Abstract
Purpose
Increasingly epidemiological evidence supports that environmental factors are associated with breast cancer (BC) outcomes after a BC diagnosis. Although evidence suggests that air pollution exposure is associated with higher mortality in women with BC, studies investigating potential mechanisms have been lacking.
Methods
We evaluated women with BC (N = 151) attended at the National Cancer Institute–Mexico from 2012 to 2015. We calculated 1-year average exposures to particulate matter < 2.5 μm (PM2.5) at home address before diagnosis. We used linear and logistic regression models to determine the associations between PM2.5 exposure and BC aggressiveness (tumor size, molecular phenotype).
Results
Average annual PM2.5 exposure of this population was 23.0 μg/m3 [standard deviation (SD)]: 1.90 μg/m3]. PM2.5 levels were positively correlated with tumor size at diagnosis (r = 0.22; p = 0.007). Multivariable linear models had a similar inference [risk ratio (RR): 1.32; 95% confidence interval (95% CI): 1.04, 1.674]. We did not observe differences in this association by age or menopause status. Further, women with triple-negative BC (TNBC) had significantly higher PM2.5 levels compared with other phenotypes (p = 0.015). Multivariable-adjusted logistic regression models assessing the association between PM2.5 and tumor size had a similar inference (RR 1.41; 95% CI 1.05, 1.89) overall for all ages and also for women who were ≤ 50 years old at diagnosis (RR 1.63; 95% CI 1.036, 2.57).
Conclusions
Our findings suggest a significant association between long-term PM2.5 exposure and BC aggressiveness based on tumor size and phenotype, as well as a worse outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite improvements in overall survival after diagnosis, breast cancer (BC) remains a major cause of death worldwide, with more than 627,000 estimated deaths in 2018 [1]. Recent reports have shown increases in age-specific and stage-specific BC incidence in the US [2]. However, the annual increase in BC, particularly in women < 50 years old [2], cannot be explained by increasing lifespan or changes in parity, a long-established risk factor for BC [3]. Thus, changes in other risk factors and environmental exposures may be related to these secular trends [4].
Air pollution is considered the world’s most massive single environmental health risk [5]. Air pollution contains suspended particles or particulate matter (PM) as well as secondary contaminants. In 2013, PM was classified as carcinogenic to humans and a causative agent of lung cancer [6]. Further, the ESCAPE study showed a clear association between PM10 and PM2.5 exposure and incident lung adenocarcinoma [7]. This evidence is consistent with the fact that lungs are the organ most directly affected by air pollutants. Yet, extensive evidence describes systemic effects of air pollution, particularly low-grade systemic inflammation and oxidative stress—both mechanisms linked to cancer progression [8].
Higher air pollution may be linked with increased cancer mortality. For example, long-term (1-year) PM2.5 exposure was associated with all-cancer mortality, mainly from BC in women and lung cancer [9]. Similarly, a Japanese study revealed a higher BC mortality [10] as well as in the US [11]. These findings suggest that long-term PM exposure during carcinogenesis and once cancer is established may have direct and indirect effects contributing to cell proliferation, invasiveness, and potentially metastasis, including in BC. However, the specific contributions of PM2.5 to BC worse outcomes have not been determined. This study aimed to determine the specific contributions of long-term PM2.5 on breast cancer patients.
Methods
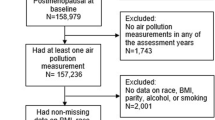
Population
The cohort included patients with locally advanced breast cancer and advanced breast cancer treated at the National Cancer Institute in Mexico City. Patients were recruited from 2012 to 2015. Inclusion criteria were individuals who had histopathological confirmation of stage I–IV breast adenocarcinoma, were ≥ 18 years of age, lived in Mexico City for at least 1 year before diagnosis, and had not received previous cancer treatment. The exclusion criterion was histopathological confirmation of a diagnosis different from adenocarcinoma. The total eligible population included in the study was 151 women and they were followed up until March 2020 (5–8 years of follow-up). Socioeconomic status was obtained from the social worker's initial review based on income and home characteristics and classified as follows: level 1 (lowest stratum) to level 5 (highest stratum).
