23):2187–2198
Kodali S, Williams M, Smith S, Lars G, Webb JG, Makkar RR et al (2012) Two-year outcomes after transcatheter or surgical aortic-valve replacement. N Engl J Med 366:1686–1695
Hahn R, Pibarot P, Stewart W, Weissman NJ, Gopalakrishnan D, Keane MG et al (2013) Comparison of transcatheter and surgical aortic valve replacement in severe aortic stenosis a longitudinal study of echocardiography parameters in Cohort A of the PARTNER trial (placement of aortic transcatheter valves). JACC 61(25):2514–21
Holmes DR, Mack MJ, Kaul S, Agnihotri A, Alexander KP, Bailey SR et al (2012) 2012 ACCF / AATS / SCAI / STS expert consensus document on transcatheter aortic valve replacement. Cathet Cardiovasc Interv 79:1023–1082
Avanzas P, Pascual I, Muñoz-García AJ, Segura J, Alonso-briales JH, Suárez de Lezo J et al (2017) Seguimiento a largo plazo de pacientes con estenosis aórtica grave tratados con prótesis autoexpandible. Rev Esp Cardiol 70(4):247–253
Lancellotti P, Pibarot P, Chambers J et al (2016) Recommendations for the imaging assessment of prosthetic heart valves: a report from the European Association of Cardiovascular Imaging endorsed by the Chinese Society of Echocardiography, the Inter-American Society of Echocardiography, and the Brazilian Department of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 17:589–590
Kappetein AP, Head SJ, Genereux P, Piazza N, Van Mieghem NM, Blackstone EH et al (2012) Updated standardized endpoint definitions for transcatheter aortic valve implantation: the Valve Academic Research Consortium-2 consensus document. Eur J Cardiothorac Surg 42:S45–S60
Dumesnil J, Pibarot P (2011) Prosthesis-patient mismatch: an update. Curr Cardiol Rep 13(3):250–257
Takagi H, Yamamoto H, Iwata K, Goto SN, Umemoto T (2012) A meta-analysis of effects of prosthesis-patient mismatch after aortic valve replacement on late mortality. Int J Cardiol 159(2):150–154
Chen J, Lin Y, Kang B, Wang Z (2014) Indexed effective orifice area is a significant predictor of higher mid- and long-term mortality rates following aortic valve replacement in patients with prosthesis-patient mismatch. Eur J Cardio-thoracic Surg 45(2):234–240
Takagi H, Umemoto T (2016) Prosthesis-patient mismatch after transcatheter aortic valve implantation. Ann Thorac Surg 101(3):872–880
Pibarot P, Weissman NJ, Stewart WJ, Hahn RT, Lindman BR, McAndrew T et al (2014) Incidence and sequelae of prosthesis-patient mismatch in transcatheter versus surgical valve replacement in high-risk patients with severe aortic stenosis: a PARTNER trial cohort-a analysis. J Am Coll Cardiol 64(13):1323–1334
Muñoz-García AJ, Muñoz-García M, Carrasco-Chinchilla F, Molina-Mora MJ, Rodríguez-Bailón I, Domínguez-Franco AJ et al (2013) Incidence and clinical outcome of prosthesis-patient mismatch after transcatheter aortic valve implantation with the CoreValve prosthesis. Int J Cardiol 167(3):1074–1076
Zorn GL, Little SH, Tadros P, Deeb GM, Gleason TG, Heiser J et al (2016) Prosthesis-patient mismatch in high-risk patients with severe aortic stenosis: a randomized trial of a self-expanding prosthesis. J Thorac Cardiovasc Surg 151(4):1014–1023
da Silva C, Sahlen A, Winter R, Bäck M, Rück A, Settergren M et al (2014) Prosthesis-patient mismatch after transcatheter aortic valve implantation: impact of 2D-transthoracic echocardiography versus 3D-transesophageal echocardiography. Int J Cardiovasc Imaging 30:1549–1557
Zoghbi WA, Chambers JB, Dumesnil JG, Foster E, Gottdiener JS, Grayburn PA et al (2009) Recommendations for evaluation of prosthetic valves with echocardiography and doppler ultrasound. A report from the American Society of Echocardiography’s guidelines and standards committee and the task force on prosthetic valves, developed in conjunction. J Am Soc Echocardiogr 22(9):975–1014
