Abstract
Purpose
Whether peripheral immune cell subsets can predict pathological complete response (pCR) in breast cancer patients remains to be elucidated. We aimed to dissect the relationship between peripheral immune cell subsets and pCR.
Methods
Two hundred and twenty-six eligible patients from two prospective clinical trials (SHPD001 and SHPD002) in China were randomly divided into a training cohort and a validation cohort. The breast cancer subtypes in this study included hormone receptor (HR)-positive/human epidermal growth factor receptor 2 (HER2)-negative (n = 95), HER2-positive (n = 100), and triple negative (n = 31) breast cancer. We defined the “Neo-Peripheral Adaptive Immune Score” for neoadjuvant chemotherapy (neoPAI Score) based on the percentages of CD4 + T cells, CD8 + T cells, B cells, and the CD4 + /CD8 + ratio in peripheral blood. We also evaluated the ability of the neoPAI Score derived from tumor-infiltrating immune cells (TIICs) to predict survival by employing The Cancer Genome Atlas-Breast Cancer (TCGA-BRCA) database.
Results
In the training cohort, multivariate analysis showed that HR status [odds ratio (OR) 0.325; 95% confidence interval (CI) 0.135–0.761; P = 0.010], HER2 status (OR 2.657; 95% CI 1.266–5.730; P = 0.011), Ki67 index (OR 3.191; 95% CI 1.509–6.956; P = 0.003), histological grade (OR 2.297; 95% CI 1.031–5.290; P = 0.045) and neoPAI Score (OR 4.451; 95% CI 1.608–13.068; P = 0.005) were independent predictors of pCR. In the validation cohort, histological grade (OR 3.779; 95% CI 3.793–1.136 × 103; P = 0.008) and neoPAI Score (OR 90.828; 95% CI 3.827–9.843 × 103; P = 0.019) were independent predictors of pCR. The Immune Model that integrated the neoPAI Score was more accurate in predicting pCR than the Clinical Model that exclusively contained clinicopathological parameters in both cohorts. In TCGA-BRCA database, the neoPAI Score constructed from TIICs can predict the progression-free interval (P = 0.048) of breast cancer.
Conclusion
The neoPAI Score defined by the percentages of peripheral immune cell subsets could be used as a potential biomarker for neoadjuvant chemotherapy efficacy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The immune system plays an important role in the antitumor process. An increasing number of studies have shown that either human epidermal growth factor receptor 2 (HER2)-positive or triple negative breast cancer is an immunogenic disease, and a considerable number of lymphocytes infiltrate into the microenvironment where tumor cells are located [1]. Neoadjuvant chemotherapy is the standard treatment for locally advanced breast cancer (LABC) patients and can provide better surgical conditions and breast-conserving opportunities for patients [2]. Tumor-infiltrating lymphocytes (TILs) can locally mediate antitumor immunity [3,4,5], thus affecting the cytotoxicity of chemotherapy. Studies have shown that the existence of TILs at diagnosis is related to an increased possibility of pathological complete response (pCR) and better disease-free survival (DFS) and overall survival (OS) after neoadjuvant chemotherapy [6,7,8]. However, the evaluation of TILs is complicated and requires obtaining a tumor sample, which makes it almost impossible to observe dynamically throughout the entire disease process [9]. In contrast, peripheral blood can be easily repeatedly obtained. Therefore, it is important to develop a repeatable, simple and minimally invasive biomarker derived from peripheral blood.
Antitumor immunity can be classified into innate immunity and adaptive immunity. The adaptive immune system consists of T cells and B cells. Cytotoxic CD8 + T cells have long been considered the main antitumor immune cells and are associated with a good prognosis [10]. Recently, the antitumor effect of CD4 + T cells and B cells has also been elucidated [11, 12]. Intratumoral cytotoxic CD4 + T cells expressing cytolytic effector proteins were identified in human bladder cancer, and a gene signature of cytotoxic CD4 + T cells was predictive of the response to PD-1 blockade [13]. In addition, another study reported that tumor-infiltrating CD4 + T cells acquire both T helper and cytotoxic features and promote rejection of established tumors [14]. B cells kill tumor cells by mediating humoral immunity and can also enhance the function of T cells through antigen presentation, the provision of costimulatory signals and the secretion of cytokines [15, 16]. It is worth noting that distinguishing immune cell subtypes within tumor tissues is dependent on invasive biopsies or surgical resection. Therefore, it becomes difficult to evaluate patients’ TILs at frequent intervals. Thus, we intended to search for a more minimally invasive index in peripheral blood which can be assessed repeatedly as a surrogate parameter for TILs.
Previous studies have revealed that the adaptive immune response can be enhanced to eliminate tumors, and its effectiveness has been confirmed in many solid tumors [17,18,19]. However, to date, an immune score that reflects the adaptive immune response level of antitumor therapy and predicts the efficacy of neoadjuvant chemotherapy in breast cancer is not available. We integrated the levels of CD4 + T cells, CD8 + T cells, B cells, and the CD4 + /CD8 + ratio in peripheral blood and defined a new index, namely, the “Neo-Peripheral Adaptive Immune Score” for neoadjuvant chemotherapy (neoPAI Score). We aimed to determine whether the neoPAI Score has a good predictive value in response to neoadjuvant treatment for breast cancer patients.
