Abstract
Background
Neoadjuvant chemotherapy (NACT) is a cornerstone in managing breast cancer. There is no defined consensus on the optimal time between NACT and surgery. We analyze the effect of time between the end of NACT and surgery on overall survival (OS) and disease-free survival (DFS) in breast cancer patients who received NACT followed by surgery.
Methods
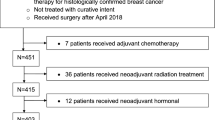
This is a retrospective analysis of 468 patients with breast cancer (stage I–III) who received and completed the same regimen of NACT (Anthracyclines and Taxanes B27 protocol) at King Hussein Cancer Center (KHCC) (2006–2014). Patients have been divided into three groups according to the duration between the end of NACT and surgery, <4 weeks, 4–8 weeks and >8 weeks.
Results
Most patients were stages II–III breast cancer with only four patients with stage I. Almost all patients (99%) had either invasive ductal or invasive lobular carcinomas. Adjuvant radiotherapy was given to 96% of patients. Most patients were alive at the time of analysis (84%).
Complete pathological response was achieved in 20% of patients. Local recurrence rate was 6.6% with a median follow up of 3.8 years (interquartile range 0.6–10.9). Analysis showed that the groups had equivalent DFS. However, OS was adversely affected if patients had their surgery after 8 weeks of NACT compared to those who had their surgery between 4 and 8 weeks.
Conclusions
Breast cancer surgery post NACT within the first 8 weeks had no impact on survival. However, surgery after 8 weeks of NACT showed negative impact on OS. Therefore, delaying surgery after 8 weeks is not recommended.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The utilization of neoadjuvant chemotherapy (NACT) in breast cancer has been well established, especially after randomized controlled trials showing equal outcomes in survival compared to adjuvant chemotherapy [1, 2]. Not only did NACT allow downsizing the tumor in a group of patients who were otherwise not suitable for breast conservation [3], it also assisted in testing the tumor biology in vivo which allowed the evaluation of systemic therapy effects and tumor response. Furthermore, it has also allowed downstaging the clinically positive axilla in exceptional responders, thus performing less morbid surgeries [4, 5].
In Jordan, breast cancer is the most common cancer and the leading cause of cancer-related mortality in women, comprising 19.7% of all diagnosed cancer cases [6]. Moreover, about a third of patients present with locally advanced and or metastatic disease at a median age of 50, which is about a decade earlier than in the west. This makes the use of NACT more paramount in our population [7, 8]. The B-27 protocol (anthracycline taxanes) NACT has been used in our Jordanian patients with established efficacy and safety [9].
Limited data is available regarding the optimal timing to perform surgery after completing NACT, and major studies that addressed this issue showed contrasting results [10,11,12,13]. However, several published studies investigated the suitable time to initiate adjuvant chemotherapy, which lead several bodies of oncology to propose not delaying systemic adjuvant chemotherapy more than 6 weeks post-surgery [14,15,16,17,18,19].
In this retrospective comparative study, we aim to find the optimal time between completing NACT and having the surgery in relation to disease-free (DFS) and overall survival (OS).
Methods
Patient population
A retrospective chart review of 468 patients treated with NACT followed by surgery at King Hussein Cancer Center (KHCC) between 2006 and 2014. All patients had pathologically proven breast cancer, who received and completed the same regimen of NACT (B27 protocol [1]). Anti-Her2 agent (Trastuzumab) was added if the patients were eligible. Patients with de novo metastasis were excluded. Time to surgery was defined as the duration between the last cycle of NACT and the date of tumor removal. All patients were discussed in our specialized breast cancer multidisciplinary meeting, where recommendations were reached based on mammograms, histology and clinical presentation.
The study was conducted at KHCC Amman, Jordan, approved by the Institutional Review Board (IRB) with approval Number (17 KHCC 49).
Operative technique
All patients who underwent curative surgery were included in our analysis irrespective of the surgical technique involved.
Data collection and follow up
Patient demographics and medical histories were extracted pre-chemotherapy. We followed up with our patients with six monthly mammograms for 2 years and then every year thereafter and an annual computed tomography chest/abdomen/pelvis for 5 years.
