Abstract
The efforts for a broad application of the appropriate use criteria to reduce inappropriate nuclear stress testing have frequently been unsuccessful and the reported rates of inappropriateness have varied widely between studies. We sought to analyze the criteria of clinical appropriateness of a cohort of consecutive patients referred to our nuclear cardiology laboratory to perform stress myocardial perfusion imaging (MPI) and to assess the relationships between test appropriateness and the evaluation of ischaemia. A cohort of 251 consecutive patients, admitted to our Institute from January to March 2015, who underwent stress/rest MPI on a dedicated cardiac camera equipped with cadmium–zinc–telluride detectors, was selected. The level of clinical appropriateness of each MPI test was categorized in each patient according to the AUC criteria. According to the accepted criteria, the majority of the MPI stress-tests could be classified as clinically appropriate (218 of 251, 87 % of the tests), while only 16 (6 %) and 17 (7 %) resulted of uncertain appropriateness or clearly inappropriate, respectively. Of the 251 appropriate tests, 22 (10 %), 65 (30 %), and 131 (60 %) showed the presence of a mild (SDS < 4), moderate (4 ≥ SDS < 7), and severe (SDS ≥ 7) ischemic burden, respectively, while none of the inappropriate test showed moderate-to-severe ischaemia (P < 0.001 for comparisons). The rate of inappropriate MPI tests is considerably low in a high-volume laboratory. Appropriate and inappropriate studies identify patients at high and low probability of significant ischemia, respectively, providing insights on the effects of the level of appropriateness on stress-test results.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The use of cardiovascular imaging modalities has increased dramatically over the past decade [1–4], raising concerns on its economical and clinical sustainability [5–7]. This is particularly true in the case of imaging tests that theoretically expose patients to potential collateral risks, such as radionuclide imaging modalities [8]. Nevertheless, despite its theoretical limitations (i.e. radiation exposure), myocardial perfusion imaging (MPI) still represents one of the most frequent tests for the non-invasive evaluation of myocardial ischemia, due to its intrinsic versatility, and recognized reproducibility of the results.
On the other hand, cost-effectiveness studies have clearly demonstrated the pivotal role of non-invasive imaging for the selection of patients undergoing more expensive procedures [9], such as invasive coronary interventions, underscoring the positive clinical impact of test appropriateness [5].
Therefore, in order to promote an appropriate use of nuclear cardiology testing, in 2009 the American College of Cardiology Foundation updated the Appropriate Use Criteria (AUC) for radionuclide imaging [10]. Up to now, efforts for broad application of the AUC to reduce inappropriate nuclear stress tests have frequently been unsuccessful [11–13]. In fact, the reported rates of inappropriate nuclear testing have ranged widely between studies [14–16].
In a recent retrospective analysis on the appropriate use of nuclear stress tests in the U.S., Ye et al. [17] characterized the pattern of inappropriate testing and demonstrated the difficulty that individual clinicians may have to identify inappropriate tests, further stressing on the existence of a relevant clinical barrier against the successful implementation of AUC criteria. In this respect, the widespread use of imaging techniques poses relevant doubts on their economic sustainability and on the non-negligible health risks of an inappropriate imaging test [18].
Despite these limitations, AUCs remain, up to now, the only accepted way to evaluate appropriateness in nuclear cardiology.
With these considerations in mind, we sought to analyze the criteria of appropriateness in a cohort of consecutive patients referred to our nuclear cardiology laboratory to perform stress MPI and to further assess the relationships between the patterns of test appropriateness and the detection of ischemia.
Methods
We retrospectively selected a cohort of 251 consecutive patients, admitted to our institution between January and March 2015, who had undergone stress/rest MPI on a dedicated cardiac camera equipped with cadmium–zinc–telluride (CZT) detectors according to a single day protocol. Most of the patients (90 %) were referred to MPI by a clinical cardiologist, while the remainders by a general practitioner (10 %).
The level of clinical appropriateness of each MPI test was categorized in each patient according to the AUC criteria [10].
