Abstract
Microvascular obstruction (MVO) and transmural infarct size are prognostic factors after acute myocardial infarction (AMI). We assessed the value of myocardial deformation patterns using 3D speckle tracking imaging (3DSTI) in detecting myocardial and microvascular damage after AMI. One hundred patients with first ST-segment elevation MI from the REMI Study were prospectively included. Transthoracic echocardiography with 3DSTI and CMR were performed within 72 h after revascularization therapy. Global (3DG) and segmental (3DS) values of LV longitudinal (LS), circumferential and radial area strain were obtained. Late gadolinium enhancement (LGE) and MVO was quantified as transmural (>50 %) or non-transmural (<50 %). Predictive performance was assessed by area under the receiver operating curve characteristic (AUC). Mean LVEFCMR was 45.8 ± 9.2 % with 22.2 ± 12.7 % transmural LGE. MVO was present in 55 patients (MVO transmural extent 11.4 ± 11.8 %). In global analysis, all 3DG strain values were correlated with LVEFCMR and infarct size, with the best correlation obtained for 3DGAS (r = −0.678; p < 0.0001). All 3DG strain values, with the exception of LS, were significantly different between patients with and without MVO. In segmental analysis, all 3DS strain values were significantly lower in transmurally infarcted segments than in non-infarcted segments, and all 3DS values except 3DSRS were significantly lower in non-transmural infarcted segments than in non-infarcted segments. The best 3DS strain for detecting non-viable segments with MVO (MVO > 75 %) was 3DSAS [AUC 0.867 (0.849–0.884), 78.0 % sensitivity and 81.1 % specificity for 3DSAS = −16.1 %]. Importantly, 3DSRS and 3DSAS were associated with an increase in diagnostic accuracy of both transmural LGE and MVO over 3DSLS (all increase in AUC > 0.04, all p < 0.01). The newly developed 3DSTI, especially 3DSAS, is a sensitive and reproducible tool to predict and quantify the transmural extent of scar. This new early imaging strategy improve the prediction of MVO while enabling to assess the success of reperfusion and the risk of late systolic remodeling in STEMI.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Left ventricular (LV) ejection fraction (EF) remains the main prognostic indicator for adverse outcomes after an acute myocardial infarction (AMI) [1]. However, with the enhanced performance of new revascularization therapies, risk stratification has become increasing challenging in patients with smaller infarct sizes.
A significant association between infarct size and major adverse cardiac events has been demonstrated although the correlation between infarct size and LVEF is modest in patients with relatively preserved LVEF and ST-elevation MI (STEMI) undergoing revascularization [2].
Microvascular obstruction (MVO) has been recently extensively studied and found to have additional predictive value for adverse LV remodeling, permanent inability to recover contractility and subsequent cardiovascular events, regardless of infarct size [3]. Additionally, cardiac magnetic resonance imaging (CMR) has gained a pivotal role in assessing myocardial viability and in defining microvascular damage and salvaged myocardium [4]. Unfortunately, CMR is rarely performed in the acute phase of STEMI mainly due to lack of machine time and to hemodynamic and/or respiratory instability [5].
Two-dimensional (2D) deformation parameters derived from speckle tracking imaging (STI) have been introduced as markers of systolic function and display better correlation with infarct size than conventional transthoracic (TTE) LVEF [6]. Previous studies have mainly focused on 2D longitudinal strain (2DLS), probably because of its easier collection from the 3 apical views as compared to radial (RS) and circumferential (CS) components calculated from short axis acquisitions which are more likely to have poorer tracking quality. [7]. But several studies have highlighted the additional value of CS to differentiate transmural from non-transmural lesions as well as in predicting remodeling [8]. These results emphasize the need for a distinct assessment of longitudinal, radial and circumferential functions in order to avoid the loss of useful information. Accordingly, three-dimensional STI (3DSTI) has been validated as a new and reliable quantification tool to assess the 3 components of deformation [9] in addition to providing supplemental deformation information called area strain. Since the latter takes into account both longitudinal and circumferential components of myocardial deformation, it allows a more accurate assessment of regional function, a parameter of growing interest in ischemic myocardial diseases [10, 11].
