Abstract
Background
Compared to tamoxifen, adjuvant treatment with aromatase inhibitors improves disease outcomes of postmenopausal women with hormone receptor-positive early breast cancer. In the international, randomized, double-blind BIG 1-98 trial, 8010 women were randomized to receive tamoxifen, letrozole, or sequential use of the agents for 5 years. With a focus on switching between agents, we investigated cardiovascular events over the entire 5-year treatment period.
Methods
Of the 6182 patients enrolled, 6144 started trial treatment and were included in this analysis. Adverse events occurring during study treatment until 30 days after cessation were considered. Eight cardiovascular event types were defined. Cumulative incidence of events were estimated using the Kaplan–Meier method, without consideration for competing events. Multivariable Cox models estimated hazard ratios (HR) with 95% confidence intervals (CI) for pairwise comparisons of treatment arms.
Results
While on study treatment, 6.5% of patients (n = 397) had any cardiac events reported; for 2.4%, the event was grades 3–5, of which 11 (0.2%) were grade 5. Letrozole monotherapy was associated with higher risk of grade 1–5 ischemic heart disease (HR = 1.81; 95% CI, 1.06–3.08) compared with tamoxifen monotherapy. Patients assigned sequential tamoxifen →letrozole (HR = 1.59; 95% CI, 0.92–2.74) or sequential letrozole → tamoxifen (HR = 1.20; 95% CI, 0.68–2.14) showed a lesser degree of risk elevation. Patients assigned to tamoxifen-containing regimens had significantly higher risk of grade 1–5 thromboembolic events (tamoxifen monotherapy HR = 2.10; 95% CI, 1.42–3.12; tamoxifen → letrozole HR = 1.96; 95% CI, 1.32–2.92; letrozole → tamoxifen HR = 1.56; 95% CI 1.03–2.35) as compared with patients assigned letrozole alone.
Conclusion
When initiating or switching between adjuvant endocrine treatments in postmenopausal patients, age and medical history, with special attention to prior cardiovascular events, should be balanced with expected benefit of the treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Aromatase inhibitors (AIs) improve disease outcomes, as compared with tamoxifen, among postmenopausal women with hormone receptor-positive early breast cancer and have become the standard of care [1]. The four-arm, randomized, double-blind, phase III BIG 1-98 trial, which compared 5 years of adjuvant letrozole versus tamoxifen versus their sequences, was one of the trials establishing the role of AIs in this population [2,3,4,5,6,7,8]. Letrozole improved disease-free survival, overall survival, distant recurrence-free interval, and breast cancer-free interval as compared with tamoxifen after median follow-up of 8.1 years [6] and with longer follow-up [8]. The safety profiles of the 4 treatment regimens differ substantially, in particular for the incidence of musculoskeletal events, gynecological and vasoactive symptoms, and cardiovascular events. Women assigned to sequential treatment with tamoxifen followed by letrozole (tamoxifen → letrozole) more frequently discontinued treatment (17.9% by 5 years) after switching because of adverse events when compared to the other 3 treatment arms. The letrozole-containing treatment arms had comparable rates of discontinuation up to 2 years (time of treatment switch in sequential arms), after which, the rates of discontinuation in the sequential arms increased [9].
The initial report of BIG 1-98 [2] described an increased number of thromboembolic AEs in patients assigned tamoxifen and a small increase in some types and grades of cardiac AEs in patients assigned letrozole. A more detailed report, after a median follow-up of 30 months [10], documented a low overall incidence of cardiovascular AEs, which differed between treatment arms. The current study investigates the effects of these treatment regimens on cardiovascular events over the entire 5-year treatment period, with particular focus on the effects of switching between the two agents.
Methods
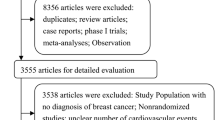
BIG 1-98 is an international, multicenter, randomized, double-blind, phase III trial that enrolled 8010 postmenopausal women with hormone receptor-positive operable invasive breast cancer [6]. Initially, between 1998 and 2000, 1828 women were randomly assigned to receive monotherapy with letrozole (2.5 mg orally daily) or tamoxifen (20 mg orally daily) for 5 years. Beginning in 1999 until 2003, 6182 women were randomly assigned to one of four arms: monotherapy with tamoxifen or letrozole for 5 years or sequential therapy consisting of letrozole for 2 years followed by tamoxifen for 3 years, or tamoxifen for 2 years followed by letrozole for 3 years. In this study, we focused on patients enrolled during the 4-arm randomization period. Patients who never started trial treatment were excluded.