Determining long-term PM2.5 exposure before BC diagnosis
Long-term (1-year average) PM2.5 exposure was established using high-resolution satellite aerosol optical depth measurements for 1 × 1 km2 grids [12]. The daily prediction model used calibrations using municipal ground monitors (≥ 18 h available collected on Tapered Element Oscillating Microbalance devices), land use, and meteorological features. Mexico City Atmospheric Monitoring System (SIMAT) provided meteorological stations and networks, including temperature and humidity data for the final prediction model. The exposure for each patient was obtained using their home address from 1 year before diagnosis. Our study included the region of Mexico City between the longitudes of − 99.42 to − 98.67 W and latitudes of 19.09–19.77 N. To avoid the mountainous uninhabited area to the southeast and east of the city, we delimited the study area to the valley adjacent to Mexico City.
Clinical and histopathological characteristics of BC patients
We obtained and registered all available clinical characteristics (e.g., tumor size, stage, body mass index, lymph node status) in research datasets. Histopathological assessment of the initial biopsies was done by expert pathologists and included type, grade [according to the Nottingham classification using the Scarff–Bloom–Richardson (SBR) scale as a surrogate and obtained for every sample included], presence of inflammatory cells, presence or absence of in situ components, lymphovascular invasion, perineural invasion, and other parameters. Cell proliferation markers Ki67 (anti-Ki67, RTU, clone MIB-1; Dako North America, CA, USA) were evaluated using standard immunohistochemical protocols. In brief, in full histologic sections, at least three high-power (× 40 objective) fields were selected to represent the spectrum of staining seen on initial overview of the whole section. We use the invasive edge of the tumor and only nuclear staining was considered positive and counting at least 500 malignant invasive cells. Three independent observers assessed the immunostaining. Cell proliferation index was calculated according to the presence of Ki67 as the ratio of positively stained nuclei to total nuclei in malignant cells.
Statistical analyses
For descriptive analyses, we determined the measures of central tendency and variability of all variables included. We examined correlation between PM2.5 levels and the values of continuous variables. Subsequently, multivariable-adjusted analysis was performed using logistic (i.e., triple-negative phenotype) and linear (i.e., tumor size at diagnosis), to determine the associations between PM2.5 exposure and the characteristic of worse prognosis. We adjusted the models for potential confounders, including age and body mass index (as a continuous variables), socioeconomic status [low (levels 1 and 2) vs. high (levels 3, 4, and 5)], family history of BC (present vs. absent), smoking status (positive vs negative, anytime before diagnosis), and histologic grade [low and intermediate (SBR < 8) vs. high grade (SBR ≥ 8)]. We also tested for linearity of the associations for continuous variables and explored the role of categorized age (> 50 vs. ≤ 50 years) and menopause (present vs absent at diagnosis) in subanalyses. All analyses were run using R studio software (R Project for Statistical Computing, CRAN, The Comprehensive R Archive Network, Vienna).
Results
Population and PM2.5 levels
A total of 151 women diagnosed with BC living in Mexico City and treated at the National Cancer Institute—Mexico were included. Mean age was 51.9 years (SD 11.0 years). The population included a high frequency of overweight (BMI > 25) and obese (BMI > 30) individuals (33.8 and 38.4%, respectively), with a mean of 29.0 kg/m2 (SD 5.9 kg/m2). The frequency of comorbidity was 13.9% for type two diabetes mellitus. Mean tumor size at diagnosis was 6.4 cm, and the most frequent clinical stage was IIIA (38.7%) (Table 1). BC patients lived in heterogeneous locations within the city (Fig. 1). Long-term PM2.5 estimations indicated a mean concentration of 23.0 µg/m3 (SD 1.9 µg/m3), with a normal distribution (p = 0.11, Shapiro–Wilk Test, Supplementary Fig. 1).
Association between long-term PM2.5 exposure and clinical characteristics
We observed positive correlation between long-term PM2.5 exposure and tumor size at diagnosis (Pearson correlation coefficient, r = 0.22; p = 0.007) (Supplementary Fig. 2). Subsequently, a multivariable linear regression model adjusted for age, socioeconomic status, Ki67, histological grade, and smoking status indicated an independent linear association between long-term PM2.5 exposure and tumor size at diagnosis [Risk Ratio (RR): 1.39; 95% CI 1.10, 1.76; p = 0.007] (Table 2, Supplementary Figs. 2, 3). According to these results, for every increase of two standard deviations (3.88 µg/m3) in long-term PM2.5 exposure, BC tumors increased by 0.8 cm. Analysis by subgroups did not show a clear effect on younger (RR 1.31; 95% CI 0.99, 1.73; p = 0.06) but a significant effect on postmenopausal women (RR 1.49; 95% CI 1.04, 2.13; p = 0.028). No significant association was observed related to clinical stage (p = 0.94), or node status (p = 0.61).
