Abstract
Purpose
We examined the associations between intake of meat and fish by preparation methods and breast cancer in the Carolina Breast Cancer Study, a racially diverse population-based case–control study.
Methods
African American (AA) and European American (EA) women aged 20–74 years with a first diagnosis of invasive or in situ breast cancers were frequency matched by race and age group to controls identified through the North Carolina Division of Motor Vehicles and Medicare lists [AA: 548 cases, 452 controls; EA: 858 cases, 748 controls]. Participants self-reported meat preparation methods and intake frequencies. Adjusted odds ratios (OR) and 95% confidence intervals (CIs) were calculated using multivariable logistic regression adjusted for age, race, alcohol intake, body mass index, family income, lactation, marital status, use of oral contraceptives, postmenopausal hormone use, smoking status, and offsets.
Results
Positive associations with breast cancer were observed for intakes of grilled/barbecued hamburger (≥ once/week, OR: 1.28; 95% CI 1.01, 1.63), and pan-fried/oven-broiled beef steak (≥ once/week, OR: 1.36; 95% CI 1.08, 1.72). Inverse associations were observed for pan-fried fish (≥ once/week, OR: 0.77; 95% CI 0.60, 0.98), and for grilled/ barbecued pork chops (> 0 time/week OR: 0.81, 95% CI 0.68, 0.97). Associations tended to be stronger among EA women than among AA women.
Conclusion
More frequent consumption of beef prepared with high temperature methods was associated with higher odds of breast cancer while more frequent consumption of pan-fried fish or grilled/barbecued pork chops was associated with lower odds of breast cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most common cancer and the second leading cause of cancer deaths among women in the USA [1]. Several dietary factors including red meat are suggested to contribute to the risk of breast cancer [2, 3]. Processed meat may contain N-nitroso compounds (NOCs) and preparing meat at high temperatures such as grilling or pan-frying could increase the production of heterocyclic amines (HCAs) and polycyclic aromatic hydrocarbons (PAHs), which are implicated in breast carcinogenesis [4,5,6]. In addition, advanced glycation end-products formed from non-enzymatic reaction of sugars and proteins or lipids have been implicated in oxidative stress and inflammation [7], and high levels have been detected in food cooked at high temperatures, particularly meat and animal products [8] and associated with increased risk of breast cancer [9, 10].
Several studies have reported an increase in breast cancer risk with high intake of red meat [3, 11, 12] especially meat prepared at high degrees of temperature or doneness [2, 13,14,15]. However, not all findings have been supportive [16, 17]. A meta-analysis from 2018 combining data from up to 15 prospective studies found increased breast cancer risk with consumption of processed meat and a nonsignificant increased risk for consumption of red meat [18]. AA women were reported to have higher total meat intake compared to EA women [19]. Studies on the association between red meat and poultry and breast cancer stratified by race have produced mixed results [20] but few studies have enrolled enough AA women to precisely examine these associations. Data on relationships by breast cancer hormone receptor status are also limited but some studies show differential associations by estrogen receptor (ER)/progesterone receptor (PR) status [20, 21]. In this study, we examined associations between meat and fish cooked by various preparation methods and risk of breast cancer among AA and EA North Carolina women enrolled in the population-based Carolina Breast Cancer Study (CBCS). We further examined whether associations differed by ER status and menopausal status.
Materials and methods
Study population
The CBCS is a population-based case–control study of women diagnosed with breast cancer across 24 counties in central and eastern North Carolina. Women aged between 20 and 74 years and diagnosed with invasive breast cancer between 1993 and 2001 were enrolled in Phases 1 & 2 and carcinoma in situ (CIS) cases diagnosed between 1996 and 2001 were enrolled in Phase 2 [22]. AAs and younger women aged less than 50 years were oversampled [23, 24]. Controls were selected from the North Carolina Division of Motor Vehicles (for women younger than 65 years) or selected from the US Health Care Financing Administration (for women aged 65 and older) and were approximately frequency matched to cases by age and race [22].
Data collection
Questionnaires were administered to subjects in the home by a trained registered nurse. The median time between diagnosis and data collection by the registered nurse for cases was 3 months (ranged between 1 and 19 months; 80% interviewed by 5 months). For controls, the median time from enrollment to interview was 2 months (ranged between 0 and 26 months; 80% interviewed by 5 months). The questionnaire requested information on demographic data, reproductive and family history of cancer and dietary practices. In the section on dietary intake, information was acquired on intake levels of eight meat and fish items five years prior to the interview.
Outcome assessment
Cases were identified using the North Carolina Central Cancer Registry’s rapid case ascertainment system. Invasive and CIS cases were enrolled. CIS included women with ductal carcinoma in situ (DCIS), DCIS with micro invasion to a depth of 2 mm, lobular CIS (LCIS) and mixed DCIS and LCIS. Immunohistochemistry (IHC) profiles were created by microarray analysis and IHC staining for ER, human epidermal growth factor receptors-1 & -2 (HER2 and HER1), and cytokeratin 5/6 [25]. Cases were further classified based on ER status as ER-positive or ER-negative.