During trial drug administration, AEs were reported for each 6-month period using checkboxes on the case report forms while grading used the National Cancer Institute’s (NCI) Common Toxicity Criteria Version 2.0. The following targeted cardiovascular AEs were explicitly collected on the case report forms: myocardial infarction, cerebrovascular accident (CVA)/transient ischemic attack (TIA), angina requiring PTCA (percutaneous transluminal coronary angioplasty) or CABG (coronary artery bypass grafting), thromboembolic event, and hypercholesterolemia. Other AEs were collected using an open-text comment field for specification by the investigator. Open-text fields were reviewed and coded according to MedDRA preferred terms by medical reviewers at the International Breast Cancer Study Group (IBCSG) Coordinating Center as part of the standard procedures of this double-blind trial. Three additional groups of events were identified: cardiac failure, other cardiovascular event, and hypertension.
For the current study, AEs that occurred during the study treatment, or up to 30 days after patients discontinued treatment, were considered in order to define eight cardiovascular event types. We determined the worst grade of any cardiac event reported, which included reports of ischemic heart disease (including myocardial infarction, coronary artery disease, and angina), arrhythmia and cardiac arrest, cardiac failure, cardiopathy, valvular disease/large vessel disease, ECG changes (such as electrical conduction blocks and bradycardia), sudden cardiac death, and cardiac NOS. The maximum grade of other cardiovascular events was determined from AE reports coded as cardiovascular NOS or other vascular. The highest grades of hypercholesterolemia, hypertension, and CVA/TIA (only grades 3–5 were recorded) were each determined from a single coded AE type. We determined the highest grade of thromboembolic events, including reports of thromboembolism, deep vein thrombosis, phlebitis, and thrombosis.
We further determined the time to first event of each cardiovascular event type, defined as time from randomization to the first report of the specific event type, or censored at 30 days after the last dose of study treatment. For CVA/TIA, time to first grade 3–5 event was examined. For other events, time to both first grades 1–5 and first grades 3–5 was examined. Patients randomized to receive five years of tamoxifen, but who chose to cross over to letrozole subsequent to the publication of initial efficacy results, were included in the analysis only while on tamoxifen.
The baseline patient characteristics that were potential risk factors for developing cardiovascular events, including history of previous cardiovascular events, were summarized according to treatment groups. Cumulative incidence of events of interest was estimated using the Kaplan–Meier method; no competing events were considered. Multivariate Cox proportional hazards models were used to estimate hazard ratios (HR) with 95% confidence intervals (CI) for pairwise comparisons of treatment arms and to test for differences between treatment groups using a 3-degree of freedom Wald test. The models were adjusted for age at randomization (> 65 years vs ≤ 65 years), body mass index (normal vs. overweight vs. obese), history of any cardiac events, CVA/TIA events, hypercholesterolemia, hypertension, thromboembolic events, and other cardiovascular events. Ischemic heart disease and cardiac failure are subevents of any cardiac event, and therefore, prior histories of these events were not included individually in the multivariate models.
Hazard rates for events of interest within a time interval were calculated using the maximum likelihood estimate from a piecewise exponential model. These estimates (reported per 100 person-years) are number of events occurring within that time interval divided by the total patient time at risk during that time interval. A constant hazard was estimated within each time interval, and tests comparing hazards between time intervals or between treatment arms were based on normal approximation of the difference between estimates.
There was no adjustment of p-values for multiple testing.
Results
Patients
Of the 6182 patients randomized during the 4-arm option, 6144 patients started trial treatment and were included in this analysis. The median follow-up of the patients is 45.8 months. In the population, 30.0% of patients were over age 65, 34.2% were overweight and 20.4% obese, and 17.6% were current smokers, while 18.9% were former smokers (Table 1). History of hypertension was frequent, reported for 32.3% of patients, 13.3% had history of hypercholesterolemia, and 6.0% of patients had history of prior cardiac events. Prior thromboembolic events were reported for 3.3% and CVA/TIA for 1.3% of patients. Medical histories were well balanced across the four treatment arms (Fig. 1).
