Abstract
Non-invasive fractional flow reserve measured by coronary computed tomography angiography (FFRCT) has demonstrated a high diagnostic accuracy for detecting coronary artery disease (CAD) in selected patients in prior clinical trials. However, feasibility of FFRCT in unselected population have not been fully evaluated. Among 60 consecutive patients who had suspected significant CAD by coronary computed tomography angiography (CCTA) and were planned to undergo invasive coronary angiography, 48 patients were enrolled in this study comparing FFRCT with invasive fractional flow reserve (FFR) without any exclusion criteria for the quality of CCTA image. FFRCT was measured in a blinded fashion by an independent core laboratory. FFRCT value was evaluable in 43 out of 48 (89.6 %) patients with high prevalence of severe calcification in CCTA images [calcium score (CS) >400: 40 %, and CS > 1000: 19 %). Per-vessel FFRCT value showed good correlation with invasive FFR value (Spearman’s rank correlation = 0.69, P < 0.001). The area under the receiver operator characteristics curve (AUC) of FFRCT was 0.87. Per-vessel accuracy, sensitivity, specificity, positive predictive value, and negative predictive value were 68.6, 92.9, 52.4, 56.5, and 91.7 %, respectively. Even in eight patients (13 vessels) with extremely severely calcified lesions (CS > 1000), per-vessel FFRCT value showed a diagnostic performance similar to that in patients with CS ≤ 1000 (Spearman’s rank correlation = 0.81, P < 0.001). FFRCT could be measured in the majority of consecutive patients who had suspected significant CAD by CCTA in real clinical practice and demonstrated good diagnostic performance for detecting hemodynamically significant CAD even in patients with extremely severe calcified vessels.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Coronary computed tomography angiography (CCTA) is a noninvasive diagnostic testing for detecting coronary artery disease (CAD) and is used with increasing frequency in real clinical practice [1]. CCTA images provide anatomic information of CAD such as location and severity of stenosis, disease burden and characteristics of atherosclerotic plaque [2–5]. However, despite its high sensitivity for detecting CAD, CCTA often overestimate the coronary stenosis severity, leading to increased referral of patients without obstructive CAD to invasive coronary angiography [6–8].
Fractional flow reserve measured by computed tomography angiography (FFRCT) is a novel technology developed to noninvasively identify functional myocardial ischemia. Previous clinical studies showed the excellent diagnostic accuracy of FFRCT in detecting CAD with invasive fractional flow reserve (FFR) as the reference standard [9–11]. However, the previous studies mostly enrolled selected patients with CCTA images suitable for FFRCT measurement. The feasibility and diagnostic performance of FFRCT have not been yet fully evaluated in unselected population in real clinical practice.
The aim of the current study, therefore, is to evaluate the feasibility and diagnostic performance of FFRCT in consecutive patients who had suspected significant CAD by CCTA in real clinical practice, where a large population of patients might have inadequate CCTA image quality due to image artifacts and severe calcification.
Methods
Study design
The REAL-FFRCT (Real-world fEAsibiLlity of noninvasive Fractional Flow Reserve derived from coronary Computed Tomography angiography) study was a prospective cross-sectional study comparing FFRCT with invasive FFR, intended to enroll consecutive patients who had suspected significant CAD by CCTA and undergoing invasive coronary angiography within 60 days after acquisition of CCTA in real clinical practice. Suspected significant CAD by CCTA was defined as all significant coronary stenosis in CCTA and clinically suspected CAD with non-significant coronary stenosis in CCTA. There were no exclusion criteria for the quality of CCTA images influenced by various artifacts, such as coronary motion, opacification of coronary artery lumen by calcified plaque, and misregistration. Exclusion criteria about patients clinical characteristics were the same as in the prior FFRCT clinical studies [9, 12, 13]; We excluded those patients with characteristics unsuitable for CCTA and invasive FFR, including contraindication to beta blockers, nitrates, or adenosine advanced bradycardia, severe tachyarrhythmia, severe hypotension, severe asthma, chronic obstructive pulmonary disease, congenital heart disease, previous artificial device implantation such as pacemaker or prosthetic valve, previous percutaneous coronary intervention (PCI) with coronary stents, previous coronary artery bypass grafting, serum creatinine level greater than 1.5 mg/dL with or without hemodialysis, allergy to iodine contrast, pregnant state, acute coronary syndrome requiring emergency coronary angiography, recent myocardial infarction within 30 days before CCTA or coronary angiography, life expectancy less than 2 years, and inability to adhere to the study procedures.
