Abstract
Purpose
Helicobacter pylori infection is considered to have a positive association with colorectal neoplasms. In this study, we evaluated the association between H. pylori infection and colorectal adenomas, based on the characteristics of these adenomas in Korea, where the prevalence of H. pylori infection is high and the incidence of colorectal cancer continues to increase.
Methods
The study cohort consisted of 4,466 subjects who underwent colonoscopy and esophagogastroduodenoscopy during screening (1,245 colorectal adenomas vs. 3,221 polyp-free controls). We compared the rate of H. pylori infection between patients with adenoma and polyp-free control cases, using multivariable logistic regression analysis.
Results
The overall rate of positive H. pylori infection was higher in adenoma cases than in polyp-free control cases (55.0 vs. 48.5%, p < 0.001). The odds ratio (OR) of positive H. pylori infection in patients with adenoma compared to polyp-free controls was 1.28 (95% CI 1.11–1.47). The positive association of H. pylori infection with colorectal adenomas was more prominent in advanced adenomas (OR 1.84, 95% CI 1.25–2.70) and multiple adenomas (OR 1.72, 95% CI 1.26–2.35). Based on the location of these adenomas, the OR was significant only in patients with colonic adenomas (OR 1.31, 95% CI 1.13–1.52) and not in those with rectal adenoma (OR 0.85, 95% CI 0.58–1.24).
Conclusion
Helicobacter pylori infection is an independent risk factor for colonic adenomas, especially in cases of advanced or multiple adenomas, but not for rectal adenomas.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence of colorectal cancer (CRC) has continued to increase in most of East Asia including Korea, while in Western countries, it shows a plateau or marginal decline after peaking [1, 2]. Recent cancer statistics in Korea indicate that CRC is the third most common cancer and the fourth leading cause of death among all cancers [3]. Since early detection of colorectal adenomas can prevent the development of CRC, identification of high-risk patients for colorectal adenomas and adequate surveillances for them are important. The previous research studies highlight smoking, alcohol intake, factors relating to metabolic syndrome, and other lifestyle-related contributors as risk factors for colorectal adenomas [4,5,6,7]. In addition, some meta-analyses have suggested that Helicobacter pylori infection confers 1.2–1.6 times greater risk of CRC [8,9,10,11]. The risk of colorectal adenomas was also increased in H. pylori-infected subjects in meta-analyses [odds ratio (OR) 1.8–1.9] [8, 12]. Recently, a large-scale Western study based on a national database showed that the association between H. pylori-positive gastritis and colonic neoplasm was strengthened with the increase in size and number of colonic adenomas. This was further corroborated based on the histopathological progression, from hyperplastic polyp to an adenomatous polyp, advanced adenoma, and/or adenocarcinoma [13]. In a Japanese case–control study, H. pylori infection was also a risk factor for colorectal adenomas. Moreover, the research indicated that H. pylori-related chronic gastritis cases were at higher risk of proximal adenomas, and not of distal adenomas [14]. In addition, several Korean studies have found that positive serology for H. pylori is associated with colorectal adenomas. However, they showed different outcomes based on the location of adenomas [15, 16]. In the interim, the seroprevalence of H. pylori infection has been as high as over 50% in Korea, despite the gradually decreasing trend [17]. Thus, it is important to determine whether H. pylori infection is an independent risk factor for colorectal adenomas in Korea, where the prevalence of H. pylori infection is still high and the incidence of CRC continues to increase over time. The aim of this study was to evaluate the association between H. pylori infection and colorectal adenomas in Korea and identify how the severity and the location of the adenomas influence the association.
