Abstract
Purpose
To better understand the relevance of environmental factors to the changing patterns of bone cancer subtypes, we examine the incidence of osteosarcoma (OS), Ewing sarcoma (ES), and chondrosarcoma (CS) using data from cancer incidence in five continents.
Methods
Age-specific and age-standardized incidence rates (ASRs) per 100,000 person-years were computed and stratified by country (n = 43), subtype, and sex during 2003–2007. Temporal patterns of ASRs were examined during 1988–2007 (12 countries). Age–period–cohort models were fitted for the USA and UK by subtype.
Results
For most countries, OS represented 20–40 % of all bone cancers, ES < 20 %, while CS proportions varied more considerably. Overall ASRs of bone cancers were 0.8–1.2/100,000 in men and 0.5–1.0 in women (0.20–0.35/100,000 for OS and 0.10–0.30/100,000 for CS in both men and women, and <0.10–0.25/100,000 in men and 0.05–0.25/100,000 in women for ES). The age-specific incidence rates revealed a bimodal peak of OS, one peak of ES in childhood, and a more heterogeneous pattern for CS. The overall bone cancer incidence trends are generally flat, but more heterogeneous for ES and CS. A declining OS incidence was observed in the UK and USA (men), an increase in CS in the UK and USA (female), and an apparent increase in ES, followed by a leveling off in successive US and UK cohorts.
Conclusion
Monitoring bone cancer incidence trends with data assembled from a geographically broader range of registries may generate hypotheses about additional risk factors and ensure that high-risk populations are not overlooked in cancer control efforts.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Compared to many other types of cancer, primary bone cancers are rare tumors worldwide [1]. They encompass many different subtypes, the most common of which are osteosarcoma (OS), Ewing sarcoma (ES), and chondrosarcoma (CS). Apart from a few established risk factors for OS and ES, and a male predominance for each of the three subtypes, relatively little is known about their etiological pathways for bone cancer and its subtypes [2].
OS occurs both in adolescence and at older ages [2], and numerous putative factors have been implicated in its etiology: exposure to radiation [3–5] and chemotherapy [3, 4], parental employment in farming, horticulture, and animal husbandry [6], and a person’s birth weight and height [7, 8]. While earlier studies have shown an association between higher fluoride exposure and OS risk [9], more recent findings are contradictory but somewhat inconclusive given they were based on aggregate statistics (fluoride level) for individual’s residence area rather than individual exposure measurements [10]. ES occurs mostly in children and young adults (<35 years) and is particularly rare among Asian and black populations [2] with risk factors including parental exposure to farm [6, 11–13], farm chemicals [12, 13], farm animals [11], organic and wood dust [11], glues, and solvents [12]. High incidence of hernias [12–14] among ES cases has been widely reported, with common embryological pathway (neuroectodermal origin) and environmental factors (farming) the possible link between these two entities [15]. CS usually afflicts people over 40 years, and incidence rates rise with age. Although there is some evidence that ionizing radiation may play a role [2, 16], risk factors for CS are largely unknown. Genetic abnormalities have been the subject of intense scrutiny as possible causes for bone cancers, and single nucleotide polymorphisms have been identified as a possible risk factors for OS [17–21] and a few for ES [22, 23]. However, no studies have yet found definitive pathways for either OS or ES development.
With a view to searching for novel environmental factors that may be associated with the changing patterns of bone cancer subtypes worldwide, we examine the descriptive epidemiology of the incidence of OS, ES, and CS, using data from the latest volume (X) of cancer incidence in five continents (CI5) [1]. We report the incidence patterns of primary bone cancer in 43 countries across four continents, comparing age-specific and age-adjusted incidence rates for the period 2003–2007. We also assess trends in incidence by 5-year calendar period 1988–2007 and for selected populations by birth cohort using age–period–cohort (APC) analyses and data from successive CI5 volumes (http://ci5.iarc.fr/CI5I-X/Default.aspx).
Methods
New cases of bone cancer diagnosed in 68 countries (312 registry populations including separate data for US whites and blacks) were available from CI5 [1] volume X for the period 2003–2007. Cases were categorized by sex, age (0–4, 5–9, … >85 years), and morphology. Corresponding population data were available from the same source. Incidence rates were grouped for OS (ICD-O-3 9180-9200), ES (ICD-O-3 9260), and CS (ICD-O-3 9210-9243) [24]; all other morphologies were categorized as “other,” and those with unspecified morphologies as “unspecified bone tumors” [1].