Materials and methods
Patients and treatment
The patients involved in this study were from two prospective clinical trials, SHPD001 (NCT02199418) and SHPD002 (NCT02221999) conducted in China. We analyzed blood immune cells from a total of 226 patients enrolled in SHPD001 and SHPD002. SHPD001 was a single-arm, open-label clinical trial, which explored whether paclitaxel combined with cisplatin on a weekly basis as neoadjuvant chemotherapy regimen is effective and tolerable for locally advanced breast cancer. SPHD002 was a prospective, randomized, open-label clinical trial, which investigated whether neoadjuvant chemotherapy combined with endocrine therapy may improve the pCR rate. Both clinical trials were approved by the Ethics Committee of Renji Hospital, School of Medicine, Shanghai Jiao Tong University [SHPD001, approval ID (2014)14 K; SHPD002, approval ID (2017)088]. All patients signed informed consent forms. Medical research involving human subjects was conducted in accordance with the Helsinki Declaration. All patients were histologically confirmed as invasive breast cancer (clinical tumor size ≥ 2 cm or clinical N1-3) with no distant metastasis. The main inclusion criteria were peripheral immune cell subsets detected before the first dose of neoadjuvant treatment and surgery performed after neoadjuvant treatment.
Detailed inclusion criteria, exclusion criteria and treatment schemes of the two clinical trials have been reported in a previous publication [20]. All patients were administered 80 mg/m2 paclitaxel intravenously on Days 1, 8, 15, 22 every 28 days for four cycles and 25 mg/m2 cisplatin on Days 1, 8, 15 every 28 days for four cycles. Patients with HER2-positive cancer were allowed treatment with trastuzumab concomitantly at a loading dose of 4 mg/kg followed by a maintenance dose of 2 mg/kg on day 1, weekly, for 16 weeks. In SHPD002, HR-positive patients were randomized to receive neoadjuvant chemotherapy with or without endocrine therapy. In the neoadjuvant chemotherapy combined with endocrine therapy group, postmenopausal patients were treated with aromatase inhibitors, whereas premenopausal patients were treated with gonadotropin-releasing hormone agonists. After completing neoadjuvant chemotherapy, patients received surgery.
Data collection
We prospectively collected records of peripheral immune cell subsets before neoadjuvant treatment upon patient enrollment. In addition, we prospectively collected clinicopathological characteristics of patients, including age at diagnosis, clinical stage of tumor and pathological biopsy information of tumor before neoadjuvant treatment. The definition of pCR was the absence of invasive cancer in the breast and no pathological involvement of axillary lymph nodes at the time of surgery.
Peripheral immune cell subsets were examined by the Department of Clinical Laboratory, Renji Hospital, School of Medicine, Shanghai Jiao Tong University. The BD Multitest™ IMK kit, a four-color direct immunofluorescence reagent kit for use with a suitably equipped flow cytometer (BD FACSCanto™), was used to identify and determine the percentages of the following mature human lymphocyte subsets in erythrocyte-lysed whole blood: total T lymphocytes (CD3 +), B lymphocytes (CD19 +), helper/inducer T lymphocytes (CD3 + CD4 + T cells) and cytotoxic T lymphocytes (CD3 + CD8 + T cells).
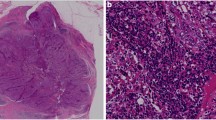
All tissues were histologically diagnosed as invasive breast cancer by the Department of Pathology, Renji Hospital. Estrogen receptor (ER) and progesterone receptor (PR) positivity was defined as immunohistochemistry staining showing ≥ 1% stained cells, and HR positivity was defined as ER-positive and/or PR-positive. HER2 positivity was defined as 3 + by immunohistochemistry or amplification by fluorescence in situ hybridization (FISH).
Definition of neoPAI Score
The neoPAI Score consisted of the component of adaptive immunity [CD4 + T cells (%), CD8 + T cells (%), B cells (%) and CD4 + /CD8 + ratio]. The coefficient of each variable was determined according to the corresponding odds ratio in the multiple logistic regression model for the training cohort. Variables with an odds ratio between 1. 1–2 were assigned 1 point, variables with an odds ratio between 2. 1–3 were assigned 2 points, and variables with an odds ratio between 3. 1–4 were assigned 3 points. The Youden index method was applied to define the optimal cutoff values for the percentages of peripheral immune cell subsets. According to the receiver operating characteristic (ROC) curve, the optimal cutoff values were 49.15%, 24.28%, 12.45%, and 2.27% for the percentages of peripheral CD4 + T cells, CD8 + T cells, B cells and the ratio of CD4 + /CD8 + cells, respectively. We defined neoPAI Score as follows: neoPAI Score = 3*CD4 + T cells (%) + 1*CD8 + T cells (%) + 1*B cells (%) + 1*CD4 + /CD8 + ratio. Patients were then divided into the neoPAI Score-low group and neoPAI Score-high group according to Table 1.