Association between long-term PM2.5 exposure and histopathological characteristics
We did not find a significant association with long-term PM2.5 exposure (p = 0.87) or Ki67 levels (p = 0.09). We did not observe any significant association regarding pathologic complete response (pCR) in the subset of patients (n = 100) who received neoadjuvant chemotherapy (p = 0.63). Five intrinsic BC subtypes are characterized based on estrogen and progesterone receptors (ER, PR) and the human epidermal growth factor receptor 2 (HER2-enriched). Compared with other subtypes (luminal A, luminal B, and HER2−enriched), triple-negative BC (TNBC; ER−/PR−/HER2−) represents around 15% of all BC and confers a worse prognosis. Long-term PM2.5 levels were not associated with luminal A (23.1%; p = 0.74), luminal B (53.6%; p = 0.28), or HER2+ phenotype (10.5%; p = 0.69). However, TNBC patients (12.5%) had a median exposure of 24.10 µg/m3 [interquartile range (IQR): 1.19 µg/m3], which was significantly higher than other phenotypes (median: 22.80 µg/m3; IQR 1.17 µg/m3; p = 0.015) (Supplementary Fig. 4). This association was evident in multivariable-adjusted models (RR 1.59; 95% CI 1.13, 2.23; p = 0.008) (Table 3) adjusted for age, family history of breast cancer, histologic grade, socioeconomic status, and smoking. Remarkably, this effect was stronger and statistically significant in younger women (RR 2.182; 95% CI 1.15, 4.14; p = 0.035). We also found a significant association in premenopausal women (RR 1.90; 95% CI 1.008, 3.58; p = 0.047). Exploring differences in molecular subtypes according to clinical stage potentially related to our finding in TNBC, we found significant differences for luminal A-like, but not for TNBC (p = 0.67, Supplementary Table 1).
Cross-effect of outcomes linked to long-term PM2.5 exposure
Using sensitivity models, we explored whether significant outcomes associated with long-term PM2.5 exposure influenced the observed effects. We found that the effect of long-term PM2.5 exposure on tumor size at diagnosis was independent of molecular phenotype (i.e., TNBC), keeping consistency of the estimates and statistical association. For the association between long-term PM2.5 exposure and TNBC, we did not found changes in the estimates, and the statistical significance remained (p = 0.011) (Table 4).
Effect of long-term PM2.5 exposure, tumor size, and TNBC on overall survival
We did not observe any significant association between long-term PM2.5 exposure and relapse-free and overall survival (p > 0.05 for both analyses, log-rank test; Fig. 2a). We also did not find a significant association between tumor size and relapse-free and overall survival (p > 0.05). However, we observed an expected significant association between TNBC and overall survival (p < 0.001; Fig. 2b), even with a low number of deaths (n = 19) at the time of analysis.
Discussion
We observed an association between higher long-term PM2.5 exposure levels (1-year average) and larger tumors at diagnosis as well as higher risk of TNBC. Both factors are related to poor prognosis in BC patients, particularly those with TNBC. TNBC generally shows aggressive biological and clinical characteristics, including earlier onset of metastatic disease, visceral metastases, rapidly progressive disease, short response duration to available therapies, and inferior survival outcomes [13]. TNBC is a heterogeneous subtype of breast cancer that is beginning to be refined by its molecular characteristics and clinical response to a targeted therapeutic approach [14]. TNBC represents 15% of all breast cancers. However, its prevalence varies in different settings, with the highest prevalence of 39% of breast cancers in premenopausal African American women compared to 13% in all women in the US [15]. TNBC confers a poor prognosis, mainly because it cannot be treated with endocrine or anti-HER2 therapy; hence, chemotherapy appears to be the only available treatment modality [16]. Other factors linked to TNBC include higher body mass index during premenopausal years, higher parity, and lower lifetime duration of breastfeeding [17]. Probably, most relevant finding linked to the association between air pollution and TNBC phenotype is BRCA1 mutations. More than 75% of tumors arising in women carrying a BRCA1 mutation have TNBC and a basal-like phenotype (one of five intrinsic subgroups of breast cancer), although most TNBC tumors are not mutated for BRCA1 [18].