Age-specific incidence rates per 100,000 person-years were computed and stratified by country, morphologic type, and sex. Age-standardized incidence rates (ASRs) per 100,000 person-years were similarly estimated using the Segi world standard population [25]. Rates based on less than ten cases may be particularly unstable and should be interpreted with caution (see Supplementary Table 1 for detailed information regarding number of cases per 5 years by country, sex, and morphologic type). To examine temporal patterns, ASRs were also computed by morphologic type, sex, for the periods 1988–1992 [26], 1993–1997 [27], 1998–2002 [28], and 2003–2007 [1] for countries (n = 12) with <25 % unspecified bone cancers and total number of bone cancer cases (men and women) >120 (or 30 per 5-year period) across the four time-periods. Cases of bone cancer were available from CI5 volumes VII [26], VIII [27], IX [28], and X [1]. Comparisons of ASRs by calendar time were restricted to cancer registries that contributed data to each of these periods. Three groups were defined on the basis of their level of incidence, namely “low risk” (<0.25/100,000 for OS, <0.15/100,000 for ES, and <0.2/100,000 for CS), “high risk” (>0.35/100,000 for OS, >0.25/100,000 for ES, and >0.30/100,000 for CS), alongside an intermediate range. Tertiles were used to define the cutoff points as whole numbers.
We analyzed and compared incidence trends in men and women according to calendar period and birth cohort for each subtype in two countries (USA, UK), for which registry data were available in the three most recent consecutive CI5 volumes and with the largest number of respective bone cancer cases [1, 26–28]. Birth cohorts were obtained on subtracting the midpoints of 5-year age groups from the corresponding 5-year periods, and trends in incidence rates versus birth cohort by age were plotted using a semilog scale. Assuming that incidence rates were constant within the 5-year age classes and 5-year periods of diagnosis, an APC model was fitted [29, 30]. We assumed the number of new cases followed a Poisson random variable with the logarithm of the person-years at risk specified as an offset:
where λ refers to the rate, α a , β p , and γ c are functions of the age variable a, the period p, and the birth cohort c, respectively. The age, period, and cohort effects were estimated using the full APC model. The non-identifiability inherent in APC analyses—knowledge of the values of any two of age, period, and cohort implies knowledge of the third, making one of the factors redundant—was managed by constraining the linear component of the cohort effect to have zero slope in presenting the period effects. We present the estimates, assuming that the changes in rates (and specifically the underlying linear trends) may be attributed to birth cohort influences. Other interpretations and solutions are possible, and the model-based results should be interpreted with caution.
Synthetic birth cohorts were derived from 1-year period to 5-year age groups and the necessary smoothing was obtained using a natural splines function, with the number of parameters set to five for the age, period, and cohort effects, and hence, the number of events was the same between them. The longitudinal age-specific incidence rates and cohort rate ratios are presented using the reference cohort 1945 using the apcfit command (http://www.stata-journal.com/sjpdf.html?articlenum=st0211) in Stata [31]. As in a previous analysis, concerns regarding the data quality in the elderly for ES and the relatively sparse numbers of cases meant that modeling analyses were restricted to ages 0–64 years for ES; for the other histologic types, the age range was 0–84 years [32].
Results
Proportions of major subtypes 2003–2007
In the majority of the 68 countries included, OS represented 20–40 % of all bone cancers, ES represented less than 20 %, and for CS a larger variability was observed, with proportions ranging from <10 % in India and Saudi Arabia to over 45 % in Finland, Slovenia, and the Netherlands (Fig. 1). In general, in high-resource settings (e.g., Australia, Finland, France), there was a relatively small proportion (<20 %) of unspecified bone cancers. In low- to medium-resource areas (e.g., Algeria, Uganda, China, and Chile), the proportion of unspecified bone cancers tended to be higher, reaching 63 % in Uganda. For 25 countries, the unspecified proportion was >25 %; these datasets were considered to be of insufficient quality to report incidence by subtype and were thus excluded from further analysis. The total number of bone cancer cases from the 43 countries included in this report was 32,985 (28.5 % were OS, 15.0 % Ewing sarcoma, and 26.7 % CS). Detailed information regarding the number of cases per 5 years by bone cancer subtype, sex, and country is available in Supplementary Table 1.
