Abstract
Purpose
Neoadjuvant anti-PD-(L)1 therapy improves the pathological complete response (pCR) rate in unselected triple-negative breast cancer (TNBC). Given the potential for long-term morbidity from immune-related adverse events (irAEs), optimizing the risk–benefit ratio for these agents in the curative neoadjuvant setting is important. Suboptimal clinical response to initial neoadjuvant therapy (NAT) is associated with low rates of pCR (2–5%) and may define a patient selection strategy for neoadjuvant immune checkpoint blockade. We conducted a single-arm phase II study of atezolizumab and nab-paclitaxel as the second phase of NAT in patients with doxorubicin and cyclophosphamide (AC)-resistant TNBC (NCT02530489).
Methods
Patients with stage I–III, AC-resistant TNBC, defined as disease progression or a < 80% reduction in tumor volume after 4 cycles of AC, were eligible. Patients received atezolizumab (1200 mg IV, Q3weeks × 4) and nab-paclitaxel (100 mg/m2 IV,Q1 week × 12) as the second phase of NAT before undergoing surgery followed by adjuvant atezolizumab (1200 mg IV, Q3 weeks, × 4). A two-stage Gehan-type design was employed to detect an improvement in pCR/residual cancer burden class I (RCB-I) rate from 5 to 20%.
Results
From 2/15/2016 through 1/29/2021, 37 patients with AC-resistant TNBC were enrolled. The pCR/RCB-I rate was 46%. No new safety signals were observed. Seven patients (19%) discontinued atezolizumab due to irAEs.
Conclusion
This study met its primary endpoint, demonstrating a promising signal of activity in this high-risk population (pCR/RCB-I = 46% vs 5% in historical controls), suggesting that a response-adapted approach to the utilization of neoadjuvant immunotherapy should be considered for further evaluation in a randomized clinical trial.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Immune checkpoint blockade has significantly altered the treatment landscape of triple-negative breast cancer (TNBC). In the metastatic setting, the addition of anti-PD-(L)1 therapy to chemotherapy has significantly improved progression-free and overall survival in patients with PD-L1 expressing TNBC [1,2,3,4]. More recently, two large randomized phase III studies demonstrated that the addition of anti-PD-(L)1 therapy, specifically atezolizumab or pembrolizumab, to anthracycline-based chemotherapy in the curative neoadjuvant setting resulted in a significant improvement in rates of pathological complete response (pCR) [5, 6] with subsequent follow-up data revealing a statistically significant difference in event-free survival (EFS) [7]. These data resulted in the approval of pembrolizumab for patients with high-risk, early-stage TNBC in combination with chemotherapy as neoadjuvant treatment, and then continued as a single agent as adjuvant therapy after surgery. However, given the potential for long-term morbidity from immune-related adverse events (irAEs), it is important to optimize the risk–benefit ratio for these agents in patients who are being treated with curative intent.
In contrast to the success of immune checkpoint blockade when used in combination with chemotherapy, the efficacy of immune checkpoint inhibitor monotherapy has been modest in TNBC [8]. Collectively, these data suggest that chemotherapy augments the clinical efficacy of immune checkpoint blockade in TNBC. Indeed, chemotherapeutic agents commonly used in TNBC such as anthracyclines, cyclophosphamide, taxanes, and platinum compounds have been shown to augment antitumor immunity [9,10,11,12,13]. Notably, anthracyclines have been shown to induce immunogenic cell death which is characterized by release of high mobility group box 1 and enhanced tumor antigen uptake and presentation by dendritic cells [14] and resistance to initial anthracycline-based neoadjuvant chemotherapy portends a low probability of pathological complete response (pCR) with additional chemotherapy [15, 16]. Thus, given the key role of chemotherapy in facilitating antitumor immunity and response to immune checkpoint blockade, it is unclear if anthracycline resistance abrogates the clinical benefit of immune checkpoint blockade in patients with TNBC. However, in addition to immunogenic effects mediated by tumor cell killing, anthracyclines have been reported to relieve suppression of antitumor immunity by favorably altering the immune milieu through elimination of myeloid-derived suppressor cells [17]. Thus, it is plausible that even in the setting of anthracycline resistance, direct immunogenic effects of anthracyclines may prime the tumor-immune microenvironment, paving the way for enhanced efficacy of immune checkpoint blockade in combination with other classes of chemotherapeutic agents such as taxanes, which have been shown to enhance T-cell and natural killer cell function in patients with stage II–III breast cancer [18].
Atezolizumab is a humanized immunoglobulin G1 monoclonal antibody that selectively targets PD-L1 thereby interfering with its interaction with the PD-1 receptor [1]. It has demonstrated a good safety profile in patients with TNBC, either as monotherapy [19] or in combination with chemotherapy [1]. Specifically, the combination of atezolizumab and nab-paclitaxel has demonstrated a favorable safety profile and promising signs of antitumor activity in patients with metastatic, PD-L1-expressing, TNBC [1].
Based on this background, we conducted a single institution, phase II study to determine the efficacy of neoadjuvant atezolizumab and nab-paclitaxel in patients with anthracycline-resistant, stage I-III TNBC.
Methods
Eligibility
Patients who were at least 18 years old were eligible for the study if they had histologically confirmed stage I-III TNBC and were planned to receive neoadjuvant chemotherapy. TNBC was defined as breast cancers with < 10% estrogen receptor (ER) and progesterone receptor (PR) staining of invasive tumor cells by immunohistochemistry (IHC) that was also negative for the human epidermal growth factor receptor 2 (HER2) according to HER2 testing guidelines from the American Society of Clinical Oncology/College of American Pathologists [20]. The primary tumor or a histologically confirmed regional nodal metastases had to be at least 1.5 cm on mammography, ultrasound, or MRI.
