Abstract
Purpose
To evaluate changes in cancer mortality burden over time by assessing temporal trends in life expectation for Australian residents diagnosed with cancer.
Methods
The study cohort consisted of all people diagnosed with cancer in the period 1990–2000 and aged 15–89 years (n = 1,275,978), with mortality follow-up to 31 December 2010. Flexible parametric survival models incorporating background age–sex–year-specific population mortality rates were applied to generate the observed survival curves for all cancers combined and selected major cancer types. Predicted values of loss of life expectancy (LOLE) in years were generated and then averaged across calendar year and age group (15–49, 50–69 and 70–89 years) or spread of disease (localized, regional, distant, unknown).
Results
The greatest LOLE burden was for lung cancer (14.3 years per diagnosis) and lowest for melanoma (2.5 years). There was a significant decrease in LOLE over time (−0.13 LOLE per year) for all cancers combined. Decreases were also observed for female breast cancer (−0.21), prostate cancer (−0.17), colorectal cancer (−0.08), melanoma (−0.07) and stomach cancer (−0.02), with slight increases for lung cancer (+0.04). When restricted to the sub-cohort from New South Wales with spread of disease information, these decreases in LOLE were primarily among cancers categorized as localized or regional spread at diagnosis.
Conclusions
In Australia, persons diagnosed with cancer have a steadily improving outlook that exceeds that expected by general improvement in population life expectancy. The overall improvement is observed in persons with localized or regional cancers but not in those with advanced cancers, findings which encourage earlier diagnosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Assessing the changing impact of disease through cause-specific mortality trends has an enduring history in health research. However, population trends in mortality rates alone do not quantify the disproportionate impact of deaths in younger age groups on population life expectancy, nor how those impacts may be changing over time. Recent studies in diverse countries have sought to better quantify the changing mortality burden through examination of (person) years of life lost (PYLL or YLL) [1–4].
While offering advantages over standard mortality rates, an important limitation of the YLL measure is that it requires accurate cause of death information. In addition, since it is calculated using mortality information only, the YLL measure does not consider when cancer patients were diagnosed with the disease. Therefore, the experience of a specific period-defined cohort diagnosed with the disease is not captured.
Recently, we have published population-based estimates of a newer measure, the loss of life expectancy (LOLE) [5, 6], which addresses the question “On average, how much does my life expectancy change now that I have been diagnosed with cancer?” LOLE (measured in years) was calculated using flexible parametric models [5, 7] to estimate and extrapolate a cohort’s observed and expected survival, and represents the difference between the expectation of life in the general population and the expectation of life among cancer patients. By the use of a relative survival approach, the LOLE is not dependent on accurate cause of death information and additionally provides estimates of the loss in expectation of life for an entire cohort diagnosed with a specific cancer compared to the general population, irrespective of whether they died from that cancer. Although the specific methods differ, there are similarities between this approach and that developed by Hwang and Wang [8, 9] and applied recently [10], in that they both take background mortality information into account for extrapolation of survival beyond the end of follow-up.
In a country where population life expectancies are increasing [11], it remains unclear whether those diagnosed with cancer are experiencing similar improvements in outcomes. By using data from population-based registries in Australia, we evaluated temporal trends in life expectations for people diagnosed with cancer to assess how the mortality burden caused by cancer in Australia has changed over time.
Methods
Cancer cohort
State and Territory Cancer Registries provided approval to access and use de-identified data through the Australian Institute of Health and Welfare (AIHW) [12]. The exception was the Australian Capital Territory, comprising around one percent of all cancers diagnosed in Australia [13]. Notification of all invasive cancers (excluding keratinocyte cancers) is required by law.
Since the methods used in this study have been demonstrated to have robust predictive ability when there is at least 10 years of potential follow-up [5], we restricted the study cohort to consist of all cancer patients diagnosed from 1990 through to 2000, enabling us to have at least 10 years of follow-up on mortality status to 31 December 2010, which was the latest available data at the time of the data extraction. Mortality status was obtained using routine annual linkage of cancer records with the National Death Index in Australia. We restricted the cancer cohort to patients diagnosed when aged between 15 and 89 years old due to the different cancer classifications used for pediatric cancer [14] and for consistency with our recent survival studies [6, 15]. Cases diagnosed on the basis of autopsy or death certificate only, or when the recorded date of diagnosis was after the date of death, were excluded from the cohort.