Distribution of the main bone cancer morphological subtypes (proportion of new cases 2003–2007). *Countries where the total number of bone cancer cases <150; red line depicts the 25 % cutoff point for unspecified bone cancers (those populations with proportions >25 % were excluded from the analysis)
Age-standardized incidence rates 2003–2007
There is little variability observed in the rates of bone cancers (all subtypes) across countries in men (Fig. 2) and women (data not shown). For most countries, ASRs are in the range of 0.8–1.2/100,000 in men and 0.5–1.0 in women. For the specific bone cancer subtypes (Fig. 3), ASRs of OS across countries are quite similar in men and women (data not shown), with rates ranging from 0.20 to 0.35/100,000. For ES, differences are greater and more striking in men. ASRs of ES for men in the USA (blacks), Japan, Singapore, Ecuador, and Jamaica are low (<0.1/100,000), while elsewhere, ASRs are in the region of 0.15/100,000 to about 0.25/100,000 range in men and 0.05/100,000 to about 0.25/100,000 in women. For CS, the magnitude of rates between the sexes is not dissimilar, with rates in the 0.10–0.30/100,000 range.
Age-specific incidence rates 2003–2007
The age-specific incidence rates of bone cancer by subtype are shown in Fig. 4, with countries grouped according to the magnitude of their ASR by subtype. The bimodal peak of OS incidence can be seen in the age–incidence curves in most countries in both sexes, with incidence increasing steadily to a speculative second peak at elderly ages (>75 years). Both the early-age peak and the apparent peak in the elderly appear to be less pronounced in low-incidence countries compared to high-incidence countries. A similar peak in childhood is evident in the rates of ES, and as with OS, a peak is observed slightly earlier among women than in men. No second peak at older ages is apparent for ES, however, with rates declining to close to zero by middle age (>50 years). In contrast to childhood ages, rates in men were higher than in women at ages 15–24 irrespective at each of the three risk levels.
Bone cancer age-specific incidence rates by morphological subtype and level of incidence (see Sect. 2) in selected populations+; +26 populations where total number of bone cancer cases 2003–2007 were >150 and for which <25 % were unspecified bone cancers
The age-specific incidence rates of CS convey more heterogeneity between populations, with incidence increasing steadily to elderly ages at low risk, but a peak is seen earlier and more pronounced in countries at higher risk.
Time trends 1988–2007
Time trends of ASRs of bone cancers (overall and by subtype) are shown for selected countries in Figs. 5 and 6. The overall trends are generally flat in both sexes, with minor changes in incidence in a few countries, including increases in both sexes in the Netherlands, US black, and Norwegian women, but decreases among men in Sweden. The trends for OS are also rather stable for both men and women, with notable exceptions to increase in incidence rates among US black men and among Ireland women and decrease in incidence rates among Swedish men. The trends for OS were also examined separately for cases <40 years at diagnosis and 40 years and over. Heterogeneous patterns are observed for both men and women <40 years and ≥ 40 years (Supplementary Figures 1 and 2), with increases noted in men ≥40 years in US blacks, France, and Ireland and <40 years in Israel and in women ≥40 years in Norway and <40 years in the UK and Ireland. Decreases were noted in men ≥40 years in Australia and Norway and <40 years in Sweden and Finland.
Heterogeneous patterns are observed for ES incidence, with increases noted in men in Japan, Finland, and the Netherlands and in women in Israel, Canada, France, and the Netherlands. The trends in CS reveal only small changes in incidence over time, with rises in the Netherlands and France among men and in the Netherlands and US whites among women, with equivalent decreases in CS rates among men in Sweden and women in Ireland and Japan. With respect to other bone tumors, most countries exhibit either an increase in both sexes (e.g., Australia, Ireland, Norway, and Japan) or very little change. There are few changes in the incidence of unspecified bone cancers over time.