Exposure assessment
The categories of meat included chicken; hamburger; beef steak; pork chops; bacon; breakfast sausage; and hot dog or other sausage. Fish intake was queried as fish steak or fish prepared whole. Preparation methods included “pan-fried or oven-broiled” and “grilled or barbecued” for beef and pork products; and “pan-fried,” “oven-broiled,” and “grilled or barbecued” for chicken and fish. Frequency of intake by meat and fish type and preparation method were reported as times per week, month, or year and converted to times per week. Missing values for frequency of intake of meat and fish cooked were imputed based on the most frequent responses for observations with similar information on age group, race, and breast cancer status. Preference for level of doneness on the inside of meat such as beef steak, roast, or hamburger was categorized as NA/rare to medium rare (red or dark pink); medium to medium well (light pink); or well-done (gray-brown with juice or dry) while doneness on the outside of meat was categorized as NA/not browned/lightly browned; well-browned; or heavily browned or charred.
Statistical analyses
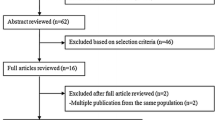
There were 4333 women in the CBCS dataset, of which 4267 self-identified as AA or EA. Women enrolled in Phase 1 (n = 1651) did not complete the meat intake questionnaire and were excluded from analyses. Women in Phase 2 who were missing meat intake information (n = 10) also were excluded (Fig. 1). Multivariable logistic regression was used to calculate adjusted odds ratios (ORs) and 95% confidence intervals (CIs) of breast cancer by frequency of intake of meat and fish cooked by various preparation methods. Offset terms derived from sampling probabilities, age at enrollment (continuous), and self-identified race (AA or EA) were included for adjustment in all models. Important potential confounders identified through a literature review on risk factors for breast cancer included alcohol intake, reproductive factors (age at menarche, parity, lactation, use of oral contraceptives, post-menopausal status), post-menopausal hormone use, family history of breast cancer, current body mass index (BMI as weight(kg)/height(m)2), BMI at 18 years, smoking, marital status, and family income. Because a complete dietary assessment method was not utilized in the study, we were unable to adjust for energy intake and considered BMI as a potential surrogate for energy intake in the multivariable analyses. Directed acyclic graphs (DAG) were used to identify a minimally sufficient set of confounders for adjustment which included alcohol intake (yes or no/missing); BMI, kg/m2 [missing, underweight (< 18.5), normal weight (18.5–24.9), overweight (25–29.9) or obese (≥ 30)]; family income (missing, < $15,000, $15,000–$30,000, $30,000–$50,000 or > $50,000); ever lactated (yes or no); marital status (never married/lived as married/missing, married/living as married, widowed or separated/divorced/no longer living as married); ever used oral contraceptives (never/missing or ever); post-menopausal hormone use (never/missing, past, current); and smoking status (never, former, or current). Further adjustments were made for fruit and vegetable intake during the summer and winter seasons of the previous year [low (< 19 half cup-sized servings/week), moderate (19–31 half cup-sized servings/week), or high (≥ 32 half cup-sized servings/week)] and regular physical activity in the previous three months (yes or no).
The results presented include analyses on the whole study population, as well as with stratification by race, menopausal status, invasiveness of disease, and fruit and vegetable intake. Interaction was assessed by including a cross-product of the meat or fish variable with race, menopausal status, or fruit and vegetable intake, and p-values for the multiplicative interaction term were reported. Multinomial logistic regression was used to calculate adjusted ORs for the associations of the frequency of intake of meat and fished cooked by various preparation methods and breast cancer by ER status. In sensitivity analyses, we mutually adjusted for other meat and fish intake variables for those dietary variables that showed significant associations in the main analyses. All statistical analyses were performed using SAS version 9.4.
Results
The analytical sample consisted of 1406 cases and 1200 controls (Fig. 1). Women diagnosed with breast cancer appeared to have similar baseline and demographic characteristics with the control group (Table 1). Associations with breast cancer were estimated using the lowest level of no reported intake of each specific meat or fish as the referent. After adjusting for DAG-identified confounders, statistically significant (p < 0.05) positive associations were found for the intakes of grilled/barbecued hamburger (one or more times per week, OR: 1.28; 95% CI 1.01, 1.63) and pan-fried/oven-broiled beef steak (one or more times per week, OR: 1.36; 95% CI 1.08, 1.72) (Table 2). Significant inverse associations were observed for pan-fried fish consumed one or more times per week (OR: 0.77; 95% CI 0.60, 0.98) and grilled/barbecued pork chops consumed more than 0 times per week (OR: 0.81; 95% CI 0.68, 0.97) (Table 2). There were no statistically significant associations for the other types of meat and cooking methods. The associations did not change after further adjustment for physical activity or fruit and vegetable intake (data not shown).
