Abstract
Objective
To investigate the effects of HER2-low expression (HER2-low) and HER2-zero expression (HER2-0) on the pathological complete response (pCR) rate and survival of patients following neoadjuvant chemotherapy.
Methods
Eighty-six patients were followed up. Patients were divided into HER2-0 (immunohistochemistry (IHC) score of 0 (IHC0)) and HER2-low (IHC1+ or IHC2+/in situ hybridization non-amplified (ISH-)) groups according to the IHC detection of puncture tissues. After neoadjuvant chemotherapy, the clinical characteristics, pCR rate and DFS were compared between the two groups.
Results
There were 24 (27.9%) cases with HER2-0 and 62 (72.1%) cases with HER2-low. Hormone receptor-positive (HR+) patients accounted for 77.4% of the HER2-low group, which was higher than 70.8% in the HER2-0 group, and there was no significant difference between the two groups (p = 0.524). There were statistical differences in the pT and pN stages between HER2-low and HER2-0 subgroups in the triple-negative breast cancer (TNBC) group after neoadjuvant chemotherapy. The HER2-low subgroup had an earlier T stage (p = 0.009), and the ratio of N0 to N1 in the HER2-low and HER2-0 subgroups was 92.9% and 71.4%, respectively (p = 0.037). The Ki-67 index and median PR value were significantly lower in the HER2-low group after neoadjuvant chemotherapy (p = 0.002, p = 0.018). The HER2 IHC score was altered in the HER2-low group, and the HER-2 (2+) score changed significantly (p = 0.002). Seventy-eight patients with complete immunohistochemical data were analyzed. The discordance rate of the IHC score of HER2 after neoadjuvant chemotherapy was 38.5%, and eight patients with HER2-low showed HER2-0 status, with a discordance rate of 10.3%. After neoadjuvant chemotherapy, The pCR rate was significantly lower in the HER2-low group compared with that in the HER2-0 group (4.8% vs. 8.3%; p = 0.914), but the recurrence and metastasis rates were lower in the HER2-low group (9.7% vs. 20.8%; p = 0.165). There were no differences in DFS between the two groups at 6, 12, 24, and 36 months (p = 0.076; p = 0.518; p = 0.245; p = 0.406). The subgroup analysis demonstrated no significant difference in DFS between HER2-low and HER2-0 subgroups in the HR + and TNBC groups (p = 0.141, p = 0.637).
Conclusion
This retrospective study indicates that HER2-low has no significant effect on neoadjuvant efficacy in operable breast cancer. There were no statistical differences in clinical characteristics, pCR rate, and DFS between the HER2-low and the HER2-0 groups. There was no evidence that a HER2-low status constitutes a unique biological subtype, suggesting that more clinical data might be needed to verify these observations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most common malignant tumor in women, and its incidence is increasing yearly. Studies have shown that this incidence surpassed that of lung cancer in 2021 and ranked top among malignant tumors [1]. The National Comprehensive Cancer Network guidelines classify breast cancer into four subtypes based on the expressions of estrogen receptor (ER), progesterone receptor (PR), human epidermal growth factor receptor-2 (HER-2), and Ki-67 proliferation index [2]. Breast cancer is a highly heterogeneous disease, and different subtypes have various prognoses. HER-2 is a receptor of transmembrane tyrosine kinase and is overexpressed in 15%-20% of human breast cancers. HER-2 overexpression is directly associated with invasive growth and poor prognosis of tumors [3]. The survival HER-2 positive patients has been significantly improved with the advent of anti-HER-2 targeted drugs. Early clinical trials like the NSABP B-47 study have found that only breast cancer with HER-2 over-expression can benefit from anti-HER2-targeting drugs [4, 5], and these findings continue to inform clinical decision-making. According to the 2018 American Society of Clinical Oncology/College of American Pathology, HER-2 is dichotomized as HER-2 positive and HER-2 negative, which means that HER-2 (3+/2+) detected by immunohistochemistry (IHC) and positive in situ hybridization (ISH) tests can be judged as HER-2 overexpression, otherwise HER-2 negative[6]. Previous clinical trials have shown the encouraging efficacy of novel HER2-targeted antibody–drug conjugates (ADCs) on HER2-low breast cancer [7]. Therefore, some scholars have proposed that such breast cancer may differ from luminal breast cancer and triple-negative breast cancer (TNBC). It has unique features and may benefit from new targeted therapies, suggesting that it is an independent biological subtype. Therefore, HER-2-negative breast cancer with IHC1 + or IHC2 + /ISH- is defined as HER2-low breast cancer and accounts for approximately 45–55% of all breast cancers[8]. Although the treatment strategy of HER2-low breast cancer follows the treatment scheme of HER2-negative breast cancer, previous research has shown that its clinical and molecular characteristics are different from HER2-0 breast cancer [9, 10]. A prospective study concluded that HER2-low breast cancer had large tumor size, high histopathological grade, and high Ki-67 proliferation index; besides, it might be more likely to involve axillary lymph node, and its PCR rate was lower than that of HER2-0, especially in the HR + subgroup. The DFS of HER2-low patients was worse than that of HER2-0 breast cancer patients and even worse than that of HER2-overexpressed breast cancer patients who had taken anti-HER2-targeted agents [11, 12]. There is little research on the prognosis of HER2-low breast cancer, and data on its prognosis and response to neoadjuvant treatment are inconsistent. Therefore, more studies are required to guide the clinical application of new ADCs in this group of patients. To identify an optimal treatment for patients with HER2-low breast cancer, this study retrospectively analyzed the clinical and pathological features, efficacy of neoadjuvant chemotherapy, and disease-free survival rate of such patients.