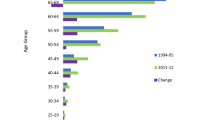
Incidence rates by calendar period and birth cohorts
Assuming a period slope of zero and hence drift attributed entirely to birth cohort, Fig. 7 presents for the USA and UK by sex the fitted longitudinal age-specific incidence rates (based on the reference cohort 1945) and relative changes (rate ratios) in incidence of OS, ES, and CS among cohorts born before and after the cohort reference. The sex-specific cohort effects conveyed some similarities in the UK and USA: A decrease in OS is evident in both sexes in the UK and among US men in cohorts born from 1890 to 1925, with minor increases thereafter. The CS incidence rate ratio increased in successive cohorts born during 1925–1955 in US females as well as in both sexes in the UK. For ES, an increase followed by a leveling off or decrease (in US women) in the rate ratios was observed in successive generations in both US and UK men and women, though caution is needed given the relatively few cases involved.
Discussion
This is the first comprehensive summary of bone cancer incidence by subtype worldwide. While there was less variation in the geographic and temporal patterns of incidence of bone cancers overall and for OS and CS, the patterns of incidence of ES showed greater variation, particularly among men. OS incidence has a bimodal age distribution across all populations globally. The first peak in adolescence coincides with the pubertal growth spurt [2], and several studies have reported a positive association between height [7, 8] and risk of OS. However, the patterns of incidence of OS across countries do not reveal a simple ecological association as incidence rates of OS are rather homogenous across populations and age groups despite, for example, a higher average adult height in Finland and Sweden compared with France, Italy, and Spain [33].
The peak in OS incidence late in life has been attributed to Paget’s disease [34, 35] of the bone (osteitis deformans), an established risk factor for OS. The incidence and prevalence of Paget’s disease vary between countries, but both burden measures have decreased in most global regions in recent years [36] with the disease becoming rare in certain Asian countries (e.g., China, Japan) [37, 38] where incidence of OS is relatively low. In particular, Mirabello et al. [35] have described the trends of OS in USA by subtype in the older age groups (age 60 years and over); incidence of OS with Paget’s disease decreased between 1973 and 2004. Although Paget disease has been linked with genetic predisposition [39], epidemiological evidence from migrant studies indicates that environmental influences are also present [40]. The mostly flat pattern of OS observed for both men and women ≥40 years in Japan, despite the decrease in prevalence of Paget’s disease, suggests that other risk factors, perhaps environmental factors, may play a role in the unchanged incidence of OS.
Development of second malignancies is a recognized late effect of chemotherapy and radiation exposure due to the treatment of childhood (e.g., 5.4 % of 3-year childhood cancer survivors developed Ewing sarcoma within 20 years [4]) [41] and adult cancers [42, 43]. Improvements in risk stratification have led to the use of lower doses of chemotherapy or radiation therapy with the aim of decreasing side effects without compromising survival outcome [41, 44]. For example, a linear relationship between risk of developing breast cancers and radiation dose among childhood cancer survivors has been reported [45]. In addition, Chung et al. [46] showed lower rates of second cancers in cancer patients treated with proton radiotherapy compared to conventional photon techniques. The rationale for proton radiotherapy is that it yields a superior dose distribution in target tissues with lower dose to normal tissues compared with other techniques and therefore likely to decrease the risk of second cancers [47, 48].
In countries as diverse as Sweden, Finland, Japan, Czech Republic, Poland, Russian Federation, and Costa Rica, the lower incidence rates appear to be mostly due to the lack of a peak in OS incidence at elderly ages. It may thus be postulated that a low incidence of Paget disease (e.g., in Japan) [36] combined with better cancer treatment over the past decades (thereby reducing late effects due to chemotherapy and radiotherapy) may have been important factors in lower incidence of OS later in life [4]. Anfinsen et al. [32] have reported age–period–cohort analysis of US data for bone cancers where a decline in incidence rates of OS in the USA during 1976–2005 among those over 60 years (cohorts born during 1905–1934) was seen. This observation, representing the second peak of the bimodal age–incidence curve of OS and a peak incidence around 70 years of age, can be extended to the UK in both sexes, but in this analysis, such a trend was not evident among US women. Mirabello et al. [49] reported that the patterns of incidence of OS in the young (<24 years) did not vary much between countries, while there was geographic variation among the elderly. Our study does not support their findings as geographic variation of both early-onset and old-age peaks in OS incidence was noted, as well as a heterogeneous pattern of trend for both age groups.
