Abstract
Purpose
The identification of biomarkers of hormonal therapy (HT) failure would allow tailored monitoring in metastatic breast cancer (mBC) patients. PIK3CA gene mutation is one of the most frequent events in mBC and is associated with HT resistance. We evaluated the early prognostic value of cell-free DNA (cfDNA) PIK3CA detection in first-line HT-treated mBC patients.
Methods
Between June 2012 and January 2014, 39 patients were prospectively included in a dedicated clinical trial (NCT01612871). Blood sampling was performed before (M0) and 4 weeks (M1), 3 months (M3) and 6 months (M6) after HT initiation, and at tumor progression. Patients were followed until progression or until the end of the study (2 years). Mutation detection was performed using droplet-based digital PCR (ddPCR). Progression-free survival (PFS) was used as primary endpoint.
Results
Median age at inclusion was 63 years (range 40–86). Most patients (34/39) received an aromatase inhibitor and presented a non-measurable disease (71.8%). PIK3CA mutations were reported in 10 (27.8%) and 5 (14.3%) cases at M0 and M1, respectively. The persistence of a detectable circulating mutation at M1 was highly correlated with a worse progression-free survival (PFS), rate at 1 year: 40% versus 76.7%; p = 0.0053).
Conclusions
Four-week persistence of cfDNA PIK3CA mutation appears highly correlated with PFS.
Trial registration
NCT01612871, registered on June 6th, 2012; https://clinicaltrials.gov/ct2/show/NCT01612871.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Hormonal therapies (HT) have improved the patients’ outcomes in estrogen-receptor-positive (ER+) metastatic breast cancer (mBC). However, the effectiveness is limited by de novo or acquired resistance, occurring in nearly all mBC patients. Multiple mechanisms responsible for HT resistance have been proposed, including activation of various intracellular pathways mainly the phosphatidylinositol 3-kinase (PI3K)/Akt/mammalian target of rapamycin (mTOR), and cyclin-dependent kinase (CDK) 4/6/retinoblastoma protein (RB) pathways. The occurrence of mutations in the PI3K catalytic subunit alpha (PIK3CA), which generally occur in one of the two hotpot regions (Exon 9: E545K or E542K, and Exon 20: H1047R), is one of the most frequent events in ER + BC and has been involved in HT resistance [1,2,3,4,5,6,7,8]. However, the clinical impact of the PIK3CA status analyzed in tissue samples remains debated and most patients affected by estrogen-receptor-positive/HER2-negative (ER+/HER2−) tumors presented only bone metastases, a metastatic site associated with technical issues regarding pathological and biological evaluations [9, 10]. However, the identification of early prognostic biomarkers under HT could help tailoring monitoring and an early change in therapy.
The search for circulating biomarkers, easily accessible by blood sampling (as opposed to the biopsy of a metastasis) could be a preferred route especially for patients who cannot be biopsied. Circulating cell-free tumor DNA (cfDNA) is a specific marker of tumor disease. Many studies, particularly in lung and colorectal cancers but also in breast cancer (BC), have shown that predictive factors of response to treatments such as KRAS, EGFR, or PI3KCA mutations could be detected in cfDNA [11,12,13]. Circulating biomarkers such as cfDNA may also allow a global evaluation of all the metastatic sites, at the time of treatment initiation and during treatment, without the need for invasive biopsies and the difficulties associated with the specific requirements of bone metastases [7, 14, 15]. The detection of specific mutations on cfDNA could thus be proposed as a dynamic surrogate endpoint for clinical efficacy of a given treatment, allowing a short-term prediction of the long-term treatment outcome.
We prospectively evaluated in a bicentric clinical trial, the early prognostic value of cfDNA PIK3CA detection and dynamics in a prospective population of locally advanced or mBC patients receiving first-line HT to explore the prognostic value of baseline and early changes of cfDNA PIK3CA mutations.