Materials and methods
Study design and population
Consecutive patients who participated in the voluntary health screening program of the National Cancer Center, Korea, between April 2007 and December 2009 were considered. Participants who underwent colonoscopy during screening were enrolled in the “Colorectal Polyp Registry at the National Cancer Center of Korea.” Among the 16,330 participants enrolled in the Colorectal Polyp Registry, 11,965 participants simultaneously underwent upper endoscopy, as well as rapid urease test and were eligible for our study. Among them, 6,601 subjects were provided informed consent forms including information on a survey for demographic and lifestyle factors. Participants with past medical history of CRC or polyps were excluded from the study (n = 1,422). In addition, participants who were diagnosed with other pathological types of colorectal polyps (i.e., hyperplastic polyp, nonspecific change, serrated polyp) were excluded (n = 713). Finally, around 4,466 participants who met the inclusion/exclusion criteria were included in the analysis (Fig. 1). Participants’ clinicopathological data were obtained from review of medical records. Body mass index (BMI) was calculated as [weight (kg)/height (m2)], which was measured using InBody 3.0 (Biospace, Seoul, Korea), which is a body composition analyzer. This study was approved by the Institutional Review Board (IRB) for the National Cancer Center (NCCNCS-13-751).
Evaluation of colonic neoplasm
All selected subjects were examined using video colonoscopy (Olympus CF-H260 or CF-Q260, Olympus Optical Co., Ltd, Tokyo, Japan) by seven experienced colonoscopists. The participants received either 4 L doses of a polyethylene glycol solution (colyte f powder, Taejoon Pharm, Seoul, Korea) or two 45 mL doses of sodium phosphate (C. B. Fleet Co., Inc., Lynchburg, Virginia) before the examinations. Almost all participants who had colonic polyps were scheduled for the endoscopic polypectomy during the procedure. Biopsy specimens were examined by experienced pathologists who were unaware of patients’ clinical findings. We reviewed histopathological data (tubular adenoma, tubulovillous or villous adenoma, and low-/high-grade dysplasia) of colonic adenomas from the pathology reports, and the information about polyp size (0–9 and 10+ mm), number (1–2 and 3+), and location (colon, rectum, and concurrent colon and rectum) from the endoscopy reports. Adenomatous polyps with villous architecture, of size 10 mm or more, and exhibiting high-grade dysplasia were considered as advanced adenomas [18].
Upper endoscopy and H. pylori evaluation
All subjects underwent upper endoscopy (GIF-Q260, Olympus Optical Co., Ltd, Tokyo, Japan), during which a gastric biopsy specimen was routinely obtained from the greater curvature of the corpus for a rapid urease test (Pronto Dry, Medical Instruments Corporation, Solothurn, Switzerland), in order to identify H. pylori. The presence of gastric lesions was recorded, and biopsy samples were obtained from the lesions for histological evaluation as appropriate.
Statistical analysis
We compared the baseline characteristics among subjects who were confirmed to have colorectal adenomas and polyp-free controls, using Pearson’s Chi-square test for categorical variables. In addition, we compared the status of H. pylori infection between cases diagnosed with adenoma and those in the control group. The differences between the two groups were then investigated according to sex and age distribution. The prevalence of colorectal adenomas was also compared based on the presence of H. pylori using Pearson’s Chi-square test. Next, the association between H. pylori infection and risk of colorectal adenomas was evaluated by logistic regression, using ORs and 95% confidence intervals (CIs). Adjustments were also made for confounding factors that were significant in the Chi-square test, among the baseline characteristics (e.g., sex, age, BMI, marital status, educational background, household income, smoking status, alcohol consumption, and family history of CRC). We then stratified the association between H. pylori infection status and risk of colorectal adenomas by severity (low risk vs. advanced adenoma) and number (1–2 and 3+) of adenomas, as well as anatomical location (colon, rectum, and concurrent colon and rectum). STATA software, version 12.0 (StataCorp, College Station, Texas, USA), was used for all of the analyses. All p values were two-sided, and p values <0.05 were considered significant.
Results
Population and baseline demographic data
Among 4,466 enrolled subjects, 1,245 subjects (27.9%) were confirmed to have colorectal adenomas and 3,221 subjects were classified as polyp-free controls. The baseline demographics of the cases with adenoma and polyp-free controls are shown in Table 1. The group of patients with adenomas was older and showed a higher proportion of males, higher BMI, lower education level, and higher consumption of alcohol and tobacco as compared to the polyp-free controls. A family history of CRC was more common in subjects with adenomas.