The current study protocol was approved by the ethics committee in Kyoto University Hospital and written informed consent was obtained from all the patients.
CCTA acquisition and analysis
CCTA was performed using single-source CT scanners with 320-slice detector rows (Aquilion ONE: Toshiba Medical systems, Tokyo, Japan) in Kyoto university hospital and double-source CT scanners with 64-slice detector rows (SOMATOM Definition: Siemens Healthcare, Erlangen, Germany) in Morishita private CT clinic, in accordance with the recommendations of the Society of Cardiovascular Computed Tomography guidelines [14, 15].
In Kyoto university hospital, CT scans were performed with bolus tracking method during end-inspiratory breath-hold after injection of iodine contrast media at 24.5 mgI/kg/sec and prospective electrocardiographic-gating was used for scan data. Scanning parameters included volume scan (without patient table sliding), 275 milliseconds gantry rotation time, 120 kVp (100 kVp for extremely low body weight below 40 kg and 135 kVp for extremely high body weight above 100 kg) tube voltage and 350–800 mA tube current. CCTA images were reconstructed in 0.5-mm axial slices with area-detector CT, using reconstruction kernel of FC04 with iterative reconstruction of AIDR 3D in ZIOSTATION 2.
In Morishita private clinic, CT scans were performed with timing bolus method during end-expiratory breath-hold after injection of iodine contrast media at 25.9 mgI/kg/sec and retrospective electrocardiographic-gating was used for scan data. Scanning parameters included heart-rate-dependent pitch (0.20, 0.22 and 0.26), 330 milliseconds gantry rotation time, 120 kVp (100 kVp for extremely low body weight below 40 kg or no calcification) tube voltage and 360–436 mA tube current. CCTA images were reconstructed in 0.75-mm axial slices with dual source CT, using reconstruction kernel of B36 HeartView medium ASA without iterative reconstruction in Aquarius iNtuition Edition version 4.4.7.
Nitroglycerin (0.3 mg) were administered to get coronary vasodilation using a sublingual tablet in Kyoto university or sublingual spray in Morhishita private clinic, with or without intravenous beta-blocker (landiolol) targeting a heart rate of <60 beats/min in both facilities. Coronary calcium scores were assessed according to the Agatston method [16], based on CT images which were scanned with prospective electrocardiographic-gating and reconstructed in 3 mm axial slices.
Experienced local physicians assessed luminal diameter stenosis in each vessels of reference vessel diameter ≥2 mm. Coronary stenosis was categorized as 0, 25, 50, 75, 90, 99, or 100 % to AHA classification [17]. Significant stenosis was defined as lumen reduction ≥75 %.
FFRCT measurement
CCTA images were transmitted to the core laboratory (HeartFlow Inc, Redwood City, California) and FFRCT value was measured in a fashion blinded to the results of invasive FFR value. Coronary blood flow and pressure were computed under conditions simulating maximal hyperemia using the most recent generation of FFRCT analysis software. The results of FFRCT measurement were provided throughout 3-dimensional coronary artery trees. FFRCT value at the target vessel was defined as the FFRCT value at the most distal location of each target vessel that could be measured in the core laboratory. Cut-off value of FFRCT for hemodynamically significant stenosis was defined as ≤0.80.