Methods
Study design and patients
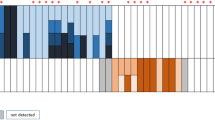
Between June 2012 and January 2014, 39 patients with ER+/HER2− metastatic or locally advanced BC treated with first-line HT in 2 comprehensive cancer centers were prospectively included in a dedicated clinical trial (NCT01612871) aiming at the identification of circulating biomarkers associated with prognosis under HT. Serial blood sampling was performed before HT initiation (M0), at 4 weeks (M1), 3 months (M3), and 6 months (M6) after HT initiation, and at tumor progression (Fig. 1). Patients were followed until progression or until the end of the study (2 years follow-up). Considering the natural history of ER+/HER2− mBC and the frequency of non-measurable disease in this subgroup, 1-year progression-free survival was used as primary endpoint. As part of the study evaluated the prognostic impact of biological markers, this manuscript adheres to the REMARK guidelines [16, 17].
Plasma isolation and cfDNAPIK3CA determination
Plasma samples were obtained from blood collected in EDTA K2 tubes before 3 h after blood draw by centrifugation at 1500×g for 15 min and were stored at − 80 °C until use. Plasma samples were processed and stored in our respective Biological Resources Centers (Biobank number BB-0033-00059), then centralized for subsequent analysis. Once thawed at room temperature, stored plasma were centrifuged at 16,000×g for 15 min at + 4 °C and cfDNA was isolated from the supernatant using the QiaAmp circulating nucleic acid isolation kit (Qiagen, Courtaboeuf, France) according to the manufacturer’s instructions. After cfDNA extraction, quality of the cfDNA was evaluated with an Agilent High Sensitivity DNA kit and the Bioanalyzer 2100 instrument (Agilent Technologies, Les Ulis, France). Subsequently, the circulating cfDNA concentration was quantified by fluorometry with the Qubit 2.0 Fluorometer (Life Technologies, Saint-Aubin, France). Mutation detection was performed using droplet digital PCR on a QX100™ system (Bio-Rad, Marnesla Coquette, France) according to a previously published method [18]. Briefly, a 20 µL reaction mixture containing 10 µl of 2 × ddPCR Supermix for probes with no dUTP (Bio-Rad), 5 µL of extracted cfDNA, 900 nM of each specific forward and reverse primer, and 250 nM of each FAM-labeled mutant probe and HEX-labeled wild-type probe were carried out. After droplet formation using 70 µL of generation oil (Bio-Rad) and the entire volume of the PCR mix, 40 µL of droplets was transferred for thermal cycling as follows: 95 °C for 10 min, 40 cycles of 94 °C for 30 s then 60 °C for 60 s followed by 98 °C for 10 min and cooling at 4 °C. The temperature ramp increment was 2 °C/s for all steps. The assays targeted wild-type PIK3CA and mutations p.E542K, p.E545K in exon 9, and p.H1047R in exon 20. Primers and TaqMan hydrolysis probes were custom designed and provided by Bio-Rad (sequences available upon request). Genomic DNA from the T84 cell line (c.1624G > A, p. E542K), MCF-7 cell line (c.1633G > A, p.E545K), and LS174T cell line (c.3140 A > G, P.H1047R) were used as positive PIK3CA mutation controls. DNA from the LNCaPcell line (wild-type PIK3CA) was the negative PIK3CA mutation control. For each series of ddPCR assays, a non-template control was carried out.
Data analysis was performed using the QuantaSoft v1.7.4 software. Thresholds for the detection of positive and negative droplets were set manually based on results from non-template control wells and negative PIK3CA mutation control (LNCaP cell line). All data were evaluated above the threshold. All experiments were performed in duplicate. First, concentration of amplified fragments, FAM-labeled or HEX-labeled were calculated (copies/reaction) based on the Poisson distribution and the quantification of mutated and wild-type alleles was estimated with the following equation: λ = − ln (1 − P), where λ is the average number of target DNA molecules per replicate reaction and P is the fraction of positive end point reactions. Finally, cfDNA target concentration was calculated as copies/reaction and cfDNA concentrations were reported as number of copies/mL of plasma. The PIK3CA mutant allele fraction (MAF % = number of mutated copies/µl/total number of copies/µl) for each sample was determined by using the QuantaSoft software V1.7.4 (Bio-Rad). To assess the limit of detection of the three assays, isogenic reference DNAs with known mutant allele frequency were used (Horizon Diagnostics, Cambridge, United Kingdom). Based on confidence intervals for Poisson parameters, a sample was considered positive for a targeted mutation if the average mutant copies detected was four copies and above per reaction.