Helicobacter pylori infection rate
The overall rate of positive H. pylori infection was higher in adenoma cases than in polyp-free controls (55.0 vs. 48.5%, p < 0.001) (Table 2), which was more prominent in the female subjects (p = 0.001) than in the male subjects (p = 0.06). In the groups of subjects in their 40’s and those are 60 years and older, the higher rates of H. pylori infection in subjects with adenoma compared with the polyp-free control group were more prominent.
Helicobacter pylori infection and risk of colorectal adenoma
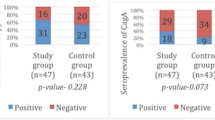
The prevalence of colorectal adenomas, even in advanced cases or multiple adenomas, was increased in H. pylori-positive subjects (30.5 vs. 25.2%) (Table 3). H. pylori infection was associated with an increased risk of adenomas after adjusting for sex, age, BMI, education level, smoking status, alcohol consumption, and family history of CRC (OR 1.28, 95% CI 1.11–1.47) (Table 4). The number of participants having advanced adenomas was 118/1,245 (9.5%), and the OR of positive H. pylori infection was high in subjects with advanced adenomas (OR 1.84, 95% CI 1.25–2.70), whereas the OR was 1.23 in subjects with low-risk adenomas. Likewise, the OR of positive H. pylori infection was higher in subjects who had three or more adenomas (OR 1.72, 95% CI 1.26–2.35) as compared to an OR of 1.22 in subjects who had one or two adenomas (Table 5). Based on the analysis of the location of adenomas, the OR was significant only in subjects with colonic adenomas, not in those with rectal adenomas (OR 1.31 vs. OR 0.85).
Discussion
We confirmed a significant increase in the rate of H. pylori infection in subjects with colorectal adenomas as compared to the rate in the polyp-free control group. This relationship between H. pylori infection and colorectal adenomas was further corroborated in cases of advanced or multiple adenomas. However, the positive relationship was only significant for adenomas of the colon and not for rectal adenomas. We excluded the individuals with non-adenomatous polyps, because the association between H. pylori infection and non-adenomatous colorectal polyps was not much evaluated, and then, it is uncertain whether its association is comparable to that of H. pylori infection with polyp-free controls. A previous study showed that hyperplastic polyps were also associated with H. pylori-positive gastritis with weaker strength than adenomatous polyps (OR 1.24 vs. OR 1.52) [13]. For reference, the rate of H. pylori infection in the individuals with non-adenomatous polyps was 49.9% (356/713) in our study, which was close to those of the polyp-free control group. In the multivariate analysis, the OR of positive H. pylori infection in patients with non-adenomatous polyps compared to the polyp-free controls was 0.97 (95% CI 0.81–1.16). The analysis including these individuals with non-adenomatous polyps as controls (n = 3,934) showed that the OR of positive H. pylori infection in patients with adenomas compared to controls was 1.29 (95% CI 1.11–1.50). More studies about a role of H. pylori in the non-adenomatous colorectal polyps are warranted in the future.
Several studies have similar outcomes regarding H. pylori as a risk factor for overall colorectal adenomas; however, they indicated conflicting results for the location of these adenomas [15, 16, 19]. One study reported that H. pylori infection increased the risk of colorectal adenomas, with a predilection for the proximal colon [16], while another study stated that the distal colon was at the greater risk [15]. The latter study was supported by several previous studies suggesting that the effect of gastrin on colorectal neoplasm was limited to the distal colon [11, 20, 21]. These are not consistent with our results that showed greater association of H. pylori with colonic adenomas rather than with rectal adenomas. Stewart et al. [22] suggested that there is a different impact of H. pylori on the colorectal area resulting from contrasting immune functions of the colon and the rectum. In line with this observation, several researchers have suggested that the rectum has a different anatomical origin and vascular drainage compared to the colon; then, there are clinical, biological, and epidemiological distinctions between colon and rectal cancers, which could be attributed to the differences in their respective immune mechanisms [23, 24]. Furthermore, the differences in the immune mechanisms might be responsible for increased risk of colonic adenomas associated with H. pylori infection, but not in case of rectal adenomas.