In the race-stratified adjusted analyses, pan-fried fish (one or more times per week, OR: 0.63; 95% CI 0.44, 0.89), grilled/barbecued beef steak (less than once per week, OR: 0.76; 95% CI 0.59, 0.98), and grilled/barbecued pork chops (more than 0 times per week, OR: 0.75; 95% CI 0.60, 0.94) were inversely associated with breast cancer in EA women (Table 3). Also, among EA women, consuming oven-broiled chicken once per week was associated with reduced odds of breast cancer (OR: 0.64; 95% CI 0.44, 0.94), while there was no association for higher intake of greater than once per week (OR: 1.25; 95% CI 0.75, 2.09), compared to no intake. Some modestly elevated or reduced ORs were observed among AA women but were more imprecise. An increased odds for breast cancer was found for AA women who preferred meat (beef steak, roast, or hamburger) cooked medium to medium well on the inside (OR: 2.77, 95% CI 1.49, 5.14) and well done on the inside (OR: 1.78, 95% CI 1.03, 3.08), when compared to AA women with preference for rare to medium rare doneness. Overall, associations appeared to be stronger among EA women but showed inconsistency within beef and fish categories depending upon cooking method and all diet x race interaction p-values were ≥ 0.05.
Among post-menopausal women, grilled/barbecued hamburger intake (one or more times per week, OR: 1.46; 95% CI 1.05, 2.03) was positively associated with breast cancer in adjusted analyses (Table 4). Pan-fried/oven-broiled beef steak was positively associated with breast cancer among pre-menopausal women (one or more times per week, OR: 1.56; 95% CI 1.08, 2.26). In post-menopausal women, reduced odds of breast cancer were observed for intakes of pan-fried fish (one or more times per week, OR: 0.72; 95% CI 0.52, 0.98), grilled/barbecued fish (one or more times per week, OR: 0.52; 95% CI 0.27, 0.99; p for interaction by menopausal status = 0.01), and for grilled/barbecued pork chops (more than 0 times per week, OR: 0.71, 95% CI 0.56, 0.90). A significant interaction (p = 0.02) between menopausal status and pan-fried/oven-broiled hamburger was observed whereby associations were inverse for pre-menopausal women and positive for post-menopausal women.
When the outcome was restricted to invasive breast cancer (Supplemental Table 1), preference for meat cooked medium to medium well on the inside was associated with increased odds of invasive breast cancer (OR: 1.39; 95% CI 1.02, 1.89) as compared to preference for rare to medium rare doneness. The associations were also assessed by breast cancer ER status as shown in Supplemental Table 2. Compared to no reported meat intake, positive associations for intakes of pan-fried/oven-broiled beef steak were observed for both ER-positive breast cancer (one or more times per week, OR: 1.33; 95% CI 1.01, 1.76) and ER-negative breast cancer (OR: 1.46; 95% CI 1.07, 1.98). An inverse association was also observed for consuming pan-fried fish one or more times per week in ER-positive breast cancer (OR: 0.73; 95% CI 0.55, 0.98) and in ER-negative breast cancer (OR: 0.77; 95% CI 0.55, 1.08) though the confidence interval included the null value. Oven-broiled chicken (less than once per week, OR: 0.69; 95% CI 0.50, 0.94) and grilled/barbecued pork chops (more than 0 times per week, OR: 0.75, 95% CI 0.59, 0.95) were inversely associated with ER-negative breast cancer.
The results were unchanged in sensitivity analyses, additional adjustment was done for meat and fish preparation methods showing significant associations with breast cancer (Supplemental Table 3). The associations were also stratified by fruit and vegetable intake (Supplemental Table 4) and the positive associations observed for pan-fried/oven-broiled beef steak were stronger among low consumers of fruits and vegetables (OR: 1.63; 95% CI 1.10, 2.42) than among moderate or high consumers of fruits and vegetables. The inverse association observed for pan-fried fish was strongest among moderate consumers of fruits and vegetables (OR: 0.59; 95% CI 0.38, 0.91), though interaction p-values were all > 0.20.
Discussion
In this racially diverse, population-based case–control study of women in central and eastern North Carolina, we examined the associations between various preparation methods of meat and fish and breast cancer. More frequent consumption of pan-fried/oven-broiled beef steak or grilled/barbecued hamburger was associated with higher odds of breast cancer. Increased odds of breast cancer were also observed with more frequent consumption of grilled/barbecued hamburger among post-menopausal women and pan-fried/oven-broiled beef steak among pre-menopausal women and among both ER-positive and ER-negative breast cancer subtypes. In contrast, more frequent consumption of pan-fried fish and weekly consumption of grilled/barbecued pork chops were associated with lower odds of breast cancer compared to less frequent consumption and the association was stronger among post-menopausal women. The positive association for pan-fried/oven-broiled beef steak and inverse association for grilled/barbecued pork chops were more pronounced among EA women than among AA women, while the positive association with grilled/barbecued hamburger and inverse association for pan-fried fish were present only among EA women and not among AA women.