Patients had to have received neoadjuvant doxorubicin and cyclophosphamide (AC), with or without 5-fluorouracil (5-FU), with radiographic evidence of anthracycline resistance, defined as disease progression during AC or a < 80% decrease in the calculated volume of the index lesion by ultrasound after 4 cycles of AC. Other than the anthracycline and cyclophosphamide chemotherapy, with or without 5-FU, no other prior treatment for breast cancer was allowed. Patients were required to have an Eastern Cooperative Oncology Group (ECOG) performance status of 1 or better, as well as adequate organ and marrow function. Patients were excluded if they had a history of autoimmune disease, were known to be human immunodeficiency virus (HIV) positive, had a prior history of allogeneic or solid organ transplants, received immunostimulatory agents within 4 weeks of enrollment, or received systemic immunosuppressants (including corticosteroids) within 1 week of enrollment.
The protocol was reviewed by The University of Texas MD Anderson Cancer Center (MD Anderson) Institutional Review Board and all patients provided written informed consent to take part in the study.
Study design and treatment
The primary objective of this study was to evaluate the efficacy of the combination of atezolizumab and nab-paclitaxel in patients with AC-resistant stage I-III TNBC, defined as the rate of pCR/residual cancer burden class I (RCB-I) disease. Atezolizumab was administered intravenously (IV) at a dose of 1200 mg every 3 weeks for 12 weeks (4 cycles). Nab-paclitaxel was administered in parallel at a dose of 100 mg/m2 IV once a week for 12 weeks. After 12 weeks of therapy, patients underwent definitive surgical resection. Within 4 weeks of surgery, patients initiated atezolizumab 1200 mg IV every 3 weeks for another 12 weeks (4 cycles) as adjuvant therapy.
Evaluations performed before and during treatment included a complete medical history, physical examinations, hematologic and metabolic profiles, relevant imaging studies, and toxicity assessments. Patients remained on study until radiologic evidence of disease progression, unacceptable toxicity, or withdrawal of consent.
Safety monitoring and dose modification guidelines
Patients were evaluated for toxicity while on study through the monitoring of all serious and non-serious adverse events, defined and graded according to the National Cancer Institute’s Common Terminology Criteria for Adverse Events (NCI CTCAE), version 4.0. Patients were followed for safety for 30 days following the last dose of study treatment or until receipt of another cancer-directed therapy, whichever occurred first.
Immune-related adverse events (irAEs) were managed at the discretion of the treating oncologist in the context of the nature of the toxicity and degree of clinical benefit to the patient, with prespecified guidelines to aid clinical decision making. Specifically, grade 1–2 irAEs were primarily managed with supportive and symptomatic care without dose interruptions. Grade 3 or higher irAEs were managed by holding atezolizumab and administering systemic steroids. Recurrent grade 2 irAEs were managed by holding atezolizumab and/or administering systemic steroids.
Grade 4 neutropenia lasting 1 week or longer was managed by a dose interruption followed by a dose reduction of nab-paclitaxel to 75 mg/m2 IV once weekly for subsequent cycles. Grade 3 or greater sensory neuropathy was also managed by a dose interruption of nab-paclitaxel followed by a dose reduction to 75 mg/m2 IV once weekly after resolution to grade 2 or less. Grade 3 hepatic toxicity was managed by a dose interruption of nab-paclitaxel followed by a dose reduction to 75 mg/m2 IV once weekly after resolution to grade 1 or less. Nab-paclitaxel was permanently discontinued in patients with grade 4 hepatic toxicity. Additional dose reductions of nab-paclitaxel to 50 mg/m2 IV once weekly for recurrent grade 3 toxicities were allowed at the discretion of the treating oncologist.
Disease monitoring
All patients enrolled in this study were evaluated for disease progression by physical examination and/or imaging at the discretion of the treating oncologist. Study therapy was discontinued in patients with evidence of disease progression. Upon early discontinuation of therapy or completion of 12 weeks of study therapy, patients underwent surgical resection. Pathological response was determined using the residual cancer burden (RCB) index [21], with pCR defined as the absence of residual invasive cancer on hematoxylin and eosin (H&E) evaluation of the complete resected breast specimen and all sampled regional lymph nodes following completion of neoadjuvant systemic therapy (ypT0/Tis ypN0). Patients experiencing disease progression during neoadjuvant therapy to such an extent that precluded definitive surgical resection were classified as having RCB-III disease.
Stromal tumor-infiltrating lymphocyte assessment and immunohistochemistry
Pre-treatment tumor tissue obtained prior to initiation of AC was used for stromal tumor-infiltrating lymphocyte (TIL) assessment and immunohistochemistry (IHC). The percentage of stromal TIL was determined on H&E-stained slides according to standard methods established by the International TILs Working Group [22]. High TIL tumors were defined as tumors with stromal TIL infiltration of ≥ 20% [23]. IHC staining for Ki67 (clone MIB-1, Dako; 1:100) and androgen receptor (AR, clone AR441, Dako; 1:30) were performed on unstained 4-µm thick tissue sections that had been prepared from a representative core biopsy paraffin block of the original untreated tumor as previously described [24]. PD-L1 expression was assessed using the PD-L1 IHC 22C3 pharmDx kit (Dako) on the Dako Autostainer Link, as previously described [24]. PD-L1 positivity was defined as a combined positive score (CPS) [25] of at least 1. At the time of study activation, thresholds for PD-L1 positivity in TNBC using the SP142 assay were not yet established. Upon study completion we additionally performed PD-L1 IHC using the Ventana SP142 assay kit (Roche Diagnostics) on the Ventana BenchMark Ultra, according to the manufacturers’ instructions. Slides were counterstained with Mayer’s hematoxylin and results were evaluated with known positive and negative tissue controls. The percentage of PD-L1 expression in tumor-infiltrating immune cells was assessed as the proportion of tumor area occupied by PD-L1-positive immune cells of any intensity in any cell compartment [1]. Stromal TIL and IHC stains were evaluated by dedicated breast pathologists (L.H., Q.Q.D.).