Invasive FFR measurement
Invasive FFR measurement was performed using 6 French guiding catheter and a 0.014-inch pressure wire (Certus G7, Certus G8 or Aeris G8, St. Jude Medical Inc. and PrimeWire PRESTIGE PLUS, Volcano Inc.) by experienced interventional cardiologists, who are blinded to the results of FFRCT measurement. Maximum hyperemia was induced by intravenous adenosine 150 μg/kg/min after crossing of the pressure wire through the target vessel. Invasive FFR value was defined as minimum FFR value within 3 min after adenosine infusion. FFR measurement was performed in all vessels with significant coronary stenosis detected by CCTA and other vessels with ≥50 % coronary stenosis detected by invasive coronary angiography excluding angiographically 99 % stenosis with delayed coronary flow and totally occluded lesions. Invasive FFR value ≤0.80 was regarded as hemodynamically significant stenosis [18–21].
Endpoints and statistical analysis
The main outcome measure of the current study was the per-vessel correlation between FFRCT and invasive FFR, which was assessed by Spearman’s correlation coefficients and Bland–Altman analysis. Diagnostic performance of FFRCT was assessed by the area under the receiver operator characteristics curve (AUC) of FFRCT for detecting hemodynamically significant coronary stenosis (invasive FFR ≤0.80 as a reference standard) on per-vessel basis. In AUC analysis, we adopted FFRCT value rounded off to one decimal place. Diagnostic accuracy, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were also evaluated with diagnostic cutoff value for hemodynamically significant CAD defined as FFRCT value ≤0.80 and invasive FFR value ≤0.80.
Pretest likelihood of CAD was evaluated with updated Diamond-Forrester model from typical chest pain, age and gender [22, 23]. After completing all the FFRCT and invasive FFR measurements, all statistical analyses were performed at the study center (Kyoto University Hospital) independently from the FFRCT core laboratory. All statistical analyses were performed using JMP 10 (SAS Institute Inc, Cary, NC) software. All the statistical analyses were two-tailed. P values <0.05 were considered statistically significant.
Results
Study population
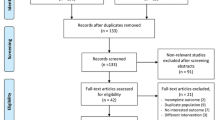
Between May 2014 and June 2015, CCTA was performed in 450 patients for suspected CAD in Kyoto university hospital or Morishita private CT clinic. After excluding 109 patients with clinical exclusion criteria and 281 patients without significant coronary artery stenosis detected by CCTA, 60 patients who were planned to undergo invasive coronary angiography were eligible for the current study (Fig. 1). After further exclusion of 9 patients who did not undergo invasive FFR measurement, and 3 patients who refused to participate in the current study, the current study population consisted of 48 consecutive patients who underwent invasive FFR measurements for the target vessels within 60 days after CCTA.
Baseline characteristics reflected the real clinical practice, including high prevalence of advanced age (70.8 ± 7.8 years of age), hypertension, dyslipidemia, and diabetes mellitus (Table 1). Median score for the pretest likelihood for CAD in this population was 55.5 and 39 patients (81.3 %) had intermediate score (20–80 %) (Table 1).
Regarding CCTA acquisition characteristics, median heart rate was 65 bpm under control by beta-blocker use (Table 2). Nitrates were administered in all patients. Among 48 patients whose CCTA images were transmitted to the FFRCT core laboratory, FFRCT measurement in the core laboratory was feasible in 43 (89.6 %) patients. FFRCT value could not be measured in three patients with image artifacts (e.g., motion, noise, contrast, blooming), one with transmission error to the core laboratory and one with severe calcification (Fig. 1 and Supplementary Fig. 1).
In the 43 patients with evaluable FFRCT value, CCTA images revealed high prevalence of severe calcification [median calcium score (CS): 285 [114–778], CS > 400: 40 %, and CS > 1000: 19 %] (Table 3). Significant coronary stenosis (≥75 %) by CCTA image was present in 41 patients (95.3 %) with 52 vessels (74.3 %). The other 18 vessels (25.7 %) had 50 % stenosis detected by CCTA.
The mean interval from CCTA acquisition to invasive FFR measurement was 23.6 ± 15.5 days.
