Abstract
Purpose
HER2-low triple-negative breast cancer (TNBC) accounted for up to 34%–39% of primary TNBC and 22.2%–32% of metastatic TNBC. Our study aims to explore the relationship between HER2 expression and clinicopathological characteristics, analyze the impact of HER2 expression on the pathological complete response (pCR) to neoadjuvant chemotherapy (NAC) in TNBC.
Methods
This study involved 191 patients with TNBC who underwent operation after NAC from October 2021 to August 2022. Clinicopathological characteristics and the frequency of pCR were compared between HER2-low and HER2-0 TNBC.
Results
42.2% (81/191) patients in our cohort were HER2-low. They exhibited differences in menopausal status, body mass index (BMI), androgen receptor (AR) expression, and histological grade (P < 0.05). Particularly, in HER2-low TNBC, AR was associated with tumor size, lymph node metastase, histological grade, and the incidence of multifocal disease (P < 0.05). The total pCR rate of entire cohor was 39.8%. Tumor size (P = 0.025), AR status (P = 0.033) and histological grade (P = 0.007) were significantly associated with the pCR rate of them, while the HER2 status did not exert a similar association. The multivariate analysis revealed that BMI (P = 0.004) and histological grade (P < 0.001) were associated with pCR of HER2-low TNBC, while tumor size (P = 0.034) and AR (P = 0.034) were associated with pCR of HER2-0 TNBC, respectively.
Conclusions
In our cohort, HER2-low TNBC patients exhibits specific clinical characteristics and response features to NAC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Triple-negative breast cancer (TNBC) is an intertwined disease exhibits highly heterogeneity, lacks effective therapeutic target, and resulting in poor prognosis [1].Therefore, novel therapeutic options are urgently needed and extensive research have conducted on anti-HER2 agents [2]. Currently, HER2 status is determined based on combined interpretation of immunohistochemistry (IHC) and fluorescence in situ hybridization (FISH) routinely. In 2018, the American Society of Clinical Oncology (ASCO)/College of American Pathologists (CAP) proposed that tumors with IHC 0, 1 + or 2 + and FISH negative are HER2-negative; tumors with IHC 3 + or 2 + and FISH positive are HER2-positive [3]. In TNBC, HER2 expression levels are ranging from IHC 0 to IHC 2 + and FISH negative. Recently, HER2-low breast cancer, which are defined as IHC 1 + or 2 + and FISH negative, have sparked intense interest. TNBC has been reclassification into HER2-low and HER2-0 subgroups [4]. Furthermore, HER2-low accounted for up to 34%-39% of primary TNBC and 22.2%–32% of metastatic TNBC [5, 6]. Historically, HER2-low patients cannot be benefited from conventional anti-HER2 therapies [7]. Nowadays, the novel antibody–drug conjugates (ADCs) have taken encouraging efficiency in HER2-low TNBC patients [8]. In addition, researches investigating the potential of HER2 vaccines and bispecific antibodies are under development [9].
About 10% to 50% of TNBC are androgen receptor (AR) positive and this subtype of TNBC characterized with distinct molecular features [10]. However, little is known about the molecular mechanism underlying HER2-low in AR-positive TNBC. The relationship between AR expression and clinicopathological characteristics of patients with different HER2 levels is still elusive. More data about HER2-low in AR-positive TNBC are urgently needed to explore effective therapeutic strategies for them.
The evaluation of neoadjuvant chemotherapy (NAC) efficacy can be conducted on the attainment of pathological complete response (pCR). In TNBC, pCR is highly correlated with favorable prognosis and has been regarded as a surrogate for forecasting prognosis such as event-free survival and overall survival (OS) [11]. However, the biology and pathology differences of HER2-0 and HER2-low TNBC and their response to standard NAC remains poorly investigated and controversial. Studies have shown that there was a similar pCR rate among these two groups, while HER2-low TNBC patients harbor aggressive clinicopathological features and worse prognosis [12]. In contrast, this population was found to have prolonged breast cancer-specific survival [13]. Therefore, further investigation which reclassify TNBC into HER2-0 and HER2-low is urgent needed, comprehensive understanding of their biological and responses to therapy may enable individualized treatment strategies.