Statistical methods
The planned enrollment for this study was 37 patients. A two-stage Gehan design was employed and 19 patients were enrolled in the first stage. If at least one of the first 19 patients experienced a favorable response, defined as a pathological response of pCR or RCB-I, enrollment was to continue for another 18 patients (total n = 37). This design provided a 38%, 14%, 5%, and 1% probability of termination after the first stage if the true response rate was 5%, 10%, 15%, and 20%, respectively. At the maximum enrollment of 37 patients, the exact 95% confidence interval (CI) for a response rate of 15% would extend from 5 to 31%. Associations between clinicopathological characteristics and pathological response were examined using logistic regression models. All reported p values were two sided and those less than 0.05 were considered statistically significant.
Results
Patients
Between 2/15/2016 and 1/29/2021, a total of 37 female patients with anthracycline-resistant TNBC were enrolled and treated at MD Anderson. The baseline clinical characteristics of patients as well as pathological features of their tumors are summarized in Table 1. The median age at diagnosis was 53.8 years (range 27.3–74.9). Twenty-seven (23%) patients had node-positive disease at the time of diagnosis. Twelve patients (32%) had tumors with high TIL infiltration (≥ 20% stromal TIL) and 21 patients (57%) had PD-L1 positive (CPS ≥ 1) tumors. All patients received neoadjuvant doxorubicin and cyclophosphamide (AC) prior to enrollment on this study. Thirty-four patients (92%) received four cycles of AC prior to enrollment on this study, one patient (3%) received three cycles, and two patients (5%) received two cycles. Figure 1 summarizes the volumetric change in tumor size by ultrasound to AC and the total number of cycles of AC received by each patient. Thirteen patients (35%) had evidence of increase in tumor volume by ultrasound after completion of AC (Fig. 1). One patient was enrolled on the study despite experiencing an 81% decrease in tumor volume by ultrasound after 4 cycles of AC at the discretion of the treating oncologist after discussion with the Principal Investigator due to substantial disease burden by physical examination, suggesting a low likelihood of pCR with standard taxane-based therapy.
Response to doxorubicin and cyclophosphamide (AC). Waterfall plot summarizing the percent volumetric change to initial AC chemotherapy prior to study enrollment. The asterix identifies a patient who experienced a 19,489% increase in tumor volume after 4 cycles of AC. Colors represent the total number of cycles of AC received prior to enrollment (red = 2; gray = 3; blue = 4) and the dashed line indicates an 80% decrease in calculated tumor volume. AC = doxorubicin plus cyclophosphamide
Efficacy
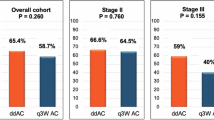
Thirty-two patients underwent an optional breast ultrasound after the last dose of neoadjuvant atezolizumab and nab-paclitaxel (end of treatment). Figures 2A–C summarize the kinetics of tumor response by ultrasound. Of the thirteen patients who had evidence of increase in tumor volume by ultrasound after completion of AC, nine experienced a decrease in tumor volume with atezolizumab and nab-paclitaxel, two experienced a further increase in tumor volume with atezolizumab and nab-paclitaxel, and the remaining two did not have an end of treatment ultrasound performed (Fig. 2A–B). Among the 13 patients with evidence of increase in tumor volume after AC, three (23%) experienced a pCR (Fig. 2B), five were found to have RCB-II disease (38%), and five were found to have RCB-III disease (38%) following treatment with atezolizumab and nab-paclitaxel. Of the 24 patients who had evidence of decrease in tumor volume by ultrasound after completion of AC, 20 patients experienced a further decrease in tumor volume with atezolizumab and nab-paclitaxel, one patient experienced an increase in tumor volume with atezolizumab and nab-paclitaxel, and the remaining three patients did not have an end of treatment ultrasound performed (Fig. 2C). Of the 37 patients enrolled, 12 (32%, 95% confidence interval [CI]: 18–50%) experienced a pCR, 5 (14%, 95% CI: 5–29%) had RCB-I, 12 (32%, 95% CI: 18–50%) had RCB-II, and 8 (22%, 95% CI: 10–38%) had RCB-III disease (Fig. 2D). We examined associations between baseline clinicopathological characteristics and pathological response after neoadjuvant therapy and found that only higher age at diagnosis (odds ratio [OR]: 2.01 per 10 years; 95% CI: 1.04–3.88, p = 0.039) and high stromal TIL (OR: 5.6; 95% CI: 1.24–25.33; p = 0.025) were significantly associated with higher odds of pCR (Fig. 3). Of note, PD-L1 positivity (22C3, CPS ≥ 1) was not significantly associated with higher odds of pCR (OR: 1.85; 95% CI: 0.44–7.74; p = 0.40, Fig. 3, Supplementary Table 1) and while using CPS ≥ 10 as the definition of PD-L1 positivity resulted in a numerically higher odds ratio, this association was not statistically significant (OR: 3.17; 95% CI: 0.74–13.59; p = 0.12, Supplementary Table 1). To comprehensively assess the role of PD-L1 expression on pathological response in this study, we retrospectively performed PD-L1 IHC using the SP142 assay and found no statistically significant associations with pathological response (OR: 4.44, 95% CI: 0.35–55.5; p = 0.25, Supplementary Table 1).