Estimation of immune cell type fractions
We obtained a gene expression profile of breast cancer tissues from The Cancer Genome Atlas-Breast Cancer (TCGA-BRCA, https://portal.gdc.cancer.gov/). Cell type identification by estimating relative subsets of RNA transcripts (CIBERSORT, https://cibersortx.stanford.edu/index.php) is a new computational algorithm for enumerating immune cell subsets using bulk gene expression data [21]. We employed CIBERSORT to quantify 22 tumor-infiltrating immune cells (including the percentages of B cells, T cells, natural killer cells, macrophages, dendritic cells, eosinophils, and neutrophils) in breast cancer. Then, we calculated the neoPAI Score for each sample. The formula was 3*CD4 + T cells (%) [T cells CD4 naïve (%) + T cells CD4 memory resting (%) + T cells CD4 memory activated (%) + T cells follicular helper (%) + T cells regulatory (%)] + 1*CD8 + T cells (%) + 1*B cells (%) [B cells naïve (%) + B cells memory (%) + plasma cells (%)] + 1*CD4 + /CD8 + ratio.
Gene ontology (GO) analysis
GO analysis was performed using DAVID (https://david.ncifcrf.gov/). GO analysis included 3 components: biological process (BP), cellular component (CC), and molecular function (MF). A P value < 0.05 was considered a statistically significant cutoff criterion.
Gene set enrichment analysis (GSEA)
In the TCGA-BRCA database, 878 invasive breast cancer cases were divided into neoPAI Score-low and neoPAI Score-high groups according to Table 1. The transcriptome data of 878 patients were selected for GSEA to detect the gene sets that were enriched in the neoPAI Score-high group. GSEA was performed using the REACTOME (Home-Reactome Pathway Database, 2021) database. The cutoff criteria were as follows: normalized enrichment scores (NES) > 1.0, false discovery rate (FDR) q < 0.25 and nominal P < 0.05.
Statistical analysis
All the eligible patients were randomly assigned to the training cohort and the validation cohort in an 8:2 ratio by a split-sample approach. To compare categorical variables in different groups, the chi-square test was used. The relationship between the percentages of peripheral immune cell subsets and pCR was assessed by univariate and multivariate logistic regression analyses. The multivariate logistic regression model included age (> 50 vs. ≤ 50), T stage (T3-4 vs. T1-2), N stage (N1-3 vs. N0), HR status (positive vs. negative), HER2 status (positive vs. negative), Ki67 index (> 50% vs. ≤ 50%), histological grade (G3 vs. G1-2) and neoPAI Score (high vs. low).
To evaluate whether the neoPAI Score combined with important clinicopathological characteristics can better predict the possibility of pCR, we first used a stepwise regression method to select the variables from traditional parameters (age, T stage, N stage, HR status, HER2 status, Ki67 index and histological grade), constructing a Clinical Model including T stage, HR status, HER2 status, Ki67 index and histological grade. Then, we constructed an Immune Model including T stage, HR status, HER2 status, Ki67 index, histological grade and neoPAI Score. A nomogram was used to visualize the two predictive models. The possibility of pCR is calculated by taking the sum of the risk points. The total points are the sum of each factor’s corresponding value for every individual patient. The calibration curve was used to evaluate the accuracy of the Immune Model. The predictive value of the Immune Model and the Clinical Model were compared with ROC curve and decision curve analysis (DCA).
The progression-free interval (PFI) is the period from the date of diagnosis until the date of the first occurrence of a new tumor event (NTE), which includes progression of the disease, locoregional recurrence, distant metastasis, new primary tumor, or death with tumor [22]. Kaplan–Meier curves were used for survival analysis, and significance was evaluated using the log-rank test. All P values were two-sided, and P < 0.05 was considered statistically significant. All statistical analyses were performed using GraphPad Prism 8.4.3 (GraphPad Software LLC, California, USA), Stata software (version 15.1) and R language version 3.6.2 (www.r-project.org).
This study followed the Reporting Recommendations for Tumor Markers in Prognostic Studies (REMARK) criteria [23].
Results
Baseline characteristics
A total of 226 patients met the inclusion criteria, including 181 patients in the training cohort and 45 in the validation cohort. The breast cancer subtypes in this study included HR-positive/HER2-negative (n = 95), HER2-positive (n = 100), and triple negative (n = 31) breast cancer. Clinicopathological characteristics of the training cohort and validation cohort were shown in Supplementary Table 1. Forty-eight patients (32.04%) in the training cohort and thirteen patients (28.89%) in the validation cohort achieved pCR. The baseline characteristics of the neoPAI Score-high and neoPAI Score-low groups were compared, and no significant differences were found between the training cohort and validation cohort (Table 2). Correlations between peripheral immune cell subsets in both cohorts were calculated. In both training and validation cohorts, CD4 + T cells, CD4 + /CD8 + ratio and B cells were correlated negatively with CD8 + T cells. Correlation coefficients and P values are displayed in Supplementary Fig. 1.