The aim of the present study was to evaluate the feasibility and accuracy of 3DSTI to detect the presence, extent and degree of scar transmurality and microvascular damage (MVO) in the acute phase of STEMI as compared to CMR late gadolinium enhancement (LGE).
Materials and methods
Populations
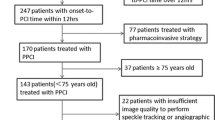
The study population encompassed all patients with successfully reperfused first acute STEMI included in a prospective monocentric cohort study (relation between aldosterone and cardiac remodeling after myocardial infarction—REMI Study) designed to determine whether aldosteronemy is predictive of cardiac remodeling in the 6 months following a STEMI performed in a university hospital between April 2010 and December 2013. Acute STEMI was confirmed by: <12 h of typical chest pain onset and angiographically-confirmed coronary artery acute occlusion or subocclusion (Thrombolysis In Myocardial Infarction flow grade 0–1). The Ethics Committee approved the trial and all patients provided written informed consent.
Cardiac function was assessed by CMR and echocardiography between the second and fifth day (median delay between TTE and CMR 155 min) following percutaneous transluminal coronary angioplasty (PTCA). Exclusion criteria were any counter-indication with CMR examination or inability to participate in a long-term trial.
A total of 111 patients with first STEMI were enrolled in the study of which 11 could not be analyzed due to lack of interpretable 3D echocardiographic images (n = 7; poor image quality; low frame rate, stitching artefacts) and/or of CMR study (n = 4; poor image quality of LGE sequence). A control group comprised of 100 healthy adults from a monocentric familial longitudinal cohort of STANISLAS COHORT; 88 males, mean age 54.9 ± 12.0 years, NS vs. STEMI group) underwent thorough clinical evaluations to exclude cardiac disease with normal conventional echocardiography.
Echocardiographic imaging and analysis
Echocardiography was performed with a commercially available standard ultrasound scanner (Vivid 9, General Electric Medical Systems) with a 2.5-MHz transducer and a 3D probe (4 V Volume Phased Array Probe).
3D image acquisition
Echocardiographic acquisition was performed according to EAE/ASE guideline recommendations for 3DTTE image acquisition [12]. From this acquisition, an automated software (4D Auto LV Quantification tool; EchoPAC PC, version 110.1.0, GE Healthcare) was used to obtain both standard and 3DSTI derived parameters. The software provides the following standard 3D echocardiographic parameter values: end-diastolic (3DLVEDV, ml) and end-systolic volumes (3DLVESV, ml) and LV ejection fraction (3DLVEF, %).
In addition, the software provides peak systolic values of longitudinal, radial and circumferential strain (S) of each of the 17 LV segments and of their mean values [3D global longitudinal strain (3D GLS), 3D global circumferential strain (3D GCS) and 3D global radial strain (3D GRS)] and area strain (3D GAS). Feasibility and reproducibility were studied including the tracking rate (Fig. 1).
3D transthoracic echocardiography and representative case of anterior infarction related to the occlusion of the proximal left anterior descending coronary artery. CMR late gadolinium enhancement slices of left ventricular short axis (SAX) and horizontal long axis (HLAX) showing transmural extension of myocardial infarct in anterior and antero-septal zones and central hypoenhancement defining microvascular obstruction (yellow arrow); and Bull eye’s view of 3D Segmental longitudinal (3DSLS), radial (3DSLS), circumferential (3DSLS) and area strain (3DSAS) measured by 3D speckle tracking imaging
Cardiac magnetic resonance
CMR was performed between the second and fifth day on a GE 3T system (General Electric 3T signa HDxt) with a phased-array cardiac coil, ECG gating and breath-holding in expiration. Cine imaging for cardiac morphology and function was performed by the steady-state free precession technique. The endocardial contours of the left and right ventricle were traced manually on all phases and slices using standard software (Mass Analysis +, 4 version, Medis, Netherlands).