Volumetric changes in tumor size during neoadjuvant therapy and pathological response following completion of neoadjuvant therapy. (A–C) Spider plots summarizing changes in tumor volume as assessed by ultrasonography before initiation of neoadjuvant therapy (pre-treatment), after completion of initial standard chemotherapy with doxorubicin and cyclophosphamide and prior to initiation of study treatment (post-AC) and after completion of all neoadjuvant therapy (end of treatment) in a single patient with significant progression (A), patients who experienced increase in tumor volume after completion of AC (B), and patients who experienced a decrease in tumor volume, albeit suboptimal, after completion of AC (C). All percentages are relative to pre-treatment measurements. Solid circles in the post-AC time point for Figs. 2A–C indicate patients who did not have an end of treatment ultrasound performed prior to surgery. Line colors represent pathological response to neoadjuvant therapy (green = pCR; red = non-pCR). (D) Pie chart summarizing the pathological responses observed following completion of neoadjuvant therapy on this study
Toxicity
All 37 patients received at least one dose of atezolizumab and nab-paclitaxel and were evaluable for toxicity. Severe (grade 3 or greater) or frequent (> 5%, any grade) treatment-related adverse events are summarized in Table 2. Two patients (5.4%) experienced grade 4 increases in serum creatinine and one patient (2.7%) experienced grade 4 neutropenia. The most common grade 3 toxicities were neutropenia in 5 patients (13.5%) and increase in alanine aminotransferase in 3 patients (8.1%). Immune-related adverse events (irAEs) led to discontinuation of atezolizumab in 7 patients (18.9%) (Table 3).
Exposure to atezolizumab
Twenty-three patients (62%) received all eight doses of atezolizumab per protocol. Of the 14 patients who did not receive all eight doses of atezolizumab, eight patients discontinued atezolizumab during the neoadjuvant phase. Among these 8 patients, the reasons for discontinuation were disease progression in one patient, interstitial nephritis in two patients, autoimmune hepatitis in two patients, muscle weakness in one patient, neuropathy in one patient, and patient preference in one patient. The remaining six patients discontinued atezolizumab in the adjuvant phase of the protocol. Reasons for discontinuation during the adjuvant phase were disease recurrence in three patients, autoimmune hepatitis and thyroiditis in one patient, adrenal insufficiency in one patient, and patient preference in one patient.
Exposure to nab-paclitaxel
Twenty patients (54%) received a total of 1200 mg/m2 of nab-paclitaxel during the neoadjuvant phase of the study per protocol. Reasons for dose reduction/early discontinuation of nab-paclitaxel in the remaining 17 patients were disease progression in one patient, neuropathy in five patients, elevated liver enzymes and hepatitis in four patients, neutropenia in two patients, myalgias in one patient, interstitial nephritis in one patient, and patient preference/physician discretion in three patients.
Discussion
Here, we report the first study investigating the use of atezolizumab in combination with nab-paclitaxel in patients with AC-resistant TNBC. In the present study, the combination of atezolizumab and nab-paclitaxel was well tolerated and demonstrated promising signals of clinical efficacy in patients with AC-resistant TNBC, supporting the use of a response-adapted approach for anti-PD-(L)1 therapy in the neoadjuvant setting. Although anti-PD-1 therapy is now FDA approved in combination with chemotherapy as neoadjuvant therapy for patients with high-risk, early-stage, TNBC, the potential for long-term morbidity from irAEs is an important clinical consideration in the curative neoadjuvant setting. In the absence of a predictive biomarker to identify patients who might derive benefit from the addition of neoadjuvant anti-PD-(L)1 therapy to chemotherapy, a response-adapted approach such as that presented in this study may widen the therapeutic window for anti-PD-(L)1 therapy, especially in patients who may be at higher risk for irAEs. Of note, an exploratory analysis of event-free survival by residual cancer burden in patients treated on the KEYNOTE-522 trial demonstrated that the greatest improvement in event-free survival attributable to the addition of anti-PD-1 therapy were among patients with RCB-II disease [26], further suggesting that early identification of patients with chemotherapy-resistant TNBC may be a viable strategy to select patients most likely to benefit from the addition of anti-PD-(L)1 therapy in the neoadjuvant setting. Further, our study is one of three reported neoadjuvant clinical trials for patients with TNBC where anti-PD-(L)1 therapy was not used in combination with anthracycline-based chemotherapy, contributing to our understanding of the optimal clinical setting for employing anti-PD-(L)1 therapy in patients with early-stage TNBC.
In the overall study population, we observed a pCR rate of 32%. Although this is lower compared to the pCR rate observed in the atezolizumab arm of IMpassion031 (pCR = 58% in atezolizumab arm) [6] where patients received atezolizumab in combination with nab-paclitaxel followed by AC as neoadjuvant treatment, the NeoTRIP study (pCR = 49% in atezolizumab arm) [27] where patients received neoadjuvant atezolizumab in combination with nab-paclitaxel and carboplatin, and the single-arm NeoPACT study (pCR = 58%) [28] where patients received neoadjuvant pembrolizumab and carboplatin plus docetaxel, it is important to note that unlike IMpassion031, NeoTRIP, and NeoPACT, our study was designed specifically for patients with chemotherapy-resistant TNBC, where a pCR rate of 32% and a pCR/RCB-I rate of 46% is significantly higher than the previously reported rate of 2–5% [15, 16]. Treatment-related adverse events observed on this study were generally similar to that reported in prior studies of atezolizumab and nab-paclitaxel [6]. Of note, 7 patients experienced irAEs leading to early discontinuation of atezolizumab. Of note, this single-arm phase II study was part of the larger ARTEMIS trial (NCT02276443) where patients with AC-resistant TNBC were preferentially enrolled on specific clinical trials based on the pathological and/or molecular characteristics of the tumor. Based on the trial allocation algorithm of ARTEMIS, patients with PD-L1 positive tumors were preferentially enrolled on this study, resulting in an enrichment of patients with PD-L1 positive tumors.