Materials and methods
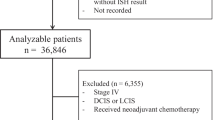
Cases source and inclusion and exclusion criteria
Breast cancer patients who were admitted to our hospital were selected from January 1, 2017, to December 31, 2020. Inclusion criteria: (1) Patients with newly diagnosed breast cancer that was confirmed by hollow needle aspiration with complete clinicopathological and follow-up data, (2) Clear status of ER, PR, HER-2, Ki-67; HER-2 (IHC2+) patients undergoing ISH detection to determine whether the HER-2 gene was amplified; and (3) Patients receiving neoadjuvant chemotherapy followed by modified radical mastectomy or breast-conserving surgery. Exclusion criteria: (1) Patients with distant metastasis by imaging examinations; (2) Patients with bilateral breast cancer; (3) Patients with a history of breast cancer; (4) Intolerance to chemotherapy or incomplete treatment; (4) Received neoadjuvant endocrine therapy; (5) Pregnancy-related breast cancer; (5) Patients with in situ carcinoma; (6) Complicated with other malignancies; and (7) severe information loss. The study met the requirements of the Declaration of Helsinki revised in 2013.
Treatment
Patients received neoadjuvant chemotherapy regimens based on anthracyclines, cyclophosphamide, and taxanes. Surgery was performed within 2 to 4 weeks after the last chemotherapy. Patients with radiotherapy indications received postoperative radiotherapy. HR-positive patients got adjuvant endocrine therapy.
Determination of biological indicators
Pathological data were reviewed, and we defined the indicators as positive with reference to ER and PR ≥ 1% by IHC. Definition of HER-2 status: HER2-zero expression (HER2-0) by IHC0; HER2-low by IHC1 + or IHC2 + /ISH-. Ki-67 ≥ 20% was defined as a high expression. The Chinese Anti-Cancer Association Guidelines and Specifications for Breast Cancer (2017 Edition) were followed for molecular typing for luminal type and triple-negative breast cancer (TNBC).
Observation indexes
The observation indexes included general clinical indicators (age, sex, and menopausal status), pathological characteristics (pathological type, histological grade, hormone receptor (HR) status, Ki-67, T stage, N stage, Miller-Payne (MP) grade, and pathological remission), recurrence, and metastasis.
Efficacy determination
The MP grading system was used to evaluate the histopathological efficacy of postoperative breasts. The pathological complete response (pCR) was defined as the absence of any malignancy or in situ carcinoma component (ypT0/Tis and ypN0 in the American Joint Committee on Cancer (AJCC) staging system) in the primary tumor and lymph nodes sampled after neoadjuvant chemotherapy. The tumor size and lymph node status were determined by the AJCC 7th edition staging system for breast cancer.
Follow-up
The follow-up was conducted by telephone, outpatient or inpatient reexamination, with a deadline of September 19, 2022. DFS was defined as the time from the surgery date to the time of tumor recurrence, metastasis or the date of the last follow-up.
Statistical methods
The IBM SPSS 23.0 software was used to establish a database and analyze data. Categorical variables were described using frequencies and rates, with the Chi-square test or Fisher’s exact test used for intergroup comparisons when there were cells with expected numbers of less than 5. Continuous variables conforming to the normal distribution were presented as means and standard deviations, and the independent samples t-test was used for intergroup comparisons. Continuous variables that did not meet the normal distribution were presented as quartiles, and the Mann–Whitney U test was used to compare the two groups. DFS was described using KM survival curves, and the log-rank test was performed to compare the survival rate between the groups. A p-value of less than 0.05 was considered statistically significant.