While on study treatment, 6.5% of patients had any cardiac events reported; for 2.4% of patients, the event was grades 3–5, of which 11 (0.2%) were grade 5 (Table 2). Ischemic heart disease was reported for 2.0% of patients (1.2% grades 3–5) and cardiac failure for 1.0% of patients (0.5% grades 3–5). Results of the multivariate Cox models are shown in Supplemental (S) tables online. No difference among treatment arms was observed in time to any grade 1–5 cardiac event (Fig. 2a; adjusted overall p = 0.33; Table S1), but differences emerged for time to any grade 3–5 cardiac events (Fig. 2b, adjusted overall p = 0.05). After adjustment for baseline risk factors, letrozole monotherapy was associated with significantly higher risk of any grade 3–5 cardiac event (HR = 1.83; 95% CI, 1.14–2.93) compared to tamoxifen monotherapy more so than sequential therapy (relative to tamoxifen monotherapy, tamoxifen → letrozole HR = 1.18; 95% CI, 0.71–1.96; letrozole → tamoxifen HR = 1.24; 95% CI 0.75–2.06). Age older than 65, smoking history and obesity at randomization (p < 0.001, p = 0.004, p = 0.004, respectively) and history of prior CVA/TIA, any prior cardiac event, and hypertension (p = 0.03, p < 0.001, p = 0.006, respectively) were associated with higher risk of any grade 3–5 cardiac event during treatment (Table S2).
Cumulative incidences plots of events of a time to any grade 1–5 cardiac events, b time to any grade 3–5 cardiac events, c time to any grade 1–5 ischemic heart disease, d time to any grade 3–5 ischemic heart disease, e time to any grade 1–5 cardiac failure, and f time to any grade 3–5 cardiac failure. No competing events were considered. Tam tamoxifen, Let letrozole, → indicates sequence of 2 years of one agent followed by 3 years of the other agent
For the specific cardiac events, differences among treatment groups were more apparent, including time to grade 1–5 ischemic heart disease (Fig. 2c; adjusted overall p = 0.12, Table S3) and grade 3–5 ischemic heart disease (Fig. 2d; adjusted overall p = 0.17, Table S4). After adjustment for baseline risk factors, including age older than 65, obesity, history of any prior cardiac events, and hypertension (p < 0.0001, p = 0.03, p = 0.02 and p = 0.03, respectively; Table S3), letrozole monotherapy was associated with higher risk of grade 1–5 ischemic heart disease (HR = 1.81; 95% CI, 1.06–3.08) compared with tamoxifen monotherapy. This association was observed to a lesser degree among patients on sequential tamoxifen → letrozole (HR = 1.59; 95% CI, 0.92–2.74) but not for those on sequential letrozole → tamoxifen (HR = 1.20; 95% CI, 0.68–2.14). Similar results were observed for grade 3–5 ischemic heart disease (Table S4).
For patients who received sequential tamoxifen → letrozole, the hazard of grade 1–5 ischemic heart disease was similar while receiving tamoxifen but remained high during subsequent letrozole treatment compared with patients who received tamoxifen monotherapy whose hazard was lower during the later years of tamoxifen monotherapy (hazards 0.047 tamoxifen → letrozole vs 0.044 tamoxifen during the first two years of tamoxifen, p = 0.84; 0.050 tamoxifen → letrozole vs. 0.020 tamoxifen during the subsequent three years, p = 0.008; Fig. 2c). Similarly for patients on sequential letrozole → tamoxifen, the hazard of ischemic heart disease declined and was lower during the subsequent 3 years of tamoxifen compared to patients on 5 years letrozole (hazards 0.042 letrozole → tamoxifen vs 0.047 letrozole during the first two years of letrozole, p = 0.75; 0.029 letrozole → tamoxifen vs 0.055 letrozole during subsequent 3 years, p = 0.06).
For cardiac failure, no statistically significant differences were observed among treatment groups for time to grade 1–5 cardiac failure (Fig. 2e; relative to tamoxifen monotherapy, letrozole monotherapy HR = 1.00, 95% CI 0.50–2.00; tamoxifen → letrozole HR = 0.67, 95% CI 0.31–1.46; and letrozole → tamoxifen HR = 0.88, 95% CI 0.43–1.80, adjusted overall p = 0.73), or for time to grade 3–5 cardiac failure (Fig. 2f; relative to tamoxifen monotherapy, letrozole monotherapy HR = 1.04, 95% CI 0.42–2.57; tamoxifen → letrozole HR = 0.52, 95% CI 0.17–1.57; and letrozole → tamoxifen HR = 0.74, 95% CI 0.27–1.99, adjusted overall p = 0.58).