Diagnostic performance of FFRCT in the entire cohort
All the results for FFRCT and invasive FFR in the individual cases were presented in Supplementary Table 1. FFRCT showed a good correlation with invasive FFR in per-vessel analysis (Spearman’s rank correlation = 0.69, P < 0.001) (Fig. 2). The extreme outliers of the difference ≥0.30 between FFRCT and invasive FFR values were found in 2 patients with 2 vessels (Fig. 3). FFRCT value ≤0.80 was present in 35 patients (81.4 %) with 46 vessels (65.7 %), while invasive FFR value ≤0.80 was present in 21 patients (48.8 %) with 28 vessels (40.0 %) (Table 3).
Per-vessel diagnostic performance of FFRCT for detecting hemodynamically significant CAD. a Correlation between FFRCT and invasive FFR value. b Bland–Altman plot of FFRCT and invasive FFR. c 2 by 2 tables for FFRCT and invasive FFR (cutoff value: 0.80). d The area under the receiver operator characteristics curve (AUC) of FFRCT. CI confidence interval
Representative cases of extreme outliers. a Coronary computed tomography angiography (CCTA) performed by a single-source CT scanners with 320-slice detector rows with prescription of beta blocker and nitrate tablet (heart rate: 61 bpm), demonstrated sub-total lesion in mid right coronary artery (RCA). FFRCT value in this case was 0.50 (orange circle). In invasive coronary angiography 8 days after CCTA acquisition, however, the target lesion in the mid RCA showed only moderate stenosis (orange arrow), and invasive fractional flow reserve (FFR) was 0.95 (white arrow). The difference of the severity of target lesion between CCTA/FFRCT and invasive coronary angiography might be caused by inadequate vasodilation at the time of CCTA. b CCTA showed moderate-severe bifurcation lesion with severe calcification in mid left anterior descending artery (LAD) (orange circle). Total calcium score in this case was 778. FFRCT value at the distal end of LAD was significant for functional ischemia (FFRCT value: 0.73). In invasive coronary angiography 32 days after CCTA acquisition, the target lesion in mid LAD showed severe coronary stenosis. Invasive FFR value at distal LAD (white arrow) was also significant for functional ischemia, but much lower than FFRCT value (FFRCT: 0.73, and FFR: 0.42). This underestimation of the functional significance of the target lesion occurred during semi-automatic reconstruction of a 3-dimensional anatomic model from CCTA image, which emphasizes the need for manual correction. This case might indicate one of the most critical limitations of FFRCT
There were 2 vessels of false negative and 20 vessels of false positive by FFRCT (Fig. 2). Regarding the two false negative vessels, both invasive FFR values were the grey zone of 0.75–0.80 and both FFRCT values were just above 0.80 (Supplementary Table 1). The mean differences between FFRCT and invasive FFR in 20 false positive vessels were 0.13 ± 0.09 (range: 0.01–0.45). The AUC of FFRCT (per-vessel) was 0.87 (95 % confidence interval 0.79–0.95) (Fig. 2). Per-vessel accuracy, sensitivity, specificity, PPV, and NPV were 68.6, 92.9, 52.4, 56.5, and 91.7 %, respectively (Fig. 4).
Per-vessel diagnostic performance of FFRCT for detecting hemodynamically significant CAD in patients with and without extremely severe calcified vessels [calcium score (CS) >1000]. a Correlation between FFRCT and invasive FFR. b 2 by 2 tables for FFRCT and invasive FFR (cutoff value: 0.80). c Diagnostic performance of FFRCT in patients with and without extremely severe calcified vessels (CS > 1000). PPV positive predictive value, NPV negative predictive value
Diagnostic performance of FFRCT in extremely severe calcified vessels
Among 43 patients with 70 vessels, 8 patients with 13 vessels had extremely severely calcified lesions as defined by CS > 1000. Good correlation between FFRCT and invasive FFR was maintained even in patients with CS > 1000 (Spearman’s rank correlation = 0.81, P < 0.001) (Fig. 4). Representative cases of extremely severely calcified vessels were presented in Fig. 5.