The variables used for this analysis included: age, sex, major cardiovascular risk factors, history of prior coronary artery disease (CAD), previous coronary revascularizations, current medical therapies.
The symptoms referred by the patient at time of the MPI stress test were also evaluated and categorized according to current guidelines [19]. Specifically, chest pain was classified as typical angina, atypical angina, and non-cardiac chest pain, and other signs and symptoms including dyspnoea, palpitations, and abnormal ECG were captured, according to the 2009 AUC for radionuclide imaging, as potential ischemic equivalents.
The study was approved by the Local Ethical Committee and conformed to the Declaration of Helsinki on human research. Written informed consent was obtained from every patient.
AUC classification and assumption
The assessment of the level of appropriateness of MPI studies was defined for each indication following the hierarchical flowchart outlined in the 2009 AUC document [10]. Accordingly, in order to correctly evaluate the level of appropriateness of the single test the following assumptions were made:
-
1.
in accordance with the 2009 AUC for radionuclide imaging document, chest pain was classified as typical angina, atypical angina or non cardiac chest pain;
-
2.
patients were considered symptomatic in presence of any constellation of clinical findings that the physician felt to be consistent with obstructive CAD (i.e. ischaemic equivalent),
-
3.
in accordance with the 2009 AUC document, in symptomatic patients the pretest probability (PTP) of CAD (based on age, sex and typical/atypical angina or non anginal chest pain) was classified as follows: very low (<5 %), low (<10 %), intermediate (10–90 %), high (>90 %);
-
4.
patients who underwent MPI tests for symptoms other than typical chest pain, such as in the presence of an ischemic equivalent, were defined to have atypical angina or non anginal chest pain for the purpose of determining the PTP of CAD;
-
5.
the assessment of individual risk in asymptomatic patients was evaluated according to the “Adult Treatment Panel III” reported probability of developing coronary heart disease over the next 10 years and classified as low (<10 %), moderate (10–20 %) or high (>20 %);
-
6.
each patient was classified in a single “clinical scenario” of the sixty-seven listed in the 2009 AUC document [10];
-
7.
in the case of a MPI test that could be classified with more than one indications that had the same level of appropriateness, the indication with the smallest AUC numeric value was assigned;
-
8.
because of the retrospective design of the study, all patients with missing data that were needed for AUC classification, such as medical therapy and results from prior test, were considered unable to be classified.
Analysis of perfusion images
Perfusion images were semi-quantitatively scored according to the 17-segment left ventricular (LV) model and a five-point scale (0-normal, 1-equivocal, 2-moderate, and 3-severe reduction in radioisotope uptake, and 4-absence of detectable tracer uptake) and the summed rest score (SRS) and summed stress score (SSS) were calculated [20]. Accordingly, the summed difference score (SDS), a measure of stress-induced reversible myocardial ischaemia, was computed in every patient. As previously described, presence of moderate ischaemia was indicated if 4 ≥ SDS < 7, while severe ischaemia was recognized in the case of a SDS ≥ 7 [21].
The residence time values needed for the dosimetric evaluation were taken from published reports [22] and entered into the OLINDA software. Adult phantoms for either men or women were taken into account in order to evaluate the average committed effective dose in relation to our diagnostic investigation.
Statistical analysis
The most common indications for appropriate and inappropriate testing were tabulated. The proportion of tests with results that were normal or probably normal by each appropriateness category was determined.
Continuous variables were expressed as mean ± 1 SD, and categorical variables as percentages. Groups were compared for categorical data using Fisher’s exact test and for continuous variables using analysis of variance followed by Fisher’s protected least significant difference for multiple comparisons. All tests were 2-sided; a P < 0.05 was considered to be significant.
Statistical analyses were performed using JMP statistical software (SAS Institute Inc, version 4.0.0) and Stata software (Stata Statistical Software: Release 10, StataCorp. 2007, College Station, TX).
Results
Characteristics of the study population
The clinical characteristics of the enrolled patients are shown in Table 1. The mean age of the population of was 67 ± 11 years, while only 83 (33 %) of the patients were females.