Quiñones M, Douglas P, Foster E, Gorcsan J, Lewis J, Pearlman A et al (2003) ACC/AHA clinical competence statement on echocardiography: a report of the American College of Cardiology/American Heart Association/American College of Physicians–American Society of Internal Medicine. Task force on clinical competence. JACC 41:687–708
Evangelista A, María Á, Gómez A, Durán RM, Yagüela MM, María J et al (2000) Guías de práctica clínica de la Sociedad Española de Cardiología en ecocardiografía. Rev Esp Cardiol 53(5):663–683
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA et al (2006) Recommendations for chamber quantification. Eur J Echocardiogr 7(2):79–108
Dubois D, Dubois E (1916) A formula to estimate the approximate surface area of height and weight be known. Arch Intern Med 17:863–871
Mesa D, Suárez de Lezo J, Alvarez-Ossorio M, Ruiz Ortiz M, Delgado Ortega M, León del Pino M et al (2011) Measurement of aortic valve annulus using different cardiac imaging techniques in transcatheter aortic valve implantation: agreement with finally implanted prosthesis size. Echocardiography 28:388–396
León C, Suárez de Lezo J, Mesa D, Pan M, Ruiz M, Delgado M et al (2011) Early development of leaks in the CoreValve percutaneous aortic valve prosthesis: echocardiographic assessment. Rev Esp Cardiol 64:67–70
Cejudo Díaz del Campo L, Mesa Rubio D, Ruiz Ortiz M, Delgado Ortega M, Pan M, Ojeda Pineda S et al (2012) Usefulness of transesophageal echocardiography during implantation of the CoreValve percutaneous aortic prosthesis: Influence of the learning curve. Catheter Cardiovasc Interv 80:964–971
Avanzas P, Munoz-Garcia A, Segura J, Pan M, Alonso-Briales J, Lozano I et al (2010) Percutaneous Implantation of the CoreValve(registered trademark) self-expanding aortic valve prosthesis in patients with severe aortic stenosis: early experience in Spain. Rev Esp Cardiol 63(2):141–148
Rodés-cabau J, Pibarot P, Suri RM, Kodali S, Thourani VH, Szeto WY et al (2014) Impact of aortic annulus size on valve hemodynamics and clinical outcomes after transcatheter and surgical aortic valve replacement insights from the PARTNER trial. Circ Cardiovasc Interv 7:701–711
Pibarot P, Clavel M, Dahou A (2015) Patient and procedure selection for the prevention of prosthesis-patient mismatch following aortic valve replacement. EuroIntervention 11:106–109
Lebera A, Eichingerc W, Rieberb J, Lieberc M, Schlegerc S, Ebersbergerb U et al (2013) MSCT guided sizing of the Edwards Sapien XT TAVI device: Impact of different degrees of oversizing on clinical outcome. Int J Cardiol 168(3):2658–2664
Samim M, Stella PR, Agostoni P, Kluin J, Ramjankhan F, Sieswerda G et al (2013) A prospective “oversizing” strategy of the Edwards SAPIEN bioprosthesis: results and impact on aortic regurgitation. J Thorac Cardiovasc Surg 145(2):398–405
Dayan V, Soca G, Stanham R, Lorenzo A, Ferreiro A (2015) Is patient–prosthesis mismatch a predictor of survival or a surrogate marker of co-morbidities in cardiac surgery? Int J Cardiol 190:389–392
Tzikas A, Piazza N, Geleijnse ML, Van Mieghem N, Nuis RJ, Schultz C et al (2010) Prosthesis-patient mismatch after transcatheter aortic valve implantation with the medtronic corevalve system in patients with aortic stenosis. Am J Cardiol 106(2):255–260
Nishimura R, Otto C, Bonow R, Mack M, Carabello B, McLeod C et al (2017) 2017 AHA/ACC focused update of the 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Circulation 135(21):1–123
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors whose names are listed in the first page report no affiliation nor involvement in an organization or entity with a financial or non-financial interest in the subject matter or materials discussed in this manuscript.
Rights and permissions
About this article
Cite this article
León del Pino, M.C., Ruíz Ortiz, M., Delgado Ortega, M. et al. Prosthesis-patient mismatch after transcatheter aortic valve replacement: prevalence and medium term prognostic impact. Int J Cardiovasc Imaging 35, 827–836 (2019). https://doi.org/10.1007/s10554-018-01519-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-018-01519-z