Results
Patients and clinical characteristics
A total of 86 patients were enrolled, including 85 females and one male, with a median age of 53 years (range, 28–80 years). There were 41 premenopausal patients (31.7% HER2-0 vs. 68.3% HER2-low), 44 postmenopausal patients (4.5% HER2-0 vs. 95.5% HER2-low), and one male (HER2-0). There were 74 cases with invasive ductal carcinoma (27% HER2-0 vs. 73% HER2-low), two with invasive lobular carcinomas (HER2-low), and ten with invasive ductal carcinoma complicated with other cancer components, such as micropapillary carcinoma, metaplastic carcinoma, mucinous carcinoma, medullary carcinoma, neuroendocrine carcinoma, and sweat gland (40% HER2-0 vs. 60% HER2-low). Twenty-four patients (27.9%) were HER2-0, and 62 (72.1%) were HER2-low. IHC1 + accounted for 48.4%, and IHC2 + for 51.6% in the HER2-low group. The median follow-up time was 32 months (range: 2–54 months). This study recruited 65 (75.6%) patients with HR-positive breast cancer and 21 (24.4%) with TNBC. There were no statistically significant differences in pathological type, histological grade, hormone receptor status, Ki-67 index, neoadjuvant chemotherapy response, pathological stage, and pCR, recurrence, and metastasis rates between HER2-low and HER2-0 groups and between HR + subgroups. However, the pT and pN stages were statistically different in the TNBC group after neoadjuvant chemotherapy. The HER2-low subgroup showed an earlier T stage (p = 0.009). The ratio of N0 to N1 was 92.9% and 71.4% in the HER2-low and HER2-0 subgroups, respectively (p = 0.037) (Table 1). The Ki-67 index and median PR value were significantly lower in the HER2-low group after neoadjuvant chemotherapy (p = 0.002, p = 0.018). The IHC score of HER2 was altered in the HER2-low group, and the HER-2 (2+) score changed significantly (p = 0.002) (Table 2). Except for five patients with complete pathological remission and three postoperative cases with missing parameter, 78 cases with complete pathological and immunohistochemical data before and after neoadjuvant chemotherapy were analyzed. The discordance rate of the HER2 score after neoadjuvant chemotherapy was 38.5%, mainly due to the change in IHC2 + status. We found that 7.7% of IHC2+ converted to IHC0 and 17.9% converted to IHC1+. Specifically, there were 21 cases of IHC0 before neoadjuvant chemotherapy, which remained IHC0 after neoadjuvant chemotherapy. There were 27 cases of IHC1+ before neoadjuvant chemotherapy, 2 (2.6%) of them converted to IHC0 after neoadjuvant chemotherapy, and 8 (10.3%) converted to IHC2+. There were 30 patients with HER2 (IHC2+) before neoadjuvant chemotherapy, 6 (7.7%) of them converted to IHC0 and 14 (17.9%) converted to IHC1+ after neoadjuvant chemotherapy (Fig. 1a). Besides, eight patients with HER2-low showed HER2-0 status after neoadjuvant chemotherapy, with a discordance rate of 10.3%. (Fig. 1b).
a Evolution of HER2 expression. This Sankey diagram shows the evolution of HER2 expression from baseline biopsy to residual disease after neoadjuvant chemotherapy in patients failing to achieve pCR. b This Sankey diagram shows the evolution of HER2-zero and HER2-low convertion from baseline biopsy to residual disease after neoadjuvant chemotherapy in patients failing to achieve pCR
Effect of HER-2 status on pCR
According to the pCR definition, the pCR rate of HER2-low and HER2-0 groups after neoadjuvant chemotherapy was 4.8% and 8.3%, respectively. The pCR rate of the HER2-low group was half of that of the HER2-0 group, with no statistical difference between the two groups (p = 0.914). In the HR + subgroup, the pCR rate was 5.9% in HER2-0 cases and 0% in HER2-low cases, with no statistical difference (p = 0.262). In the TNBC subgroup, the pCR rate was 14.3% in HER2-0 cases and 21.4% in HER2-low cases, with no significant difference (p = 1.000). Analysis of HR-positive and TNBC subtypes showed that HER-2 status did not affect the pCR rate (Fig. 2).
Effect of HER-2 status on recurrence and metastasis
The number of recurrent and metastatic cases was similar between the two groups but was higher in the HER2-0 group (HER2-low 6/62, 9.7%; HER2-0 5/24, 20.8%), with no significant difference (p = 0.165). In the HR + and TNBC groups, there was no statistical difference in recurrence and metastasis rates between HER2-low and HER2-0 subgroups (p = 0.179, p = 1.000). In the HR + group, the recurrence and metastasis rates of HER2-low and HER2-0 subgroups were 10.4% (5/48) and 23.5% (4/17), respectively. In the TNBC group, the recurrence and metastasis rates of HER2-low and HER2-0 subgroups were 7.1% (1/14) and 14.3% (1/7), respectively (Table 1).