The patterns of incidence of ES across countries concur with the published literature [2] with rates somewhat higher among males than females up to the early peak in female incidence (at ages 10–14) which occurs 5 years earlier on average than in men; women have higher rates at ages 15–24. Although the cause of ES remains unknown, some clues regarding its etiology have emerged from the few case–control studies reported. Parental exposure to environmental factors [6, 11–13] leading to the disruption of normal embryological development of tissues by hormonal, environmental, or genetic factors during pregnancy has been implicated in its etiology [15]. It is not known whether risk factors for ES cases in adulthood are the same as for younger cases. The pronounced peak in teenage years in high- and mid-range incidence countries suggests that the varying patterns of incidence across countries may be associated with varying patterns of environmental exposure or the genetic makeup of the population in such countries. Furthermore, the fact that the incidence of adult ES cases appeared to be fairly similar across countries may suggest that the risk factors for this age group are different from those for younger cases.
Estrogen is involved in cartilage metabolism and plays an important role in human growth [50]. Estrogen receptor alpha is present in CS tumors supporting a possible role of estrogen signaling in CS proliferation [51]. Furthermore, estrogen has been shown to stimulate vascular endothelial growth factor, which is a characteristic trait of progression of CS [16]. Anfinsen et al. [32] have reported an increase in incidence rates of CS among females in the USA during 1976–2005 (although no change in incidence among men was seen). The declining cohort trends among US women born during 1935–1975 are replicated for UK women in this study, corresponding to the introduction of exogenous estrogen exposures (oral contraceptives, hormone therapy) in the 1960s. While the increasing use of oral contraceptive in the USA and the UK coincides with the generational increases seen in CS risk among women, the cohort-specific increases seen additionally among UK men in the 1960s remain unexplained by such an estrogen hypothesis. This suggests that other factors may also be associated with such an increase in incidence during this critical period.
Some cancer registries (e.g., UK, New Zealand, USA) have complete population coverage for incidence, while in other lower-resource areas data may be incomplete and of variable quality [52]. Such diversity in the availability, completeness, and validity of the data from different sources indicates that comparisons should be interpreted with caution. Nevertheless, registries included here were population based and considered consistently high quality, having been included in successive CI5 volumes. The CI5 process involves careful attention to the quality and comparability of the data (e.g., definition of an incident case of cancer, completeness of enumeration of cases in the population covered, stability of incidence rates over time, proportion of cases microscopically verified) [1]. In an attempt to ensure valid comparative analyses of bone cancer by subtype, we excluded data from countries where there was a substantial proportion of bone cancer cases for which subtype was not specified, and there were <150 bone cancer cases reported. This way we limited the analysis to regions where cancer registries provide data of good quality and attempted to avoid the problem of small numbers of cases which result in a large amount of variability in the distributions by diagnostic grouping. However, some calculations by subtype were based on rather few cases; these results should be interpreted with particular caution. The drawback in such an exclusion criterion is the incomplete geographic coverage.
The epidemiological patterns of bone cancer incidence worldwide showed rather limited variations in the geographic and temporal patterns of bone cancers overall, for OS and CS, but with greater variability seen for ES where rates in some registries were based on a small number of cases. Changes in successive birth cohorts may reveal the introduction, withdrawal, or change in one or more risk determinants, thus producing a change in disease incidence (increase or decrease) for individuals born at a particular point in time. Even though certain cohort effects were identified (for OS and CS), it remains difficult to link these to specific environmental causes, given the paucity of incidence data, inherent complexities in the model, and the limited insight presently into the underlying causes by subtype. A more complete account of the patterns of bone cancer incidence by subtype would be possible if comparable data were assembled from a broader range of registries that better describe the global extent of variation of incidence seen for ES or the heterogeneity between populations seen for CS where countries with “high risk” appear to have a pronounced increase in incidence early in life. Monitoring of incidence rates of bone cancers by subtype may also help generate hypothesis about additional risk factors and elucidate the relation between these cancers and known or suspected risk factors. In particular, APC analysis can help identify specific cohorts with high incidence of a particular bone cancer subtype enabling etiologic hypotheses that may explain the observed changes. Such monitoring will ensure that high-risk populations are not overlooked in cancer control efforts.