Patients were divided into three groups according to the time to surgery: group 1: <4 weeks; group 2: 4–8 weeks; and group 3: >8 weeks. DFS and OS were calculated from the date of diagnosis to the date of recurrence or death, respectively.
Statistical analysis
Patients’ characteristics such as histology, stage and hormone status were presented in terms of counts and percentages. Duration between NACT and surgery was divide into three sequenced ranges based on ROC optimal thresholds and AUC. Accordingly, duration between NACT and surgery (<4, 4–8 and ≥8 weeks) was compared using Chi-square test, Fishers exact or Wilcoxon rank as appropriate and based on each assumption. DFS and OS were presented by Kaplan Meier curves and the comparisons were performed using Log Rank test. Significant factors were included in Cox regression and Adjusted Hazards ratios, their 95% CI and Adjusted p values were reported. All analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC).
Results
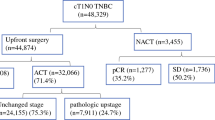
The analysis included 468 patients who underwent NACT followed by surgery between 2006 and 2014. Seventy-five patients (16%) were dead at the time of the analysis. Complete pathological response was achieved in 20% of patients, the local recurrence rate was 6.6% (n = 31) and the distant metastasis rate was 22% (n = 102). Median follow up for the whole cohort was 46 months (interquartile range 7–131). There were 142 patients in the <4 weeks group, 284 patients in the 4–8 weeks group, and 42 patients in the >8 weeks group. Their clinical characteristics are shown in Table 1. The three groups were not statistically different regarding age, cancer histology, grade, hormonal receptor status, the use of adjuvant hormonal or radiotherapy or the pathologic complete response (pCR). And the <4 weeks groups had more percentage of patients with lymphovascular invasion (LVI) (p < 0.03) and long duration of follow up (median) 4.6 years with (p = 0.022) and the >8 weeks group had fewer patients who initially presented with stage III breast cancer (p < 0.0001).
The 5-year survival rates were 89%, 77%, and 85.6% for the groups <4 weeks, 4–8 weeks and >8 weeks, respectively. The Kaplan Meier curves for OS and DFS for all groups are shown in Figs. 1 and 2.
In the univariable analysis, Table 2, TNM clinical and pathological stage, LVI, nuclear grade, pathological response and Hormonal receptor status affected DFS. Whereas time to surgery, TNM clinical and pathological stage, LVI, nuclear grade and Hormonal receptor status were statistically significant factors for OS. Breast reconstruction did not have an influence on DFS nor OS.
In the multivariate Cox regression, Table 3, only the presenting clinical stage (III vs. I/II) and LVI were shown to be associated with worse OS, whereas in DFS, grade, LVI and the clinical stage were shown to be significant detrimental factors. Time to surgery did not have an influence on neither DFS nor OS.
In comparing the groups’ OS and DFS (Tables 4 and 5, respectively), patients who underwent surgery beyond 8 weeks post NACT had worse OS than the 4–8 weeks group.
Discussion and conclusion
This retrospective comparative study aims to study the effect of time of breast cancer surgery after NACT on patients’ survival. Our data showed that when comparing patients who had surgery beyond 8 weeks to patients who had the surgery between 4 and 8 weeks, the former group showed worse OS. Also, when the >8 weeks group was compared to the combined cohort of <8 weeks post treatment, there was a statistical trend towards worse OS.
Scheduling patients who completed NACT for surgery is dictated by many factors; toxicity from chemotherapy, which was shown to be the major cause of delay to surgery [3], patients’ medical status and anxiety can play a role in delaying surgery. In addition, operating theatre slot availability and surgical waiting lists might also be taken into consideration.
In the literature, there is no clear-cut evidence on the optimal time to perform the surgery post NACT.
A published study by Sanford et al. was the first to address this issue [10]. It was a retrospective review of 1101 patients diagnosed with stages I, II and III. Time between NACT and surgery was categorized as <4 weeks (30.4% of patients), 4–6 weeks (47.6%), or >6 weeks (22%). The 5-year OS estimate was 79%, 87% and 81% respectively (p = 0.03). They did not find a difference between the three groups in terms of DFS. Patients who underwent surgery at ≤4 or >6 weeks had worse OS but not DFS.