When the clinical indications for MPI stress testing were evaluated, the most frequent ones resulted: the evaluation of ischemia in symptomatic patients after coronary revascularization (indication 55; 43 patients, 17 %); the detection of significant CAD in symptomatic patients with high pre-test probability (indication 5; 42 patients, 17 %); the assessment of individual risk in patient with known CAD and intermediate risk after ECG stress-test (indication 38; 41 patients, 16 %); the detection of CAD in symptomatic patients with intermediate pre-test probability, interpretable ECG and able to exercise (indication 3; 34 patients, 14 %); and the assessment of individual risk in patient with known CAD, new or worsening symptoms and abnormal coronary angiography or abnormal prior stress imaging study (indication 30; 20 patients, 8 %). Seventy-one patients (28 %) presented one of the other AUC indications for MPI stress test (less than 5 % of incidence for each indication) (Fig. 1).
Most common indication for nuclear stress tests. Clinical scenarios: [3] intermediate pretest probability of CAD. ECG interpretable AND able to exercise; [5] high pretest probability of CAD regardless of ECG interpretability and ability to exercise; [30] abnormal coronary angiography OR abnormal prior stress imaging study; [38] Intermediate-risk Duke treadmill score; [55] evaluation of ischemic equivalent
Evaluation of the appropriateness of the imaging studies
According to the accepted criteria [10], the majority of the MPI stress-tests performed could be classified as clinically appropriate (218/251, 87 % of the tests), while only 16 (6 %) and 17 (7 %) resulted of uncertain appropriateness or clearly inappropriate, respectively (Fig. 2).
Specifically, of the 17 patients with inappropriate stress tests, 13 (77 %) were submitted to MPI despite a low pre-test probability of CAD and/or despite the availability of other clinically indicated, less-expensive, stress modalities, while the remainders underwent MPI despite being clearly asymptomatic and at relatively low risk of CAD (Table 2).
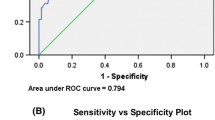
Correlation between appropriateness and scintigraphic results
The relationship between stress-tests’ appropriateness and ischemic burden on MPI was analyzed.
Interestingly, while the majority of the clinically appropriate MPI tests demonstrated the presence of a moderate-to-severe ischemic burden, only a marginal proportion of the stress-tests with uncertain clinical appropriateness or clearly inappropriate revealed a relevant myocardial ischemic burden.
Specifically, of the 218 appropriate tests, 22 (10 %), 65 (30 %), and 131 (60 %) showed the presence of mild (SDS < 4), moderate (4 ≥ SDS < 7), and severe (SDS ≥ 7) ischemia, respectively. On the other hand, of the 16 patients submitted to MPI despite an uncertain clinical appropriateness, 6 (38 %) showed a SDS < 4, while only 9 (56 %) and 1 (6 %) presented a moderate and severe ischemic burden, respectively. Finally, of the 17 inappropriate tests, the great majority (13, 76 %) showed normal-to-mildly abnormal MPI results, while in no patient the presence of severe myocardial ischemia was revealed (P < 0.001 for comparisons between groups).
Radiation exposure
As expected, no difference regarding the global radiation burden of the MPI tests was observed between the different patients’ categories. Specifically, patients’ radiation burden remained considerably low, irrespective of appropriateness categories: the mean injected doses were 177.23, 172.22, and 176.24 MBq for stress studies, and 377.98, 362.88, and 362.88 MBq for rest studies in case of appropriate, uncertain, and inappropriate MPI tests, respectively (P = NS between groups).
Discussion
Present data, obtained in a consecutive cohort of patients studied in a single high-volume center, indicate that the majority of the clinical indications for MPI stress-test are in accordance with the AUC criteria, while only a minor subgroup of subjects was submitted to MPI with inappropriate or uncertain indications.
Considering the time-period of the analyzed MPI stress-tests (January–March 2015), our data represent a close picture of the population currently submitted to MPI, offering a snapshot of the main clinical indications for stress radionuclide imaging with the pertinent level of appropriateness.