The time to grade 1–5 hypercholesterolemia differed among groups (Fig. 3a; relative to tamoxifen monotherapy, letrozole monotherapy HR = 2.77, 95% CI 0.2.45–3.14; tamoxifen → letrozole HR = 1.74, 95% CI 1.53–1.98; and letrozole → tamoxifen HR = 2.28, 95% CI 2.00–2.59, adjusted overall p < 0.0001), with incidence rates ranging from 24.5% on tamoxifen monotherapy to 53.2% on letrozole monotherapy. Grade 3–5 hypercholesterolemia only occurred in 23 patients (about 0.4%, Table 2). The reduced incidence of hypercholesterolemia under tamoxifen monotherapy was noted previously [10]. The pattern for grade 1–5 hypercholesterolemia on sequential therapy echoed that of ischemic heart disease. For patients on sequential tamoxifen → letrozole, the hazard of hypercholesterolemia was greater during letrozole treatment compared to tamoxifen monotherapy (hazards 0.76 tamoxifen → letrozole vs 0.89 tamoxifen during the first 2 years of tamoxifen, p = 0.07; 1.46 tamoxifen → letrozole vs 0.35 tamoxifen during the subsequent 3 years, p < 0.001). For patients on sequential letrozole → tamoxifen, the hazard of hypercholesterolemia was lowest during the final 3 years of tamoxifen compared to letrozole monotherapy (hazards 2.45 letrozole → tamoxifen vs 2.55 letrozole during the first 2 years of letrozole, p = 0.48; 0.26 letrozole → tamoxifen vs 0.81 letrozole during the subsequent 3 years, p < 0.001). No differences among treatment groups were observed for time to grade 3–5 hypercholesterolemia (Fig. 3b; relative to tamoxifen monotherapy, letrozole monotherapy HR = 1.56, 95% CI 0.37–6.54; tamoxifen → letrozole HR = 1.59, 95% CI 0.38–6.69; and letrozole → tamoxifen HR = 3.09, 95% CI 0.83–11.5, adjusted overall p = 0.30).
Cumulative incidences plots of events of time to any grade 1–5 hypercholesterolemia, time to grade 3–5 hypercholesterolemia time to any grade 1–5 hypertension, time to any grade 3–5 hypertension time to any grade 1–5 thromboembolic events, and time to any grade 3–5 thromboembolic events. No competing events were considered. Tam tamoxifen, Let letrozole, → indicates sequence of 2 years of one agent followed by 3 years of the other agent
While on treatment, grade 1–5 hypertension was reported for 5.7% of patients (2.2% grades 3–5, Table 2). There were no differences among the treatment groups (Fig. 3c, relative to tamoxifen monotherapy, letrozole monotherapy HR = 0.96, 95% CI 0.71–1.31; tamoxifen → letrozole HR = 1.18, 95% CI 0.87–1.58; and letrozole → tamoxifen HR = 0.96, 95% CI 0.70–1.30, adjusted overall p = 0.47), not for grade 3–5 hypertension (Fig. 3d, relative to tamoxifen monotherapy, letrozole monotherapy HR = 0.95, 95% CI 0.54–1.65; tamoxifen → letrozole HR = 1.54, 95% CI 0.93–2.54; and letrozole → tamoxifen HR = 1.41, 95% CI 0.85–2.35, adjusted overall p = 0.14).
Other cardiovascular events were reported for 0.9% of patients (0.1% grades 3–5). No significant differences were observed among the treatment arms for time to other grade 1–5 cardiovascular events (adjusted overall p = 0.12) nor for time to other grade 3–5 cardiovascular events (adjusted overall p = 0.88).
While on study treatment, 4.1% of patients had any grade 1–5 thromboembolic events reported; for 2.4% of patients, the event was grade 3–5 (Table 2). The time to thromboembolic events differed among the groups both for time to grade 1–5 events (Fig. 3e; adjusted overall p = 0.001, Table S5) and for the subset of grade 3–5 events (Fig. 3f, adjusted overall p = 0.001, Table S6). After adjusting for baseline risk factors (including age over 65 years [p < 0.001], overweight or obesity [p = 0.01], history of prior thromboembolic event [p < 0.001], cardiovascular event [p < 0.001], and hypertension [p = 0.005]), patients on tamoxifen-containing regimens had significantly higher risk of grade 1–5 thromboembolic events (tamoxifen monotherapy HR = 2.10, 95% CI 1.42–3.12; tamoxifen → letrozole HR = 1.96, 95% CI 1.32–2.92; and letrozole → tamoxifen HR = 1.56, 95% CI 1.03–2.35; Table S5) as compared with patients on letrozole monotherapy. Similar results were observed for grade 3–5 thromboembolic events (Table S6). For patients on sequential letrozole → tamoxifen, the hazard of grade 1–5 thromboembolic events increased during the last 3 years on tamoxifen and was higher compared to patients who received letrozole monotherapy (hazards 0.048 letrozole → tamoxifen vs 0.053 letrozole during the first two years of letrozole, p = 0.77; 0.11 letrozole → tamoxifen vs 0.05 letrozole during the subsequent three years, p = 0.002; Fig. 3e). For patients on sequential tamoxifen → letrozole, the hazard of thromboembolic events declined during the last 3 years on letrozole and tended to be lower compared to patients who received tamoxifen monotherapy (hazards 0.17 tamoxifen → letrozole vs 0.14 tamoxifen during the first 2 years of tamoxifen, p = 0.27; 0.04 tamoxifen → letrozole vs 0.07 tamoxifen during the subsequent 3 years, p = 0.07; Fig. 3e).