Late gadolinium-enhanced (LGE) imaging was acquired 10–15 min after a cumulative total dose of 0.3 mmol/kg Gd contrast in matched short and long-axis planes with a T1-weighted 2D segmented inversion recovery gradient-echo sequence during diastolic standstill. The LGE imaging parameters included a 4.8/1.3 ms repetition time/echo time with a 200–300 ms inversion time adjusted to null normal myocardium.
Transmural LGE extent was assessed visually and scored on a 17-segment model on 3 matched short-axis slices (basal, mid, apical) [13]. The segmental extent of the LGE was considered as non-infarcted if there was no LGE. In case of hyperenhancement, infarcted segments were classified as transmural if LGE > 50 % of mural extent, non-viable if LGE > 75 % and non-transmural if LGE < 50 %. MVO was identified by the presence of a central hypoenhancement within the bright signal within the infarcted segments, usually located in the subendocardium and included as part of the infarct. In presence of MVO, the infarcted segment was defined as transmural (MVO > 50 %) or non-transmural (MVO < 50 %). Analysis of MVO and LGE series was performed independently from, and blinded to, the results of 3D echocardiography.
Statistical analysis
Statistical analysis was performed using SPSS for Windows (SPSS version 20, Chicago, IL). Quantitative values are expressed as mean values ± SD. Intergroup comparisons were performed by the independent samples Student t test or Mann–Whitney U test when appropriate. For multiple comparisons, analysis of variance along with a post hoc Bonferroni test was performed. Pearson correlation was used to study correlation and concordance between 3DTTE and CMR. As used previously, receiver-operator characteristic (ROC) along with tracing of the area under the curve (AUROC) was performed to identify a 3D segmental strain value to define LGE and MVO transmurality (>75 %) [14]. Direct comparisons of AUC were then performed to quantify the increase in diagnostic accuracy between techniques.
3D strain measurements were repeated by two independent observers. Inter- and intra-observer reproducibility of 3D strain measurement was analyzed among 15 patients of the STEMI group. Agreements were assessed using the intraclass correlation coefficient (ICC) for quantitative 3DSTI values and using Kappa analysis for qualitative CMR LGE data.
For all tests, a p value < 0.05 was considered to indicate statistical significance.
Results
Baseline characteristics
One hundred patients had both CMR and 3DTTE assessments. Mean age was 55.8 ± 10.4 years with most patients being men (87/100, 87 %). The mean delay between CMR and TTE was 19.2 ± 23.1 h.
Fifty-six patients (44 %) had inferior MI, among whom 9 (9 %) had infero-lateral MI, and 44 (56 %) had anterior MI. Reperfusion therapy was achieved in a delay of 277.7 ± 199.3 min after symptoms onset. The culprit vessel was left anterior descending coronary artery (LAD) in 53 patients (53 %), diagonal LAD branch in 6 patients (6 %), circumflex artery (Cx) in 6 patients (6 %), marginal Cx branch in 3 patients (3 %) and right coronary artery in 35 patients (35 %) (Table 1).
Global left ventricular function assessment
The overall mean LVEFCMR was 45.8 ± 9.2 % and 3DLVEFTTE 52.9 ± 8.1 % (Table 2). A moderate correlation was observed between LVEFCMR and global 3DSTI parameters (3DGLS r = 0.595; 3DGCS r = 0.608; 3DGRS r = 0.632; 3DGAS r = 0.678; all correlation p values p < 0.0001) which were similar or superior to 3DLVEFTTE (r = 0.569). Weaker correlations between the percentage of transmural infarct size and echocardiographic 3DSTI parameters were observed (r = 0.386 for 3DLVEFTTE, 0.400 for 3DGLS, 0.397 for 3DGCS, 0.418 for 3DRS and 0.446 for 3DGAS, p < 0.0001).