Pointing the accent on the high level of appropriateness of MPI studies that was observed in the present study, our results are very encouraging since they reflect consistent differences in ordering patterns with respect to previously published data obtained in different practice and temporal settings [9, 16, 17].
The role that the evaluation of test’s appropriateness plays in current clinical practice is exemplified by the fact that, in the last decade, audits and training courses involving cardiologist, general practitioners, and nuclear medicine specialists have been developed and implemented on the basis of the dedicated guidelines.
This point is crucial for improving the accuracy in the application of the criteria of clinical appropriateness of a given imaging modality [10]. As a matter of fact, only when a proper knowledge of clinical evidences is coupled by a deep understanding of the technical characteristics of the different imaging modalities, appropriate indications are favored over inappropriate ones, reducing sanitary costs and patients’ overall risk burden [23].
In line with this way of thinking, the presence in our laboratory of a dedicated specialist in nuclear cardiology (specialized in both cardiology and nuclear medicine) has allowed to improve the quality of the service, both on a technical and clinical point of view. This “double gatekeeper” is one of the critical point of the whole process, since it allows a rapid and effective exchange of information between the different medical figures (general practitioner, clinical and interventional cardiologist) involved in the management of a specific patient, paving the way for an increase in the level of clinical appropriateness of the imaging studies for the referring physicians as well as for the involved nuclear cardiologist.
This way of conduct is in line with the new strategy of the European Association of Cardio-Vascular Imaging that, on behalf of the European Society of Cardiology, tries to stimulate and disseminate the knowledge and the use of cardiac imaging through education, quality control, research, and training. In particular, the European Association of Cardio-Vascular Imaging provides the foremost individual certification and laboratory accreditation programs for professional excellence in Europe with the aim is to raise quality standards of practice across Europe in a uniform manner, improving accuracy and reducing costs.
The second and closely related issue of this study relies on the clinical impact of the use of appropriateness criteria. In fact, only when an indication for MPI is in agreement with the current guidelines and/or with the accepted AUC criteria, one may expect a consistent reduction of both radiation exposure and sanitary costs, helping to increase a patient-oriented clinical decision-making. Ideally, in fact, a cardiovascular imaging test should significantly alter patient management, theoretically improving the clinical outcome [24].
Accordingly, our data showed that moderate-to-severe myocardial ischaemia was mainly observed in appropriately referred patients (>90 %), while could be revealed only in a marginal proportion of studies with uncertain clinical appropriateness or clearly inappropriate, that, almost by definition, identified patients at lower cardiovascular risk, i.e. asymptomatic patients with low pre-test probability of CAD.
Therefore, the application of AUC criteria in routine clinical practice can reduce unnecessary testing, helping to concentrate clinical efforts on those intermediate-risk patients, where the result of the test is more likely to effect the cardiological management and overall clinical outcome, possibly reducing healthcare costs and downstream high-risk investigation, such as invasive coronary interventions.
Of interest, we found that 41 % of all uncertain examinations and 34 % of all inappropriate examinations were due to 1 and 2 indications, respectively. This highly repetitive pattern of inappropriateness points to the need for educational programs to achieve further improvements in the quality of ordering indications.
Since in the present study no comparison between stress modalities has been made, our results do not, obviously, allow to state that MPI is the preferred stress-test modality in patients with suspected or known CAD over, for example, wall-motion imaging (stress echo or magnetic resonance). Multi-imaging outcome studies that included the categorization of patients for level of test appropriateness are deeply needed to address this topic of key clinical relevance.
Study limitations
Several limitations should be acknowledged. The first limitation is that this is a single center study, possibly introducing a selection bias.
Despite being a retrospective database, all patients submitted to MPI in a predetermined time-interval were consecutively enrolled. Moreover, in the entire study population all data entered the database at the time of initial assessment without any filter.