There is growing recognition of the importance of anthracyclines in facilitating responses to anti-PD-(L)1 therapy in TNBC. First, data from the TONIC study demonstrated that compared with cisplatin and cyclophosphamide, induction with doxorubicin led to higher rates of response to anti-PD-1 therapy in patients with metastatic TNBC [29]. Second, although not the primary endpoint of the trial, the addition of atezolizumab to a non-anthracycline chemotherapy backbone did not significantly increase the pCR rate in the NeoTRIP study [27]. These data suggest that anthracyclines play an important role in determining response to anti-PD-(L)1 therapy. However, because anthracyclines are known to augment antitumor immunity both indirectly through immunogenic cell death and directly by altering the immune cell composition in the microenvironment, whether tumor cell resistance to anthracyclines limits clinical benefit from anti-PD-(L)1 therapy through a lack of immunogenic cell death remains controversial. In this study, we demonstrate that patients with AC-resistant TNBC derive clinical benefit from the combination of atezolizumab and nab-paclitaxel, suggesting that direct effects of anthracycline-based chemotherapy on the tumor-immune microenvironment are critical in promoting response to anti-PD-(L)1 therapy in the setting of resistance to AC. We further identified higher age and higher stromal TIL as clinicopathological features that significantly associate with pCR to atezolizumab plus nab-paclitaxel in patients with AC-resistant TNBC. Collectively, these data suggest that anthracycline resistance does not abrogate clinical benefit from anti-PD-(L)1 therapy and clinicopathological factors may aid in patient selection to maximize therapeutic benefits of anti-PD-(L)1 agents in the curative neoadjuvant setting for patients with TNBC.
In addition to our focus on patients with chemotherapy-resistant TNBC, another strength of our study is the inclusion of patients with clinical N3 node-positive disease who were excluded from the KEYNOTE-522 study [5] but formed 32% of our study population. Notably, the pCR rate among the 12 patients with clinical N3 node-positive disease was aligned with the pCR rate in our overall study population, suggesting that patients with clinical N3 disease may derive clinical benefit from neoadjuvant anti-PD-(L)1 therapy.
One limitation of our study is the lack of a contemporaneous control arm of patients with chemotherapy-resistant TNBC treated with nab-paclitaxel alone which precludes definite conclusions on the role of atezolizumab in this setting. However, to the best of our knowledge, this is the first reported study evaluating immune checkpoint blockade in combination with chemotherapy specifically in patients with AC-resistant TNBC and the encouraging signal of activity should inform the design of future studies. Another limitation of our study is the use of nab-paclitaxel in taxane-naïve patients which may present a real-world barrier to this approach with the currently available data. However, data in the metastatic setting showing that combining atezolizumab with paclitaxel does not improve PFS and OS versus paclitaxel alone suggest that nab-paclitaxel may be the superior chemotherapy backbone when used in combination with atezolizumab. Thus, until additional translational data which could help elucidate the reasons behind the lack of efficacy when atezolizumab is combined with paclitaxel in metastatic TNBC, future studies involving atezolizumab should consider using nab-paclitaxel as the preferred chemotherapy backbone.
In conclusion, the combination of atezolizumab and nab-paclitaxel has demonstrated promising signals of activity in patients with AC-resistant TNBC and suggests that a response-adapted approach to the use of immune checkpoint blockade may be a viable strategy to widen the therapeutic window for patients with TNBC in the curative neoadjuvant setting, and should be considered for further evaluation in a randomized clinical trial.
Data availability
For eligible studies, qualified researchers may request access to individual patient level clinical data from the corresponding author. Anonymized records for individual patients across more than one data source cannot, and should not, be linked due to a potential increase in risk of patient re-identification.