Representative cases of extremely severe calcified vessels. a Coronary computed tomography angiography (CCTA) demonstrated diffuse severe calcified lesions in both proximal left anterior descending artery (LAD) and left circumflex coronary artery (LCx). Total calcium score (CS) was 4153. FFRCT showed hemodynamically significant ischemia in LAD lesion and FFRCT value at the distal end of LAD (black arrow) was 0.65. Invasive FFR also showed significant ischemia and invasive FFR value at the distal LAD (white arrow) was 0.77. b CCTA demonstrated severe coronary calcification from left main trunk to proximal LAD with severe stenosis in distal LAD. Total CS was 1772. FFRCT value at distal end of LAD was 0.50, although major step up was observed only at distal severe LAD lesion (orange arrow). Coronary angiography revealed only moderate coronary stenosis in severe calcified lesions at proximal LAD (orange arrow). Invasive FFR value at the distal LAD was 0.51, and Step up was also observed at distal severe LAD lesion
Per-vessel accuracy, sensitivity, specificity, PPV, and NPV were 76.9, 100, 62.5, 62.5, and 100 % in patients with severely calcified vessels, and 66.7, 91.3, 50.0, 55.2, and 89.5 % in patients without severely calcified vessels (Fig. 4).
Discussion
The main findings in the current study were as follows; (1) Measurement of FFRCT was feasible in the majority of consecutive patients who suspected significant CAD by CCTA in real clinical practice; (2) FFRCT showed a good correlation with invasive FFR, but tended to overestimate the functional significance of the stenosis compared with invasive FFR; and (3) FFRCT showed good for detecting hemodynamically significant CAD defined as invasive FFR ≤0.80 regardless of existence of extremely severely calcified vessels.
In the current study enrolling consecutive patients who were suspected significant CAD by CCTA, FFRCT could be measured in the majority of cases despite inclusion of a significant proportion of patients with extremely severely calcified vessels (CS > 1000: 18.6 %), revealing the feasibility of FFRCT in daily clinical use. Furthermore, the diagnostic performance of FFRCT in the current study enrolling unselected patients including those with heavily calcified vessels was acceptable, although that was lower than that in the prior clinical trials [9–11].
Considering the daily clinical use of FFRCT, well understanding common reasons for the difference between FFRCT and invasive FFR is important. According to the findings in the current study, FFRCT tended to overestimate the functional significance of the stenosis compared with invasive FFR, leading to low false negative rate and relatively high false positive rate. One of the reasons for the smaller FFRCT values as compared with invasive FFR might be that FFRCT value indicated value at the most distal portion of the target vessels, whereas invasive FFR values are not usually measured at the most distal portion of the target vessel because of the gap between the tip and pressure censor in pressure wire. The lack of adequate vasodilation, furthermore, might cause the difference between FFRCT and invasive FFR value; timely administration of adequate dose of nitrate is essential for preventing vasoconstriction leading to overestimation of the functional significance of the stenosis by FFRCT [24]. In the one of the two cases of extreme outliers in the current study, the severity of target lesion by CCTA was apparently more severe than that by coronary angiography, suggesting the possibility of inadequate vasodilation at the time of CCTA.
The existence of coronary calcification is known to be a major factor for decreasing diagnostic performance of conventional CCTA due to blooming and beam-hardening artifacts, which leads to overestimation of the severity of target lesions. Intuitively, in patients with severely calcified vessels, diagnosis of hemodynamically significant CAD using FFRCT seems to be challenging. In the substudy of the Analysis of Coronary Blood Flow Using CT Angiography: Next Steps (NXT) trial, FFRCT was reported to provide high diagnostic performance and discrimination for ischemia over a wide range of coronary calcification severity [10, 25]. In the NXT trial, however, the extent of coronary calcification seemed to be milder than that encountered in daily clinical practice. Indeed, extremely severe calcification of CS > 1000 was present in only 13 out of 214 (6 %) patients [10]. In the current study including consecutive patients without any exclusion criteria for the quality of CCTA image, the extent of coronary calcification was much greater than that in the NXT trial (median CS: 285, CS > 1000: 18.6 %). Even in the setting of patients with extremely severe calcified vessels (CS > 1000), good correlation between FFRCT and invasive FFR was maintained in the current study, supporting the feasibility of using this new technology in the wide range of population in daily clinical practice. In symptomatic patients with a very high calcium score who might have a high odds of having a significant coronary stenosis, however, FFRCT might not offer a sufficiently low NPV to avoid conventional coronary angiography. Further investigation is needed to clarify the role of FFRCT in these patients.