The relationships between peripheral immune cell subsets and pCR
In the training cohort, patients with higher percentages of peripheral CD4 + T cells (P = 0.010), B cells (P = 0.043) and neoPAI Score (P = 0.002) might have higher pCR rates. In the validation cohort, patients with higher percentage of peripheral CD4 + T cells (P = 0.028), CD4 + /CD8 + ratio (P = 0.019) and neoPAI Score (P = 0.028) might have higher pCR rates (Fig. 1).
The relationships between peripheral immune cell subsets, neoPAI Score and pCR. a–e The pCR rates by CD4 + T cells (%), CD8 + T cells (%), CD4 + /CD8 + ratio, B cells (%) and neoPAI Score in the training cohort. f–j The pCR rates by CD4 + T cells (%), CD8 + T cells (%), CD4 + /CD8 + ratio, B cells (%) and neoPAI Score in the validation cohort. P values were calculated by the chi-square test. *: p < 0.05, **: p < 0.01. pCR pathological complete response, neoPAI Score neo-peripheral adaptive immune score for neoadjuvant chemotherapy
The univariate analysis showed that clinical T stage (OR 0.404; 95% CI 0.176–0.920; P = 0.030), HR status (OR 0.305; 95% CI 0.143–0.640; P = 0.002), HER2 status (OR 2.836; 95% CI 1.500–5.469; P = 0.002), Ki67 index (OR 2.843; 95% CI 1.502–5.460; P = 0.001), histological grade (OR 3.879; 95% CI 1.948–8.153; P < 0.001), the percentages of peripheral CD4 + T cells (OR 2.943; 95% CI 1.263–6.967; P = 0.012), B cells (OR 1.955; 95% CI 1.028–3.809; P = 0.044) and the neoPAI Score (OR 4.030; 95% CI 1.650–10.320; P = 0.003) were predictive indicators of pCR in the training cohort. In the validation cohort, Ki67 index (OR 4.950; 95% CI 1.292–22.091; P = 0.025), histological grade (OR 7.333; 95% CI 1.806–38.412; P = 0.009), the percentages of peripheral CD4 + T cells (OR 6.667; 95% CI 1.117–54.202; P = 0.045), CD4 + /CD8 + ratio (OR 5.056; 95% CI 1.268–21.904; P = 0.024) and the neoPAI Score (OR 6.667; 95% CI 1.117–54.202; P = 0.045) could predict pCR (Table 3).
In the multivariate analysis, HR status (OR 0.325; 95% CI 0.135–0.761; P = 0.010), HER2 status (OR 2.657; 95% CI 1.266–5.730; P = 0.011), Ki67 index (OR 3.191; 95% CI 1.509–6.956; P = 0.003), histological grade (OR 2.297; 95% CI 1.031–5.290; P = 0.045) and the neoPAI Score (OR 4.451; 95% CI 1.608–13.068; P = 0.005) were independent predictors of pCR in the training cohort. However, in the validation cohort, histological grade (OR 3.779; 95% CI 3.793–1.136 × 103; P = 0.008) and the neoPAI Score (OR 90.828; 95% CI 3.827–9.843 × 103; P = 0.019) were independent predictors of pCR (Table 4). The inclusion of menstrual status instead of age in the multivariate analysis did not change the result (Supplementary Table 2). We also performed the multivariate analysis of CD4 + T cells (%), CD8 + T cells (%), B cells (%), and CD4 + /CD8 + ratio , respectively with age, clinical T stage, clinical lymph node metastasis, HR status, HER2 status, Ki67 index, and histological grade, which showed that CD4 + T cells (%) was an independent predictor of pCR in both training cohort and validation cohort (Table 5).
A prediction model including the neoPAI Score for pCR
A nomogram was used to visualize the Clinical Model in the training cohort (Fig. 2a) and validation cohort (Fig. 3a). The nomogram of the Immune Model for both cohorts is shown in Fig. 2b and Fig. 3b. The accuracy of the Immune Model was evaluated using a calibration curve. The calibration curve was close to the dashed line of the ideal case, which indicates that the predicted pCR rate of the Immune Model was highly consistent with the actual pCR situation for both cohorts (Figs. 2c, 3c). The calibration curve of the Clinical Model is shown in Supplementary Fig. 2. We compared the predictive value of these two models using the ROC curve. The area under curve (AUC) of the Immune Model (training cohort, 0.798; validation cohort, 0.891) was higher than that of the Clinical Model (training cohort, 0.777; validation cohort, 0.832; Figs. 2d, 3d). DCA revealed that adding the neoPAI Score to the Clinical Model increased the clinical benefit and helped clinical decision-making in either the training cohort (Fig. 2e) or the validation cohort (Fig. 3e). Thus, compared with the Clinical Model including only clinicopathological factors, the Immune Model integrating the neoPAI Score could predict pCR with increased accuracy.