Influence of HER-2 status on DFS
There was no significant difference in DFS between the two groups. The DFS rates of HER2-low and HER2-0 groups at 6, 12, 24, and 36 months were 95%, 95%, 90.9%, and 87.9%, and 100%, 90.5%, 79.2% and 79.2%, respectively (Fig. 3). The subgroup analysis showed no significant difference in DFS between HER2-low and HER2-0 subgroups in HR + and TNBC groups (p = 0.141, p = 0.637) (Fig. 4).
Discussion
The molecular typing of breast cancer originated from the 2013 St. Gallen International Consensus on Breast Cancer. The HER-2 status was divided into HER-2 positive and HER-2 negative, and this dichotomy was reconfirmed by the 2017 American Society of Clinical Oncology/College of American Pathologists (ASCO/CAP). Previous literature has confirmed that only patients with HER-2 amplification could benefit from anti-HER-2 targeted therapy [13]. However, HER-2 could not be classified as positive or negative since it was always expressed in tumor tissues [14]. This dichotomy is currently challenged by the advent of antibody–drug conjugates (ADCs) [7, 15,16,17]. Clinicians are paying closer attention to whether HER2-low breast cancer can be defined as a new biological subtype.
In this study, the proportion of patients with HER2-low expression was 72.1%, which is higher than the reported 33% to 64% in foreign literature [9, 18,19,20,21]. This difference might be related to the small number of samples and the high proportion of IHC1+. There was no clinical significance between HER-2 IHC0 and IHC1+, which might have affected the accuracy of the pathologist’s scores [21]. However, our data were consistent with domestic reports that indicated a proportion of 72.0% HER2-low [22]. Semi-quantitative IHC was insensitive, and some research revealed that formalin fixation can decrease protein expression, leading to the incorrect interpretation of HER-2 IHC0 and IHC1+, Moreover, ischemic time, fixation time, and the resection time from tissue blocks to unstained sections might be influencing factors [4, 23]. Although the IHC score of HER2 followed ASCO/CAP guidelines, its reproducibility could not be guaranteed, especially the IHC score of 0 or 1+. Moreover, recent literature has reported a poor agreement (< 70%) in the ERBB2 proficiency between cases of IHC0 and IHC1+ [24]. Therefore, the specimen evaluations in this study were performed in strict accordance with the guidelines by an experienced breast pathologist to reduce errors. With the therapeutic benefit of ADCs in HER2-low breast cancer, the differentiation of IHC0 and IHC1 + of HER2 needs urgent attention. New and more sensitive detection methods, such as fluorescence in situ hybridization (FISH), reverse transcription-polymerase chain reaction (RT-PCR), and PAM50, are required to confirm our results.
HR-positive expression (HR+ accounted for 77.4% in the HER2-low group, which was consistent with previous findings that reported a range of 65% to 83% [11, 19, 20]. There is also a crosstalk between the HER-2 and the ER pathways. A molecular analysis study on the expression characteristics of the PAM50 gene in HER2-low breast cancer found that the ERBB2 levels were higher in HR+/HER2-low tumors than in TNBC/HER2-low tumors [11]. Agostinetto et al. demonstrated that more than 50% of luminal breast cancer patients were HER2-low by PAM50 analysis, which is possibly due to the "luminal gene" being a tumor driver gene in these patients, while HER2 was not [20]. The above data indicated that the HR status is essential in HER2-low breast cancer patients.
This study showed that the general clinical characteristics of the two groups, such as median age of onset, menopausal status, differentiation grade, and pathological type, were similar and did not exhibit any distinctive features, which were consistent with previous reports [25]. Moreover, these data were not statistically different among HR+ subgroups. However, the HER2-low cases in the TNBC group showed earlier T/N stage after neoadjuvant chemotherapy. Horisawa et al. [26] also concluded that HR-/HER2-0 had a larger tumor size than HR-/HER2-low (p = 0.002). Nevertheless, there were small TNBC cases included in our investigation, which might lead to result bias. The clinicopathological characteristics of HER2-low and HER2-0 breast cancer were distinct due to the different HR statuses, especially in the TNBC subgroup, which might involve more complex mechanisms and need further in-depth study. The instability of HER2 expression levels in primary and residual lesions of breast cancer after neoadjuvant chemotherapy has previously been reported [27, 28], mainly the conversion between IHC1+/2+ and IHC0 [29, 30]. Our study found that the HER2 status of residual lesions changed after neoadjuvant chemotherapy, mainly IHC2+, which led to the conversion from HER2-low to HER2-0 in eight patients (10.3%). In contrast, the IHC0 status was relatively stable. Our study confirmed the frequent transformation of HER2 status in primary and residual lesions after neoadjuvant chemotherapy. Therefore, it was necessary to identify and screen HER2-low breast cancer for appropriate treatment.