The analyses are presented for all invasive cancers combined (ICD-O-3 codes C00-C80), in addition to the individual types of cancers listed in Table 1. Disease stage at diagnosis is not routinely collected by most population-based cancer registries. However, New South Wales (NSW), the most populous state in Australia comprising 35 % of the overall study cohort, does collect a measure of disease stage. We therefore used the NSW cohort to investigate the impact of spread of disease at diagnosis on the temporal changes in LOLE.
Relative survival
For members of the study cohort who died before 31 December 2010, survival time was calculated as the time between diagnosis and death. For patients who were not known to have died before this date, the follow-up time was censored at the censoring date (31 December, 2010). Since the purpose of this study was to assess trends in LOLE over time of diagnosis, we used the cohort method to calculate relative survival.
Flexible parametric relative survival models [16, 17] incorporating background age–sex–year-specific population mortality rates were applied to generate the observed survival curves. These models use restricted cubic splines for the baseline and so can more readily capture the shape of the underlying excess hazard function compared to more traditional methods such as the Cox proportional hazards model [5]. The expected survival curves were obtained using the age–sex–year-specific population mortality rates.
For each cancer group, we included year of diagnosis, age at diagnosis and sex in the model. The variables age and year of diagnosis were included as continuous variables using restricted cubic splines (four and three degrees of freedom, respectively), and where model convergence requirements enabled it, variables were allowed to have a time-dependent effect.
While extrapolating the observed survival curves beyond the available follow-up is difficult, Andersson et al. [5, 6] demonstrated that it was possible to extrapolate the relative survival curve through modeling of the excess mortality component. We assumed a linear trend in the log cumulative excess hazard when extrapolating observed survival for the individual cancer sites; however, examination of the observed and predicted relative survival curves suggested that the statistical cure model fitted best for all cancers combined. For completeness, we have shown the impact of the different assumptions on the final LOLE values (Supplementary Table 1). Predicted values of LOLE were generated by averaging the differences in the areas under the projected survival curve across calendar year and broad age group (15–49, 50–69 and 70–89 years) for the cancer patients and the general population. For the NSW cohort only, it was also possible to investigate the impact of spread of disease, classified as localized, regional, distant or unknown.
We conducted sensitivity analysis by varying the maximum length of follow-up time for each cancer patient and then looking at the impact on the temporal trends between 1990 and 2000. This meant that we ran three iterations of the model: censoring records at 5 years after diagnosis, censoring records at 10 years after diagnosis, and censoring records at the maximum follow-up (i.e., 31 December 2010).
The direction, magnitude and significance of linear trends in the LOLE estimates over time were quantified using linear regression models, in which the outcome variable was the age- and year-specific LOLE estimate, and year and age group at diagnosis were explanatory variables. Due to the very large cohort size, we used p < 0.001 to indicate statistical significance for these trend coefficients. All statistical analyses were performed using Stata/SE version 12.1 for Windows (StataCorp, TX, USA). Flexible parametric survival models were fitted using the stpm2 package [16, 17].
Results
Australian cohort
A total of 814,806 Australian residents were diagnosed with cancer between 1990 and 2000 when aged between 15 and 89 years. Of these, 263 (0.03 %) were excluded due to missing or negative follow-up times and 7,668 (0.9 %) were excluded due to the diagnosis being based on death certificate only. The remaining 806,875 patients formed the study cohort (Table 1). The median age at diagnosis was 67–71 years for most of the specified types of cancer but was about 10 years younger for melanoma and female breast cancer. The median time of observed follow-up among the cohort for all cancers combined was 5.3 years (range 0–21 years) and varied across the different cancer types from 0.6 years for lung cancer to 12.5 years for melanoma. Over two-thirds (68 %) of all patients died from any cause before the end of 2010, ranging from 37 % for melanomas to 96 % for lung cancer.
Across the whole study period, the average estimated cohort life expectancy from the time of diagnosis (Table 1) was 12.4 years for all cancers combined and ranged from 24.5 years for those diagnosed with melanoma to 2.4 years for lung cancer. This, however, was influenced by the differing age and sex distributions of the cancers, resulting in slight variation in age–sex-matched population life expectancy for each cancer type (Supplementary Figure 1). When subtracting the cohort life expectancy from the population life expectancy, the average LOLE for all cancers combined was 8.2 years, ranging from 2.5 years for melanoma to 14.3 years for lung cancer (Table 1).