The majority of studies that have examined total red meat intake in relation to overall breast cancer have found no or weak associations [21, 26,27,28] but a few found significant positive associations with red and processed meat intake [11, 26, 29, 30]. Many of these studies did not account for preparation methods and doneness levels when collecting data on meat intake. Some studies examining meat preparation methods found increased risk of breast cancer with increasing intake of red and processed meat cooked to well-done by methods that promote carcinogen formation [31,32,33]. Similarly, findings on consumption of meat cooked at high temperature were supported by some [2, 13, 21, 34] but not all studies [32, 35].
In our study, consumption of pan-fried fish once or more per week when compared to no consumption was inversely associated with breast cancer which was consistent with one prior study [36] though was not supported in a meta-analysis [37]. The inverse association may be attributed to the omega-3 polyunsaturated fatty acids (PUFA) contained in fish products which may have anti-inflammatory and other anti-cancer effects, and intake of PUFAs were associated with reduced breast cancer risk in the same meta-analysis [37].
The finding of an inverse association with grilled/barbecued pork chops was unexpected since pork is a red meat. In the South, the term “barbecue” often refers to a marinade-based slow-roasting method unlike the traditional grilling method that can result in charring of the meat surfaces. It has been shown that marinating meat with antioxidant rich marinades prior to grilling may reduce the formation of carcinogens [38, 39]. On the other hand, the use of marinades with a sugar rich base may increase the formation of carcinogens [40]. We hypothesize that women with higher consumption of barbecued pork may be consuming pork in place of other meats that have been cooked with methods that promote carcinogen formation, which may partially explain the inverse associations observed with the consumption of grilled/barbecued pork chops. It is also possible that certain meat products are more commonly prepared at home or served with different vegetables and thus, may be a marker for a healthier diet overall. We did not have data on these dietary patterns and preparation methods to assess this possible explanation.
Our results reported stronger associations among EA women with no statistically significant associations observed among AA women except for preference for medium or well-done meat on the inside. Similarly in previous studies, the risks in AA women were not statistically significant [20, 27] while positive associations were reported in EA women [20]. It is unclear why a differential association was observed between EA and AA women, though other factors may play a larger role in breast cancer risk among AA women such as socioeconomic inequalities and other patterns of risk factors affecting access to health care [41]. Differences in frequencies of polymorphisms in NAT1, NAT2, GSTM1, and GSTT1 genes which encode enzymes involved in detoxification of HCAs may also play a role in the racial differences observed in the associations between meat and fish intake and breast cancer [20, 42]. For example, the stronger associations observed among EA women for grilled/barbecued hamburger or pan-fried/oven-broiled beef steak may be attributed to GSTM1 deletions occurring more frequently in EA women compared to AA women, resulting in reduced ability to detoxify HCAs [43]. In the CBCS, smaller numbers of AA women and greater imprecision of effect estimates may also explain the differential effects observed.
Previous studies observed stronger positive associations for pan-fried meat intake and ER-positive/PR-negative breast tumors [21] and among post-menopausal women [13] consuming grilled/barbecued and smoked meat [15]. Our positive associations observed between breast cancer and red meat consumption were similar in ER-positive and ER-negative tumors and pre- and post-menopausal women. However, pan-fried fish and grilled/barbecued fish were inversely associated with breast cancer among post-menopausal women only.
Carcinogenic combustion byproducts formed during cooking are one plausible biological mechanism underlying these results. HCAs and PAHs are two classes of carcinogens that are formed inside and on the surface of meat when cooked at high temperatures for long periods of time and have been shown in experimental studies to be implicated in DNA damage, promoting the development of mammary cancers [5]. The levels of HCAs formed vary by the preparation method, temperature, preparation time, and type of meat prepared [44]. In particular, pan-frying and grilling are methods that create high levels of HCAs in red meat and the formation of HCAs increases with higher temperatures [44, 45]. PAHs are formed when the smoke produced from drippings of meat prepared on open flame, adhere to meat surfaces [46]. NOCs are carcinogens formed in processed meat and are also produced endogenously through the nitrosylation of heme found in red meat [47,48,49]. We found the strongest positive associations in women reporting high intakes of red meat cooked by pan-frying, oven-broiling or grilled/barbecued, supporting our hypothesis that HCAs and PAHs may play a role in the etiology of human breast cancer. Though a meta-analysis showed increased breast cancer risk with high consumption of processed meat [18], we did not find an association with individual processed meat products (bacon, breakfast sausage, or hot dog). Other plausible mechanisms, most notably that distinct dietary patterns may be associated with intake of specific types of meat, could account for the observed associations.