The pathological stages of HER2-low and HER2-0 cases were primarily below stage II after neoadjuvant chemotherapy. The previously reported data were different. In a retrospective study of 72 cases of breast cancer, the proportion of stage III patients was 65.9% in the HER2-low group, while stage II was predominant in the HER2-0 group, accounting for about 61.3%. A significant difference between the two groups was also observed [19]. Previous data showed that Ki-67 was lower in the HER2-low group [21, 31]. Although there was no statistical difference in this study, the median Ki-67 value was significantly lower in the HER2-low group than in the HER2-0 group, which is possibly due to the higher Ki-67 values of TNBC. Besides, the proportion of HR + patients was higher in the HER2-low group. The Ki-67 index and median PR value decreased significantly in the HER2-low group after neoadjuvant chemotherapy, which was consistent with previous reports [32], indicating that chemotherapeutic drugs could alter PR and Ki-67 expressions. Therefore, reassessment of these two biomarkers after neoadjuvant chemotherapy can provide more valuable information for the treatment response and prognosis of breast cancer patients.
This study showed no statistical difference in pCR rate between HER2-low and HER2-0 cases in the overall analysis or HR + /TNBC subgroup analysis. In the overall cohort, the HER2-0 cases showed a higher pCR rate than HER2-low cases, but the overall pCR rate was lower in the HR + group (1.5%, 1/65) than in the TNBC group (23.5%, 4/17), suggesting that HER-2 status and pCR rate were not significantly correlated and that the chemotherapy sensitivity depended on HR status rather than HER2 expression. Moreover, the high proportion of HR + in the HER2-low group could indirectly affect its PCR rate. This was consistent with previous reports that showed no statistical difference in pCR rates in subgroups stratified by HR status [19, 31]. In contrast, Denkert et al. reported that HR expression affects the overall pCR rate. Neoadjuvant chemotherapy had a considerably lower benefit rate in HER2-low patients compared with that in HER2-0 patients, with pCR rates of 29.2% and 39.0%, respectively. In the subgroup analysis, the pCR rate varied across the HR + subgroups (17.5% vs. 23.6%, p = 0.024) but not between the TNBC categories [21]. However, in a retrospective study of 331 patients at the 2020 San Antonio conference, there was no difference in the pCR rate between HER2-0 and HER2-low cases in the HR + group (8% vs 13%; p = 0.35). The pCR rate of the HER2-0 case was higher than that of the HER2-low case in the TNBC group, with no statistical significance (56% vs 39%; p = 0.09) [33]. In general, the pCR rate was lower in the HER2-low group, possibly due to the higher proportion of HR + patients in the HER2-low group and the low response of HR + patients to traditional chemotherapy regimens. Therefore, more attention should be paid to the treatment regimens for HER2-low breast cancer patients.
Although the proportion of cases with recurrence and metastasis was higher in the HER2-0 group (20.8%) in this study, there was no statistical difference between the two groups, There was no difference in the recurrence and metastasis rates between HER2-low and HER2-0 subgroups in the HR + and TNBC groups. And, therefore, HER-2 status might not affect the prognosis. It remains controversial whether a HER2-low status might affect survival. Some literature reported that HER-2 status does not affect survival. Nevertheless, various evaluation indicators were used in other literature, such as recurrence-free survival (RFS), progression-free interval (PFI), disease-free interval (DFI), DFS, and overall survival (OS) [11, 19, 20, 22]. Some literature has suggested that it was crucial to determine whether HER2-low or HER2-0 was affected by different prognoses in luminal or triple-negative breast cancer and that the breast cancer should be stratified by HR status. However, regardless of HR status, there was no difference in the 5-year DFS rate between HER2-low and HER2-0 [34]. In contrast, Denkert et al. analyzed the data from four prospective neoadjuvant clinical trials and concluded that DFS and OS were significantly different between HER2-low and HER2-0 groups. DFS and OS were significantly longer in HER2-low patients than in HER2-0 patients in the TNBC subgroup. Although not statistically significant, there were prolonged DFS and OS tendencies in the HER2-low patients in the HR + subgroup [21]. Similarly, Hong et al. [35] concluded that a HER2-low status is a risk factor for postoperative recurrence or metastasis in TNBC patients with low DFS rates. In our study, the survival curve analysis showed that the DFS rate of early-stage HER2-0 is higher than that of HER2-low, but there was no advantage after eight months. This is possibly due to that most HER2-low patients showed positivity for HR and were in the endocrine maintenance treatment stage, which delayed disease recurrence and metastasis. Therefore, an extended follow-up was required for further verification.