Study limitations
The first and most important limitation in the current study was a small number of enrolled patients, although the current study is the first study evaluating utility of FFRCT in consecutive CAD patients who were suspected significant CAD by CCTA. Considering a small number of enrolled patients and relatively low diagnostic accuracy in the current study, further large scale study would be needed to confirm the utility of FFRCT in daily clinical practice. Second, the study results cannot generalize all the patients who receive CCTA because we enrolled only patients who were suspected significant CAD by CCTA and whose FFRCT value could be measured by the core laboratory. However, this novel technology of FFRCT may indicate patients who are suspected significant CAD by CCTA in daily clinical use, because conventional CCTA have an adequately high NPV for ruling out significant CAD. Third, it is possible that the nitrate protocol used in the current study may have led to incomplete vasodilation at the acquisition of CCTA in some patients. Finally, because the current study was performed in the university hospital and CT specialized clinic where high quality CCTA acquisition was achieved, generalizing these results in other settings should be done with caution.
Conclusions
FFRCT could be measured in the majority of consecutive patients who had suspected significant CAD by CCTA in real clinical practice, and demonstrated good diagnostic performance for detecting hemodynamically significant CAD even in patients with extremely severely calcified vessels.
Abbreviations
- AUC:
-
Area under the receiver operator characteristics curve
- CAD:
-
Coronary artery disease
- CCTA:
-
Coronary computed tomography angiography
- CS:
-
Calcium score
- FFR:
-
Fractional flow reserve
- FFRCT :
-
Fractional flow reserve measured by coronary computed tomography angiography
- NPV:
-
Negative predictive value
- PCI:
-
Percutaneous coronary intervention
- PPV:
-
Positive predictive value
References
Zorlak A, Zorlak A, Thomassen A et al (2015) Patients with suspected coronary artery disease referred for examinations in the era of coronary computed tomography angiography. Am J Cardiol 116:344–349
Miller JM, Rochitte CE, Dewey M et al (2008) Diagnostic performance of coronary angiography by 64-row CT. N Engl J Med 359:2324–2336
Meijboom WB, Meijs MF, Schuijf JD et al (2008) Diagnostic accuracy of 64-slice computed tomography coronary angiography: a prospective, multicenter, multivendor study. J Am Coll Cardiol 52:2135–2144
Puchner SB, Liu T, Mayrhofer T et al (2014) High-risk plaque detected on coronary CT angiography predicts acute coronary syndromes independent of significant stenosis in acute chest pain: results from the ROMICAT-II trial. J Am Coll Cardiol 64:684–692
Min JK, Shaw LJ, Berman DS (2010) The present state of coronary computed tomography angiography a process in evolution. J Am Coll Cardiol 55:957–965
Douglas PS, Hoffmann U, Patel MR et al (2015) Outcomes of anatomical versus functional testing for coronary artery disease. N Engl J Med 372:1291–1300
Meijboom WB, Van Mieghem CA, van Pelt N et al (2008) Comprehensive assessment of coronary artery stenoses: computed tomography coronary angiography versus conventional coronary angiography and correlation with fractional flow reserve in patients with stable angina. J Am Coll Cardiol 52:636–643
Schuijf JD, Wijns W, Jukema JW et al (2006) Relationship between noninvasive coronary angiography with multi-slice computed tomography and myocardial perfusion imaging. J Am Coll Cardiol 48:2508–2514
Koo BK, Erglis A, Doh JH et al (2011) Diagnosis of ischemia-causing coronary stenoses by noninvasive fractional flow reserve computed from coronary computed tomographic angiograms. results from the prospective multicenter DISCOVER-FLOW (diagnosis of ischemia-causing stenoses obtained via noninvasive fractional flow reserve) study. J Am Coll Cardiol 58:1989–1997