One limitation of the study is that a complete dietary assessment method was not utilized so we did not have information on total energy intake or on other aspects of the diet besides fruits and vegetables to adjust for potential confounding. It is possible that the relationship between intake of pan-fried or oven-broiled beef steak and breast cancer could be confounded by total energy intake given that obesity, as a surrogate for high energy intake, is an established risk factor for post-menopausal breast cancer and may also be correlated with meat intake. Though we queried about several types of meats, cooking methods, and doneness preferences, a validated method such as that developed by Sinha et al. [50] which utilizes color photographs of meats at varying levels of doneness was not utilized in this study. Future studies of cooked meat and cancer may benefit from using the color photographs to more accurately estimate exposure to cooked meat carcinogens. Given the retrospective nature of the case–control study design, recall bias is also a possibility in this study. The diagnosis of disease may cause breast cancer cases to recall cooked meat intake differently than controls, resulting in differential misclassification of the exposure which could bias the effect estimates. A strength of our study is the oversampling of AA women and women younger than 50 years to allow for examination of associations between cooked meat and breast cancer among different racial groups and by menopausal status. However, some subgroup analyses (e.g., by race and ER status) were limited by sample size resulting in imprecision.
In conclusion, we found a modest increased risk of breast cancer in women consuming beef at least once per week prepared in ways that enhance carcinogen formation compared to non-consumers, and a reduced risk of breast cancer for higher intake of fish or barbecued pork. The results build upon the evidence for a role of meat and fish intake in the etiology of breast cancer and are consistent with dietary guidelines aimed at reducing fried or broiled red meat intake and increasing fish intake for cancer prevention.
Data availability
Data from the Carolina Breast Cancer Study can be requested from study investigators at the following: https://unclineberger.org/cbcs/for-researchers/data-sharing/.
Abbreviations
- AA:
-
African American
- BMI:
-
Body mass index
- CBCS:
-
Carolina Breast Cancer Study
- CI:
-
Confidence interval
- CIS:
-
Carcinoma in situ
- DAG:
-
Directed acyclic graph
- DCIS:
-
Ductal carcinoma in situ
- EA:
-
European American
- ER:
-
Estrogen receptor
- HCA:
-
Heterocyclic amines
- HER:
-
Human epidermal growth factor receptor
- IHC:
-
Immunohistochemistry
- LCIS:
-
Lobular carcinoma in situ
- NOCs:
-
N-Nitroso compounds
- OR:
-
Odds ratio
- PAH:
-
Polycyclic aromatic hydrocarbons
- PR:
-
Progesterone receptor
- PUFA:
-
Polyunsaturated fatty acid
References
Siegel RL, Miller KD, Fuchs HE, Jemal A (2021) Cancer statistics. CA Cancer J Clin 71(1):7–33. https://doi.org/10.3322/caac.21654
Boldo E, Castello A, Aragones N, Amiano P, Perez-Gomez B, Castano-Vinyals G, Martin V, Guevara M, Urtiaga C, Dierssen-Sotos T, Fernandez-Tardon G, Moreno V, Solans M, Peiro R, Capelo R, Gomez-Acebo I, Castilla J, Molina AJ, Castells X, Altzibar JM, Lope V, Kogevinas M, Romieu I, Pollan M (2018) Meat intake, methods and degrees of cooking and breast cancer risk in the MCC-Spain study. Maturitas 110:62–70. https://doi.org/10.1016/j.maturitas.2018.01.020
Wu J, Zeng R, Huang J, Li X, Zhang J, Ho JC, Zheng Y (2016) Dietary protein sources and Incidence of Breast Cancer: A Dose-Response Meta-Analysis of Prospective Studies. Nutrients. https://doi.org/10.3390/nu8110730
International Agency for Research on Cancer (2018) Red meat and processed meat. For more information contact publications@iarc.fr. International Agency for Research on Cancer, Lyon
Papaioannou MD, Koufaris C, Gooderham NJ (2014) The cooked meat-derived mammary carcinogen 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine (PhIP) elicits estrogenic-like microRNA responses in breast cancer cells. Toxicol Lett 229(1):9–16. https://doi.org/10.1016/j.toxlet.2014.05.021