Spread of disease at diagnosis—NSW cohort
In NSW, 280,901 residents were diagnosed with cancer between 1990 and 2000, of whom 38 % were diagnosed with localized cancer, 19 % were diagnosed with regional cancer, and 14 % were diagnosed with distant cancer. The proportion with distant disease ranged from 4 % for melanoma to 31 % for lung cancer. About one quarter (29 %) of cancers in the NSW cohort had no information about spread of disease at diagnosis; this percentage ranged from 4 % for melanoma to 47 % for prostate cancer.
When combined across the spread of disease categories and years, the average LOLE for the various cancer types in NSW was similar to the corresponding Australian averages (Tables 1, 2). For all types of cancer examined, the average LOLE was lowest among people diagnosed with localized cancer, intermediate for those with regional cancer and highest for people diagnosed with advanced cancer (Table 2).
Changes over time
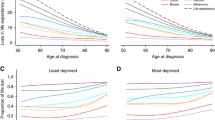
There was a general decrease in LOLE estimates over time in Australia (Fig. 1; Table 3). Among 15- to 89-year-olds combined, the average LOLE for all cancers decreased from 9.4 years for people diagnosed in 1990 to 7.7 years for people diagnosed in 2000, reflecting a significant average annual decrease of −0.13 LOLE per calendar year (Table 3). Decreases over time were also observed in LOLE for female breast cancer (from 8.6 in 1990 to 5.1 in 2000, −0.28 LOLE/year), prostate cancer (4.5 to 2.5, −0.15 LOLE/year), colorectal cancer (7.9 to 6.6, −0.08 LOLE/year), melanoma (3.0 to 2.3, −0.07 LOLE/year), while the LOLE trends for stomach cancer were stable (12.1 to 11.8, −0.00 LOLE/year). In contrast, while the 2000 LOLE point estimate was lower than the 1990 point estimate for lung cancer, over the time interval there was a small, but significant linear increase in LOLE estimates (14.5 to 14.2, +0.07 LOLE/year).
For most specified cancers, the LOLE declined significantly over time in each age group. The magnitude of change in LOLE over time was higher among those diagnosed aged between 15 and 49 years compared to those diagnosed at older ages (Table 3). Exceptions to these patterns were the significant increases in LOLE over time for patients diagnosed with lung cancer while aged 50–69 and 70–89 years of age, and the stable LOLE over time for stomach cancer patients in the two older age groups (Table 3).
When restricting the analysis to the NSW cohort, there were generally similar trends to those reported from the national cohort, with the exception of a non-significant decrease in colorectal cancer, whereas this decrease was significant in the national cohort. Analysis stratified by spread of disease showed that for cases categorized as local or regional, decreases in LOLE over time were observed across all cancer types studied, with the exception of regional lung cancer, which showed significant increases in LOLE over time (Table 4; Fig. 2). However, where spread of disease was categorized as distant, LOLE remained stable over time for stomach cancer and all cancers combined and significantly increased for both colorectal cancer and lung cancer (Table 4; Fig. 2).
Results from the sensitivity analyses are shown in Supplementary Figures 1 (Australia) and 2 (New South Wales). Using only 5 years of follow-up tended to inflate the LOLE estimates, whereas there was little quantitative difference between 10 years and “maximum” follow-up (up to 20 years).
Discussion
In a population in which overall life expectancy is increasing [11], we found that, on average, Australians diagnosed with cancer in 2000 were projected to experience lower loss of life expectancy due to their cancer than those diagnosed in the early 1990s. This is an encouraging result as it indicates that not only have cancer patients experienced an increase in life expectancy over time, but that this increase has occurred at a greater rate than that for the general population. While the annual improvement in overall survival following cancer diagnosis, −0.13 LOLE per year, may appear modest, it translates to more than 1 year of added life expectancy between 1990 and 2000, in addition to the increases in general population life expectancy over that time.
While the precise reasons for these results are likely to be numerous and beyond of the scope of this study, some possible explanations are worth considering. Of note for the results for all cancers combined is that the mix of cancers has changed over time. In particular, the proportion of cancers that were lung and stomach cancer (with poor survival) decreased over the study period, while the proportion of prostate cancers (higher survival) increased.