Air pollution components including polycyclic aromatic hydrocarbons as benzo(a)pyrene, 3 dioxins, sulfur-containing compounds (SO3, H2SO4), and 3-nitrobenzanthron have been shown to be mutagenic in human cells, with a clear dose–response relationship [19]. However, the direct effects of PM on epithelial cells are unlikely to induce mutagenesis. Still, indirect effects (e.g., low-grade inflammation or oxidative damage) can cause DNA damage, adducts, and mutations. Inflammation generates reactive oxygen and nitrogen species, which can help combat pathogens and stimulate tissue repair and regeneration. However, these species can also damage DNA, which, in turn, can promote mutations that initiate and promote cancer [20]. If air pollution contributes to TNBC, as suggested by our results, BRCA1 mutations might be a plausible pathway. To our knowledge, this is the first evidence of an association between air pollution and BC phenotypes, particularly TNBC.
In countries with limited economic and health resources, BC is usually diagnosed in advanced stages leading to worse outcomes including higher mortality. Further, air pollution is strongly linked to poverty [21]. Evidence suggests that nearly 92% of pollution-related deaths occur in low- and middle-income countries [22]. Our study found an association between long-term PM2.5 levels and tumor size at diagnosis, suggesting potential co-occurrence of late or absent screening in this population as well as a potential contribution to cell proliferation or inhibition of cell death facilitated by air pollution [23]. Experimental studies observed that tumor growth occurs in an exponential or Gompertzian manner, and cells die by apoptosis in each generation; some cells undergo senescence, while others are eliminated by the immune system [24]. Therefore, transformed cells need several divisions to form a macroscopic tumor, thus requiring a more extended time window than afforded by this study (1 year before diagnosis). In addition, in vitro evidence suggests that air pollution components may exert an effect on cell proliferation as well as on apoptosis and may justify our finding related to tumor size, with stronger and significant effect in postmenopausal women [25].
Hypotheses and evidence about the carcinogenic mechanism of suspended particles abound, including release of cytokines and induction of oxidative stress, activation of signaling pathways mediated by microRNA dysregulation, promotion of angiogenesis through upregulation of vascular endothelial growth factor, and p53 mutations [26]. Our findings might suggest that long-term PM exposure can generate a microenvironment favoring cancer cell proliferation, although the mechanisms underlying this potential association as well as in vitro demonstration are needed. Further studies about other factors linked to air pollution and late diagnosis (e.g., poverty, low education level) are also needed.
Mexico City is one of the largest cities in the world [27] with a population exceeding 20 million and with heavy vehicular traffic, responsible for emission of > 220 tons/month of suspended particles. The geographic characteristics of the region [28] result in PM2.5 levels higher than most US and European urban areas [12], and frequent environmental emergencies arise due to air pollution in Mexico City. This highly polluted environment poses higher risks to all citizens, but our findings suggest an effect on patients with breast cancer and potentially on other cancer patients.
Suspended particles are responsible for several harmful health effects. In urban areas, fossil fuels are the primary source of these particles, mainly from transportation, power stations, and factories. Reducing the levels of particulate contamination after sustained interventions (especially policies and regulation) is associated with improved public health, although the potential oncological effect has not been determined. In 2009, Pope et al. analyzed PM2.5 data from 51 cities. After adjusting for other risk factors, they found that reduction of PM2.5 levels during 1980–2000 was strongly associated with an overall increase of 2.7 years in life expectancy [14]. Likewise, the SAPALIDIA study conducted in Switzerland in 1991–2002 analyzed lung diseases in adults from eight communities and showed that decreased annual mean concentrations of PM10 levels by 5–6 μg/m3 attenuated the yearly rate of lung function decline. These data suggest that continued improvement of air quality is needed to decrease morbidity and mortality associated with exposure to suspended particles. Our results open exciting avenues into whether reducing air pollution may mitigate worse outcomes and mortality in cancer patients.
Our study has some limitations including limited statistical power and inability to control for some confounding by factors derived from the geographic region (Mexico City), which might be correlated with both exposure and lack of BC screening and thus with tumor size at diagnosis. Our findings may also be influenced by other factors not included in the final multivariable models (e.g., diet, educational level) because of power limitations. Other limitations of this study are that we only explored the effect of PM2.5 exposure, but ambient air pollution combines several different pollutants and mixtures, including metals, polycyclic aromatic hydrocarbons, and gases. However, this is one of the first studies conducted focusing on cancer outcomes and tumor characteristics, which lays foundations to continue exploring the effects of other environmental pollutants such as PM10, ozone, endocrine disruptors, or metals on the clinical, pathological, and molecular characteristics of BC patients. Lack of generalizability is also a concern, and our results may not be applicable to other patients. However, to study a homogeneous ethnical population so well characterized as ours, may gives light about air pollution effects that can be applicable to other ethnicities and geographical areas.