We analyzed the correlation of HER2 levels with clinicopathological characteristics in TNBC patients, and further analyzed their correlation according to AR status. Then, we evaluated the predict value of HER2 expression on the frequency of attaining a pCR in the NAC setting.
Methods
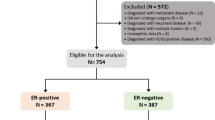
Study design and participants
We included 191 patients diagnosed with TNBC who met the inclusion and exclusion criteria in the First Affiliated Hospital of Jinzhou Medical University from October 2021 to August 2022. The basic and clinicopathological information of their core needle biopsy in initial pre-treatment status were collected from medical records, including age, menopausal status, body mass index (BMI), tumor size, lymph node metastasis, AR, Ki-67 index, histological grade, HER2, and with or without multifocal disease. Inclusion criteria: ① unilateral TNBC without distant metastasis; ② received NAC followed national and international guidelines and underwent surgery after completing NAC; ③ clinicopathological information and follow-up data were obtainable. Exclusion criteria: ① male breast cancer patients; ② patients with history of other malignancies; ③ patients who received unsystematic NAC or had severe complication. Evaluation criteria for pCR was no invasive cancer in the breast and axillary lymph nodes (ypT0/is, ypN0). AR status was evaluated by professional pathologists and AR positivity (1:100, Tenda) was defined as ≥ 1% percentage of nuclear staining cells in IHC.
HER2 evaluation
The HER2 status were evaluated by standard IHC (1:200, Roche) and FISH according to the ASCO/CAP guideline. Tumors with IHC 0 was defined as HER2-0, and tumors with IHC 1 + or IHC 2 + and FISH-negative was defined as HER2-low.
Statistical analysis
All analyses were performed using SPSS software (version 25). Chi-square analysis was used to test for the association of categorical variables. Univariate and multivariable logistic regression analysis were performed to assess the predictive factors for pCR. P < 0.05 was considered statistically significant.
Results
Relationship between HER2 expression and clinicopathological characteristics.
By HER2 expression level, 191 patients were enrolled into two groups: 81 (42.4%) patients were HER2-low TNBC and 110 (57.6%) patients were HER2-0 TNBC. Compared with HER2-low TNBC, HER2-0 TNBC exhibited more patients with premenopausal status (P = 0.011), BMI < 25 (P < 0.001), AR-negative (P < 0.001), and histological grade I/II (P = 0.031) (Table 1). There were no significant differences in other terms.
Relationship between AR expression and clinicopathological characteristics of patients with different HER2 levels.
According to different AR and HER2 levels, patients were enrolled into four groups. In HER2-low TNBC group, 35 (43.2%) patients were AR-negative and 46 (56.8%) patients were AR-positive; in HER2-0 TNBC group, 86 (78.2%) patients were AR-negative and 24 (21.8%) patients were AR-positive. Within the HER2-low TNBC group, AR-positive patients had smaller tumors (P = 0.007), fewer lymph node metastases (P = 0.002), lower histological grade (P = 0.008), and a lower incidence of multifocal disease (P = 0.022). The remaining clinicopathological characteristics were statistically insignificant (P > 0.05) (Table 2).
Univariate and multivariate analysis for pCR in TNBC.
We assessed the impact of each clinicopathological characteristic on pCR in TNBC. The total pCR rate of all enrolled patients was 39.8%. The univariate analysis showed that age (OR: 2.066; 95% CI 1.050–4.064; P = 0.036), tumor size (OR: 0.334; 95% CI 0.155–0.718; P = 0.005), AR status (OR: 2.154; 95% CI 1.147–4.043; P = 0.017) and histological grade (OR: 0.340; 95% CI 0.187–0.620; P < 0.001) were significant factors associated with pCR, respectively. Furthermore, multivariate analysis showed tumor size (OR: 0.393; 95% CI 0.173–0.892; P = 0.025), AR status (OR: 2.072; 95% CI 1.059–4.053; P = 0.033), and histological grade (OR: 0.414; 95% CI 0.219–0.783; P = 0.007) were independent factors for pCR. There was no statistical significance of pCR among patients with different menopausal status, BMI, lymph node metastasis status, Ki-67 expression levels, HER2 expression levels, and with and without multifocal disease (P > 0.05) (Table 3).