Advances in cancer management over time are one potential explanation for the observed trends in specific cancer types. Increasing use of neoadjuvant therapies, endocrine therapies, and the introduction of second- and third-generation chemotherapy agents have resulted in improvements in survival for women diagnosed with breast cancer [18]. The increase in treatment of surgical colorectal cancer cases with adjuvant therapies has been suggested as a contributor to the survival increases in South Australia [19] and to the reported differences in colorectal cancer survival between the USA and Europe [20]. Similarly, for stomach cancer, reductions in perioperative morbidity and the use of extended lymphadenectomy in early-stage tumors, along with continued improvements in chemotherapeutic regimens for stage III tumors, have been thought to have contributed to improvements in survival [21]. However, the diverging trends in LOLE for colorectal cancer in Australia compared to the NSW cohort, and the lack of any systemic difference in colorectal cancer management in NSW suggests that cancer management alone does not provide the sole reason for the observed trends.
As in all survival-based studies, the interpretation of trends over time may be impacted by the effects of screening and earlier diagnosis. Lead-time bias refers to the length of time between the detection of a disease (typically through screening) and when diagnosis would have been made without screening. When the diagnosis is made earlier, this will increase the observed survival and thus increase the estimate of observed life expectancy. The expected survival will also increase to some extent, because the matched cohort will be younger and the calendar year earlier. However, it is only if these increases are of similar magnitude that the LOLE will be unaffected, and unpublished simulation studies (Andersson, personal communication) have shown that lead-time bias can spuriously decrease estimates of LOLE. While we adjusted for spread of disease, the categories are broad and it is likely that there is a survival gradient within, as well as between, categories. If there has been a similar shift over time within the spread of disease categories, then this may explain at least part of the observed temporal decrease in LOLE.
The temporal trends in LOLE reported here may also have been influenced by changes in risk factors, if the impact of risk factors was to change the disease progression after the cancer is diagnosed, as has been previously observed in associations with cancer survival [22]. However, the evidence for the role of most risk factors (such as obesity [23–26]) and cancer prognosis is mixed and depends on the cancer type.
The lack of any favorable trend in LOLE for people diagnosed with lung cancer, particularly among those aged 50 years and over when diagnosed, reflects the poor survival outcomes for this cancer. While there have been slight improvements in lung cancer survival in Australia and among other more socioeconomically developed countries during recent decades [27], further efforts are hampered by the lack of effective screening tests for the whole population and curative treatments beyond surgical resection for localized tumors [28].
The results for melanoma highlight the importance of LOLE when communicating the full implications of a cancer diagnosis to patients. Melanoma is often categorized as a high survival cancer, particularly when most tumors are diagnosed when thin and therefore treated with curative intent using excision. However, our findings that even people diagnosed with localized melanoma can expect, on average, to have some loss of life expectancy are consistent with the reported survival gradient by thickness even among thin (≤1.0 mm) melanomas [29]. Further, more people in Queensland, Australia, have been reported to die following diagnosis of a thin melanoma than the number who die from thick (>4 mm) melanomas, due to the much larger number of melanomas that are diagnosed with localized spread of disease [30].
Our results also demonstrate the very high burden that cancer has on the community. We estimate that the over 800,000 Australians diagnosed with cancer between 1990 and 2000 will lose over six and a half million years of life expectancy. It also highlights the importance of detecting cancer early. Not only were the greatest LOLE estimates among those people whose cancer was diagnosed at a distant spread of disease, but for several cancers there was either no evidence of an improvement or even a significant increase in LOLE over time among patients with more advanced disease at diagnosis. That localized cancer had a much lower and reducing impact on LOLE underlines the need to prioritize public health efforts to increase awareness of the signs of early cancer, seek prompt medical clarification and participate in recognized screening programs.
On face value, the measure of YLL provides more up to date information about life expectancy than LOLE because YLL is based on more recent mortality statistics than the diagnostic period on which our study is necessarily based to allow for extrapolation of the expected and observed survival curves. For example, a recent Norwegian study reported YLL up to the year 2012 [1]. However, not only are these mortality statistics based on people diagnosed much earlier, the actual diagnostic period is typically not known or reported. Treatment for cancer usually occurs soon after diagnosis, so the impact that earlier diagnosis or treatment may have on loss of life expectancy would occur closer to the time of diagnosis rather than the time of death. Therefore, by reporting estimates of life expectancy according to diagnostic period, not mortality period, we provide a more realistic and transparent picture of the contemporariness and relevance of the results.