Grade 3–5 CVA/TIA was reported for 1.7% of patients while on treatment. No differences among the treatment groups were observed for time to CVA/TIA (Fig. 4; relative to tamoxifen monotherapy, letrozole monotherapy HR = 0.87, 95% CI 0.49–1.56; tamoxifen → letrozole HR = 1.18; 95% CI 0.69–2.02; and letrozole → tamoxifen HR = 1.02, 95% CI 0.58–1.78, adjusted overall p = 0.76).
Discussion
In this analysis, we present detailed data about thromboembolic and cardiovascular events occurring during treatment with letrozole and/or tamoxifen in patients enrolled during the 4-arm randomization period of the randomized, double-blind BIG 1-98 trial. No differences were observed in the incidence rate of new or worsening hypertension or in the incidence rate of severe hypercholesterolemia (grade 3 and higher) as well as for CVA/TIA. Cholesterol-lowering medication was initiated more often among patients in the letrozole monotherapy arm compared to the tamoxifen and sequential arms [11]. These findings are in line with the known beneficial effect of tamoxifen on the lipid profile [12], although the role of the different cardiometabolic effects of endocrine treatment is still not fully explained and further studies are needed [13, 14]. As expected, patients treated with tamoxifen alone and tamoxifen followed by letrozole appeared to have a higher incidence of thromboembolic events during treatment with tamoxifen. For patients receiving two years of initial letrozole, the rate of thromboembolic events increased dramatically after they switched to tamoxifen. Patients at risk for such events, in particular those with a history of previous thromboembolic events, hypertension or other cardiovascular disease, should be cautious when considering the use of adjuvant treatment with tamoxifen. Patients on the letrozole monotherapy showed a higher incidence of grade 3–5 cardiac events and of grade 3–5 ischemic heart disease, in particular those over 65 years of age. But, generally the incidence of clinically relevant thromboembolic and cardiovascular events, in particular grade 3 and higher, was low with both drugs and comparable with data from other trials using an AI and tamoxifen [1, 15,16,17,18]; however, these results are sometime inconsistent and the methods used to evaluate the safety are different. In particular the ATAC trial [19] showed no significant difference in the occurrence of ischemic cardiovascular events, but the adverse events were not collected in a systematic predefined way. In a recently published population-based cohort study [20], aromatase inhibitors were associated with increased risks of heart failure and cardiovascular mortality compared with tamoxifen, this confirming the result of a systematic review and meta-analysis of randomized controlled trials and observational studies [21].
BIG1-98 showed a clinically meaningful improved DFS and in OS with IPCW analysis for the use of letrozole especially for patients at higher risk [22, 23]. However, for postmenopausal patients taking adjuvant endocrine treatment, the initial choice of agents, and also switching between endocrine agents, should be considered and balanced with the medical history, with special attention for cardiovascular events and the age of the patient, with the expected benefit of the treatment.