We routinely used the rapid urease test for all subjects, which is different from recent Korean studies that used serological tests. [15, 16] Thus, our study explains the association between existing H. pylori infection status and colorectal adenomas more accurately; however, it is not sufficient to identify the duration of infection. Meanwhile, there have been only a few studies that used the rapid urease test for H. pylori evaluation. Moreover, they rarely adjusted for possible confounding factors. Two studies have failed to prove the association between H. pylori and colorectal adenomas [25, 26]. However, a multivariable analysis using direct H. pylori test showed that current H. pylori infection increased the risk of colorectal adenoma (OR 1.37) [27]. Our study not only had figures similar to theirs, but also confirmed the plausible relationship between current H. pylori infection and colorectal adenomas by evaluating advanced or multiple adenomas. Another recent study that involved histopathological evaluation of gastric biopsy specimens also found positive correlation between H. pylori-related gastritis and colonic adenomas [13]. In particular, it was more significant in cases of advanced adenomas (OR 1.80), which is consistent with (OR 1.84) our study. These recent studies using direct H. pylori test strongly imply that current H. pylori infection is an independent risk factor for colonic adenomas. Most of the previous studies using serology for H. pylori have shown inconsistent and inconclusive results [12], and it is possible that different direct or indirect modalities for testing for H. pylori infection may affect the study outcomes.
With reference to a causal relationship between H. pylori infection and colorectal neoplasm, several mechanisms have been suggested. One of the most reliable mechanisms is that H. pylori-induced hypergastrinemia stimulates colonic carcinogenesis by cell proliferation, and some studies have supported this claim [20, 28]. However, other studies failed to determine the relationship between hypergastrinemia and colorectal neoplasms [29, 30]. Similarly, a limited number of studies have found a direct effect of H. pylori colonization on the colonic mucosa [31, 32]. Another suggestion is that specific H. pylori toxin-induced inflammatory response may be responsible for activating colonic carcinogenesis [33]. It was postulated that H. pylori cagA seropositivity was especially associated with increased risk of colonic neoplasm in some studies [34, 35], whereas there was no significant association between cagA seropositivity and CRC, in other studies [36, 37]. In addition, H. pylori-related chronic atrophic gastritis (CAG) increased the risk of colorectal neoplasm, that is, CAG-induced hypochlorhydria might contribute to colorectal carcinogenesis [38]. Further studies with regard to pathogenic mechanisms should be continued that can help reveal critical points about H. pylori infection and its involvement in the development of colorectal adenomas.
Alcohol consumption, smoking, obesity, and family history of colorectal neoplasms are well-known risk factors for colorectal neoplasm [4, 5, 39,40,41,42]. These risk factors may possibly act as significant confounders in the analysis of the role played by H. pylori infection in developing colorectal neoplasms. These risk factors need to be considered and statistically evaluated. The present study, which was conducted on a relatively large-scale, evaluated the variable confounding factors, thereby supporting previous studies, indicating H. pylori infection as an independent risk factor for colorectal adenomas.
In this study, the overall prevalence of colorectal adenoma was 27.9%. The prevalence of adenoma was 36.4 and 17.9% in males and females, respectively, which was comparable with data from other Korean studies during the same period [19, 42]. In the meantime, it has been known that estrogen along with progestin reduced the risk of CRC [43]. Another study stated that metabolic syndrome posed as a risk factor for CRC, indicating conflicting results based on gender differences and tumor location, which implied that the proximal colon might be influenced to a greater extent by sex hormones [44]. We found that H. pylori infection is significantly associated with colorectal adenomas in female patients (p = 0.001), which supports observations in several previous studies that showed a strong association of H. pylori infection with colorectal adenomas in females [45, 46]. However, the effect of H. pylori infection on the relationship between colorectal neoplasm and sex hormone has been rarely studied, which warrants further investigation.