The rationale behind this approach of calculating remaining life expectancy following a cancer diagnosis is similar to that proposed by Liu et al. [10] who used a semiparametric extrapolation method on annual life tables in the USA to calculate expected years of life lost (EYLL), similar in meaning to our LOLE measure. Across a similar time period (1992–2005 vs 1990–2000) but with a shorter follow-up (2006 vs 2010), Liu et al. found similar, but generally lower, estimates of EYLL for Americans to our results in LOLE for Australians with lung cancer (EYLL = 13.8 years vs LOLE = 14.3 years), colorectal cancer (6.5 vs 7.2), female breast cancer (6.3 vs 6.7) and prostate cancer (1.8 vs 2.9). Importantly, both methods do not require accurate cause of death information. These methods are in contrast to other recent studies [1, 2] reporting years of life lost due to cancer. One advantage the flexible parametric method has over that described by Liu et al. [10] is that it is readily implemented using existing routines [7, 17] available in standard statistical software such as Stata (Statacorp, College Station, Texas 77845 USA), thus enabling access to a large suite of post-estimation and visualization options.
Despite the differences in methodology mentioned above, our results showing a reduction in LOLE over time are consistent with a recent study in the USA [2] that used life table methods to separate the competing impacts of YLL due to cancer mortality and those due to other causes. This investigation also found an overall reduction in the burden of cancer-specific mortality across time for most cancer types.
Strengths of our study include the use of national data for cancer registration, population mortality and estimated resident population, an advantage over a recent US study on PYLL that obtained cancer and non-cancer mortality rates from different geographical areas [2]. While the national estimates were not adjusted for spread of disease at diagnosis, by using state-specific data we were able to demonstrate that the decreases in LOLE were generally consistent across localized and regional cancers, but less evident among distant cancers.
Limitations include the lack of additional information about management strategies and that the use of population mortality rates may be less valid for some cancer types due to shared risk factors for other causes of deaths. For example, smoking is related to lung cancer, but it also greatly increases the risk of cardiovascular death. It has been demonstrated that the predictive ability of the flexible parametric method is robust [5], particularly when the cohort had at least 10 years of potential follow-up, and this is consistent with the results of our sensitivity analyses. This is the case for all years in our study cohort, and further analyses (Supplementary Figure 3) demonstrated a strong concordance between the observed relative survival estimates and the modeled estimates.
In conclusion, the observed reduction in LOLE experienced by people diagnosed with cancer in Australia should provide hope for patients and increased motivation for those involved in cancer care, support, research and policy to continue their efforts to reduce the burden of cancer in the community.
References
Brustugun OT, Moller B, Helland A (2014) Years of life lost as a measure of cancer burden on a national level. Br J Cancer 111:1014–1020
Soneji S, Beltran-Sanchez H, Sox HC (2014) Assessing progress in reducing the burden of cancer mortality, 1985–2005. J Clin Oncol 32:444–448
van Kruijsdijk RC, van der Graaf Y, Koffijberg H et al (2016) Cause-specific mortality and years of life lost in patients with different manifestations of vascular disease. Eur J Prev Cardiol 23:160–169
Ibayashi H, Pham TM, Fujino Y et al (2011) Estimation of premature mortality from oral cancer in Japan, 1995 and 2005. Cancer Epidemiol 35:342–344
Andersson TM, Dickman PW, Eloranta S, Lambe M, Lambert PC (2013) Estimating the loss in expectation of life due to cancer using flexible parametric survival models. Stat Med 32:5286–5300
Baade P, Youlden D, Andersson TM et al (2015) Estimating the change in life expectancy after a diagnosis of cancer among the Australian population. BMJ Open 5:e006740
Royston P, Parmar MK (2002) Flexible parametric proportional-hazards and proportional-odds models for censored survival data, with application to prognostic modelling and estimation of treatment effects. Stat Med 21:2175–2197
Hwang JS, Wang JD (1999) Monte Carlo estimation of extrapolation of quality-adjusted survival for follow-up studies. Stat Med 18:1627–1640
Hwang JS, Wang JD (2004) Integrating health profile with survival for quality of life assessment. Qual Life Res 13:1–10; discussion 1–4