Infarcted segment analysis
Overall, 1577 of 1700 segments (92.7 %) were analyzable by CMR and 3DSTI. CMR identified 441 infarcted segments (378 with transmural and 63 with non-transmural extent) which accounted for 25.95 % of total myocardium, and 1136 non-infarcted segments (figure supplemental material).
A decrease absolute 3D strain value was noted in all infarcted segments compared to non-infarcted segments. Among myocardial necrotic segments, all absolute 3D strain values were significantly decreased compared to control values and all absolute strain values were also significantly lower in segments with transmural comparatively to segments with non-transmural scar extent (Fig. 2). Furthermore, non-infarcted segments had significantly lower absolute values than control segments for all strains with the exception of radial strain (Table 3).
Among infarcted and non-infarcted segments 3DAS, 3DCS and 3DRS had an AUROC > 0.80 in detecting the transmural non-viable segments (LGE > 75 %) suggesting good predictive values whereas 3SDLS had lower AUROC (0.752) (Fig. 3). Importantly, 3DSRS, 3DSAS and 3DSCS were significantly associated with an increase in diagnostic accuracy of transmural LGE (LGE > 75 %) over 3DSLS (all increase in AUC > 0.05, all p < 0.001). 3DSRS was associated with an increase in prediction of transmural LGE of 0.072 (0.054–0.090) over 3DSLS (p < 0.001) and of 0.017 (−0.001 to 0.033) over 3DSCS (p = 0.06). Likewise, 3DSAS as associated with an increase in prediction of transmural LGE of 0.073 (0.056–0.091) over 3DSLS (p < 0.001) and of 0.018 (0.000–0.035) over 3DSCS (p = 0.04). 3DSCS was also associated with a significant increase in diagnostic accuracy of transmural LGE over 3DSLS [AUC delta 0.055 (0.023–0.087), p < 0.001] but to a lower extent that what was observed with 3DSRS and 3DSAS.
ROC curves of 3D segmental longitudinal (3DSLS), radial (3DSLS), circumferential (3DSLS) and area strain (3DSLS) measured by 3D speckle tracking imaging for distinction of non-viable segments (Late gadolinium enhancement >75 %) on the left panel and microvascular obstruction >75 % on the right panel
Microvascular obstruction segment analysis
MVO was diagnosed in 172 segments (107 with transmural and 65 with non-transmural extent) in 55 patients (55 %) accounting for a mean MVO extent of 10.4 % of total myocardium. Patients with MVO had significantly larger myocardial infarct size, lower LVEF and higher total creatinine kinase peak (Table 1). Transmural segments with transmural MVO had significant lower segmental strain value than other transmural segments (Table 3).
The distinction between transmural segments with and without MVO was also more accurate using area strain as opposed to using the isolated longitudinal component of myocardial deformation (Table 3). When considering non-viable transmural MVO segments (LGE > 75 and MVO > 75 %), 3DAS and 3DRS had an AUROC > 0.85 while 3DLS and 3DCS strains had an AUROC > 0.80 (Fig. 3). Importantly, 3DSRS and 3DSAS were associated with an increase in diagnostic accuracy of transmural MVO (LGE > 75 and MVO > 75 %) over 3DSLS and 3DSCS (all increase in AUC > 0.03, all p < 0.05). Specifically, 3DSRS was associated with a significant increase in prediction of MVO of 0.047 (0.018–0.076) over 3DSLS (p = 0.001) and of 0.041 (0.009–0.073) over 3DSCS (p = 0.01). Likewise, 3DSAS was associated with a significant increase in prediction of MVO of 0.044 (0.015–0.073) over 3DSLS (p = 0.003) and of 0.037 (0.005–0.070) over 3DSCS (p = 0.03). In contrast, 3DSCS was not associated with an increase in diagnostic accuracy of MVO over 3DSLS (AUC delta 0.007 (−0.052 to 0.065), p = 0.82).