References
Schmid P, Adams S, Rugo HS, Schneeweiss A, Barrios CH, Iwata H, Dieras V, Hegg R, Im SA, Shaw Wright G, Henschel V, Molinero L, Chui SY, Funke R, Husain A, Winer EP, Loi S, Emens LA, Investigators IMT (2018) Atezolizumab and Nab-paclitaxel in advanced triple-negative breast cancer. N Engl J Med 379(22):2108–2121. https://doi.org/10.1056/NEJMoa1809615
Cortes J, Cescon DW, Rugo HS, Nowecki Z, Im SA, Yusof MM, Gallardo C, Lipatov O, Barrios CH, Holgado E, Iwata H, Masuda N, Otero MT, Gokmen E, Loi S, Guo Z, Zhao J, Aktan G, Karantza V, Schmid P, Investigators K (2020) Pembrolizumab plus chemotherapy versus placebo plus chemotherapy for previously untreated locally recurrent inoperable or metastatic triple-negative breast cancer (KEYNOTE-355): a randomised, placebo-controlled, double-blind, phase 3 clinical trial. Lancet 396(10265):1817–1828. https://doi.org/10.1016/S0140-6736(20)32531-9
Schmid P, Rugo HS, Adams S, Schneeweiss A, Barrios CH, Iwata H, Dieras V, Henschel V, Molinero L, Chui SY, Maiya V, Husain A, Winer EP, Loi S, Emens LA, Investigators IM (2020) Atezolizumab plus nab-paclitaxel as first-line treatment for unresectable, locally advanced or metastatic triple-negative breast cancer (IMpassion130): updated efficacy results from a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol 21(1):44–59. https://doi.org/10.1016/S1470-2045(19)30689-8
Emens LA, Adams S, Barrios CH, Dieras V, Iwata H, Loi S, Rugo HS, Schneeweiss A, Winer EP, Patel S, Henschel V, Swat A, Kaul M, Molinero L, Patel S, Chui SY, Schmid P (2021) First-line atezolizumab plus nab-paclitaxel for unresectable, locally advanced, or metastatic triple-negative breast cancer: impassion130 final overall survival analysis. Ann Oncol 32(8):983–993. https://doi.org/10.1016/j.annonc.2021.05.355
Schmid P, Cortes J, Pusztai L, McArthur H, Kummel S, Bergh J, Denkert C, Park YH, Hui R, Harbeck N, Takahashi M, Foukakis T, Fasching PA, Cardoso F, Untch M, Jia L, Karantza V, Zhao J, Aktan G, Dent R, O’Shaughnessy J, Investigators K (2020) Pembrolizumab for early triple-negative breast cancer. N Engl J Med 382(9):810–821. https://doi.org/10.1056/NEJMoa1910549
Mittendorf EA, Zhang H, Barrios CH, Saji S, Jung KH, Hegg R, Koehler A, Sohn J, Iwata H, Telli ML, Ferrario C, Punie K, Penault-Llorca F, Patel S, Duc AN, Liste-Hermoso M, Maiya V, Molinero L, Chui SY, Harbeck N (2020) Neoadjuvant atezolizumab in combination with sequential nab-paclitaxel and anthracycline-based chemotherapy versus placebo and chemotherapy in patients with early-stage triple-negative breast cancer (IMpassion031): a randomised, double-blind, phase 3 trial. Lancet 396(10257):1090–1100. https://doi.org/10.1016/S0140-6736(20)31953-X
Schmid P, Cortes J, Dent R, Pusztai L, McArthur H, Kümmel S, Bergh J, Denkert C, Park YH, Hui R, Harbeck N, Takahashi M, Untch M, Fasching PA, Cardoso F, Ding Y, Tryfonidis K, Aktan G, Karantza V, O’Shaughnessy J (2021) VP7-2021: KEYNOTE-522: Phase III study of neoadjuvant pembrolizumab + chemotherapy vs. placebo + chemotherapy, followed by adjuvant pembrolizumab vs. placebo for early-stage TNBC. Ann Oncol 32(9):1198–1200. https://doi.org/10.1016/j.annonc.2021.06.014
Nanda R, Chow LQ, Dees EC, Berger R, Gupta S, Geva R, Pusztai L, Pathiraja K, Aktan G, Cheng JD, Karantza V, Buisseret L (2016) Pembrolizumab in patients with advanced triple-negative breast cancer: phase Ib KEYNOTE-012 study. J Clin Oncol 34(21):2460–2467. https://doi.org/10.1200/JCO.2015.64.8931
van der Most RG, Currie AJ, Cleaver AL, Salmons J, Nowak AK, Mahendran S, Larma I, Prosser A, Robinson BW, Smyth MJ, Scalzo AA, Degli-Esposti MA, Lake RA (2009) Cyclophosphamide chemotherapy sensitizes tumor cells to TRAIL-dependent CD8 T cell-mediated immune attack resulting in suppression of tumor growth. PLoS ONE. https://doi.org/10.1371/journal.pone.0006982
Ramakrishnan R, Assudani D, Nagaraj S, Hunter T, Cho HI, Antonia S, Altiok S, Celis E, Gabrilovich DI (2010) Chemotherapy enhances tumor cell susceptibility to CTL-mediated killing during cancer immunotherapy in mice. J Clin Invest 120(4):1111–1124. https://doi.org/10.1172/JCI40269
Zitvogel L, Kepp O, Senovilla L, Menger L, Chaput N, Kroemer G (2010) Immunogenic tumor cell death for optimal anticancer therapy: the calreticulin exposure pathway. Clin Cancer Res 16(12):3100–3104. https://doi.org/10.1158/1078-0432.CCR-09-2891
Kaneno R, Shurin GV, Kaneno FM, Naiditch H, Luo J, Shurin MR (2011) Chemotherapeutic agents in low noncytotoxic concentrations increase immunogenicity of human colon cancer cells. Cell Oncol (Dordr) 34(2):97–106. https://doi.org/10.1007/s13402-010-0005-5
Ghebeh H, Lehe C, Barhoush E, Al-Romaih K, Tulbah A, Al-Alwan M, Hendrayani SF, Manogaran P, Alaiya A, Al-Tweigeri T, Aboussekhra A, Dermime S (2010) Doxorubicin downregulates cell surface B7–H1 expression and upregulates its nuclear expression in breast cancer cells: role of B7–H1 as an anti-apoptotic molecule. Breast Cancer Res 12(4):R48. https://doi.org/10.1186/bcr2605