Data availability
The data analyzed during the current study are not publicly available. Access to IBCSG data are contingent upon IBCSG review and approval. To request access to data, contact the IBCSG Statistical Center (stat_center@ibcsg.org)
References
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) (2015) Aromatase inhibitors versus tamoxifen in early breast cancer: patient-level meta-analysis of the randomised trials. Lancet 386:1341–1352
Breast International Group (BIG) 1-98 Collaborative Group. Thurlimann B, Keshaviah A, Coates AS, Mouridsen H, Mauriac L, Forbes JF, Paridaens R, Castiglione-Gertsch M, Gelber RD, Rabaglio M, Smith I, Wardley A, Price KN, Goldhirsch A (2005) A comparison of letrozole and tamoxifen in postmenopausal women with early breast cancer. N Engl J Med 353:2747–2757
Coates AS, Keshaviah A, Thurlimann B, Mouridsen H, Mauriac L, Forbes JF, Paridaens R, Castiglione-Gertsch M, Gelber RD, Colleoni M, Lang I, Del Mastro L, Smith I, Chirgwin J, Nogaret JM, Pienkowski T, Wardley A, Jakobsen EH, Price KN, Goldhirsch A (2007) Five years of letrozole compared with tamoxifen as initial adjuvant therapy for postmenopausal women with endocrine-responsive early breast cancer: update of study BIG 1-98. J Clin Oncol 25:486–492
Giobbie-Hurder A, Price KN, Gelber RD, for the International breast Cancer Study Group and BIG 1-98 Collaborative Group (2009) Design, conduct, and analyses of BIG 1-98 A randomized, double-blind, phase-III study comparing letrozole and tamoxifen as adjuvant endocrine therapy for postmenopausal women with receptor-positive, early breast cancer. Clin Trials 6:272–287
BIG 1-98 Collaborative Group, Mouridsen H, Giobbie-Hurder A, Goldhirsch A, Thurlimann B, Paridaens R, Smith I, Mauriac L, Forbes J, Price KN, Regan MM, Gelber RD, Coates AS (2009) Letrozole therapy alone or in sequence with tamoxifen in women with breast cancer. N Engl J Med 361:766–776
Regan MM, Neven P, Giobbie-Hurder A, Goldhirsch A, Ejlertsen B, Mauriac L, Forbes JF, Smith I, Lang I, Wardley A, Rabaglio M, Price KN, Gelber RD, Coates AS, Thurlimann B, BIG 1-98 Collaborative Group; International Breast Cancer Study Group (IBCSG) (2011) Assessment of letrozole and tamoxifen alone and in sequence for postmenopausal women with steroid hormone receptor-positive breast cancer: The BIG 1-98 randomised clinical trial at 81 years median follow-up. Lancet Oncol 12:1101–1108
Regan MM, Price KN, Giobbie-Hurder A, Thurlimann B, Gelber RD, for the International Breast Cancer Study Group and BIG 1-98 Collaborative Group (2011) Interpreting Breast International Group (BIG) 1-98: a randomized, double-blind, phase III trial comparing letrozole and tamoxifen as adjuvant endocrine therapy for postmenopausal women with hormone receptor-positive, early breast cancer. Breast Cancer Res 13:209
Ruhstaller T, Giobbie-Hurder A, Colleoni M, Jensen MB, Ejlertsen B, de Azambuja E, Neven P, Lang I, Jakobsen EH, Gladieff L, Bonnefoi H, Harvey VJ, Spazzapan S, Tondini C, Del Mastro L, Veyret C, Simoncini E, Gianni L, Rochlitz C, Kralidis E, Zaman K, Jassem J, Piccart-Gebhart M, Di Leo A, Gelber RD, Coates AS, Goldhirsch A, Thurlimann B, Regan MM, and for the members of the BIG 1-98 Collaborative Group and the International Breast Cancer Study Group C ( 201) Adjuvant Letrozole and Tamoxifen Alone or Sequentially for Postmenopausal Women With Hormone Receptor-Positive Breast Cancer: Long-Term Follow-Up of the BIG 1-98 Trial. J Clin Oncol 37:105–114
Chirgwin JH, Giobbie-Hurder A, Coates AS, Price KN, Ejlertsen B, Debled M, Gelber RD, Goldhirsch A, Smith I, Rabaglio M, Forbes JF, Neven P, Lang I, Colleoni M, Thurlimann B (2016) Treatment Adherence and Its Impact on Disease-Free Survival in the Breast International Group 1-98 Trial of Tamoxifen and Letrozole, Alone and in Sequence. J Clin Oncol 34:2452–2459
Mouridsen H, Keshaviah A, Coates AS, Rabaglio M, Castiglione-Gertsch M, Sun Z, Thurlimann B, Mauriac L, Forbes JF, Paridaens R, Gelber RD, Colleoni M, Smith I, Price KN, Goldhirsch A (2007) Cardiovascular adverse events during adjuvant endocrine therapy for early breast cancer using letrozole or tamoxifen: safety analysis of BIG 1-98 trial. J Clin Oncol 25:5715–5722
Borgquist S, Giobbie-Hurder A, Ahern TP, Garber JE, Colleoni M, Lang I, Debled M, Ejlertsen B, von Moos R, Smith I, Coates AS, Goldhirsch A, Rabaglio M, Price KN, Gelber RD, Regan MM, Thurlimann B (2017) Cholesterol, Cholesterol-Lowering Medication Use, and Breast Cancer Outcome in the BIG 1-98 Study. J Clin Oncol 35:1179–1188