Statistical analyses
Data were presented by frequencies and percentages for categorical variables and by medians and ranges for continuous variables. The association between clinicopathological factors and PIK3CA mutations at baseline was performed by the Chi-square test or the Fisher’s exact test. All survival times were calculated from the date of inclusion to the progression or the death. Patients progression-free or alive were censored at the time of their last follow-up. Progression-free survival rates were analyzed using the Kaplan–Meier method and presented with 95% confidence intervals (95% CI). For univariate analyses, the log-rank test was used for categorical variables and the Cox proportional hazards model for continuous variables. Multivariate analyses were performed using the Cox proportional hazards model including significant covariates indicated by p < 0.10 in univariate analyses and hazard ratios with 95% confidence intervals were presented for each covariate in the models.
Results
Patients’ characteristics
The main clinical characteristics of the study population are summarized in Table 1. The patients’ median age at inclusion was 63 years (range 40–86). Most patients (34/39, 87.2%) received an aromatase inhibitor as first-line HT (letrozole, n = 32, tamoxifen, n = 5, anastrozole, n = 1 and exemestane, n = 1 patient). Patients mainly presented with a non-measurable disease (n = 28, 71.8%) and 27 had bone metastases precluding a relevant evaluation of prognostic factors for response.
Response and survival
The overall objective response rate was 24.3% (2 complete responses, 5.4%; 7 partial responses, 18.9%), while 70.3% of the patients achieved stable disease. The one- and 2-year progression-free survival (PFS) rates were 67.6% [95% CI (50.0; 80.1)] and 32.4% [95% CI (18.2; 47.5)], respectively, with 25 progression events (64.1%) by the end of the study.
cfDNA PIK3CA determination and clinicopathological correlates
Plasma sample results were available for 36, 35, 33, and 30 patients at M0, M1, M3, and M6, respectively. PIK3CA mutations were present in 10 (27.8%), 5 (14.3%), 3 (9.1%), and 4 (13.3%) cases at M0, M1, M3, and M6, respectively. M0 cfDNAPIK3CA mutations were detected in the helical domain in 6 (60%) samples (c.1624G > A, p. E542K, (n = 4), c.1633G > A, p.E545K, (n = 2)) and in 4 (40%) samples in the catalytic kinase domain (c.3140 A > G, P.H1047R). The MAF ranged from 1.35% to 76.7%. M0 cfDNA PIK3CA mutation detection was significantly associated with the presence of bone metastases (10/10 patients with detectable mutated PIK3CA cfDNA vs. 14/25 patients without detectable mutated PIK3C AcfDNA, p = 0.0146; Table 2). To evaluate the correlation between cfDNA parameters and tumor burden, we analyzed the correlations between all the evaluated cfDNA parameters and the number of metastatic sites as an indirect reflect of tumor burden (0–1 sites, N = 24 vs. 2+ sites, N = 15). No statistically significant correlation was seen with any of the evaluated parameters (data not shown).
Univariate and multivariate analyses of prognostic factors
In univariate analyses (Supplementary Tables 1 and 2), the only clinical variable close to the significance threshold was the presence of lymph node metastases (p = 0.0615). Baseline cfDNA concentration and baseline PIK3CA MAF (%) were found to be significantly associated with PFS in univariate analysis, while a trend was seen for 1 month PIK3CA MAF (%, p = 0.069) and cfDNA concentration evolution (1 month—baseline).