Fucikova J, Kralikova P, Fialova A, Brtnicky T, Rob L, Bartunkova J, Spisek R (2011) Human tumor cells killed by anthracyclines induce a tumor-specific immune response. Cancer Res 71(14):4821–4833. https://doi.org/10.1158/0008-5472.CAN-11-0950
von Minckwitz G, Kummel S, Vogel P, Hanusch C, Eidtmann H, Hilfrich J, Gerber B, Huober J, Costa SD, Jackisch C, Loibl S, Mehta K, Kaufmann M, German Breast G (2008) Neoadjuvant vinorelbine-capecitabine versus docetaxel-doxorubicin-cyclophosphamide in early nonresponsive breast cancer: phase III randomized GeparTrio trial. J Natl Cancer Inst 100(8):542–551. https://doi.org/10.1093/jnci/djn085
Smith IC, Heys SD, Hutcheon AW, Miller ID, Payne S, Gilbert FJ, Ah-See AK, Eremin O, Walker LG, Sarkar TK, Eggleton SP, Ogston KN (2002) Neoadjuvant chemotherapy in breast cancer: significantly enhanced response with docetaxel. J Clin Oncol 20(6):1456–1466. https://doi.org/10.1200/JCO.2002.20.6.1456
Alizadeh D, Trad M, Hanke NT, Larmonier CB, Janikashvili N, Bonnotte B, Katsanis E, Larmonier N (2014) Doxorubicin eliminates myeloid-derived suppressor cells and enhances the efficacy of adoptive T-cell transfer in breast cancer. Cancer Res 74(1):104–118. https://doi.org/10.1158/0008-5472.CAN-13-1545
Carson WE 3rd, Shapiro CL, Crespin TR, Thornton LM, Andersen BL (2004) Cellular immunity in breast cancer patients completing taxane treatment. Clin Cancer Res 10(10):3401–3409. https://doi.org/10.1158/1078-0432.CCR-1016-03
Emens LA, Cruz C, Eder JP, Braiteh F, Chung C, Tolaney SM, Kuter I, Nanda R, Cassier PA, Delord JP, Gordon MS, ElGabry E, Chang CW, Sarkar I, Grossman W, O’Hear C, Fasso M, Molinero L, Schmid P (2019) Long-term clinical outcomes and biomarker analyses of atezolizumab therapy for patients with metastatic triple-negative breast cancer: a phase 1 study. JAMA Oncol 5(1):74–82. https://doi.org/10.1001/jamaoncol.2018.4224
Wolff AC, Hammond ME, Hicks DG, Dowsett M, McShane LM, Allison KH, Allred DC, Bartlett JM, Bilous M, Fitzgibbons P, Hanna W, Jenkins RB, Mangu PB, Paik S, Perez EA, Press MF, Spears PA, Vance GH, Viale G, Hayes DF, American Society of Clinical O, College of American P (2013) Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American society of clinical oncology/college of american pathologists clinical practice guideline update. J Clin Oncol 31(31):3997–4013. https://doi.org/10.1200/JCO.2013.50.9984
Symmans WF, Peintinger F, Hatzis C, Rajan R, Kuerer H, Valero V, Assad L, Poniecka A, Hennessy B, Green M, Buzdar AU, Singletary SE, Hortobagyi GN, Pusztai L (2007) Measurement of residual breast cancer burden to predict survival after neoadjuvant chemotherapy. J Clin Oncol 25(28):4414–4422. https://doi.org/10.1200/JCO.2007.10.6823
Salgado R, Denkert C, Demaria S, Sirtaine N, Klauschen F, Pruneri G, Wienert S, Van den Eynden G, Baehner FL, Penault-Llorca F, Perez EA, Thompson EA, Symmans WF, Richardson AL, Brock J, Criscitiello C, Bailey H, Ignatiadis M, Floris G, Sparano J, Kos Z, Nielsen T, Rimm DL, Allison KH, Reis-Filho JS, Loibl S, Sotiriou C, Viale G, Badve S, Adams S, Willard-Gallo K, Loi S, International TWG (2015) The evaluation of tumor-infiltrating lymphocytes (TILs) in breast cancer: recommendations by an international TILs working group 2014. Ann Oncol 26(2):259–271. https://doi.org/10.1093/annonc/mdu450
Abuhadra N, Sun R, Litton JK, Rauch GM, Yam C, Chang JT, Seth S, Bassett R Jr, Lim B, Thompson AM, Mittendorf E, Adrada BE, Damodaran S, White J, Ravenberg E, Candelaria R, Arun B, Ueno NT, Santiago L, Saleem S, Abouharb S, Murthy RK, Ibrahim N, Sahin AA, Valero V, Symmans WF, Tripathy D, Moulder S, Huo L (2022) Prognostic impact of high baseline stromal tumor-infiltrating lymphocytes in the absence of pathologic complete response in early-stage triple-negative breast cancer. Cancers (Basel). https://doi.org/10.3390/cancers14051323
Yam C, Alatrash G, Yen E-Y, Garber H, Philips AV, Huo L, Yang F, Bassett RL, Sun X, Cuentas ERP, Symmans WF, Seth S, White JB, Rauch GM, Damodaran S, Litton JK, Wargo JA, Hortobagyi GN, Moulder SL, Mittendorf EA (2020) Immune phenotype and response to neoadjuvant systemic therapy (NAST) in triple negative breast cancer (TNBC). J Clin Oncol. https://doi.org/10.1200/JCO.2020.38.15_suppl.509
Kulangara K, Hanks DA, Waldroup S, Peltz L, Shah S, Roach C, Juco JW, Emancipator K, Stanforth D (2017) Development of the combined positive score (CPS) for the evaluation of PD-L1 in solid tumors with the immunohistochemistry assay PD-L1 IHC 22C3 pharmDx. J Clin Oncol. https://doi.org/10.1200/JCO.2017.35.15_suppl.e14589
Pusztai L, Denkert C, O’Shaughnessy J, Cortes J, Dent RA, McArthur HL, Kuemmel S, Bergh JCS, Park YH, Hui R, Harbeck N, Takahashi M, Untch M, Fasching PA, Cardoso F, Zhu Y, Pan W, Tryfonidis K, Schmid P (2022) Event-free survival by residual cancer burden after neoadjuvant pembrolizumab + chemotherapy versus placebo + chemotherapy for early TNBC: exploratory analysis from KEYNOTE-522. J Clin Oncol. https://doi.org/10.1200/JCO.2022.40.16_suppl.503