Liu PH, Wang JD, Keating NL (2013) Expected years of life lost for six potentially preventable cancers in the United States. Prev Med 56:309–313
AIHW (2015) Life expectancy. Australian Institute of Health and Welfare. (http://www.aihw.gov.au/deaths/life-expectancy/) Accessed 7th Apr 2015
AIHW (2013) Cancer in Australia: actual incidence data from 1991 to 2009 and mortality data from 1991 to 2010 with projections to 2012. Asia Pac J Clin Oncol 9:199–213
AIHW, AACR (2012) Cancer in Australia: an overview, 2012. Cancer series 74. Cat. No. CAN 70. Australian Institute of Health and Welfare (AIHW) and Australasian Association of Cancer Registries (AACR), Canberra
Baade PD, Youlden DR, Valery PC et al (2010) Trends in incidence of childhood cancer in Australia, 1983–2006. Br J Cancer 102:620–626
Baade PD, Youlden DR, Chambers SK (2011) When do I know I am cured? Using conditional estimates to provide better information about cancer survival prospects. Med J Aust 194:73–77
Lambert PC, Royston P (2009) Further development of flexible parametric models for survival analysis. Stata J 9:265–290
Royston P, Lambert PC (2011) Flexible parametric survival analysis using stata: beyond the cox model. Stata Press, College Station
Van Ewijk RJ, Schwentner L, Wockel A et al (2013) Trends in patient characteristics, treatment and survival in breast cancer in a non-selected retrospective clinical cohort study of 2600 patients. Arch Gynecol Obstet 287:103–110
Roder D, Karapetis CS, Wattchow D et al (2015) Colorectal cancer treatment and survival: the experience of major public hospitals in South Australia over three decades. Asian Pac J Cancer Prev APJCP 16:2431–2440
Allemani C, Rachet B, Weir HK et al (2013) Colorectal cancer survival in the USA and Europe: a CONCORD high-resolution study. BMJ Open 3:e003055
Rosa F, Alfieri S, Tortorelli AP, Fiorillo C, Costamagna G, Doglietto GB (2014) Trends in clinical features, postoperative outcomes, and long-term survival for gastric cancer: a western experience with 1278 patients over 30 years. World J Surg Oncol 12:217
Wei EK, Wolin KY, Colditz GA (2010) Time course of risk factors in cancer etiology and progression. J Clin Oncol 28:4052–4057
Parkin E, O’Reilly DA, Sherlock DJ, Manoharan P, Renehan AG (2014) Excess adiposity and survival in patients with colorectal cancer: a systematic review. Obes Rev 15:434–451
Allott EH, Masko EM, Freedland SJ (2013) Obesity and prostate cancer: weighing the evidence. Eur Urol 63:800–809
Goodwin PJ (2010) Commentary on: “effect of obesity on survival in women with breast cancer: systematic review and meta-analysis” (Melinda Protani, Michael Coory, Jennifer H. Martin). Breast Cancer Res Treat 123:637–640
Protani M, Coory M, Martin JH (2010) Effect of obesity on survival of women with breast cancer: systematic review and meta-analysis. Breast Cancer Res Treat 123:627–635
Allemani C, Weir HK, Carreira H et al (2015) Global surveillance of cancer survival 1995–2009: analysis of individual data for 25,676,887 patients from 279 population-based registries in 67 countries (CONCORD-2). Lancet 385:977–1010
Moyer VA, Force USPST (2014) Screening for lung cancer: U.S. preventive services task force recommendation statement. Ann Intern Med 160:330–338
Green AC, Baade P, Coory M, Aitken JF, Smithers M (2012) Population-based 20-year survival among people diagnosed with thin melanomas in Queensland, Australia. J Clin Oncol 30:1462–1467
Whiteman DC, Baade PD, Olsen CM (2015) More people die from thin melanomas (1 mm) than from thick melanomas (>4 mm) in Queensland, Australia. J Investig Dermatol 135:1190–1193
Acknowledgments
We thank the staff of the State and Territory Cancer Registries and the Australian Cancer database, from which these study data were obtained.
Funding
Philippa Youl is funded by a National Health and Medical Research Council Early Career Fellowship (#1054038). The funding body had no input into the study design, the collection, analysis and interpretation of data, the writing of the report or the decision to submit the article for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest.
Ethical approval
Approval for the use of the anonymized data was provided by all of the individual State and Territory Cancer Registries through the Australian Institute of Health and Welfare (AIHW), with the exception of the Australian Capital Territory (ACT).
Informed consent
Since no individuals were identified nor able to be contacted, informed consent was not required.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Baade, P.D., Youlden, D.R., Andersson, T.M. et al. Temporal changes in loss of life expectancy due to cancer in Australia: a flexible parametric approach. Cancer Causes Control 27, 955–964 (2016). https://doi.org/10.1007/s10552-016-0762-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-016-0762-1