Inter- and intra-observer variability
Inter- and intra-observer variability for 3D segmental strain with tracking quality assessment and CMR segmental qualification (LGE and MVO segments) is described in Table 4.
Control group
By definition, the 100 patients of the control group had normal systolic function (3DLVEFTTE 62.6 ± 4.4 %; 3DLVEDV 88.0 ± 26.7 mL/m2) and mean deformation values of −34.8 ± 8.9 % for 3DGAS, −19.9 ± 5.9 % for 3DGLS, −19.5 ± 6.2 % for 3DGCS and 56.2 ± 19.1 % for 3DGRS [15].
Discussion
The main findings of this study can be summarized as follows: (1) in patients with STEMI undergoing early PTCA, 3D global strain values were better correlated with LVEFCMR than 3DLVEFTTE and had a good predictive value of transmural extent; (2) MVO as determined by CMR was a relatively frequent finding being present in 55 % of cases and was well differentiated by all 3D strains except longitudinal strain; (3) with regard to segmental analysis, 3DSAS, which takes into account both longitudinal and circumferential motion, represented the best tool to discriminate LGE with or without MVO in non-viable segments.
As previously reported, we found that 3DLVEFTTE overestimated LVEF as measured by CMR along with a modest correlation between infarct size and 3DLVEFTTE [16]. Meanwhile, the 3DSTI technique for LV volume measurements has been validated and demonstrated superior accuracy and reproducibility over previously used 2DSTI technique [17]. In our study, all global 3D strains showed good to moderate correlations with the gold standard LVEFCMR and infarct size, with 3DGAS having the highest correlation coefficient among all strain parameters.
At the segmental level, our data confirmed a significant difference in longitudinal function between non-transmural and transmural infarcted segments. Longitudinal function is known to be attenuated independently of scar transmurality [18]. Indeed subendocardial fiber layers have the most significant contribution to long-axis function compared to the middle and subepicardial layers which mainly contribute to wall thickening as well as radial and circumferential function. Indeed, Takeuchi et al. [19] showed that longitudinal function was altered in small subendocardial MI whereas circumferential deformation and short axis function were initially preserved. This longitudinal alteration is usually associated with compensatory circumferential mechanics thus becoming a key determinant of preserved global LV function [20].
Numerous studies have already shown the potential diagnostic value of circumferential strain in discriminating non-transmural and transmural infarction although only using 2DSTI [21]. However, 2D assessment of circumferential strain requires acquisition of 3 short axis views and heart rate; in addition, loading conditions may change between different acquisitions and therefore influence deformation values. Moreover, only one parasternal short axis view at the level of the papillary muscle was performed in most of the above studies. To the best of our knowledge, the present study is the first to assess radial and circumferential deformation over the 17-segments in 3 dimensions. Beyond the analysis of LV volumes, 3DSTI allows the assessment of the different myocardial layer functions by avoiding poor speckle tracking as encountered in monoplane 2D analysis.
Motion assessment of all 17 myocardial segments is performed in a single analysis step, which significantly reduces analysis time. In the present series, we observed a gradual decrease in absolute strain values in the 3 directions of myocardial motion in parallel with the gradual importance of transmural damage. A threshold value of −20.0 % was defined herein for 3DSAS enabling to discriminate LGE transmurality (>75 %) with good diagnostic values. Previous studies with smaller patient samples concluded that 3DSTI can determine transmural involvement and therefore the viability of the infarcted segment [22].