Univariate and multivariate analysis for pCR in HER2-low and HER2-0 TNBC
We further assessed the impact of clinicopathological characteristics on the frequency of pCR in TNBC with distinct HER2 expression levels, as demonstrated in Tables 4 and 5. The pCR rate was 34.6% in HER2-low patients and 42.7% in HER2-0 patients, the difference was not statistically significant. In HER2-low TNBC patients, BMI (OR: 0.346; 95% CI 0.126–0.951; P = 0.040) and histological grade (OR: 0.121; 95% CI 0.040–0.372; P < 0.001) were significant factors associated with pCR, respectively. Furthermore, multivariate analysis showed BMI (OR: 0.165; 95% CI 0.048–0.567; P = 0.004) and histological grade (OR: 0.072; 95% CI 0.020–0.257; P < 0.001) were still the independent factors for pCR of HER2-low TNBC. While in HER2-0 TNBC patients, tumor size (OR: 0.326; 95% CI 0.125–0.852; P = 0.022), AR status (OR: 2.864; 95% CI 1.037–7.910; P = 0.042) and Ki-67 level (OR: 0.285; 95% CI 0.088–0.924; P = 0.037) were significant factors associated with pCR, respectively. Furthermore, multivariate analysis showed tumor size (OR: 0.337; 95% CI 0.123–0.923; P = 0.034) and AR status (OR: 2.973; 95% CI 1.031–8.577; P = 0.044) were independent factors for pCR of HER2-0 TNBC.
Discussion
Given the dearth of validated therapeutic targets of TNBC and its unfavorable prognosis, continuous endeavors are being made to meet the unmet need of efficacious treatment alternatives for them [14]. The antibody of ADCs specifically binds to cell-surface proteins and translocate into cell, then release high concentration cytotoxic payloads [15]. Fam-trastuzumab deruxtecan (T-DXd), a novel HER2-targeted ADC prolonged survival of HER2-low patients, was the first FDA-approved therapeutic approach for advanced HER2-low breast cancer [16, 17]. With the significant anti-tumor activity and substantial bystander effect of ADCs, the traditional binary classification pattern of HER2 has been broken, a lot of research have focused on HER2-low breast cancer for comprehensively characterize them [18]. We characterized the clinicopathological features of HER2-low and HER2-0 TNBC and compared their response to NAC.
HER2-low TNBC occupied 42.4% of our entire cohort and they exhibited a higher proportion of postmenopausal status, BMI > 25, AR-positive, and high histological grade patients. Our result suggest HER2-low may take a propensity toward high-risk prognostic factors in TNBC. Within TNBC, a positive relation between HER2 and AR expression was recently reported. Concordance with our results, AR was an independent factor associated with HER2 status [13, 19]. In the molecular apocrine tumors, a specific subgroup of TNBC with AR expressing, the percentage of HER2-low was higher than that of HER2-0 [20]. Similarly, the higher prevalence of HER2-enriched subtype in the luminal androgen receptor subtype of TNBC supporting our results [21]. However, the clinicopathological characteristics of TNBC with different patterns of HER2 and AR expression remains poorly investigated. Particularly, we categorized patients into subgroups based on HER2 and AR expressions. In our cohort, AR-negative patients were inclined to have large tumor sizes, lymph node metastasis, high histological grade, and multifocal disease in HER2-low TNBC patients. Owing to the highly clinical efficacy and well tolerated side effects, AR inhibitor have spurred a new era of treatment approach for AR-positive TNBC patients [22]. The combining use of enzalutamide and trastuzumab have taken durable disease control for HER2 and AR-positive patients, the analysis of the AR-positive HER2-low TNBC patients may provide a reference for further combined treatment scheme in this targetless subtype [23].