References
International Agency for Research on Cancer (2013) Cancer incidence in five continents, volume X (electronic version). In: Forman D, Bray F, Brewster D, Mbalawa CG, Kohler B, Piñeros M, Steliarova-Foucher E, Swaminathan R, Ferlay J (eds). IARC, Lyon http://ci5.iarc.fr. Accessed 10 Jan 2014
Miller RW, Boice JD, Curtis RE (2006) Cancer epidemiology and prevention. In: Schottenfeld D, Fraumeni FJ (eds) Cancer epidemiology and prevention, 3rd edn. Oxford University Press, New York, pp 946–958
Le Vu B, de Vathaire F, Shamsaldin A et al (1998) Radiation dose, chemotherapy and risk of osteosarcoma after solid tumours during childhood. Int J Cancer 77:370–377
Hawkins MM, Wilson LM, Burton HS et al (1996) Radiotherapy, alkylating agents, and risk of bone cancer after childhood cancer. J Natl Cancer Inst 88:270–278
Finkelstein MM, Kreiger N (1996) Radium in drinking water and risk of bone cancer in Ontario youths: a second study and combined analysis. Occup Environ Med 53:305–311
Hum L, Kreiger N, Finkelstein MM (1998) The relationship between parental occupation and bone cancer risk in offspring. Int J Epidemiol 27:766–771
Troisi R, Masters MN, Joshipura K, Douglass C, Cole BF, Hoover RN, The National Osteosarcoma Etiology Group (2006) Perinatal factors, growth and development, and osteosarcoma risk. Br J Cancer 95:1603–1607
Mirabello L, Pfeiffer R, Murphy G, Daw NC, Patino-Garcia A, Troisi RJ, Hoover RN, Douglass C, Schuz J, Craft AW, Savage SA (2011) Height at diagnosis and birth-weight as risk factors for osteosarcoma. Cancer Causes Control 22:899–908
Bassin EB, Wypij D, Davis RB, Mittleman MA (2006) Age-specific fluoride exposure in drinking water and osteosarcoma (United States). Cancer Causes Control 17:421–428
Blakey K, Feltbower RG, Parslow RC, James PW, Gomez Pozo B, Stiller C, Vincent TJ, Norman P, McKinney PA, Murphy MF, Craft AW, McNally RJ (2014) Is fluoride a risk factor for bone cancer? Small area analysis of osteosarcoma and Ewing sarcoma diagnosed among 0–49-year-olds in Great Britain, 1980–2005. Int J Epidemiol 43:224–234
Moore LE, Gold L, Stewart PA, Gridley G, Prince JR, Zahm SH (2005) Parental occupational exposures and Ewing’s sarcoma. Int J Cancer 114:472–478
Valery P, McWhirter W, Sleigh A, Williams G, Bain C (2002) Farm exposures, parental occupation and risk of Ewing’s sarcoma in Australia: a national case-control study. Cancer Causes Control 13:263–270
Holly EA, Aston DA, Ann DK, Kristiansen JJ (1992) Ewing’s bone sarcoma, paternal occupational exposure, and other factors. Am J Epidemiol 135(2):122–129
Winn DM, Li FP, Robison LL, Mulvihill JJ, Daigle AE, Fraumeni JF Jr (1992) A case-control study of the etiology of Ewing’s sarcoma. Cancer Epidemiol Biomarkers Prev 1:525–532
Valery PC, Holly EA, Sleigh AC, Williams G, Kreiger N, Bain C (2005) Hernias and Ewing’s sarcoma family of tumours: a pooled analysis and meta-analysis. Lancet Oncol 6:485–490
Bovee JV, Hogendoorn PC, Wunder JS, Alman BA (2010) Cartilage tumours and bone development: molecular pathology and possible therapeutic targets. Nat Rev Cancer 10:481–488
Savage SA, Burdett L, Troisi R, Douglass C, Hoover RN, Chanock SJ (2007) Germ-line genetic variation of TP53 in osteosarcoma. Pediatr Blood Cancer 49:28–33
Savage SA, Woodson K, Walk E et al (2007) Analysis of genes critical for growth regulation identifies insulin-like Growth Factor 2 Receptor variations with possible functional significance as risk factors for osteosarcoma. Cancer Epidemiol Biomarkers Prev 16:1667–1674