Gianni L, Huang CS, Egle D, Bermejo B, Zamagni C, Thill M, Anton A, Zambelli S, Bianchini G, Russo S, Ciruelos EM, Greil R, Semiglazov V, Colleoni M, Kelly C, Mariani G, Del Mastro L, Maffeis I, Valagussa P, Viale G (2022) Pathologic complete response (pCR) to neoadjuvant treatment with or without atezolizumab in triple-negative, early high-risk and locally advanced breast cancer: NeoTRIP Michelangelo randomized study. Ann Oncol. https://doi.org/10.1016/j.annonc.2022.02.004
Sharma P, Stecklein SR, Yoder R, Staley JM, Schwensen K, O’Dea A, Nye LE, Elia M, Satelli D, Crane G, Madan R, O’Neil MF, Wagner JL, Larson KE, Balanoff C, Phadnis MA, Godwin AK, Salgado R, Khan QJ, O’Shaughnessy J (2022) Clinical and biomarker results of neoadjuvant phase II study of pembrolizumab and carboplatin plus docetaxel in triple-negative breast cancer (TNBC) (NeoPACT). J Clin Oncol. https://doi.org/10.1200/JCO.2022.40.16_suppl.513
Voorwerk L, Slagter M, Horlings HM, Sikorska K, van de Vijver KK, de Maaker M, Nederlof I, Kluin RJC, Warren S, Ong S, Wiersma TG, Russell NS, Lalezari F, Schouten PC, Bakker NAM, Ketelaars SLC, Peters D, Lange CAH, van Werkhoven E, van Tinteren H, Mandjes IAM, Kemper I, Onderwater S, Chalabi M, Wilgenhof S, Haanen J, Salgado R, de Visser KE, Sonke GS, Wessels LFA, Linn SC, Schumacher TN, Blank CU, Kok M (2019) Immune induction strategies in metastatic triple-negative breast cancer to enhance the sensitivity to PD-1 blockade: the TONIC trial. Nat Med 25(6):920–928. https://doi.org/10.1038/s41591-019-0432-4
Funding
This study was funded in part by Genentech, USA Inc., generous philanthropic contributions to The University of Texas MD Anderson Cancer Center Moon Shots Program, a Conquer Cancer Career Development Award supported by Fleur Fairman (to C.Y.) and philanthropic support from the Still Water Foundation (to D.T.). Dr. Yam was additionally supported by the 2018 Gianni Bonadonna Breast Cancer Research Fellowship (Conquer Cancer Foundation), the Allison and Brian Grove Endowed Fellowship for Breast Medical Oncology and the Susan Papizan Dolan Fellowship in Breast Oncology. Any opinions, findings, and conclusions expressed in this material are those of the author(s) and do not necessarily reflect those of the sponsors.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
C.Y. has received research funding (to the institution) from Genentech, Gilead, BostonGene, Sanofi, Amgen, Pfizer, Astellas, Novartis and has served on advisory boards for Gilead. E.A.M. has received research support from Roche/Genentech (via the SU2C grant), and Gilead, has served on steering committees for Bristol Myers Squib, Lilly, Roche/Genentech, and has served on scientific advisory boards for AstraZeneca, Exact Sciences (formerly Genomic Health), Merck, Roche/Genentech. R.K.M. has received honoraria from Puma biotechnology, Seattle genetics, Genetech, Novartis, and Astrazeneca; has served in a consulting or advisory role for Sanofi, Novartis, AstraZeneca, Pfizer, Genentech/Roche, Seattle Genetics, Puma Biotechnology; has received research funding (to the institution) from Seattle Genetics, Genetch/Roche, Pfizer, Daiichi Sankyo, AstraZeneca, EMD Serono; has received travel, accommodations, expenses from Genentech, Seattle Genetics. E.A.R. is currently employed at Eli Lilly (previously employed by MD Anderson at the time the study was conducted). W.F.S. is a co-inventor/patent of US Patent No. 11,459,617 “Targeted measure of transcriptional activity related to hormone receptors” issued on 10/4/2022 (applicant proprietor: University of Texas MD Anderson Cancer Center. Licensed to Delphi Diagnostics, Inc. and has co-founder equity from Delphi Diagnostics, Inc. A.T. is related by marriage to an employee of Eli Lilly. D.T. has received research support (to the institution) from Novartis, Pfizer, Polyphor and has served as a consultant to AstraZeneca, Glaxosmithkline, Gilead, Oncopep, Pfizer, Novartis, AMBRX, Personalis, Sermonix, Stemline-Menarini, Puma Biotechnology. S.L.M. is currently employed by Eli Lilly (previously employed by MD Anderson at the time the study was conducted). J.K.L. has received grant or research support from Novartis, Medivation/Pfizer, Genentech, GSK, EMD-Serono, AstraZeneca, Medimmune, Zenith, Jounce; participated in Speaker’s Bureau for MedLearning, Physician’s Education Resource, Prime Oncology, Medscape, Clinical Care Options; received honoraria from UpToDate; served on advisory committees or review panels for AstraZeneca, Ayala, Pfizer (all uncompensated), NCCN, ASCO, NIH, PDQ, SITC Breast Committee, SWOG Breast Committee. All other authors declare that they have no relevant conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These data were presented in part at the ESMO 2018 Congress and the 2021 ASCO Annual Meeting.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yam, C., Mittendorf, E.A., Garber, H.R. et al. A phase II study of neoadjuvant atezolizumab and nab-paclitaxel in patients with anthracycline-resistant early-stage triple-negative breast cancer. Breast Cancer Res Treat 199, 457–469 (2023). https://doi.org/10.1007/s10549-023-06929-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-023-06929-9