To conclude, our study provides the first evidence of an effect of long-term PM2.5 exposure (1 year before diagnosis) on specific clinical and pathological characteristics, including larger breast tumors and triple-negative phenotype. These characteristics are associated with poor prognosis in women with BC. Future prospective studies with higher statistical power in other populations are needed to confirm and generalize our findings.
Data availability
The data (identified participant data and data dictionary) that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
References
Bray F, Ferlay J, Soerjomataram I et al (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424. https://doi.org/10.3322/caac.21492
Kehm RD, Yang W, Tehranifar P, Terry MB (2019) 40 years of change in age- and stage-specific cancer incidence rates in US women and men. JNCI Cancer Spectr. https://doi.org/10.1093/jncics/pkz038
Lima SM, Kehm RD, Swett K et al (2020) Trends in parity and breast cancer incidence in US women younger than 40 years from 1935 to 2015. JAMA Netw Open. https://doi.org/10.1001/jamanetworkopen.2020.0929
Terry MB, Michels KB, Brody JG et al (2019) Environmental exposures during windows of susceptibility for breast cancer: a framework for prevention research. Breast Cancer Res BCR. https://doi.org/10.1186/s13058-019-1168-2
World Health Organization 7 million premature deaths annually linked to air pollution. In: Media Cent. https://www.who.int/mediacentre/news/releases/2014/air-pollution/en/. Accessed 2 Sep 2019
Loomis D, Grosse Y, Lauby-Secretan B et al (2013) The carcinogenicity of outdoor air pollution. Lancet Oncol 14:1262–1263. https://doi.org/10.1016/S1470-2045(13)70487-X
Raaschou-Nielsen O, Andersen ZJ, Beelen R et al (2013) Air pollution and lung cancer incidence in 17 European cohorts: prospective analyses from the European Study of Cohorts for Air Pollution Effects (ESCAPE). Lancet Oncol 14:813–822. https://doi.org/10.1016/S1470-2045(13)70279-1
Fiorito G, Vlaanderen J, Polidoro S et al (2018) Oxidative stress and inflammation mediate the effect of air pollution on cardio- and cerebrovascular disease: a prospective study in nonsmokers. Environ Mol Mutagen 59:234–246. https://doi.org/10.1002/em.22153
Wong CM, Tsang H, Lai HK et al (2016) Cancer mortality risks from long-term exposure to ambient fine particle. Cancer Epidemiol Prev Biomark 25:839–845. https://doi.org/10.1158/1055-9965.EPI-15-0626
Iwai K, Mizuno S, Miyasaka Y, Mori T (2005) Correlation between suspended particles in the environmental air and causes of disease among inhabitants: cross-sectional studies using the vital statistics and air pollution data in Japan. Environ Res 99:106–117. https://doi.org/10.1016/j.envres.2004.11.004
Hu H, Dailey AB, Kan H, Xu X (2013) The effect of atmospheric particulate matter on survival of breast cancer among US females. Breast Cancer Res Treat 139:217–226. https://doi.org/10.1007/s10549-013-2527-9
Just AC, Wright RO, Schwartz J et al (2015) Using high-resolution satellite aerosol optical depth to estimate daily PM2.5 geographical distribution in Mexico city. Environ Sci Technol 49:8576–8584. https://doi.org/10.1021/acs.est.5b00859
Dent R, Trudeau M, Pritchard KI et al (2007) Triple-negative breast cancer: clinical features and patterns of recurrence. Clin Cancer Res 13:4429–4434. https://doi.org/10.1158/1078-0432.CCR-06-3045
Lyons TG (2019) Targeted therapies for triple-negative breast cancer. Curr Treat Options Oncol 20:82. https://doi.org/10.1007/s11864-019-0682-x
Carey LA, Perou CM, Livasy CA et al (2006) Race, breast cancer subtypes, and survival in the carolina breast cancer study. JAMA 295:2492–2502. https://doi.org/10.1001/jama.295.21.2492
Brenton JD, Carey LA, Ahmed AA, Caldas C (2005) Molecular classification and molecular forecasting of breast cancer: ready for clinical application? J Clin Oncol 23:7350–7360. https://doi.org/10.1200/JCO.2005.03.3845