There were several limitations in this study. Firstly, the enrolled subjects voluntarily participated in colonoscopic examinations, and the overall rate of H. pylori infection was somewhat lower than 56–59% as stipulated by previous Korean studies during comparable years [47, 48]. It is likely that our subjects may have had higher health concerns, better lifestyles, or economic statuses as compared with the general population. Secondly, since the information relating to the previous history of CRC or polyps mainly relied on self-reported questionnaires, this may be vulnerable to recall bias and can affect the association that we found. However, colorectal neoplasms were objectively categorized by highly experienced colonoscopists, who were blinded to the results of the rapid urease test and patients’ clinical information, in order to minimize errors from the information. Thirdly, we cannot exclude a possibility of reversal causality caused from the cross-sectional nature of the study, which makes it difficult to estimate the chronology of colorectal histological changes with the age and the period of H. pylori affected. Fourthly, we did not investigate H. pylori-specific Ab including CagA and VacA. Hence, there is no knowledge of heterogeneity of the H. pylori exposure that might affect the development of colorectal adenomatous polyp. Fifthly, the individuals who did not undergo a simultaneous upper endoscopy and excluded from the study may differ from study participants who did upper endoscopy. However, a simultaneous upper endoscopy was also performed for screening purpose, not for the clinical indications. Meanwhile, biennial gastric cancer screening via either an upper endoscopy or an upper gastrointestinal series has been conducted in Korea nationwide since 1999 [49]. Thus, some participants, who had undergone upper endoscopy by the national screening just before our study enrollment, did not want to undergo a simultaneous upper endoscopy. Sixthly, only 55% of the participants with both colonoscopy and upper endoscopy provided informed consent, which may lead the selection bias and affect generalizability of the study. Finally, some lifestyle factors that were missed in the present study cannot be ignored. Factors such as physical activity, use of NSAIDs or aspirin, and routine dietary habits may also have positive or negative association with the prevalence of colorectal adenomas [6, 7]. Thus, our findings need to be substantiated by considering these lifestyle factors and eliminating possible confounders in future studies.
This study has the following implications. Firstly, this is a large-scale study conducted in an area that has a high prevalence of H. pylori infection. We especially considered other demographic or clinical confounding factors that can influence the development of colorectal adenomas. Secondly, we obtained detailed information for the respective endoscopies based on the size, number, and location of the colorectal adenomas. Therefore, statistically, our results support previous studies, in that H. pylori infection increases the risk of colonic adenomas. Thirdly, the sensitivity and specificity of the rapid urease test performed at the greater curvature of the colonic corpus to detect the presence of H. pylori were as high as 96 and 100%, respectively, in our institute [50]. In addition, it has the advantage of minimizing selection bias, since we routinely performed the rapid urease test in all subjects who underwent screening with upper endoscopy. Finally, many of subjects who are screened at our center usually undergo upper endoscopy and colonoscopy at a few years’ intervals, and the patients who have been endoscopically diagnosed with gastric or duodenal ulcers (scar) are eligible for H. pylori treatment in Korea. Therefore, further evaluation of the effects of H. pylori treatment or persistent infection on the development or recurrence of colorectal adenomas seems possible.