Conclusion
HER2-low breast cancer accounted for about half of all breast cancers, and its role in clinical treatment decisions has received unprecedented attention with the publication of the DESTINY-BREAST 04 study. The above research found that low HER2 expression could not yet be an independent biological subtype, which was consistent with our conclusion that low HER-2 expression had no significant effect on neoadjuvant efficacy in operable cancer. Moreover, there was a switch of HER2 status between primary and residual lesions after neoadjuvant chemotherapy, which could affect the HER2 subtypes between HER2-low and HER2-0 subgroups. At present, HER2 detection mainly relies on IHC and ISH. However, the semi-quantitative detection of IHC0 and IHC1 + has some limitations and lacks the gold standard for lower-limit detection of HER2-low. Therefore, how to accurately identify and screen the benefit population of ADCs deserves in-depth studies. Nevertheless, the study had the following shortcomings: small sample size, single-center retrospective study, short follow-up time, and only clinical data on DFS, recurrence, and metastasis. Future research will expand the sample size, prolong the follow-up period, and carry out multi-center cooperation to confirm our findings.
Data availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
References
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer Statistics. CA Cancer J Clin. 2021;71(1):7–33. https://doi.org/10.3322/caac.21669.
Gradishar WJ, Moran MS, Abraham J, Aft R, Agnese D, Allison KH, et al. Breast Cancer, Version 3.2022, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2022;20(6):691–722. https://doi.org/10.6004/jnccn.2022.0030.
Yarden Y, Sliwkowski MX. Untangling the ErbB signalling network. Nat Rev Mol Cell Biol. 2001;2(2):127–37. https://doi.org/10.1038/35052073.
Fehrenbacher L, Cecchini RS, Geyer CE Jr, Rastogi P, Costantino JP, Atkins JN, et al. NSABP B-47/NRG Oncology Phase III randomized trial comparing adjuvant chemotherapy with or without trastuzumab in high-risk invasive breast cancer negative for HER2 by FISH and With IHC 1+ or 2. J Clin Oncol. 2020;38(5):444–53. https://doi.org/10.1200/JCO.19.01455.
Gianni L, Lladó A, Bianchi G, Cortes J, Kellokumpu-Lehtinen PL, Cameron DA, et al. Open-label, phase II, multicenter, randomized study of the efficacy and safety of two dose levels of Pertuzumab, a human epidermal growth factor receptor 2 dimerization inhibitor, in patients with human epidermal growth factor receptor 2-negative metastatic breast cancer. J Clin Oncol. 2010;28(7):1131–7. https://doi.org/10.1200/JCO.2009.24.1661.
Wolff AC, Hammond MEH, Allison KH, Harvey BE, Mangu PB, Bartlett JMS, et al. Human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists Clinical Practice Guideline Focused Update. J Clin Oncol. 2018;36(20):2105–22. https://doi.org/10.1200/JCO.2018.77.8738. (Epub 2018 May 30).
Modi S, Park H, Murthy RK, Iwata H, Tamura K, Tsurutani J, et al. Antitumor activity and safety of trastuzumab deruxtecan in patients With HER2-low-expressing advanced breast cancer: results from a Phase Ib study. J Clin Oncol. 2020;38(17):1887–96. https://doi.org/10.1200/JCO.19.02318.
Tarantino P, Hamilton E, Tolaney SM, Cortes J, Morganti S, Ferraro E, et al. HER2-low breast cancer: pathological and clinical landscape. J Clin Oncol. 2020;38(17):1951–62. https://doi.org/10.1200/JCO.19.02488. (Epub 2020 Apr 24).
Schettini F, Chic N, Brasó-Maristany F, Paré L, Pascual T, Conte B, et al. Clinical, pathological, and PAM50 gene expression features of HER2-low breast cancer. NPJ Breast Cancer. 2023;9(1):32. https://doi.org/10.1038/s41523-020-00208-2.
Zhang G, Ren C, Li C, Wang Y, Chen B, Wen L, et al. Distinct clinical and somatic mutational features of breast tumors with high-, low-, or non-expressing human epidermal growth factor receptor 2 status. BMC Med. 2022;20(1):142. https://doi.org/10.1186/s12916-022-02346-9.