Millikan RC, Newman B, Tse C-K et al (2008) Epidemiology of basal-like breast cancer. Breast Cancer Res Treat 109:123–139. https://doi.org/10.1007/s10549-007-9632-6
Rakha EA, Reis-Filho JS, Ellis IO (2008) Basal-like breast cancer: a critical review. J Clin Oncol 26:2568–2581. https://doi.org/10.1200/JCO.2007.13.1748
Feretti D, Pedrazzani R, Ceretti E et al (2019) “Risk is in the air”: polycyclic aromatic hydrocarbons, metals and mutagenicity of atmospheric particulate matter in a town of Northern Italy (Respira study). Mutat Res 842:35–49. https://doi.org/10.1016/j.mrgentox.2018.11.002
Kay J, Thadhani E, Samson L, Engelward B (2019) Inflammation-induced DNA damage, mutations and cancer. DNA Repair 83:102673. https://doi.org/10.1016/j.dnarep.2019.102673
Mehta S, Sbihi H, Dinh TN et al (2014) Effect of poverty on the relationship between personal exposures and ambient concentrations of air pollutants in Ho Chi Minh City. Atmos Environ 95:571–580. https://doi.org/10.1016/j.atmosenv.2014.07.011
Landrigan PJ, Fuller R, Acosta NJR et al (2018) The lancet commission on pollution and health. Lancet 391:462–512. https://doi.org/10.1016/S0140-6736(17)32345-0
Environment UN (2019) Air pollution hurts the poorest most. In: UN Environ. http://www.unenvironment.org/news-and-stories/story/air-pollution-hurts-poorest-most. Accessed 11 Jun 2020
Retsky MW, Swartzendruber DE, Wardwell RH, Bame PD (1990) Is Gompertzian or exponential kinetics a valid description of individual human cancer growth? Med Hypotheses 33:95–106. https://doi.org/10.1016/0306-9877(90)90186-I
Novack L, Yitshak-Sade M, Landau D et al (2016) Association between ambient air pollution and proliferation of umbilical cord blood cells. Environ Res 151:783–788. https://doi.org/10.1016/j.envres.2016.09.009
Wei H, Liang F, Cheng W et al (2017) The mechanisms for lung cancer risk of PM2.5: induction of epithelial-mesenchymal transition and cancer stem cell properties in human non-small cell lung cancer cells. Environ Toxicol 32:2341–2351. https://doi.org/10.1002/tox.22437
Vega E, Eidels S, Ruiz H et al (2010) Particulate air pollution in Mexico city: a detailed view. Aerosol Air Qual Res 10:193–211. https://doi.org/10.4209/aaqr.2009.06.0042
Molina LT, Molina MJ (2004) Improving air quality in megacities: Mexico City case study. Ann N Y Acad Sci 1023:142–158. https://doi.org/10.1196/annals.1319.006
Acknowledgements
We thank Clementina Castro for critical revision of this manuscript.
Funding
This work was supported by the National Institutes of Health (R01ES025225, P30ES009089 Baccarelli; R21ES027087 Prada and Baccarelli), Breast Cancer Foundation (Terry), and Consejo Nacional de Ciencia y Tecnología (FOSISS 2017-289503 Prada; FOSISS 2017-90412 Pérez; FOSISS 2018-A3-S-49533 Caro).
Author information
Authors and Affiliations
Contributions
DP and AAB designed the study and the statistical analysis; LV and PC collected clinical data and discussed the results; AJ and IK contributed air pollution modeling; DP, AAB, and MBT contributed with statistical modeling and analyses; HC contributed pathologic analysis of samples; DP, AAB, MBT, CGC, YS, DeP, RC, CC, JDC, AMG, DCL, LAH, and EB contributed to discussion of results and preparation of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
This study was conducted following the Declaration of Helsinki, all patients provided written informed consent, and the study was approved by the IRB (Comité de Investigación y Comité de Ética en Investigacion—Instituto Nacional de Cancerología, 012/048/IMO/CB/806).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Prada, D., Baccarelli, A.A., Terry, M.B. et al. Long-term PM2.5 exposure before diagnosis is associated with worse outcome in breast cancer. Breast Cancer Res Treat 188, 525–533 (2021). https://doi.org/10.1007/s10549-021-06167-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-021-06167-x