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D (2011) Global cancer statistics. CA Cancer J Clin 61:69–90
Center MM, Jemal A, Ward E (2009) International trends in colorectal cancer incidence rates. Cancer Epidemiol Biomarkers Prev 18:1688–1694
Jung KW, Won YJ, Kong HJ, Oh CM, Lee DH, Lee JS (2014) Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2011. Cancer Res Treat 46:109–123
Shin A, Hong CW, Sohn DK, Kim BC, Han KS, Chang HJ, Kim J, Oh JH (2011) Associations of cigarette smoking and alcohol consumption with advanced or multiple colorectal adenoma risks: a colonoscopy-based case–control study in Korea. Am J Epidemiol 174:552–562
Kim BC, Shin A, Hong CW, Sohn DK, Han KS, Ryu KH, Park BJ, Nam JH, Park JW, Chang HJ, Choi HS, Kim J, Oh JH (2012) Association of colorectal adenoma with components of metabolic syndrome. Cancer Causes Control 23:727–735
Fu Z, Shrubsole MJ, Smalley WE, Wu H, Chen Z, Shyr Y, Ness RM, Zheng W (2012) Lifestyle factors and their combined impact on the risk of colorectal polyps. Am J Epidemiol 176:766–776
Sanchez NF, Stierman B, Saab S, Mahajan D, Yeung H, Francois F (2012) Physical activity reduces risk for colon polyps in a multiethnic colorectal cancer screening population. BMC Res Notes 5:312
Wang F, Sun MY, Shi SL, Lv ZS (2014) Helicobacter pylori infection and normal colorectal mucosa-adenomatous polyp-adenocarcinoma sequence: a meta-analysis of 27 case–control studies. Colorectal Dis 16:246–252
Zhao YS, Wang F, Chang D, Han B, You DY (2008) Meta-analysis of different test indicators: Helicobacter pylori infection and the risk of colorectal cancer. Int J Colorectal Dis 23:875–882
Zumkeller N, Brenner H, Zwahlen M, Rothenbacher D (2006) Helicobacter pylori infection and colorectal cancer risk: a meta-analysis. Helicobacter 11:75–80
Zhang Y, Hoffmeister M, Weck MN, Chang-Claude J, Brenner H (2012) Helicobacter pylori infection and colorectal cancer risk: evidence from a large population-based case–control study in Germany. Am J Epidemiol 175:441–450
Guo Y, Li HY (2014) Association between Helicobacter pylori infection and colorectal neoplasm risk: a meta-analysis based on East Asian population. J Cancer Res Ther 10(Suppl):263–266
Sonnenberg A, Genta RM (2013) Helicobacter pylori is a risk factor for colonic neoplasms. Am J Gastroenterol 108:208–215
Inoue I, Mukoubayashi C, Yoshimura N, Niwa T, Deguchi H, Watanabe M, Enomoto S, Maekita T, Ueda K, Iguchi M, Yanaoka K, Tamai H, Arii K, Oka M, Fujishiro M, Takeshita T, Iwane M, Mohara O, Ichinose M (2011) Elevated risk of colorectal adenoma with Helicobacter pylori-related chronic gastritis: a population-based case–control study. Int J Cancer 129:2704–2711
Nam KW, Baeg MK, Kwon JH, Cho SH, Na SJ, Choi MG (2013) Helicobacter pylori seropositivity is positively associated with colorectal neoplasms. Korean J Gastroenterol 61:259–264
Hong SN, Lee SM, Kim JH, Lee TY, Kim JH, Choe WH, Lee SY, Cheon YK, Sung IK, Park HS, Shim CS (2012) Helicobacter pylori infection increases the risk of colorectal adenomas: cross-sectional study and meta-analysis. Dig Dis Sci 57:2184–2194
Lim SH, Kwon JW, Kim N, Kim GH, Kang JM, Park MJ, Yim JY, Kim HU, Baik GH, Seo GS, Shin JE, Joo YE, Kim JS, Jung HC (2013) Prevalence and risk factors of Helicobacter pylori infection in Korea: nationwide multicenter study over 13 years. BMC Gastroenterol 13:104
Winawer SJ, Zauber AG (2002) The advanced adenoma as the primary target of screening. Gastrointest Endosc Clin N Am 12:1–9