The Clinical Model and the Immune Model in the training cohort. a The nomogram of the Clinical Model. b The nomogram of the Immune Model. c The calibration curve of the Immune Model. d The ROC curve of the Clinical Model and Immune Model. e The decision curve of the Clinical Model and Immune Model. HR hormone receptor, HER2 human epidermal growth factor receptor 2, neoPAI Score neo-peripheral adaptive immune score for neoadjuvant chemotherapy, ROC receiver operating characteristic, AUC area under curve, AUDC area under decision curve
The Clinical Model and the Immune Model in the validation cohort. a The nomogram of the Clinical Model. b The nomogram of the Immune Model. c The calibration curve of the Immune Model. d The ROC curve of the Clinical Model and Immune Model. e The decision curve of the Clinical Model and Immune Model. HR hormone receptor, HER2 human epidermal growth factor receptor 2, neoPAI Score neo-peripheral adaptive immune score for neoadjuvant chemotherapy, ROC receiver operating characteristic, AUC area under curve, AUDC area under decision curve
The neoPAI score constructed by tumor-infiltrating immune cells predicted survival in TCGA database
TCGA-BRCA gene expression profiles of breast cancer tissues were analyzed by CIBERSORT to quantify 22 tumor-infiltrating immune cells. We calculated the neoPAI Score for each sample and used Kaplan–Meier curves to evaluate the prognostic value of the neoPAI Score. A higher neoPAI Score was correlated with a better PFI (P = 0.048, Fig. 4a). A total of 878 TCGA samples were classified into neoPAI Score-low and neoPAI Score-high groups. We analyzed differentially expressed genes (DEGs) between the neoPAI Score-low and neoPAI Score-high groups. MYH6, ECEL1, SERPINA6, MYH7, ACY3, CHGB and SYNPO2L were most significantly overexpressed in the neoPAI Score-high group (Fig. 4b). Genes enriched in the neoPAI Score-high group were analyzed by GO, and significantly enriched pathways of DEGs, including muscle filament sliding, neuropeptide signaling pathway and muscle contraction, were identified (Fig. 4c). Moreover, GSEA revealed that the neoPAI Score-high group was highly enriched in activation of NMDA receptors and postsynaptic events, adaptive immune system, costimulation by the CD28 family, immunoregulatory interactions between lymphoid and non-lymphoid cells, and integrin cell surface interaction (Fig. 4f).
Kaplan–Meier curve of neoPAI Score predicting PFI in the TCGA database and bioinformatics analysis of signaling pathways. a PFI in the TCGA database. b Volcano plot showing DEGs between the neoPAI Score-low and neoPAI Score-high groups in the TCGA database. Genes labeled in red or blue are significantly differentially up- or down-regulated, respectively. c The GO terms of the BP category enrichment of the DEGs. d The GO terms of the CC category enrichment of the DEGs. e The GO terms of the MF category enrichment of the DEGs. f GSEA for biological pathways and processes in the neoPAI Score-high TCGA cohort. neoPAI Score neo-peripheral adaptive immune score for neoadjuvant chemotherapy, PFI progression-free interval, TCGA the cancer genome atlas, DEG differentially expressed gene, GO Gene Ontology, GSEA gene set enrichment analysis, BP biological process, CC cellular component, MF molecular function
Discussion
To the best of our knowledge, we proposed an easily detectable and traceable immune score derived from peripheral blood in the neoadjuvant setting. We defined the neoPAI Score, which may reflect the state of the body's systemic adaptive immune response at the time of assessment. Our study showed that the neoPAI Score was a good predictor of the efficacy of neoadjuvant chemotherapy for LABC. We also verified that the neoPAI Score was a prognostic biomarker for PFI in the TCGA database.
To date, few clinical studies have reported that immune cell subsets derived from peripheral blood could predict the efficacy of neoadjuvant chemotherapy for locally advanced breast cancer. One previous study reported that the “immune score” calculated based on the density of total T lymphocytes and CD8 + T lymphocytes within the tumor and at the infiltrating margin of the tumor could reflect the adaptive immune response against the tumor and can effectively predict the risk of recurrence for patients with colon cancer [24, 25]. In breast cancer, the increase in total infiltrating lymphocytes or CD8 + T lymphocytes after neoadjuvant chemotherapy was proposed to be associated with better prognosis [26]. All of these studies focused on tumor-infiltrating immune cells; however, we defined a new indicator derived from peripheral blood, neoPAI Score, incorporating the percentages of peripheral CD4 + T cells, CD8 + T cells, and B cells and the CD4 +/CD8 + ratio. Our findings suggested that the neoPAI Score was a good predictor of the efficacy of neoadjuvant chemotherapy. Additionally, the neoPAI Score defined in our study can be monitored dynamically, and evaluation of the neoPAI Score is minimally invasive. Therefore, the neoPAI Score is of high value in clinical application.