Sahebkar A, Serban M-C, Penson P, Gurban C, Ursoniu S, Toth PP, Jones SR, Lippi G, Kotani K, Kostner K, Rizzo M, Rysz J, Ganach M (2017) Lipid and Blood Pressure Meta-analysis Collaboration (LBPMC) Group. Drugs 77(11):1187–1197
Cheung YM, Ramchand SK, Yeo B, Grossmann M (2019) Cardiometabolic Effects of Endocrine Treatment of Estrogen Receptor-Positive Early Breast Cancer. J Endocr Soc 3(7):1283–1301
Wasan KM, Goss PE, Pritchard PH, Shepherd L, Palmer MJ, Liu S, Tu D, Ingle JN, Heath M, Deangelis D, Perez EA (2005) The influence of letrozole on serum lipid concentrations in postmenopausal women with primary breast cancer who have completed 5 years of adjuvant tamoxifen (NCIC CTG MA. 17L). Ann Oncol 16(5):707–715
Baum M, Budzar AU, Cuzick J, Forbes J, Houghton JH, Klijn JG, Sahmoud T, ATAC Trialists’ Group (2002) Anastrozole alone or in combination with tamoxifen versus tamoxifen alone for adjuvant treatment of postmenopausal women with early breast cancer: first results of the ATAC (Arimidex, Tamoxifen, Alone or in Combination) randomised trial. Lancet 359:2131–2139
Howell A, Cuzick J, Baum M, Buzdar A, Dowsett M, Forbes JF, Hoctin-Boes G, Houghton J, Locker GY, Tobias JS, ATAC Trialists’ Group (2005) Results of the ATAC (Arimidex, Tamoxifen, Alone or in Combination) trial after completion of 5 years’ adjuvant treatment for breast cancer. Lancet 365:60–62
Boccardo F, Rubagotti A, Puntoni M, Guglielmini P, Amoroso D, Fini A, Paladini G, Mesiti M, Romeo D, Rinaldini M, Scali S, Porpiglia M, Benedetto C, Restuccia N, Buzzi F, Franchi R, Massidda B, Distante V, Amadori D, Sismondi P (2005) Switching to anastrozole versus continued tamoxifen treatment of early breast cancer: Preliminary results of the Italian Tamoxifen Anastrozole Trial. J Clin Oncol 23:5138–5147
Jakesz R, Jonat W, Gnant M, Mittlboeck M, Greil R, Tausch C, Hilfrich J, Kwasny W, Menzel C, Samonigg H, Seifert M, Gademann G, Kaufmann M, Wolfgang J, Austrian Breast and Colorectal Cancer Study Group (ABCSG) and the GABG (2005) Switching of postmenopausal women with endocrine-responsive early breast cancer to anastrozole after 2 years’ adjuvant tamoxifen: combined results of ABCSG trial 8 and ARNO 95 trial. Lancet 366:455–462
Arimidex Tamoxifen, Alone or in Combination Trialists’ Group, Buzdar A, Howell A, Cuzick J, Wale C, Distler W, Hoctin-Boes G, Houghton, J, Locker GY, Nabholtz, JM, (2006) Comprehensive side-effect profile of anastrozole and tamoxifen as adjuvant treatment for early-stage breast cancer: long-term safety analysis of the ATAC trial. Lancet Oncol 7:633–643
Khosrow-Khavar F, Filion KB, Bouganim N, Suissa S, Azoulay L (2020) Aromatase inhibitors and the risk of cardiovascular outcomes in women with breast cancer: A population-based cohort study. Circulation 141(7):549–559
Matthews A, Stanway S, Farmer RE, Strongman H, Thomas S, Lyon AR, Smeeth L, Bhaskaran K (2018) Long term adjuvant endocrine therapy and risk of cardiovascular disease in female breast cancer survivors: Systematic review. BMJ 363:k3845
Colleoni M, Giobbie-Hurder A, Regan MM, Thurlimann B, Mouridsen H, Mauriac L, Forbes JF, Paridaens R, Láng I, Smith I, Chirgwin J, Pienkowski T, Wardley A, Price KN, Gelber RD, Coates AS, Goldhirsch A (2011) Analyses adjusting for selective crossover show improved overall survival with adjuvant letrozole compared with tamoxifen in the BIG 1-98 study. J Clin Oncol 29(9):1117–1124
Viale G, Regan MM, Dell’Orto P, Mastropasqua MG, Maiorano E, Rasmussen BB, MacGrogan G, Forbes JF, Paridaens RJ, Colleoni M, Láng I, Thurlimann B, Mouridsen H, Mauriac L, Gelber RD, Price KN, Goldhirsch A, Gusterson BA, Coates AS, BIG 1-98 Collaborative and International Breast Cancer Study Groups (2011) Which patients benefit most from adjuvant aromatase inhibitors? Results using a composite measure of prognostic risk in the BIG 1-98 randomized trial. Ann Oncol 22(10):2201–2207
Acknowledgements
The authors are indebted to the women, physicians, nurses, and data managers who participated in the Breast International Group (BIG) 1-98 clinical trial; to the BIG Collaborative Group, BIG Headquarters, and BIG 1-98 Steering Committee; to the International Breast Cancer Study Group (IBCSG) for the design of the trial, coordination, data management, medical review, and statistical support; and to SAKK and the Foundation for Clinical Cancer Research of Eastern Switzerland OSKK for their support of BIG 1-98.