Kim HS, Baik SJ, Kim KH, Oh CR, Lee SI (2013) Prevalence and risk factors of colorectal adenoma in 14,932 Koreans undergoing screening colonoscopy. Korean J Gastroenterol 62:104–110
Georgopoulos SD, Polymeros D, Triantafyllou K, Spiliadi C, Mentis A, Karamanolis DG, Ladas SD (2006) Hypergastrinemia is associated with increased risk of distal colon adenomas. Digestion 74:42–46
Houli N, Loh SW, Giraud AS, Baldwin GS, Shulkes A (2006) Mitogenic effects of both amidated and glycine-extended gastrin-releasing peptide in defunctioned and azoxymethane-treated rat colon in vivo. Regul Pept 134:9–16
Stewart T, Henderson R, Grayson H, Opelz G (1997) Reduced incidence of rectal cancer, compared to gastric and colonic cancer, in a population of 73,076 men and women chronically immunosuppressed. Clin Cancer Res 3:51–55
Perez-Ruiz E, Berraondo P (2016) Immunological landscape and clinical management of rectal cancer. Front Immunol 7:61
Tamas K, Walenkamp AM, de Vries EG, van Vugt MA, Beets-Tan RG, van Etten B, de Groot DJ, Hospers GA (2015) Rectal and colon cancer: not just a different anatomic site. Cancer Treat Rev 41:671–679
Abbass K, Gul W, Beck G, Markert R, Akram S (2011) Association of Helicobacter pylori infection with the development of colorectal polyps and colorectal carcinoma. South Med J 104:473–476
Bae RC, Jeon SW, Cho HJ, Jung MK, Kweon YO, Kim SK (2009) Gastric dysplasia may be an independent risk factor of an advanced colorectal neoplasm. World J Gastroenterol 15:5722–5726
Lin YL, Chiang JK, Lin SM, Tseng CE (2010) Helicobacter pylori infection concomitant with metabolic syndrome further increase risk of colorectal adenomas. World J Gastroenterol 16:3841–3846
Thorburn CM, Friedman GD, Dickinson CJ, Vogelman JH, Orentreich N, Parsonnet J (1998) Gastrin and colorectal cancer: a prospective study. Gastroenterology 115:275–280
Robertson DJ, Sandler RS, Ahnen DJ, Greenberg ER, Mott LA, Cole BF, Baron JA (2009) Gastrin, Helicobacter pylori, and colorectal adenomas. Clin Gastroenterol Hepatol 7:163–167
Selgrad M, Bornschein J, Kandulski A, Hille C, Weigt J, Roessner A, Wex T, Malfertheiner P (2014) Helicobacter pylori but not gastrin is associated with the development of colonic neoplasms. Int J Cancer 135:1127–1131
Jones M, Helliwell P, Pritchard C, Tharakan J, Mathew J (2007) Helicobacter pylori in colorectal neoplasms: is there an aetiological relationship? World J Surg Oncol 5:51
Soylu A, Ozkara S, Alis H, Dolay K, Kalayci M, Yasar N, Kumbasar AB (2008) Immunohistochemical testing for Helicobacter pylori existence in neoplasms of the colon. BMC Gastroenterol 8:35
Epplein M, Pawlita M, Michel A, Peek RM Jr, Cai Q, Blot WJ (2013) Helicobacter pylori protein-specific antibodies and risk of colorectal cancer. Cancer Epidemiol Biomarkers Prev 22:1964–1974
Shmuely H, Passaro D, Figer A, Niv Y, Pitlik S, Samra Z, Koren R, Yahav J (2001) Relationship between Helicobacter pylori CagA status and colorectal cancer. Am J Gastroenterol 96:3406–3410
Hartwich A, Konturek SJ, Pierzchalski P, Zuchowicz M, Labza H, Konturek PC, Karczewska E, Bielanski W, Marlicz K, Starzynska T, Lawniczak M, Hahn EG (2001) Helicobacter pylori infection, gastrin, cyclooxygenase-2, and apoptosis in colorectal cancer. Int J Colorectal Dis 16:202–210
Chen XZ, Schottker B, Castro FA, Chen H, Zhang Y, Holleczek B, Brenner H (2016) Association of Helicobacter pylori infection and chronic atrophic gastritis with risk of colonic, pancreatic and gastric cancer: a ten-year follow-up of the ESTHER cohort study. Oncotarget 7:17182–17193