Rossi V, Sarotto I, Maggiorotto F, Berchialla P, Kubatzki F, Tomasi N, et al. Moderate immunohistochemical expression of HER-2 (2+) without HER-2 gene amplification is a negative prognostic factor in early breast cancer. Oncologist. 2012;17(11):1418–25. https://doi.org/10.1634/theoncologist.2012-0194.
Eggemann H, Ignatov T, Burger E, Kantelhardt EJ, Fettke F, Thomssen C, et al. Moderate HER2 expression as a prognostic factor in hormone receptor positive breast cancer. Endocr Relat Cancer. 2015;22(5):725–33. https://doi.org/10.1530/ERC-15-0335.
Goldhirsch A, Winer EP, Coates AS, Gelber RD, Piccart-Gebhart M, Thürlimann B, et al. Personalizing the treatment of women with early breast cancer: highlights of the St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer. Ann Oncol. 2013;24(9):2206–23. https://doi.org/10.1093/annonc/mdt303. (Epub 2013 Aug 4).
Marchiò C, Annaratone L, Marques A, Casorzo L, Berrino E, Sapino A. Evolving concepts in HER2 evaluation in breast cancer: Heterogeneity, HER2-low carcinomas and beyond. Semin Cancer Biol. 2021;72:123–35. https://doi.org/10.1016/j.semcancer.2020.02.016. (Epub 2020 Feb 26).
Xu Z, Guo D, Jiang Z, Tong R, Jiang P, Bai L, et al. Novel HER2-Targeting Antibody-Drug Conjugates of Trastuzumab Beyond T-DM1 in Breast Cancer: Trastuzumab Deruxtecan(DS-8201a) and (Vic-)Trastuzumab Duocarmazine (SYD985). Eur J Med Chem. 2019;183:111682. https://doi.org/10.1016/j.ejmech.2019.111682. (Epub 2019 Sep 6).
Modi S, Jacot W, Yamashita T, Sohn J, Vidal M, Tokunaga E, et al. Trastuzumab deruxtecan in previously treated HER2-low advanced breast cancer. N Engl J Med. 2022;387(1):9–20. https://doi.org/10.1056/NEJMoa2203690. (Epub 2022 Jun 5).
Tamura K, Tsurutani J, Takahashi S, Iwata H, Krop IE, Redfern C, et al. Trastuzumab deruxtecan (DS-8201a) in patients with advanced HER2-positive breast cancer previously treated with trastuzumab emtansine: a dose-expansion, phase 1 study. Lancet Oncol. 2019;20(6):816–26. https://doi.org/10.1016/S1470-2045(19)30097-X. (Epub 2019 Apr 29).
Eiger D, Agostinetto E, Saúde-Conde R, de Azambuja E. The exciting new field of HER2-low breast cancer treatment. Cancers (Basel). 2021;13(5):1015. https://doi.org/10.3390/cancers13051015.
De Moura LL, Cesca MG, Tavares MC, Santana DM, Saldanha EF, Guimarães PT, et al. HER2-low status and response to neoadjuvant chemotherapy in HER2 negative early breast cancer. Breast Cancer Res Treat. 2021;190(1):155–63. https://doi.org/10.1007/s10549-021-06365-7. (Epub 2021 Aug 18).
Agostinetto E, Rediti M, Fimereli D, Debien V, Piccart M, Aftimos P, et al. HER2-low breast cancer: molecular characteristics and prognosis. Cancers (Basel). 2021;13(11):2824. https://doi.org/10.3390/cancers13112824.
Denkert C, Seither F, Schneeweiss A, Link T, Blohmer JU, Just M, et al. Clinical and molecular characteristics of HER2-low-positive breast cancer: pooled analysis of individual patient data from four prospective, neoadjuvant clinical trials. Lancet Oncol. 2021;22:1151–61. https://doi.org/10.1016/S1470-2045(21)00301-6. (Epub 2021 Jul 9).
Shao Y, Yu Y, Luo Z, Guan H, Zhu F, He Y, et al. ASO visual abstract: clinical, pathological complete response, and prognosis characteristics of HER2-low breast cancer in the neoadjuvant chemotherapy setting—a retrospective analysis. Ann Surg Oncol. 2022;29(13):8035–6. https://doi.org/10.1245/s10434-022-12420-4.
Fernandez AI, Liu M, Bellizzi A, Brock J, Fadare O, Hanley K, et al. Examination of low ERBB2 protein expression in breast cancer tissue. JAMA Oncol. 2022;8(4):1–4. https://doi.org/10.1001/jamaoncol.2021.7239.