There is currently no consensus as to how and when MVO should be assessed after AMI. Accurate detection and quantification of MVO is important since previous studies have shown that MVO is independently associated with adverse ventricular remodeling and patient prognosis [3]. In our study, although 100 % of the patients had a TIMI flow grade 3 after PTCA with acceptable revascularization delay, MVO was nonetheless diagnosed by CMR in 55 % of cases at day 3. Hence, there is clearly a need for “in-lab” tools able to assist in the early identification of patients at increased risk of MVO. Rather than ECG or per procedural myocardial blush grade, CMR is currently considered to be the most reliable method for determining MVO in the first days after reperfusion [23]. However, CMR has a number of limitations, including cost and accessibility. Our findings furthermore indicate that <10 % patients have CMR in the first month following AMI. In the acute phase of MI, segmental and global 2DLS have been shown to be significantly altered by the presence of MVO in addition to MI size [24]. 2DSTI has recently emerged as valuable tool to precociously assess microvascular damage, after a STEMI as well as a marker for persistent akinetic territories [25]. Herein, we confirm a close association between myocardial deformation and the degree of MVO. Our data reveal that both 3DSRS and 3DSCS were further decreased with MVO while displaying a marked decrease in their absolute values in segments with MVO > 50 %. Moreover, the combined analysis of longitudinal and circumferential deformation through 3DSAS was the main indicator in differentiating transmural non-viable segments with or without MVO. On the other hand, 3DLS was shown to be altered irrespective of the presence or absence of MVO. These results thus support the theory of cross-fiber shortening suggesting that passive radial thickening of segments with non-transmural infarction is generated by the shortening of viable epicardial fibers. In the case of transmural no-reflow segments, the circumferential fibers, which are predominant in the mid layer of myocardium, are severely damaged [26].
Assessment of the presence and extent of MVO is a surrogate endpoint for therapeutic strategies due to adverse LV remodeling in case of MVO. The ACC/AHA guidelines for management of STEMI have stressed the importance of the development of simple, accurate, readily available noninvasive techniques to assess adjunctive reperfusion agents and revascularization therapy strategies and to evaluate the no-reflow phenomenon within the first hours of MI [27]. After a STEMI, CMR is increasingly used for coronary microvascular status assessment and quantification of infarct size [28]. Unfortunately, CMR is rarely performed in acute phase of MI (<10 %) in most countries and hospitals due mainly to a lack of machine time [5]. 3DSTI is an accessible prognostic marker that could identify patients with microvascular dysfunction after reperfusion at the acute phase of MI. Indeed, the assessment of segmental deformation can be used to identify the localization of MI and monitor microvascular damage. As a result, 3DSTI could represent a useful tool to detect those patients with MVO in whom access to MRI is difficult during their initial hospital stay for AMI. Given the high prognostic value of MVO after MI, therapeutic interventions and the intensity of follow-up could hence be adequately adapted in patients likely to have MVO based on 3DSTI evaluation. Further studies assessing the pragmatic clinical usefulness of this 3DTSI-based strategy are warranted.
Limitations
The main limitation of the present study is the small infarct size with low proportion of transmural segments, which may explain the modest correlations of LVEFCMR and infarct size with TTE parameters. However, these limited infarct sized are the reflection of the evolution of modern cardiology, especially in tertiary centers. In addition, it is in these patients with limited infarct size that risk assessment is the most difficult, thus increasing the potential usefulness of new 3DSTI methods in this population.
Conclusions
The use of 3D deformation in the acute phase of a MI may represent an easy, fast and reliable means to assess myocardial deformation of MVO in the infarcted area. Global deformation analysis helps in the assessment of MI and, more specifically, the new area strain parameter is best correlated with the reference LVEFCMR and differentiates patients with and without MVO. In addition, regional 3D deformation can estimate LV regional mechanics of scarring and yield reliable results in discriminating transmural from non-transmural extent. Indeed, results herein demonstrated a close association between myocardial deformation in patients with a recent AMI and the degree of diminished microcirculation. Circumferential strain value was severely altered in the no-reflow segment and showed notable diagnostic value in the differentiation of infarcted segments with and without no-reflow.