Several studies have evaluated the correlation between peripheral immune cell subsets and the prognosis of metastatic cancer patients [27,28,29,30]. A study included 40 patients with metastatic colon cancer who planned to receive first-line chemotherapy, and the immune cell subsets in the peripheral blood of these patients were tested. This study found that high monocytic myeloid-derived suppressor cells (M-MDSCs), low CD4 + T lymphocytes and low CD8 + T lymph cells were unfavorable factors for progression-free survival (PFS) [29]. In contrast, another study retrospectively analyzed the peripheral lymphocyte subset data of 482 patients with metastatic breast cancer, and multivariate survival analysis indicated that CD4 + T lymphocytes [hazard ratio (HR) 0.538, 95% CI 0.313–0.926, P = 0.025] and CD3 + T lymphocytes (HR 0.437, 95% CI 0.248–0.772, P = 0.004) were indicative of worse prognosis for HER2-positive metastatic breast cancer patients [30]. However, few studies have reported the predictive value of peripheral immune cell subsets or immune scores in the context of neoadjuvant chemotherapy [31, 32]. We analyzed the predictive value of each single peripheral immune cell subset in the neoadjuvant setting, and our data indicated that the neoPAI Score and several peripheral immune cells, which reflect systemic immune status, have a good predictive value for pCR. To build a good predictive model of pCR, we constructed an Immune Model including clinicopathological parameters and the neoPAI Score. Importantly, both ROC curve and DCA indicated that the Immune Model was numerically better than the Clinical Model in predicting pCR. Thus, the neoPAI Score is a promising biomarker that can well predict the efficacy of neoadjuvant chemotherapy.
Studies have demonstrated a quantitative relationship between TILs and peripheral immune cells [33, 34]. On the one hand, from the perspective of antitumor immune processes, tumor antigens are recognized by antigen-presenting cells and presented to T cells. Antigen-specific T cells are activated against the tumor antigen. The activated T cells migrate to the tumor through the blood vessels and then penetrate into the tumor, playing an effective role. On the other hand, T-cell clones are classified according to complementarity-determining region 3 (CDR3). The parallel infiltration of highly amplified T-cell clonotypes into tumors and normal adjacent tissue has a strong relationship with peripheral clonal expansion, suggesting that T-cell clonotypes in tumors are derived from peripheral blood [35]. In addition, Gros et al. successfully isolated tumor antigen-specific CD8 + T lymphocytes from the peripheral blood of melanoma patients. Similar to tumor-infiltrating T lymphocytes, these T lymphocytes can be expanded in vitro and then infused back into the patient to mediate antitumor treatment [36]. These studies support our results that the neoPAI Score generated from peripheral blood immune cells performed well to predict neoadjuvant chemotherapy efficacy.
Given the lack of a peripheral blood database, we quantified 22 tumor-infiltrating immune cells (including B cells, T cells, natural killer cells, macrophages, dendritic cells, eosinophils, and neutrophils) from the TCGA-BRCA database by CIBERSORT to explore the prognostic value of neoPAI score in breast cancer. We adopted tumor-infiltrating immune cells to substitute for peripheral immune cells and calculated the neoPAI Score for each sample based on tumor-infiltrating immune cells. We found that the neoPAI Score derived from tumor-infiltrating immune cells was significantly predictive of a better PFI in patients with breast cancer. GSEA suggested that NMDA receptors and postsynaptic events, adaptive immune system, costimulation by the CD28 family, immunoregulatory interactions between lymphoid and non-lymphoid cells, and integrin cell surface interaction may contribute to better survival in the neoPAI Score-high group.
There are several limitations in our study. First, the sample size of this study was small. However, this is a retrospective analysis of the prospective studies, and the results were indirectly validated by external online datasets. Our study may suggest underlying rules and provide a rationale for prospective studies with large samples. Moreover, our patients used cisplatin-paclitaxel regimens for neoadjuvant chemotherapy. Whether the same conclusion can be obtained in patients using other neoadjuvant chemotherapy regimens needs to be investigated in the future. In addition, CD4 + T lymphocytes can be further divided into several subgroups, such as Th1, Th2, Th17, CD4 + follicular helper T cells (Tfhs) and regulatory T cells (CD4 + Tregs). Tfhs are associated with good prognosis [37], whereas CD4 + Tregs are associated with poor prognosis [38]. Therefore, a more detailed classification of peripheral immune cell subsets may further improve the accuracy of prediction.
In conclusion, our research showed that peripheral immune cell subsets, especially when assessed using the neoPAI Score, are predictors of response to neoadjuvant chemotherapy for breast cancer patients. This study provides a rationale for further prospective clinical trials to explore the role of peripheral immune cell subsets in breast cancer patients, which will allow us to predict the efficacy of neoadjuvant chemotherapy for each patient based on individual characteristics.
Data availability
Data are contained within the article, supplementary materials and from the corresponding author upon request.