In the entire cohort of our study, tumor size, AR status, and histological grade were independent factors for the rate of pCR. Specially, we explored the significant factors associated with pCR in HER2-low and HER2-0 TNBC patients respectively. In HER2-low TNBC patients, BMI < 25 and histological grade I/II presented a higher probability to attain pCR. While in HER2-0 TNBC patients, smaller tumor size and AR-positive were identified as independent positive factors for pCR. The effect of HER2-low in efficiency of NAC was unclear at present. In this study, HER2 expression level had no effect on the frequency of pCR. In a study of 2310 patients, the pCR rate of HER2-0 patients was higher than that of HER2-low patients in hormone receptor (HR) positive group, but no difference of pCR was seen in TNBC group [5]. Coherently, another study found that the pCR rate of HER2-0 group was a little lower than HER2-low group with no statistical difference [24]. Basing on existing results, HER2 expression may not associated with the efficacy of NAC in TNBC [25, 26].
We analyzed pCR as a surrogate for survival based on the FDA recommendation and pCR is an important evaluation index in NAC of TNBC. Patients who could not obtain pCR receive additional adjuvant capecitabine therapy have become the standard treatment in TNBC [27]. While the association between HER2 level and the survival of TNBC patients remains controversial. In early-stage TNBC, HER2-low group showed a shorter DFS and OS [28]. Some studies observed no significant survival value of HER2 expression in TNBC [25, 29, 30]. In contrast, it was found that HER2-low predicted a significant longer OS in early-stage TNBC [31]. Similarly, another analysis found that DFS and OS were significantly longer in the HER2-low group [26]. The lack of distinction between HER2 IHC 0 and 1 + by pathologists could be a crucial cause of the inconsistent results. Therefore, highly concordance in HER2 scoring is indispensable to further characterize HER2-low TNBC.
Our study presents some limitations. The sample size of is limited, and patients were selected from a single-center. A larger scale analysis is needed to further prove our conclusions rigorously. Moreover, due to the short follow-up duration, it was not feasible to assess the long-term prognosis of them. However, pCR served as an alternative surrogate endpoint for prediction of prognostic in TNBC. Consequently, we will scientifically conduct long-term follow-up to draw more conclusive conclusions.
Conclusion
This study revealed the biological properties and clinical features of HER2-low and HER2-0 TNBC, provides a crucial foundation of the predictive value on pCR and prognostic significance for them from a clinical perspective. In particularly, this study shed new light on HER2-low TNBC with different AR status, our analysis can potentially guiding research direction and providing clinical implications on the possibility of combined AR inhibition and novel ADCs treatment.
Data availability
Enquiries about data availability should be directed to the authors.
References
Bianchini G, De Angelis C, Licata L, Gianni L (2022) Treatment landscape of triple-negative breast cancer—expanded options, evolving needs. Nat Rev Clin Oncol 19:91–113. https://doi.org/10.1038/s41571-021-00565-2
Corti C, Giugliano F, Nicolò E, Tarantino P, Criscitiello C, Curigliano G (2023) HER2-low breast cancer: a new subtype? Curr Treat Options Oncol 24:468–478. https://doi.org/10.1007/s11864-023-01068-1
Wolff AC, Hammond MEH, Allison KH, Harvey BE, Mangu PB, Bartlett JMS et al (2018) Human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists Clinical practice guideline focused update. Arch Pathol Lab Med 142:1364–1382. https://doi.org/10.5858/arpa.2018-0902-SA
Tarantino P, Hamilton E, Tolaney SM, Cortes J, Morganti S, Ferraro E et al (2020) HER2-low breast cancer: pathological and clinical landscape. J Clin Oncol 38:1951–1962. https://doi.org/10.1200/JCO.19.02488