White AJ, Bradshaw PT, Herring AH, Teitelbaum SL, Beyea J, Stellman SD, Steck SE, Mordukhovich I, Eng SM, Engel LS, Conway K, Hatch M, Neugut AI, Santella RM, Gammon MD (2016) Exposure to multiple sources of polycyclic aromatic hydrocarbons and breast cancer incidence. Environ Int 89–90:185–192. https://doi.org/10.1016/j.envint.2016.02.009
Clarke RE, Dordevic AL, Tan SM, Ryan L, Coughlan MT (2016) Dietary Advanced Glycation End Products and Risk Factors for Chronic Disease: A Systematic Review of Randomised Controlled Trials. Nutrients 8(3):125. https://doi.org/10.3390/nu8030125
Uribarri J, Cai W, Sandu O, Peppa M, Goldberg T, Vlassara H (2005) Diet-derived advanced glycation end products are major contributors to the body’s AGE pool and induce inflammation in healthy subjects. Ann N Y Acad Sci 1043:461–466. https://doi.org/10.1196/annals.1333.052
Omofuma OO, Turner DP, Peterson LL, Merchant AT, Zhang J, Steck SE (2020) Dietary Advanced Glycation End-products (AGE) and Risk of Breast Cancer in the Prostate, Lung, Colorectal and Ovarian Cancer Screening Trial (PLCO). Cancer Prev Res (Phila) 13(7):601–610. https://doi.org/10.1158/1940-6207.CAPR-19-0457
Peterson LL, Park S, Park Y, Colditz GA, Anbardar N, Turner DP (2020) Dietary advanced glycation end products and the risk of postmenopausal breast cancer in the National Institutes of Health-AARP Diet and Health Study. Cancer 126(11):2648–2657. https://doi.org/10.1002/cncr.32798
Inoue-Choi M, Sinha R, Gierach GL, Ward MH (2016) Red and processed meat, nitrite, and heme iron intakes and postmenopausal breast cancer risk in the NIH-AARP Diet and Health Study. Int J Cancer 138(7):1609–1618. https://doi.org/10.1002/ijc.29901
Lo JJ, Park YM, Sinha R, Sandler DP (2020) Association between meat consumption and risk of breast cancer: Findings from the Sister Study. Int J Cancer 146(8):2156–2165. https://doi.org/10.1002/ijc.32547
Fu Z, Deming SL, Fair AM, Shrubsole MJ, Wujcik DM, Shu XO, Kelley M, Zheng W (2011) Well-done meat intake and meat-derived mutagen exposures in relation to breast cancer risk: the Nashville Breast Health Study. Breast Cancer Res Treat 129(3):919–928. https://doi.org/10.1007/s10549-011-1538-7
Guo J, Wei W, Zhan L (2015) Red and processed meat intake and risk of breast cancer: a meta-analysis of prospective studies. Breast Cancer Res Treat 151(1):191–198. https://doi.org/10.1007/s10549-015-3380-9
Steck SE, Gaudet MM, Eng SM, Britton JA, Teitelbaum SL, Neugut AI, Santella RM, Gammon MD (2007) Cooked meat and risk of breast cancer–lifetime versus recent dietary intake. Epidemiology 18(3):373–382. https://doi.org/10.1097/01.ede.0000259968.11151.06
Wu K, Sinha R, Holmes MD, Giovannucci E, Willett W, Cho E (2010) Meat mutagens and breast cancer in postmenopausal women–a cohort analysis. Cancer Epidemiol Biomark Prev 19(5):1301–1310. https://doi.org/10.1158/1055-9965.epi-10-0002
Alexander DD, Morimoto LM, Mink PJ, Cushing CA (2010) A review and meta-analysis of red and processed meat consumption and breast cancer. Nutr Res Rev 23(2):349–365. https://doi.org/10.1017/s0954422410000235
Farvid MS, Stern MC, Norat T, Sasazuki S, Vineis P, Weijenberg MP, Wolk A, Wu K, Stewart BW, Cho E (2018) Consumption of red and processed meat and breast cancer incidence: a systematic review and meta-analysis of prospective studies. Int J Cancer 143(11):2787–2799. https://doi.org/10.1002/ijc.31848
Wang Y, Beydoun MA, Caballero B, Gary TL, Lawrence R (2010) Trends and correlates in meat consumption patterns in the US adult population. Public Health Nutr 13(9):1333–1345. https://doi.org/10.1017/s1368980010000224
Chandran U, Zirpoli G, Ciupak G, McCann SE, Gong Z, Pawlish K, Lin Y, Demissie K, Ambrosone CB, Bandera EV (2013) Racial disparities in red meat and poultry intake and breast cancer risk. Cancer Causes Control 24(12):2217–2229. https://doi.org/10.1007/s10552-013-0299-5
Larsson SC, Bergkvist L, Wolk A (2009) Long-term meat intake and risk of breast cancer by oestrogen and progesterone receptor status in a cohort of Swedish women. Eur J Cancer (Oxf, Engl 1990) 45(17):3042–3046. https://doi.org/10.1016/j.ejca.2009.04.035
Newman B, Moorman PG, Millikan R, Qaqish BF, Geradts J, Aldrich TE, Liu ET (1995) The Carolina Breast Cancer Study: integrating population-based epidemiology and molecular biology. Breast Cancer Res Treat 35(1):51–60
Weinberg CR, Wacholder S (1990) The design and analysis of case-control studies with biased sampling. Biometrics 46(4):963–975