Only published guidelines were considered as the only reference standards for the evaluation of the level of clinical appropriateness of a given test. In this respect, the approach for defining tests’ appropriateness from guidelines is simple but is limited because this process does not allow the evaluation of specific clinical nuances according to the situation of the patient. In addition, most of the guidelines and society recommendations are based on level of evidence C, which is the consensus of the monitoring committee in the absence of a firm evidences [21].
In the present study, ejection fraction was not considered as an enrollment criteria, therefore prohibiting any meaningful conclusion about the prevalence of heart failure in the population analyzed.
Finally, since most of the MPI tests were referred by clinical cardiologists, the observed level of appropriateness might theoretically being spuriously increased. On the other hand, the obtained results point to the importance of the clinical competence of the referring physician to increase test’s appropriateness.
Conclusions
Tests’ appropriateness is mandatory in contemporary medicine and is the fruit of a paradigm shift in health care towards a more cost-affordable and patient-oriented clinical approach.
Our results show how the rate of inappropriate MPI tests is considerably low in a high-volume laboratory and provide insights into the clinical performance of radionuclide imaging appropriateness criteria on test results, since appropriate and inappropriate studies identify patients at high and low probability of significant ischemia, respectively.
References
Iglehart JK (2006) The new era of medical imaging—progress and pitfalls. N Engl J Med 354:2822–2828
Fazel R, Krumholz HM, Wang Y, Ross JS, Chen J, Ting HH et al (2009) Exposure to low-dose ionizing radiation from medical imaging procedures. N Engl J Med 361:849–857
Rozanski A, Gransar H, Hayes SW, Min J, Friedman JD, Thomson LE et al (2013) Temporal trends in the frequency of inducible myocardial ischemia during cardiac stress testing: 1991 to 2009. J Am Coll Cardiol 61:1054–1065
Lucas FL, DeLorenzo MA, Siewers AE, Wennberg DE (2006) Temporal trends in the utilization of diagnostic testing and treatments for cardiovascular disease in the United States, 1993–2001. Circulation 113:374–379
Redberg R (2007) The appropriateness imperative. Am Heart J 154:201–202
Shaw LJ, Marwick TH, Zoghbi WA, Hundley WG, Kramer CM, Achenbach S et al (2010) Why all the focus on cardiac imaging? J Am Coll Cardiol Cardiovasc Imaging 3:789–794
Gibbons RJ (2008) Finding value in imaging: what is appropriate? J Nucl Cardiol 15:178–185
Einstein AJ, Weiner SD, Bernheim A, Kulon M, Bokhari S, Johnson LL et al (2010) Multiple testing, cumulative radiation dose, and clinical indications in patients undergoing myocardial perfusion imaging. JAMA 304:2137–2144
Shaw LJ, Hachamovitch R, Berman DS, Marwick TH, Lauer MS, Heller GV et al (1999) The economic consequences of available diagnostic and prognostic strategies for the evaluation of stable angina patients: an observational assessment of the value of precatheterization ischemia: economics of noninvasive diagnosis (END) multicenter study group. J Am Coll Cardiol 33:661–669
Hendel RC, Berman DS, Di Carli MF, Heidenreich PA, Henkin RE, Pellikka PA et al, American College of Cardiology Foundation Appropriate Use Criteria Task Force; American Society of Nuclear Cardiology; American College of Radiology; American Heart Association; American Society of Echocardiology; Society of Cardiovascular Computed Tomography; Society for Cardiovascular Magnetic Resonance; Society of Nuclear Medicine. ACCF/ASNC/ACR/AHA/ASE/SCCT/SCMR/SNM (2009) Appropriate use criteria for cardiac radionuclide imaging: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the American Society of Nuclear Cardiology, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the Society of Cardiovascular Computed Tomography, the Society for Cardiovascular Magnetic Resonance, and the Society of Nuclear Medicine. J Am Coll Cardiol 53:2201–2229