Strofilas A, Lagoudianakis EE, Seretis C, Pappas A, Koronakis N, Keramidaris D, Koukoutsis I, Chrysikos I, Manouras I, Manouras A (2012) Association of Helicobacter pylori infection and colon cancer. J Clin Med Res 4:172–176
Inoue I, Kato J, Tamai H, Iguchi M, Maekita T, Yoshimura N, Ichinose M (2014) Helicobacter pylori-related chronic gastritis as a risk factor for colonic neoplasms. World J Gastroenterol 20:1485–1492
Rueda M, Robertson Y, Acott A, Rueda S, Keikhoff A, Guerrero W, Mancino AT (2012) Association of tobacco and alcohol use with earlier development of colorectal pathology: should screening guidelines be modified to include these risk factors? Am J Surg 204:963–967
Laiyemo AO, Doubeni C, Badurdeen DS, Murphy G, Marcus PM, Schoen RE, Lanza E, Smoot DT, Cross AJ (2012) Obesity, weight change, and risk of adenoma recurrence: a prospective trial. Endoscopy 44:813–818
Fuchs CS, Giovannucci EL, Colditz GA, Hunter DJ, Speizer FE, Willett WC (1994) A prospective study of family history and the risk of colorectal cancer. N Engl J Med 331:1669–1674
Yang MH, Rampal S, Sung J, Choi YH, Son HJ, Lee JH, Kim YH, Chang DK, Rhee PL, Rhee JC, Guallar E, Cho J (2014) The prevalence of colorectal adenomas in asymptomatic Korean men and women. Cancer Epidemiol Biomarkers Prev 23:499–507
Chlebowski RT, Wactawski-Wende J, Ritenbaugh C, Hubbell FA, Ascensao J, Rodabough RJ, Rosenberg CA, Taylor VM, Harris R, Chen C, Adams-Campbell LL, White E, Women’s Health Initiative I (2004) Estrogen plus progestin and colorectal cancer in postmenopausal women. N Engl J Med 350:991–1004
Lu Y, Ness-Jensen E, Hveem K, Martling A (2015) Metabolic predispositions and increased risk of colorectal adenocarcinoma by anatomical location: a large population-based cohort study in Norway. Am J Epidemiol 182:883–893
Fujimori S, Kishida T, Kobayashi T, Sekita Y, Seo T, Nagata K, Tatsuguchi A, Gudis K, Yokoi K, Tanaka N, Yamashita K, Tajiri T, Ohaki Y, Sakamoto C (2005) Helicobacter pylori infection increases the risk of colorectal adenoma and adenocarcinoma, especially in women. J Gastroenterol 40:887–893
Wu Q, Yang ZP, Xu P, Gao LC, Fan DM (2013) Association between Helicobacter pylori infection and the risk of colorectal neoplasia: a systematic review and meta-analysis. Colorectal Dis 15:e352–e364
Yim JY, Kim N, Choi SH, Kim YS, Cho KR, Kim SS, Seo GS, Kim HU, Baik GH, Sin CS, Cho SH, Oh BH (2007) Seroprevalence of Helicobacter pylori in South Korea. Helicobacter 12:333–340
Nam JH, Choi IJ, Kook MC, Lee JY, Cho SJ, Nam SY, Kim CG (2014) OLGA and OLGIM stage distribution according to age and Helicobacter pylori status in the Korean population. Helicobacter 19:81–89
Hahm MI, Choi KS, Park EC, Kwak MS, Lee HY, Hwang SS (2008) Personal background and cognitive factors as predictors of the intention to be screened for stomach cancer. Cancer Epidemiol Biomarkers Prev 17:2473–2479
Kim CG, Choi IJ, Lee JY, Cho SJ, Nam BH, Kook MC, Hong EK, Kim YW (2009) Biopsy site for detecting Helicobacter pylori infection in patients with gastric cancer. J Gastroenterol Hepatol 24:469–474
Acknowledgments
This study was supported in part by Grants NCC-1410250-3, NCC-1610250, and NCC-0910221 from National Cancer Center, Korea. The authors thank Jeong-Hee Lee, MS for their help in manuscript preparation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nam, J.H., Hong, C.W., Kim, B.C. et al. Helicobacter pylori infection is an independent risk factor for colonic adenomatous neoplasms. Cancer Causes Control 28, 107–115 (2017). https://doi.org/10.1007/s10552-016-0839-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-016-0839-x