Savage SA, Mirabello L, Wang Z et al (2013) Genome-wide association study identifies two susceptibility loci for osteosarcoma. Nat Genet 45:799–803
Liu Y, He Z, Feng D, Shi G, Gao R, Wu X, Song W, Yuan W (2011) Cytotoxic T-lymphocyte antigen-4 polymorphisms and susceptibility to osteosarcoma. DNA Cell Biol 30:1051–1055
Ottaviani G, Jaffe N (2009) The etiology of osteosarcoma. Cancer Treat Res 152:15–32
Wang Q, Lei C, Wan H, Liu Q (2012) Improved cellular immune response elicited by a ubiquitin-fused DNA vaccine against Mycobacterium tuberculosis. DNA Cell Biol 31:489–495
Silva DS, Sawitzki FR, De Toni EC, Graebin P, Picanco JB, Abujamra AL, de Farias CB, Roesler R, Brunetto AL, Alho CS (2012) Ewing’s sarcoma: analysis of single nucleotide polymorphism in the EWS gene. Gene 509:263–266
World Health Organization (2000) International classification of diseases for oncology (ICD-0), 3rd ed. In: Fritz A, Percy C, Jack A, Shanmugaratnam K, Sobin L, Parkin DM, Whelan S (eds). World Health Organization, Geneva
Segi M (1960) Cancer mortality for selected sites in 24 countries (1950–57). In: Department of Public Health. Tohoku University of Medicine, Sendai, Japan
Parkin DM, Whelan SL, Ferlay J, Raymond L, Young J (eds) (1997) Cancer incidence in five continents, vol. VII (IARC Scientific Publications, No. 143). IARC, Lyon, France
Parkin DM, Whelan SL, Ferlay J, Teppo L, Thomas DB (eds) (2002) Cancer incidence in five continents, vol. VIII (IARC Scientific Publications, No. 155). IARC, Lyon, France
Curado MP, Edwards B, Shin HR, Storm H, Ferlay J, Heanue M, Boyle P (eds) (2007) Cancer incidence in five continents, vol. IX (IARC Scientific Publications, No. 160). IARC, Lyon, France
Clayton D, Schifflers E (1987) Models for temporal variation in cancer rates. I: age-period and age-cohort models. Stat Med 6:449–467
Clayton D, Schifflers E (1987) Models for temporal variation in cancer rates. II: age-cohort models. Stat Med 6:469–481
StataCorp (2011) Stata statistical software: release 12. StataCorp LP, College Station
Anfinsen KP, Devesa SS, Bray F, Troisi R, Jonasdottir TJ, Bruland OS, Grotmol T (2011) Age-period-cohort analysis of primary bone cancer incidence rates in the United States (1976–2005). Cancer Epidemiol Biomarkers Prev 20:1770–1777
Cavelaars AE, Kunst AE, Geurts JJ, Crialesi R, Grotvedt L, Helmert U, Lahelma E, Lundberg O, Mielck A, Rasmussen NK, Regidor E, Spuhler T, Mackenbach JP (2000) Persistent variations in average height between countries and between socio-economic groups: an overview of 10 European countries. Ann Hum Biol 27:407–421
Huvos AG (1986) Osteogenic sarcoma of bones and soft tissues in older persons. A clinicopathologic analysis of 117 patients older than 60 years. Cancer 57:1442–1449
Mirabello L, Troisi RJ, Savage SA (2009) Osteosarcoma incidence and survival rates from 1973 to 2004: data from the surveillance, epidemiology, and end results program. Cancer 115:1531–1543
Corral-Gudino L, Borao-Cengotita-Bengoa M, Del Pino-Montes J, Ralston S (2013) Epidemiology of Paget’s disease of bone: a systematic review and meta-analysis of secular changes. Bone 55:347–352
Wang WC, Cheng YS, Chen CH, Lin YJ, Chen YK, Lin LM (2005) Paget’s disease of bone in a Chinese patient: a case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 99:727–733
Okada K, Hasegawa T, Nishida J, Ogose A, Tajino T, Osanai T, Yanagisawa M, Hatori M (2004) Osteosarcomas after the age of 50: a clinicopathologic study of 64 cases—an experience in northern Japan. Ann Surg Oncol 11:998–1004