Denkert C, Seither F, Schneeweiss A, Link T, Blohmer JU, Just M et al (2021) Clinical and molecular characteristics of HER2-low-positive breast cancer: pooled analysis of individual patient data from four prospective, neoadjuvant clinical trials. Lancet Oncol 22:1151–1161. https://doi.org/10.1016/S1470-2045(21)00301-6
Gampenrieder SP, Dezentjé V, Lambertini M, De Nonneville A, Marhold M, Le Du F et al (2023) Influence of HER2 expression on prognosis in metastatic triple-negative breast cancer—results from an international, multicenter analysis coordinated by the AGMT Study Group. ESMO Open 8:100747. https://doi.org/10.1016/j.esmoop.2022.100747
Fehrenbacher L, Cecchini RS, Geyer CE, Rastogi P, Costantino JP, Atkins JN et al (2020) NSABP B-47/NRG oncology phase III randomized trial comparing adjuvant chemotherapy with or without trastuzumab in high-risk invasive breast cancer negative for HER2 by FISH and With IHC 1+ or 2+. J Clin Oncol 38:444–453. https://doi.org/10.1200/JCO.19.01455
Modi S, Jacot W, Yamashita T, Sohn J, Vidal M, Tokunaga E et al (2022) Trastuzumab deruxtecan in previously treated HER2-low advanced breast cancer. N Engl J Med 387:9–20. https://doi.org/10.1056/NEJMoa2203690
Chick RC, Clifton GT, Hale DF, Vreeland TJ, Hickerson AT, Kemp Bohan PM et al (2021) Subgroup analysis of nelipepimut-S plus GM-CSF combined with trastuzumab versus trastuzumab alone to prevent recurrences in patients with high-risk, HER2 low-expressing breast cancer. Clin Immunol 225:108679. https://doi.org/10.1016/j.clim.2021.108679
Venema CM, Bense RD, Steenbruggen TG, Nienhuis HH, Qiu SQ, Van Kruchten M et al (2019) Consideration of breast cancer subtype in targeting the androgen receptor. Pharmacol Ther 200:135–147. https://doi.org/10.1016/j.pharmthera.2019.05.005
Cortazar P, Zhang L, Untch M, Mehta K, Costantino JP, Wolmark N et al (2014) Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet 384:164–172. https://doi.org/10.1016/S0140-6736(13)62422-8
Hu XE, Yang P, Chen S, Wei G, Yuan L, Yang Z et al (2023) Clinical and biological heterogeneities in triple-negative breast cancer reveals a non-negligible role of HER2-low. Breast Cancer Res 25:34. https://doi.org/10.1186/s13058-023-01639-y
Ma Y, Jiao D, Zhang J, Lv M, Chen X, Liu Z (2023) HER2-low status was associated with better breast cancer-specific survival in early-stage triple-negative breast cancer. Oncologist. https://doi.org/10.1093/oncolo/oyad275
Leon-Ferre RA, Goetz MP (2023) Advances in systemic therapies for triple negative breast cancer. BMJ 381:e071674. https://doi.org/10.1136/bmj-2022-071674
Thomas A, Teicher BA, Hassan R (2016) Antibody–drug conjugates for cancer therapy. Lancet Oncol 17:e254–e262. https://doi.org/10.1016/S1470-2045(16)30030-4
(2022) T-DXd: new standard for HER2-low breast cancer. Cancer Discov 12:1828. https://doi.org/10.1158/2159-8290.Cd-nb2022-0043
Narayan P, Dilawari A, Osgood C, Feng Z, Bloomquist E, Pierce WF et al (2023) US Food and Drug Administration approval summary: fam-trastuzumab deruxtecan-nxki for human epidermal growth factor receptor 2-low unresectable or metastatic breast cancer. J Clin Oncol 41:2108–2116. https://doi.org/10.1200/JCO.22.02447
Schreiber AR, O’bryant CL, Kabos P, Diamond JR (2023) The emergence of targeted therapy for HER2-low triple-negative breast cancer: a review of fam-trastuzumab deruxtecan. Expert Rev Anticancer Ther 23:1061–1069. https://doi.org/10.1080/14737140.2023.2257885
Li Y, Tsang JY, Tam F, Loong T, Tse GM (2023) Comprehensive characterization of HER2-low breast cancers: implications in prognosis and treatment. EBioMedicine 91:104571. https://doi.org/10.1016/j.ebiom.2023.104571
Jacot W, Maran-Gonzalez A, Massol O, Sorbs C, Mollevi C, Guiu S et al (2021) Prognostic value of HER2-low expression in non-metastatic triple-negative breast cancer and correlation with other biomarkers. Cancers 13:6059. https://doi.org/10.3390/cancers13236059