Another study from Modena Italy showed a better OS and DFS outcome if surgery was performed before the end of 3 weeks post treatment. However the groups were mismatched in number [11]. Authors from the Kaiser Permanente Los Angeles Medical Center conducted their own review on 58 patients and found that delaying surgery beyond 60 days affects recurrence but not survival [12].
As far as we know, this is the second analysis of its kind in our region, the Middle East, outside of Europe and the United States. One of our aims was to know if findings could be replicated in our specific cohort of patients.
The retrospective nature of this study may have an adverse impact on the outcome especially with a small sample size in the >8 weeks group. It is also a single center experience and overgeneralizing results should be taken with caution. Theoretically to define the optimal time post NACT to surgery, prospective randomized trials are needed which are perhaps very difficult to conduct as they may harbor ethical issues.
With the limited data available on the subject, delaying surgery up to 8 weeks does not impact outcomes and this might give surgeons reassurance regarding scheduling their patients for surgery.
Data availability
The datasets generated during and analysed during the current study are available from the corresponding author on reasonable request.
References
Rastogi P, Anderson S, Bear H, Geyer C, Kahlenberg M, Robidoux A, Margolese R, Hoehn J, Vogel V, Dakhil S, Tamkus D, King K, Pajon E, Wright M, Robert J, Paik S, Mamounas E, Wolmark N (2008) Preoperative chemotherapy: updates of National Surgical Adjuvant Breast and Bowel Project Protocols B-18 and B-27. J Clin Oncol 26:778–785. https://doi.org/10.1200/jco.2007.15.0235
Mauri D, Pavlidis N, Ioannidis J (2005) Neoadjuvant versus adjuvant systemic treatment in breast cancer: a meta-analysis. J Natl Cancer Inst 97:188–194. https://doi.org/10.1093/jnci/dji021
Mieog J, van der Hage J, van de Velde C (2007) Neoadjuvant chemotherapy for operable breast cancer. Br J Surg 94:1189–1200. https://doi.org/10.1002/bjs.5894
Kuehn T, Bauerfeind I, Fehm T, Fleige B, Hausschild M, Helms G, Lebeau A, Liedtke C, Minckwitz G, Nekljudova V, Schmatloch S, Schrenk P, Staebler A, Untch M (2013) Sentinel-lymph-node biopsy in patients with breast cancer before and after neoadjuvant chemotherapy (SENTINA): a prospective, multicentre cohort study. Lancet Oncol 14:609–618. https://doi.org/10.1016/s1470-2045(13)70166-9
Boughey J (2013) Sentinel lymph node surgery after neoadjuvant chemotherapy in patients with node-positive breast cancer. JAMA 310:1455. https://doi.org/10.1001/jama.2013.278932
Ministry of Health | Cancer incidence in Jordan 2013. Moh.gov.jo. https://moh.gov.jo/. Accessed 18 Dec 2016
El Saghir N, Khalil M, Eid T, El Kinge A, Charafeddine M, Geara F, Seoud M, Shamseddine A (2007) Trends in epidemiology and management of breast cancer in developing Arab countries: a literature and registry analysis. Int J Surg 5:225–233. https://doi.org/10.1016/j.ijsu.2006.06.015
Chouchane L, Boussen H, Sastry K (2013) Breast cancer in Arab populations: molecular characteristics and disease management implications. Lancet Oncol 14:e417–e424. https://doi.org/10.1016/s1470-2045(13)70165-7
Abdel-Razeq H, Marei L, Saadeh S, Abdulelah H, Abu-Nasser M, Salam M, Daana W, Al-Haj Ali B, Taqash A (2017) From clinical trials to clinical practice: outcome of NSABP-B27 neoadjuvant chemotherapy regimen for high-risk early-stage breast cancer. Breast Cancer Res Treat 165:771–777. https://doi.org/10.1007/s10549-017-4359-5