Norgaard BL, Leipsic J, Gaur S et al (2014) Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: the NXT trial (analysis of coronary blood flow using CT angiography: next steps). J Am Coll Cardiol 63:1145–1155
Min JK, Leipsic J, Pencina MJ et al (2012) Diagnostic accuracy of fractional flow reserve from anatomic CT angiography. JAMA 308:1237–1245
Min JK, Berman DS, Budoff MJ et al (2011) Rationale and design of the DeFACTO (determination of fractional flow reserve by anatomic computed tomographic AngiOgraphy) study. J Cardiovasc Comput Tomogr 5:301–309
Gaur S, Achenbach S, Leipsic J et al (2013) Rationale and design of the HeartFlowNXT (HeartFlow analysis of coronary blood flow using CT angiography: NeXt sTeps) study. J Cardiovasc Comput Tomogr 7:279–288
Abbara S, Arbab-Zadeh A, Callister TQ et al (2009) SCCT guidelines for performance of coronary computed tomographic angiography: a report of the Society of Cardiovascular Computed Tomography Guidelines Committee. J Cardiovasc Comput Tomogr 3:190–204
Leipsic J, Abbara S, Achenbach S et al (2014) SCCT guidelines for the interpretation and reporting of coronary CT angiography: a report of the Society of Cardiovascular Computed Tomography Guidelines Committee. J Cardiovasc Comput Tomogr 8:342–358
Agatston AS, Janowitz WR, Hildner FJ et al (1990) Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 15:827–832
Austen WG, Edwards JE, Frye RI et al (1975) A reporting system on patients evaluated for coronary artery disease. Report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association. Circulation 51:5–40
Tonino PA, De Bruyne B, Pijls NH et al (2009) Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med 360:213–224
De Bruyne B, Fearon WF, Pijls NH et al (2014) Fractional flow reserve-guided PCI for stable coronary artery disease. N Engl J Med 371:1208–1217
De Bruyne B, Pijls NH, Kalesan B et al (2012) Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med 367:991–1001
Adjedj J, De Bruyne B, Flore V et al (2016) Significance of Intermediate Values of Fractional Flow Reserve in Patients With Coronary Artery Disease. Circulation 133:502–508
Task Force Members, Montalescot G, Sechtem U et al (2013) 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J 34:2949–3003
Genders TS, Steyerberg EW, Alkadhi H et al (2011) A clinical prediction rule for the diagnosis of coronary artery disease: validation, updating, and extension. Eur Heart J 32:1316–1330
Leipsic J, Yang TH, Thompson A et al (2014) CT angiography (CTA) and diagnostic performance of noninvasive fractional flow reserve: results from the Determination of Fractional Flow Reserve by Anatomic CTA (DeFACTO) study. AJR Am J Roentgenol 202:989–994
Norgaard BL, Gaur S, Leipsic J, Ito H et al (2015) Influence of coronary calcification on the diagnostic performance of CT angiography derived FFR in coronary artery disease: a substudy of the NXT trial. JACC Cardiovasc Imaging 8:1045–1055
Acknowledgments
We appreciated all the members of the CT and cardiac catheterization laboratory in Graduate school of cardiovascular medicine, Kyoto University and Morishita heart clinic for their contribution to this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This study was a collaborative study of Kyoto University Hospital with HeartFlow Inc. and C.A. The study was funded by the unrestricted grant of Kyoto University Hospital. FFRCT was evaluated free of charge by HeartFlow Inc. C.A. Taylor is an employee and shareholder of HeartFlow Inc. All the other authors have no conflict of disclosures.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kawaji, T., Shiomi, H., Morishita, H. et al. Feasibility and diagnostic performance of fractional flow reserve measurement derived from coronary computed tomography angiography in real clinical practice. Int J Cardiovasc Imaging 33, 271–281 (2017). https://doi.org/10.1007/s10554-016-0995-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-016-0995-9