Allison KH, Wolff AC. ERBB2-low breast cancer-is it a fact or fiction, and do we have the right assay? JAMA Oncol. 2022;8(4):610–1. https://doi.org/10.1001/jamaoncol.2021.7082.
Chen M, Chen W, Liu D, Chen W, Shen K, Wu J, et al. Prognostic values of clinical and molecular features in HER2 low-breast cancer with hormonal receptor overexpression: features of HER2-low breast cancer. Breast Cancer. 2022;29(5):844–53. https://doi.org/10.1007/s12282-022-01364-y. (Epub 2022 Jun 2 1).
Horisawa N, Adachi Y, Takatsuka D, Nozawa K, Endo Y, Ozaki Y, et al. The frequency of low HER2 expression in breast cancer and a comparison of prognosis between patients with HER2-low and HER2-negative breast cancer by HR status. Breast Cancer. 2022;29(2):234–41. https://doi.org/10.1007/s12282-021-01303-3.
Peng JH, Zhang X, Song JL, Ran L, Luo R, Li HY, et al. Neoadjuvant chemotherapy reduces the expression rates of ER, PR, HER2, Ki67, and P53 of invasive ductal carcinoma. Medicine. 2019;98(2):e13554. https://doi.org/10.1097/MD.0000000000013554.
Xian Z, Quinones AK, Tozbikian G, Zynger DL. Breast cancer biomarkers before and after neoadjuvant chemotherapy: does repeat testing impact therapeutic management? Hum Pathol. 2017;62:215–21. https://doi.org/10.1016/j.humpath.2016.12.019.
Yoshida A, Hayashi N, Suzuki K, Takimoto M, Nakamura S, Yamauchi H. Change in HER2 status after neoadjuvant chemotherapy and the prognostic impact in patients with primary breast cancer. J Surg Oncol. 2017;116(8):1021–8. https://doi.org/10.1002/jso.24762.
Miglietta F, Griguolo G, Bottosso M, Giarratano T, Lo Mele M, Fassan M, et al. HER2-low-positive breast cancer: evolution from primary tumor to residual disease after neoadjuvant treatment. NPJ Breast Cancer. 2022;8(1):66. https://doi.org/10.1038/s41523-022-00434-w.
Alves FR, Gil L, de Matos L, Baleiras A, Vasques C, Neves MT, et al. Impact of human epidermal growth factor receptor 2 (HER2) low status in response to neoadjuvant chemotherapy in early breast cancer. Cureus. 2022;14(2):e22330. https://doi.org/10.7759/cureus.22330.
Rey-Vargas L, Mejía-Henao JC, Sanabria-Salas MC, Serrano-Gomez SJ. Effect of neoadjuvant therapy on breast cancer biomarker profile. BMC Cancer. 2020;20(1):675. https://doi.org/10.1186/s12885-020-07179-4.
Reinert T, Sartori G P, Souza A A, Pellegrini R, Barrios CH. Abstract PS4–22: Prevalence of HER2-low and HER2-zero subgroups and correlation with response to neoadjuvant chemotherapy (NACT) in patients with HER2-negative breast cancer[C]// Abstracts: 2020 San Antonio Breast Cancer Virtual Symposium; December 8–11, 2020; San Antonio, Texas. 2021.https://doi.org/10.1158/1538-7445.SABCS20-PS4-22
Horisawa N, Adachi Y, Takatsuka D, Nozawa K, Endo Y, Ozaki Y, et al. The frequency of low HER2 expression in breast cancer and a comparison of prognosis between patients with HER2-low and HER2-negative breast cancer by HR status. Breast Cancer. 2022;2:29. https://doi.org/10.1007/s12282-021-01303-3. (Epub 2021 Oct 7).
Hong Y, Fang Q, Xi G, Xiaobo B. Clinical characteristics and prognosis analysis of triple negative breast cancer patients with low expression of HER-2. J China Med Univ. 2022;51(8):4.
Acknowledgements
The authors would like to express their gratitude to EditSprings (https://www.editsprings.cn) for the expert linguistic services provided.
Funding
Beijing Xisike Clinical Oncology Research Foundation.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Material preparation, data collection and analysis were performed by XY, YZ, SH, MM and DH. The first draft of the manuscript was written by XY and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Qingdao Hospital, University of Health and Rehabilitation Sciences (Qingdao Municipal Hospital) (2023− 004).
Informed consent
The study was done after agreement from the local ethics committee and written informed consent was obtained from all participants and/or their guardians.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yi, X., Hu, S., Ma, M. et al. Effect of HER2-low expression on neoadjuvant efficacy in operable breast cancer. Clin Transl Oncol 26, 880–890 (2024). https://doi.org/10.1007/s12094-023-03318-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-023-03318-y