Sanford R, Lei X, Barcenas C, Mittendorf E, Caudle A, Valero V, Tripathy D, Giordano S, Chavez-MacGregor M (2015) Impact of time from completion of neoadjuvant chemotherapy to surgery on survival outcomes in breast cancer patients. Ann Surg Oncol 23:1515–1521. https://doi.org/10.1245/s10434-015-5020-3
Omarini C, Guaitoli G, Noventa S, Andreotti A, Gambini A, Palma E, Papi S, Tazzioli G, Balduzzi S, Dominici M, Cascinu S, Piacentini F (2017) Impact of time to surgery after neoadjuvant chemotherapy in operable breast cancer patients. Eur J Surg Oncol 43:613–618. https://doi.org/10.1016/j.ejso.2016.09.020
Lin J, Anna L (2018) Clinical impact of delaying surgery in patients undergoing neoadjuvant chemotherapy on breast cancer recurrence and survival. J Glob Oncol 4:70s. https://doi.org/10.1200/jgo.18.27800
Suleman K, Almalik O, Haque E, Mushtaq A, Badran A, Alsayed A, Ajarim D, Al-Tweigeri T, Jastaniyah N, Elhassan T, Alkhayal W (2020) Does the timing of surgery after neoadjuvant therapy in breast cancer patients affect the outcome? Oncology 98:168–173. https://doi.org/10.1159/000504964
Jara Sánchez C, Ruiz A, Martín M, Antón A, Munárriz B, Plazaola A, Schneider J, del Prado P, Alba E, Fernández-Aramburo A (2006) Influence of timing of initiation of adjuvant chemotherapy over survival in breast cancer: a negative outcome study by the Spanish Breast Cancer Research Group (GEICAM). Breast Cancer Res Treat 101:215–223. https://doi.org/10.1007/s10549-006-9282-0
Cold S, Düring M, Ewertz M, Knoop A, Møller S (2005) Does timing of adjuvant chemotherapy influence the prognosis after early breast cancer? Results of the Danish Breast Cancer Cooperative Group (DBCG). Br J Cancer 93:627–632. https://doi.org/10.1038/sj.bjc.6602734
Shannon C, Ashley S, Smith I (2003) Does timing of adjuvant chemotherapy for early breast cancer influence survival? J Clin Oncol 21:3792–3797. https://doi.org/10.1200/jco.2003.01.073
Gagliato D, Gonzalez-Angulo A, Lei X, Theriault R, Giordano S, Valero V, Hortobagyi G, Chavez-MacGregor M (2014) Clinical impact of delaying initiation of adjuvant chemotherapy in patients with breast cancer. J Clin Oncol 32:735–744. https://doi.org/10.1200/jco.2013.49.7693
Senkus E, Kyriakides S, Ohno S, Penault-Llorca F, Poortmans P, Rutgers E, Zackrisson S, Cardoso F (2015) Primary breast cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 26:v8–v30. https://doi.org/10.1093/annonc/mdv298
Ditsch N, Untch M, Thill M, Müller V, Janni W, Albert U, Bauerfeind I, Blohmer J, Budach W, Dall P, Diel I, Fasching P, Fehm T, Friedrich M, Gerber B, Hanf V, Harbeck N, Huober J, Jackisch C, Kolberg-Liedtke C, Kreipe H, Krug D, Kühn T, Kümmel S, Loibl S, Lüftner D, Lux M, Maass N, Möbus V, Müller-Schimpfle M, Mundhenke C, Nitz U, Rhiem K, Rody A, Schmidt M, Schneeweiss A, Schütz F, Sinn H, Solbach C, Solomayer E, Stickeler E, Thomssen C, Wenz F, Witzel I, Wöckel A (2019) AGO recommendations for the diagnosis and treatment of patients with early breast cancer: update 2019. Breast Care 14(4):224–245
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
MA-M declares that he has no conflict of interest. BA declares that he has no conflict of interest. HA-N declares that he has no conflict of interest. TA-S declares that he has no conflict of interest. No funding to declare, the authors are employed at KHCC where this research was carried out.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional review board (IRB) at King Hussein Cancer Center (KHCC) with IRB approval # 17KHCC49.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Al-Masri, M., Aljalabneh, B., Al-Najjar, H. et al. Effect of time to breast cancer surgery after neoadjuvant chemotherapy on survival outcomes. Breast Cancer Res Treat 186, 7–13 (2021). https://doi.org/10.1007/s10549-020-06090-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-020-06090-7