References
Hammerl D, Smid M, Timmermans AM et al (2018) Breast cancer genomics and immuno-oncological markers to guide immune therapies. Semin Cancer Biol 52(Pt 2):178–188. https://doi.org/10.1016/j.semcancer.2017.11.003
Teshome M, Kuerer HM (2017) Breast conserving surgery and locoregional control after neoadjuvant chemotherapy. Eur J Surg Oncol 43(5):865–874. https://doi.org/10.1016/j.ejso.2017.02.002
Finn OJ (2012) Immuno-oncology: understanding the function and dysfunction of the immune system in cancer. Ann Oncol. https://doi.org/10.1093/annonc/mds256
Chen DS, Mellman I (2013) Oncology meets immunology: the cancer-immunity cycle. Immunity 39(1):1–10. https://doi.org/10.1016/j.immuni.2013.07.012
Palucka AK, Coussens LM (2016) The basis of oncoimmunology. Cell 164(6):1233–1247. https://doi.org/10.1016/j.cell.2016.01.049
de Melo GD, Cortes J, Curigliano G et al (2017) Tumor-infiltrating lymphocytes in breast cancer and implications for clinical practice. Biochim Biophys Acta Rev Cancer 1868(2):527–537. https://doi.org/10.1016/j.bbcan.2017.10.003
Denkert C, von Minckwitz G, Brase JC et al (2015) Tumor-infiltrating lymphocytes and response to neoadjuvant chemotherapy with or without carboplatin in human epidermal growth factor receptor 2-positive and triple-negative primary breast cancers. J Clin Oncol 33(9):983–991. https://doi.org/10.1200/JCO.2014.58.1967
Salgado R, Denkert C, Demaria S et al (2015) The evaluation of tumor-infiltrating lymphocytes (TILs) in breast cancer: recommendations by an International TILs working group 2014. Ann Oncol 26(2):259–271. https://doi.org/10.1093/annonc/mdu450
Savas P, Salgado R, Denkert C et al (2016) Clinical relevance of host immunity in breast cancer: from TILs to the clinic. Nat Rev Clin Oncol 13(4):228–241. https://doi.org/10.1038/nrclinonc.2015.215
Mahmoud SM, Paish EC, Powe DG et al (2011) Tumor-infiltrating CD8+ lymphocytes predict clinical outcome in breast cancer. J Clin Oncol 29(15):1949–1955. https://doi.org/10.1200/JCO.2010.30.5037
Nelson MA, Ngamcherdtrakul W, Luoh SW, Yantasee W (2021) Prognostic and therapeutic role of tumor-infiltrating lymphocyte subtypes in breast cancer. Cancer Metastasis Rev 40(2):519–536. https://doi.org/10.1007/s10555-021-09968-0
Kagamu H, Kitano S, Yamaguchi O et al (2020) CD4+ T-cell immunity in the peripheral blood correlates with response to anti-PD-1 therapy. Cancer Immunol Res 8(3):334–344. https://doi.org/10.1158/2326-6066.CIR-19-0574
Oh DY, Kwek SS, Raju SS et al (2020) Intratumoral CD4(+) T cells mediate anti-tumor cytotoxicity in human bladder cancer. Cell 181(7):1612–25.e13. https://doi.org/10.1016/j.cell.2020.05.017
Sledzinska A, Vila de Mucha M, Bergerhoff K et al (2020) Regulatory T cells restrain interleukin-2- and blimp-1-dependent acquisition of cytotoxic function by CD4(+) T cells. Immunity 52(1):151–66.e6. https://doi.org/10.1016/j.immuni.2019.12.007
Garaud S, Buisseret L, Solinas C et al (2019) Tumor infiltrating B-cells signal functional humoral immune responses in breast cancer. JCI Insight. https://doi.org/10.1172/jci.insight.129641
Tokunaga R, Naseem M, Lo JH et al (2019) B cell and B cell-related pathways for novel cancer treatments. Cancer Treat Rev 73:10–19. https://doi.org/10.1016/j.ctrv.2018.12.001
Varn FS, Mullins DW, Arias-Pulido H et al (2017) Adaptive immunity programmes in breast cancer. Immunology 150(1):25–34. https://doi.org/10.1111/imm.12664
Dzhandzhugazyan KN, Guldberg P, Kirkin AF (2018) Adoptive T cell cancer therapy. Nat Mater 17(6):475–477. https://doi.org/10.1038/s41563-018-0094-5
Restifo NP, Dudley ME, Rosenberg SA (2012) Adoptive immunotherapy for cancer: harnessing the T cell response. Nat Rev Immunol 12(4):269–281. https://doi.org/10.1038/nri3191
Zhou LH et al (2017) Weekly paclitaxel and cisplatin as neoadjuvant chemotherapy with locally advanced breast cancer: a prospective, single arm, phase II study. Oncotarget 8(45):79305–79314. https://doi.org/10.18632/oncotarget.17954
Newman AM, Liu CL, Green MR et al (2015) Robust enumeration of cell subsets from tissue expression profiles. Nat Methods 12(5):453–457. https://doi.org/10.1038/nmeth.3337
Liu J, Lichtenberg T, Hoadley KA et al (2018) An integrated TCGA pan-cancer clinical data resource to drive high-quality survival outcome analytics. Cell 173(2):400-416.e11. https://doi.org/10.1016/j.cell.2018.02.052
Sauerbrei W, Taube SE, McShane LM, Cavenagh MM, Altman DG (2018) Reporting recommendations for tumor marker prognostic studies (REMARK): an abridged explanation and elaboration. J Natl Cancer Inst 110(8):803–811. https://doi.org/10.1093/jnci/djy088