Weinberg CR, Sandler DP (1991) Randomized recruitment in case-control studies. Am J Epidemiol 134(4):421–432
Carey LA, Perou CM, Livasy CA, Dressler LG, Cowan D, Conway K, Karaca G, Troester MA, Tse CK, Edmiston S, Deming SL, Geradts J, Cheang MC, Nielsen TO, Moorman PG, Earp HS, Millikan RC (2006) Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. JAMA 295(21):2492–2502. https://doi.org/10.1001/jama.295.21.2492
Anderson JJ, Darwis NDM, Mackay DF, Celis-Morales CA, Lyall DM, Sattar N, Gill JMR, Pell JP (2018) Red and processed meat consumption and breast cancer: UK Biobank cohort study and meta-analysis. Eur J Cancer (Oxf, Engl 1990) 90:73–82. https://doi.org/10.1016/j.ejca.2017.11.022
Genkinger JM, Makambi KH, Palmer JR, Rosenberg L, Adams-Campbell LL (2013) Consumption of dairy and meat in relation to breast cancer risk in the Black Women’s Health Study. Cancer Causes Control (CCC) 24(4):675–684. https://doi.org/10.1007/s10552-013-0146-8
Holmes MD, Colditz GA, Hunter DJ, Hankinson SE, Rosner B, Speizer FE, Willett WC (2003) Meat, fish and egg intake and risk of breast cancer. Int J Cancer 104(2):221–227. https://doi.org/10.1002/ijc.10910
Diallo A, Deschasaux M, Latino-Martel P, Hercberg S, Galan P, Fassier P, Alles B, Gueraud F, Pierre FH, Touvier M (2018) Red and processed meat intake and cancer risk: results from the prospective NutriNet-Sante cohort study. Int J Cancer 142(2):230–237. https://doi.org/10.1002/ijc.31046
Han MA, Zeraatkar D, Guyatt GH, Vernooij RWM, El Dib R, Zhang Y, Algarni A, Leung G, Storman D, Valli C, Rabassa M, Rehman N, Parvizian MK, Zworth M, Bartoszko JJ, Lopes LC, Sit D, Bala MM, Alonso-Coello P, Johnston BC (2019) Reduction of red and processed meat intake and cancer mortality and incidence: a systematic review and meta-analysis of cohort studies. Ann Intern Med 171(10):711–720. https://doi.org/10.7326/M19-0699
Dai Q, Shu XO, Jin F, Gao YT, Ruan ZX, Zheng W (2002) Consumption of animal foods, cooking methods, and risk of breast cancer. Cancer Epidemiol Biomark Prev 11(9):801–808
Delfino RJ, Sinha R, Smith C, West J, White E, Lin HJ, Liao SY, Gim JS, Ma HL, Butler J, Anton-Culver H (2000) Breast cancer, heterocyclic aromatic amines from meat and N-acetyltransferase 2 genotype. Carcinogenesis 21(4):607–615. https://doi.org/10.1093/carcin/21.4.607
Zheng W, Gustafson DR, Sinha R, Cerhan JR, Moore D, Hong CP, Anderson KE, Kushi LH, Sellers TA, Folsom AR (1998) Well-done meat intake and the risk of breast cancer. J Natl Cancer Inst 90(22):1724–1729. https://doi.org/10.1093/jnci/90.22.1724
Pala V, Krogh V, Berrino F, Sieri S, Grioni S, Tjonneland A, Olsen A, Jakobsen MU, Overvad K, Clavel-Chapelon F, Boutron-Ruault MC, Romieu I, Linseisen J, Rohrmann S, Boeing H, Steffen A, Trichopoulou A, Benetou V, Naska A, Vineis P, Tumino R, Panico S, Masala G, Agnoli C, Engeset D, Skeie G, Lund E, Ardanaz E, Navarro C, Sanchez MJ, Amiano P, Svatetz CA, Rodriguez L, Wirfalt E, Manjer J, Lenner P, Hallmans G, Peeters PH, van Gils CH, Bueno-de-Mesquita HB, van Duijnhoven FJ, Key TJ, Spencer E, Bingham S, Khaw KT, Ferrari P, Byrnes G, Rinaldi S, Norat T, Michaud DS, Riboli E (2009) Meat, eggs, dairy products, and risk of breast cancer in the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort. Am J Clin Nutr 90(3):602–612. https://doi.org/10.3945/ajcn.2008.27173
Gertig DM, Hankinson SE, Hough H, Spiegelman D, Colditz GA, Willett WC, Kelsey KT, Hunter DJ (1999) N-acetyl transferase 2 genotypes, meat intake and breast cancer risk. Int J Cancer 80(1):13–17
Kim J, Lim SY, Shin A, Sung MK, Ro J, Kang HS, Lee KS, Kim SW, Lee ES (2009) Fatty fish and fish omega-3 fatty acid intakes decrease the breast cancer risk: a case-control study. BMC Cancer 9:216. https://doi.org/10.1186/1471-2407-9-216
Zheng JS, Hu XJ, Zhao YM, Yang J, Li D (2013) Intake of fish and marine n-3 polyunsaturated fatty acids and risk of breast cancer: meta-analysis of data from 21 independent prospective cohort studies. BMJ (Clin Res Ed) 346:f3706. https://doi.org/10.1136/bmj.f3706
Smith JS, Ameri F, Gadgil P (2008) Effect of marinades on the formation of heterocyclic amines in grilled beef steaks. J Food Sci 73(6):T100-105
Viegas O, Yebra-Pimentel I, Martinez-Carballo E, Simal-Gandara J, Ferreira IM (2014) Effect of beer marinades on formation of polycyclic aromatic hydrocarbons in charcoal-grilled pork. J Agric Food Chem 62(12):2638–2643. https://doi.org/10.1021/jf404966w