Lehmann BD, Bauer JA, Chen X, Sanders ME, Chakravarthy AB, Shyr Y et al (2011) Identification of human triple-negative breast cancer subtypes and preclinical models for selection of targeted therapies. J Clin Invest 121:2750–2767. https://doi.org/10.1172/JCI45014
Choupani E, Gomari MM, Zanganeh S, Nasseri S, Haji-Allahverdipoor K, Rostami N et al (2023) Newly developed targeted therapies against the androgen receptor in triple-negative breast cancer: a review. Pharmacol Rev 75:309–327. https://doi.org/10.1124/pharmrev.122.000665
Wardley A, Cortes J, Provencher L, Miller K, Chien AJ, Rugo HS et al (2021) The efficacy and safety of enzalutamide with trastuzumab in patients with HER2+ and androgen receptor-positive metastatic or locally advanced breast cancer. Breast Cancer Res Treat 187:155–165. https://doi.org/10.1007/s10549-021-06109-7
De Moura LL, Cesca MG, Tavares MC, Santana DM, Saldanha EF, Guimarães PT et al (2021) HER2-low status and response to neoadjuvant chemotherapy in HER2 negative early breast cancer. Breast Cancer Res Treat 190:155–163. https://doi.org/10.1007/s10549-021-06365-7
Domergue C, Martin E, Lemarié C, Jézéquel P, Frenel JS, Augereau P et al (2022) Impact of HER2 status on pathological response after neoadjuvant chemotherapy in early triple-negative breast cancer. Cancers 14:2509. https://doi.org/10.3390/cancers14102509
Ergun Y, Akagunduz B, Karacin C, Turker S, Ucar G (2023) The effect of HER2-low status on pathological complete response and survival in triple-negative breast cancer: a systemic review and meta-analysis. Clin Breast Cancer 23:567–575. https://doi.org/10.1016/j.clbc.2023.05.015
Masuda N, Lee SJ, Ohtani S, Im YH, Lee ES, Yokota I et al (2017) Adjuvant capecitabine for breast cancer after preoperative chemotherapy. N Engl J Med 376:2147–2159. https://doi.org/10.1056/NEJMoa1612645
Sanomachi T, Okuma HS, Kitadai R, Kawachi A, Yazaki S, Tokura M et al (2023) Low HER2 expression is a predictor of poor prognosis in stage I triple-negative breast cancer. Front Oncol 13:1157789. https://doi.org/10.3389/fonc.2023.1157789
Yi X, Hu S, Ma M, Huang D, Zhang Y (2023) Effect of HER2-low expression on neoadjuvant efficacy in operable breast cancer. Clin Transl Oncol. https://doi.org/10.1007/s12094-023-03318-y
Horisawa N, Adachi Y, Takatsuka D, Nozawa K, Endo Y, Ozaki Y et al (2022) The frequency of low HER2 expression in breast cancer and a comparison of prognosis between patients with HER2-low and HER2-negative breast cancer by HR status. Breast Cancer 29:234–241. https://doi.org/10.1007/s12282-021-01303-3
Wei T, Wang D, Gao S, Wang X, Yue J, Kang Y et al (2023) Clinicopathologic characteristics and prognostic significance of HER2-low expression in patients with early breast cancer: a systematic review and meta-analysis. Front Oncol 13:1100332. https://doi.org/10.3389/fonc.2023.1100332
Funding
This article is funded by Education Department Foundation of Liaoning Province of China, LJKMZ20221227, Youth Science Program of the First Affiliated Hospital of Jinzhou Medical University, FYQKR-202201.
Author information
Authors and Affiliations
Contributions
Yue Shi contributed to conceptualization, data curation, investigation, project administration, validation, writing-original draft. Heng Lu contributed to formal analysis, investigation, methodology, resources, visualization. Yiqi Zhang contributed to conceptualization, resources, supervision, funding acquisition, writing – review & editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shi, Y., Lu, H. & Zhang, Y. Impact of HER2 status on clinicopathological characteristics and pathological complete response to neoadjuvant chemotherapy in triple-negative breast cancer. Breast Cancer Res Treat 206, 387–395 (2024). https://doi.org/10.1007/s10549-024-07317-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-024-07317-7