Pages F, Mlecnik B, Marliot F et al (2018) International validation of the consensus Immunoscore for the classification of colon cancer: a prognostic and accuracy study. Lancet 391(10135):2128–2139. https://doi.org/10.1016/S0140-6736(18)30789-X
Marliot F, Chen X, Kirilovsky A et al (2020) Analytical validation of the immunoscore and its associated prognostic value in patients with colon cancer. J Immunother Cancer. https://doi.org/10.1136/jitc-2019-000272
Park YH, Lal S, Lee JE et al (2020) Chemotherapy induces dynamic immune responses in breast cancers that impact treatment outcome. Nat Commun 11(1):6175. https://doi.org/10.1038/s41467-020-19933-0
Rutkowski J, Cyman M, Ślebioda T et al (2017) Evaluation of peripheral blood T lymphocyte surface activation markers and transcription factors in patients with early stage non-small cell lung cancer. Cell Immunol 322:26–33. https://doi.org/10.1016/j.cellimm.2017.09.007
Guo Z, Liang H, Xu Y et al (2017) The role of circulating t follicular helper cells and regulatory cells in non-small cell lung cancer patients. Scand J Immunol 86(2):107–112. https://doi.org/10.1111/sji.12566
Tada K, Kitano S, Shoji H et al (2016) Pretreatment immune status correlates with progression-free survival in chemotherapy-treated metastatic colorectal cancer patients. Cancer Immunol Res 4(7):592–599. https://doi.org/10.1158/2326-6066.CIR-15-0298
Yang J, Junnan Xu, Ying E, Sun T (2019) Predictive and prognostic value of circulating blood lymphocyte subsets in metastatic breast cancer. Cancer Med 8(2):492–500. https://doi.org/10.1002/cam4.1891
Axelrod ML, Nixon MJ, Gonzalez-Ericsson PI et al (2020) Changes in peripheral and local tumor immunity after neoadjuvant chemotherapy reshape clinical outcomes in patients with breast cancer. Clin Cancer Res 26(21):5668–5681. https://doi.org/10.1158/1078-0432.CCR-19-3685
Zhou H, Li G, Yin J et al (2021) Neoadjuvant chemotherapy alters peripheral and tumour-infiltrating immune cells in breast cancer revealed by single-cell RNA sequencing. Clin Transl Med 11(12):e621. https://doi.org/10.1002/ctm2.621
Malekzadeh P, Yossef R, Cafri G et al (2020) Antigen experienced T cells from peripheral blood recognize p53 neoantigens. Clin Cancer Res 26(6):1267–1276. https://doi.org/10.1158/1078-0432.CCR-19-1874
Li T, Zhao L, Yang Y et al (2021) T cells expanded from pd-1+ peripheral blood lymphocytes share more clones with paired tumor-infiltrating lymphocytes. Cancer Res 81(8):2184–2194. https://doi.org/10.1158/0008-5472.CAN-20-2300
Wu TD, Madireddi S, de Almeida PE et al (2020) Peripheral T cell expansion predicts tumour infiltration and clinical response. Nature 579(7798):274–278. https://doi.org/10.1038/s41586-020-2056-8
Gros A, Parkhurst MR, Tran E, et al (2016) Prospective identification of neoantigen-specific lymphocytes in the peripheral blood of melanoma patients. Nat Med 22(4):433-438. https://doi.org/10.1038/nm.4051Ò
Gu-Trantien C, Loi S, Garaud S et al (2013) CD4(+) follicular helper T cell infiltration predicts breast cancer survival. J Clin Invest 123(7):2873–2892. https://doi.org/10.1172/JCI67428
Hashemi V, Maleki LA, Esmaily M et al (2020) Regulatory T cells in breast cancer as a potent anti-cancer therapeutic target. Int Immunopharmacol. https://doi.org/10.1016/j.intimp.2019.106087
Funding
This work was supported by the Shanghai Sailing Program (Grant No. 22YF1424500), National Natural Science Foundation of China (Grant No. 82103695), Clinical Research Plan of Shanghai Hospital Development Center (Grant No. SHDC2020CR3003A), Science and Technology Commission of Shanghai Municipality (Grant No. 20DZ2201600), Shanghai Municipal Key Clinical Specialty, Shanghai Rising-Star Program (Grant No. 22QC1400200), Multidisciplinary Cross Research Foundation of Shanghai Jiao Tong University (Grant No. YG2019QNA28), Nurturing Fund of Renji Hospital (Grant Nos. PYIII20-09 and RJPY-LX-002), Clinical Research Innovation Nurturing Fund of Renji Hospital and United Imaging (Grant No. 2021RJLY-002).
Author information
Authors and Affiliations
Contributions
HW, YW, WY and JL: conceptualization, HW, YW and XS: methodology, YX, TY, JZ and YL: investigation, HW: formal analysis, HW and XS: writing—original draft preparation, HW, YW, WY and JL: writing—review and editing, YY, SX, LZ, WY and JL: supervision. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, H., Sheng, X., Yan, T. et al. Neo-peripheral adaptive immune score predicts neoadjuvant chemotherapy for locally advanced breast cancer. Breast Cancer Res Treat 197, 343–354 (2023). https://doi.org/10.1007/s10549-022-06791-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-022-06791-1