Nerurkar PV, Le Marchand L, Cooney RV (1999) Effects of marinating with Asian marinades or western barbecue sauce on PhIP and MeIQx formation in barbecued beef. Nutr Cancer 34(2):147–152. https://doi.org/10.1207/s15327914nc3402_4
Newman LA, Kaljee LM (2017) Health disparities and triple-negative breast cancer in African American women: a review. JAMA Surg 152(5):485–493. https://doi.org/10.1001/jamasurg.2017.0005
Rebbeck TR (1997) Molecular epidemiology of the human glutathione S-transferase genotypes GSTM1 and GSTT1 in cancer susceptibility. Cancer Epidemiol Biomark Prev 6(9):733–743
Cotton SC, Sharp L, Little J, Brockton N (2000) Glutathione S-transferase polymorphisms and colorectal cancer: a HuGE review. Am J Epidemiol 151(1):7–32. https://doi.org/10.1093/oxfordjournals.aje.a010124
Sinha R, Rothman N, Salmon CP, Knize MG, Brown ED, Swanson CA, Rhodes D, Rossi S, Felton JS, Levander OA (1998) Heterocyclic amine content in beef cooked by different methods to varying degrees of doneness and gravy made from meat drippings. Food Chem Toxicol 36(4):279–287
Skog K, Steineck G, Augustsson K, Jagerstad M (1995) Effect of cooking temperature on the formation of heterocyclic amines in fried meat products and pan residues. Carcinogenesis 16(4):861–867. https://doi.org/10.1093/carcin/16.4.861
Larsson BK (1986) Formation of polycyclic aromatic hydrocarbons during the smoking and grilling of food. Prog Clin Biol Res 206:169–180
Cross AJ, Pollock JR, Bingham SA (2003) Haem, not protein or inorganic iron, is responsible for endogenous intestinal N-nitrosation arising from red meat. Cancer Res 63(10):2358–2360
Joosen AM, Kuhnle GG, Aspinall SM, Barrow TM, Lecommandeur E, Azqueta A, Collins AR, Bingham SA (2009) Effect of processed and red meat on endogenous nitrosation and DNA damage. Carcinogenesis 30(8):1402–1407. https://doi.org/10.1093/carcin/bgp130
Kuhnle GG, Story GW, Reda T, Mani AR, Moore KP, Lunn JC, Bingham SA (2007) Diet-induced endogenous formation of nitroso compounds in the GI tract. Free Radic Biol Med 43(7):1040–1047. https://doi.org/10.1016/j.freeradbiomed.2007.03.011
Sinha R, Rothman N (1997) Exposure assessment of heterocyclic amines (HCAs) in epidemiologic studies. Mutat Res 376(1–2):195–202
Acknowledgements
We are grateful to CBCS participants and study staff.
Funding
This work was supported by a Susan G. Komen Graduate Training in Disparities Research Grant (GTDR17500160; SES, OOO) and a Cancer Prevention Research Fellowship from the American Society of Preventive Oncology and the Prevent Cancer Foundation (SES); This research was supported by a grant from UNC Lineberger Comprehensive Cancer Center, which is funded by the University Cancer Research Fund of North Carolina, the Susan G Komen Foundation, the National Cancer Institute of the National Institutes of Health (P01CA151135), and the National Cancer Institute Specialized Program of Research Excellence (SPORE) in Breast Cancer (NIH/NCI P50-CA58223). This research recruited participants and/or obtained data with the assistance of Rapid Case Ascertainment, a collaboration between the North Carolina Central Cancer Registry and UNC Lineberger. RCA is supported by a grant from the National Cancer Institute of the National Institutes of Health (P30CA016086). We are grateful to CBCS participants and study staff.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data analysis was performed by Omonefe Omofuma. The first draft of the manuscript was written by Omonefe Omofuma and all authors commented on subsequent versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving research study participants were approved by the Institutional Review Board at the University of North Carolina at Chapel Hill (UNC IRB#92-0410). The current analyses of deidentified existing data were reviewed by the University of South Carolina Institutional Review Board and declared not human subjects research (#PR00074227).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Omofuma, O.O., Steck, S.E., Olshan, A.F. et al. The association between meat and fish intake by preparation methods and breast cancer in the Carolina Breast Cancer Study (CBCS). Breast Cancer Res Treat 193, 187–201 (2022). https://doi.org/10.1007/s10549-022-06555-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-022-06555-x