Funding
The BIG 1-98 trial was financed by Novartis and coordinated by the International Breast Cancer IBCSG. Other support for the IBCSG was provided by The Swedish Cancer Society, The Swedish Research Council, The Cancer Council Australia, Australia New Zealand Breast Cancer Trials Group, Frontier Science and Technology Research Foundation, Swiss Group for Clinical Cancer Research (SAKK), Cancer Research Switzerland, Oncosuisse, and the Foundation for Clinical Cancer Research of Eastern Switzerland (OSKK).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Manuela Rabaglio declares that she has no conflict of interest. Zhuoxin Sun declares that she has no conflict of interest. Rudolf Maibach declares that he has no conflict of interest. Anita Giobbie-Hurder reports that her institution receives support for her salary from nine National Institutes of Health (NIH) grants, including 5R01 CA193970-05, 1U24 CA224316-01, 1U24 CA224331-01, 5R01 CA229851-03, 5R01 CA190838-04, 5R01 CA221874-03, 1R01 CA244975-01, 1R01 CA252312-01, and 1R01 CA251599-01 in addition two other grants from the Susan Smith Center for Women’s Cancer and the Melanoma Research Alliance. Bent Ejlertsen reports that his institution receives research funding from AstraZeneca, Nanostring Technologies, Novartis, Pfizer, Roche, Samsung, and Venture Oncology. Vernon J. Harvey declares that he has no conflict of interest. Patrick Neven declares that he has no conflict of interest. István Láng declares that he has no conflict of interest. Hervé Bonnefoi declares that he has no conflict of interest. Andrew Wardley declares that he has no conflict of interest. Barbara Ruepp declares that she has no conflict of interest. Monica Castiglione declares that she has no conflict of interest. Alan S. Coates declares that he has no conflict of interest. Richard D. Gelber reports that his institution receives partial support for his salary from AstraZeneca, Celgene, Ferring, Ipsen, Merck, Novartis, Pfizer, and Roche. Marco Colleoni reports that he receives an honorarium from Novartis. Beat Thürlimann receives consultation fees from Amgen, AstraZeneca, Eli Lilly, Roche, and Pfizer, owns stocks in Novartis and Roche, holds leadership roles at the Swiss Cancer Research Foundation, Rising Tide for Clinical Cancer Research Foundation, Swiss Society of Senology Board of Directors, IBCSG Scientific Committee, IBCSG Biology Project Working Group, Cancer League of Eastern Switzerland Board of Directors, Swiss Foundation for Clinical Cancer Research Executive Committee, and is the Former SAKK President. Meredith M. Regan receives research funding (to the institution) from Novartis, Pfizer, Ipsen, TerSera, Merck, Ferring, Pierre Fabre, Roche, AstraZeneca, Bayer, and Bristol-Myers Squibb and receives consulting/advisory fees from Ipsen/Debiopharm (institution IBCSG), Bristol-Myers Squibb, and Tolmar Pharmaceuticals.
Ethical approval
Ethics committees and relevant health authorities approved the protocol.
Informed consent
Written informed consent was obtained from all individual participants included in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rabaglio, M., Sun, Z., Maibach, R. et al. Cumulative incidence of cardiovascular events under tamoxifen and letrozole alone and in sequence: a report from the BIG 1-98 trial. Breast Cancer Res Treat 185, 697–707 (2021). https://doi.org/10.1007/s10549-020-05981-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-020-05981-z