References
Sanz G, Castañer A, Betriu A, Magriña J, Roig E, Coll S et al (1982) Determinants of prognosis in survivors of myocardial infarction: a prospective clinical angiographic study. N Engl J Med 306(18):1065–1070
Pride YB, Appelbaum E, Lord EE, Sloan S, Cannon CP, Sabatine MS et al (2009) Relation between myocardial infarct size and ventricular tachyarrhythmia among patients with preserved left ventricular ejection fraction following fibrinolytic therapy for ST-segment elevation myocardial infarction. Am J Cardiol 104(4):475–479
De Waha S, Desch S, Eitel I, Fuernau G, Zachrau J, Leuschner A et al (2010) Impact of early vs. late microvascular obstruction assessed by magnetic resonance imaging on long-term outcome after ST-elevation myocardial infarction: a comparison with traditional prognostic markers. Eur Heart J 31(21):2660–2668
Schuleri KH, Centola M, Evers KS, Zviman A, Evers R, Lima JA et al (2012) Cardiovascular magnetic resonance characterization of peri-infarct zone remodeling following myocardial infarction. J Cardiovasc Magn Reson 14(1):24
Products - Health United States - Tables - 2011 Complete List [Internet] (2014). http://www.cdc.gov/nchs/hus/contents2011.htm#123
Gjesdal O, Helle-Valle T, Hopp E, Lunde K, Vartdal T, Aakhus S et al (2008) Noninvasive separation of large, medium, and small myocardial infarcts in survivors of reperfused ST-elevation myocardial infarction: a comprehensive tissue Doppler and speckle-tracking echocardiography study. Circ Cardiovasc Imaging 1(3):189–196 2 p following 196
Ersbøll M, Valeur N, Mogensen UM, Andersen MJ, Møller JE, Hassager C et al (2012) Relationship between left ventricular longitudinal deformation and clinical heart failure during admission for acute myocardial infarction: a two-dimensional speckle-tracking study. J Am Soc Echocardiogr 25(12):1280–1289
Altiok E, Tiemann S, Becker M, Koos R, Zwicker C, Schroeder J et al (2014) Myocardial deformation imaging by two-dimensional speckle-tracking echocardiography for prediction of global and segmental functional changes after acute myocardial infarction: a comparison with late gadolinium enhancement cardiac magnetic resonance. J Am Soc Echocardiogr 27(3):249–257
Seo Y, Ishizu T, Enomoto Y, Sugimori H, Yamamoto M, Machino T et al (2009) Validation of 3-dimensional speckle tracking imaging to quantify regional myocardial deformation. Circ Cardiovasc Imaging 2(6):451–459
Wen H, Liang Z, Zhao Y, Yang K (2011) Feasibility of detecting early left ventricular systolic dysfunction using global area strain: a novel index derived from three-dimensional speckle-tracking echocardiography. Eur J Echocardiogr 12(12):910–916
Reant P, Barbot L, Touche C, Dijos M, Arsac F, Pillois X et al (2012) Evaluation of global left ventricular systolic function using three-dimensional echocardiography speckle-tracking strain parameters. J Am Soc Echocardiogr 25(1):68–79
Lang RM, Badano LP, Tsang W, Adams DH, Agricola E, Buck T et al (2012) EAE/ASE recommendations for image acquisition and display using three-dimensional echocardiography. Eur Heart J Cardiovasc Imaging 13(1):1–46
Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK et al (2002) Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Int J Cardiovasc Imaging 18(1):539–542
Arisha MM, Girerd N, Chauveau S, Bresson D, Scridon A, Bonnefoy E et al (2013) In-hospital heart rate turbulence and microvolt T-wave alternans abnormalities for prediction of early life-threatening ventricular arrhythmia after acute myocardial infarction. Ann Noninvasive Electrocardiol 18(6):530–537
Pérez de Isla L, Millán M, Lennie V, Quezada M, Guinea J, Macaya C et al (2011) Area strain: normal values for a new parameter in healthy people. Rev Esp Cardiol 64(12):1194–1197
Kleijn SA, Aly MFA, Terwee CB, van Rossum AC, Kamp O (2012) Reliability of left ventricular volumes and function measurements using three-dimensional speckle tracking echocardiography. Eur Heart J Cardiovasc Imaging 13(2):159–168