Hendel RC, Cerqueira M, Douglas PS, Caruth KC, Allen JM, Jensen NC et al (2010) Multicenter assessment of the use of single photon emission computed tomography myocardial perfusion imaging with appropriateness criteria. J Am Coll Cardiol 55:156–162
Gibbons RJ, Askew JW, Hodge D, Kaping B, Carryer DJ, Miller T (2011) Appropriate use criteria for stress single-photon emission computed tomography sestamibi studies: a quality improvement project. Circulation 123:499–503
Lin FY, Dunning AM, Narula J, Shaw LJ, Gransar H, Berman DS et al (2013) Impact of an automated multimodality point-of-order decision support tool on rates of appropriate testing and clinical decision making for individuals with suspected coronary artery disease: a prospective multicenter study. J Am Coll Cardiol 62:308–316
Gibbons RJ, Askew JW, Hodge D, Miller TD (2010) Temporal trends in compliance with appropriateness criteria for stress single-photon emission computed tomography sestamibi studies in an academic medical center. Am Heart J 159:484–489
Saifi S, Taylor AJ, Allen J, Hendel R (2013) The use of a learning community and online evaluation of utilization for SPECT myocardial perfusion imaging. JACC Cardiovasc Imaging 6:823–829
Doukky R, Hayes K, Frogge N, Balakrishnan G, Dontaraju VS, Rangel MO et al (2013) Impact of appropriate use on the prognostic value of single-photon emission computed tomography myocardial perfusion imaging. Circulation 128:1634–1643
Ye S, Rabbani LE, Kelly CR, Kelly MR, Lewis M, Paz Y et al (2015) Can physicians identify inappropriate nuclear stress tests? An examination of inter-rater reliability for the 2009 appropriate use criteria for radionuclide imaging. Circ Cardiovasc Qual Outcomes 8:23–29
Fazel R, Gerber TC, Balter S, Brenner DJ, Carr JJ, Cerqueira MD, American Heart Association Council on Quality of Care and Outcomes Research, Council on Clinical Cardiology, and Council on Cardiovascular Radiology and Intervention et al (2014) Approaches to enhancing radiation safety in cardiovascular imaging: a scientific statement from the American Heart Association. Circulation 130:173-48
Members Task Force, Montalescot G, Sechtem U, Achenbach S, Andreotti F, Arden C, Budaj A et al (2013) ESC guidelines on the management of stable coronary artery disease: the task force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J 2013(34):2949–3003
Gimelli A, Bottai M, Genovesi D, Giorgetti A, Di Martino F, Marzullo P (2012) High diagnostic accuracy of low-dose gated-SPECT with solid-state ultrafast detectors: preliminary clinical results. Eur J Nucl Med Mol Imaging 39:83–90
Marini C, Acampa W, Bauckneht M, Daniele S, Capitanio S, Cantoni V et al (2015) Added prognostic value of ischaemic threshold in radionuclide myocardial perfusion imaging: a common-sense integration of exercise tolerance and ischaemia severity. Eur J Nucl Med Mol Imaging 45:750–760
Highley B, Smith FW, Smith T, Gemmell HG, Das Gupta P, Gvozdanovic DV et al (1993) Technetium 99 m-1,2-bis(bis(2-ethoxyethyl)phosphino)ethane: human biodistribution, dosimetry and safety of a new myocardial perfusion agent. J Nucl Med 34:30–38
Carpeggiani C, Kraft G, Caramella D, Semelka R, Picano E (2012) Radioprotection (un)awareness in cardiologists, and how to improve it. Int J Cardiovasc Imaging 28:1369–1374
Muzzarelli S, Pfisterer ME, Müller-Brand J, Zellweger MJ (2010) Gate-keeper to coronary angiography: comparison of exercise testing, myocardial perfusion SPECT and individually tailored approach for risk stratification. Int J Cardiovasc Imaging 26:871–879
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Human and animal rights
This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Gimelli, A., Rovai, I., Liga, R. et al. Appropriate use criteria in clinical routine practice: implications in a nuclear cardiology lab. Int J Cardiovasc Imaging 32, 1003–1009 (2016). https://doi.org/10.1007/s10554-016-0864-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-016-0864-6