McKusick VA (1994) Medical genetics at Johns Hopkins: past, present and future, 11th edn. Johns Hopkins University Press, Baltimore
Gardner M, Guyer P, Barker D (1978) Radiological prevalence of Paget’s disease of bone in British migrants to Australia. Br Med J 1:1655–1657
Armstrong G, Stovallb M, Robinson L (2010) Long-term effects of radiation exposure among adult survivors of childhood cancer: results from the childhood cancer survivor study. Radiat Res 174:840–850
Kumar S (2012) Second malignant neoplasms following radiotherapy. Int J Environ Res Public Health 9:4744–4759
Palumbo A, Bringhen S, Kumar SK, Lupparelli G, Usmani S, Waage A, Larocca A, van der Holt B, Musto P, Offidani M, Petrucci MT, Evangelista A, Zweegman S, Nooka AK, Spencer A, Dimopoulos MA, Hajek R, Cavo M, Richardson P, Lonial S, Ciccone G, Boccadoro M, Anderson K, Barlogie B, Sonneveld P, McCarthy PL (2014) Second primary malignancies with lenalidomide therapy for newly diagnosed myeloma: a meta-analysis of individual patient data. Lancet Oncol 15:333–342
Egas-Bejar D, Huh W (2014) Rhabdomyosarcoma in adolescent and young adult patients: current perspectives. Adolesc Health Med Ther 5:115–125
Inskip P, Robison L, Stovall M, Smith S, Hammond S, Mertens A, Whitton J, Diller L, Kenney L, Neglia J (2009) Radiation dose and breast cancer risk in the childhood cancer survivor study. J Clin Oncol 27:3901–3907
Chung K, Keating N, Yock T, Tarbell N (2008) Comparative analysis of second malignancy risk in patients treated with proton therapy versus conventional photon therapy. Int J Radiat Oncol Biol Phys 72:S8
Kozak K, Adams J, Krejcarek S, Tarbell N, Yock T (2009) A dosimetric comparison of proton and intensity-modulated photon radiotherapy for pediatric parameningeal rhabdomyosarcomas. Int J Radiat Oncol Biol Phys 74(1):179–186
MacDonald S, Safai S, Trofimov A, Wolfgang J, Fullerton B, Yeap B, Bortfeld T, Tarbell N, Yock T (2008) Proton radiotherapy for childhood ependymoma: initial clinical outcomes and dose comparisons. Int J Radiat Oncol Biol Phys 71:979–986
Mirabello L, Troisi RJ, Savage SA (2009) International osteosarcoma incidence patterns in children and adolescents, middle ages and elderly persons. Int J Cancer 125:229–234
Bovee JV, Cleton-Jansen AM, Taminiau AH, Hogendoorn PC (2005) Emerging pathways in the development of chondrosarcoma of bone and implications for targeted treatment. Lancet Oncol 6:599–607
Meijer D, Gelderblom H, Karperien M, Cleton-Jansen AM, Hogendoorn PC, Bovee JV (2011) Expression of aromatase and estrogen receptor alpha in chondrosarcoma, but no beneficial effect of inhibiting estrogen signaling both in vitro and in vivo. Clin Sarcoma Res 1:5
Bray F, Znaor A, Cueva P, Korir A, Swaminathan R, Ullrich A, Wand S, Parkin D (2014) Quality control at the population-based cancer registry. In: Planning and developing population-based cancer registration in low- and middle-income settings (IARC Technical Publication no. 43). International Agency for Research on Cancer (IARC), Lyon, France, pp 21–26
Acknowledgments
PCV was supported by an Australian Research Council Future Fellowship (#FT100100511).
Conflict of interest
We declare that we have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Valery, P.C., Laversanne, M. & Bray, F. Bone cancer incidence by morphological subtype: a global assessment. Cancer Causes Control 26, 1127–1139 (2015). https://doi.org/10.1007/s10552-015-0607-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-015-0607-3