Nesser H-J, Mor-Avi V, Gorissen W, Weinert L, Steringer-Mascherbauer R, Niel J et al (2009) Quantification of left ventricular volumes using three-dimensional echocardiographic speckle tracking: comparison with MRI. Eur Heart J 30(13):1565–1573
Munk K, Andersen NH, Nielsen SS, Bibby BM, Bøtker HE, Nielsen TT et al (2011) Global longitudinal strain by speckle tracking for infarct size estimation. Eur J Echocardiogr 12(2):156–165
Takeuchi M, Nishikage T, Nakai H, Kokumai M, Otani S, Lang RM (2007) The assessment of left ventricular twist in anterior wall myocardial infarction using two-dimensional speckle tracking imaging. J Am Soc Echocardiogr 20(1):36–44
Kansal MM, Panse PM, Abe H, Caracciolo G, Wilansky S, Tajik AJ et al (2011) Relationship of contrast-enhanced magnetic resonance imaging-derived intramural scar distribution and speckle tracking echocardiography-derived left ventricular two-dimensional strains. Eur Heart J Cardiovasc Imaging 13(2):152–158
Cimino S, Canali E, Petronilli V, Cicogna F, De Luca L, Francone M et al (2013) Global and regional longitudinal strain assessed by two-dimensional speckle tracking echocardiography identifies early myocardial dysfunction and transmural extent of myocardial scar in patients with acute ST elevation myocardial infarction and relatively preserved LV function. Eur Heart J Cardiovasc Imaging 14(8):805–811
Li Y-J, Li C, Li C-M, Zhang L, Bai W-J, Zhang X-L et al (2013) Value of three-dimensional speckle-tracking echocardiography and the novel area strain in detecting wall motion abnormalities of coronary artery diseases. Sichuan Da Xue Xue Bao Yi Xue Ban 44(4):651–656
Wu KC, Kim RJ, Bluemke DA, Rochitte CE, Zerhouni EA, Becker LC et al (1998) Quantification and time course of microvascular obstruction by contrast-enhanced echocardiography and magnetic resonance imaging following acute myocardial infarction and reperfusion. J Am Coll Cardiol 32(6):1756–1764
Bergerot C, Mewton N, Lacote-Roiron C, Ernande L, Ovize M, Croisille P et al (2014) Influence of microvascular obstruction on regional myocardial deformation in the acute phase of myocardial infarction: a Speckle-Tracking Echocardiography Study. J Am Soc Echocardiogr 27(1):93–100
Bière L, Donal E, Terrien G, Kervio G, Willoteaux S, Furber A et al (2014) longitudinal strain is a marker of microvascular obstruction and infarct size in patients with acute ST-segment elevation myocardial infarction. PLoS One 9(1):e86959
Greenbaum RA, Ho SY, Gibson DG, Becker AE, Anderson RH (1981) Left ventricular fibre architecture in man. Br Heart J 45(3):248–263
Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M et al (2004) ACC/AHA Guidelines for the management of patients with ST-elevation myocardial infarction—executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction). J Am Coll Cardiol 44(3):671–719
Wu KC (2012) CMR of microvascular obstruction and hemorrhage in myocardial infarction. J Cardiovasc Magn Reson 14:68
Acknowledgments
The REMI study and the STANISLAS COHORT were supported by grants from the French Ministry of Health (Programme Hospitalier de Recherche Clinique Inter-régional 2008 and 2009) and sponsored by the CHU Nancy, F-54000, Nancy, France.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Trial registration: NCT01109225.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Figure
Study flow chart of sample selection for the global and segmental analysis of STEMI and control patients (TIFF 50 kb)
Rights and permissions
About this article
Cite this article
Huttin, O., Zhang, L., Lemarié, J. et al. Global and regional myocardial deformation mechanics of microvascular obstruction in acute myocardial infarction: a three dimensional speckle-tracking imaging study. Int J Cardiovasc Imaging 31, 1337–1346 (2015). https://doi.org/10.1007/s10554-015-0690-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-015-0690-2