While the presence of a cfDNA PIK3CA mutation in the M0 sample was not significantly associated with PFS (rate at 12 months: 70% [95% CI (32.9; 89.2)] versus 70.8% [95% CI (48.4; 84.9)]), the persistence of a detectable circulating mutation at M1 was highly correlated with a poorer PFS (rate at 12 months: 40% [95% CI (5.2; 75.3)] versus 76.7% [95% CI (57.2; 88.1)], p = 0.0053) (Fig. 2, Supplementary Table 1).
In a second step, considering the number of recorded PFS events, we performed four multivariate analyses using the lymph node metastases variable and the selected cfDNA variables (Supplementary Table 3). Lymph node metastases remain an independent prognostic factor in three models among the four models, and the model taking into account lymph node metastases and persistence of mutated PIK3CA cfDNA at 1 month was associated with higher hazard ratios.
No correlation was reported between cfDNA PIK3CA mutation detection, whatever the time point, and the tumor response.
Discussion
In metastatic breast cancer (mBC), the evolutionary process under therapeutic pressure and genomic instability leads to the emergence of clonal populations harboring mutations associated with resistance to anticancer therapies [8]. At the same time, identification of the different clonal populations by multiple biopsies of the different metastatic sites is difficult, especially in ER+/HER2− mBC. Indeed, they frequently develop bone metastases, a metastatic site associated with technical issues for molecular analyses. Liquid biopsy appears, in this context, a sensitive and specific, minimally invasive method to identify and monitor mutations of interest [15, 19, 20].
The clinical impact of the tissue PIK3CA status remains unknown in different breast cancer histologic types, molecular subtypes as well as under various therapeutic strategies, such as in first-line HT [21]. For example, in an ancillary analysis of the MONALEESA-2 phase III study evaluating the first-line association of CDK4/6 inhibitor ribociclib and letrozole, ribociclib treatment benefit was maintained irrespective of the PIK3CA mutation status [22].
At the same time, identification of circulating cfDNA PIK3CA mutations has recently been reported to be associated with clinical behavior and response to anti-PI3K targeted therapies. In the randomized phase III BELLE-2 trial evaluating the impact of buparlisib, a PI3K inhibitor, associated with fulvestrant, tissue-based evaluation of the PI3K pathway activation (based on PI3KCA activating mutations or loss of PTEN expression) was not predictive of buparlisib efficacy [14]. However, in the same population, a significant difference in PFS was reported in the buparlisib group versus the placebo group in patients with detectable cfDNA PIK3CA mutations, while there was no difference between the groups of patients with no detectable cfDNA PIK3CA mutations. At the same time, the overlap between tissue and cfDNA PIK3CA mutations detection was partial in this study, as for the 446 patients with known tumor and cfDNA PIK3CA status, overall concordance was only 77%, emphasizing the evolutionary process occurring during metastasis.
Recently, the SOLAR-1 study showed alpelisib, a selective PI3K alpha-specific inhibitor, associated with fulvestrant nearly doubled median PFS (11.0 vs. 5.7 months) in HR+/HER2− advanced breast cancer patients with a PIK3CA mutation compared to fulvestrant alone [23]. Alpelisib is now FDA-approved for women with a PIK3CA mutation in HR+/HER2− advanced breast cancer and the use of liquid biopsy will become widespread for women with advanced BC, thus prompting the interest for identification of reliable, minimally invasive, biomarkers of sensitivity/resistance in this population.
In our dedicated prospective clinical trial, in a first-line HT setting, the 4-week persistence or occurrence of a cfDNA PIK3CA mutation, and not the baseline cfDNA PIK3CA mutation status, appeared highly correlated with PFS. Evolution of specific cfDNA mutations could increase the prognostic value of this biomarker. Our results are in accordance with those recently reported by O’Leary and colleagues [24]. In their ancillary analysis of the pivotal PALOMA-3 trial evaluating the impact of the addition of palbociclib to fulvestrant, 22% of the baseline plasma samples were positive for a PIK3CA mutation in ctDNA. No statistically significant association was seen between the baseline PIK3CA status in ctDNA and PFS in patients treated with palbociclib and fulvestrant. However, assessment of the effect of the dynamic changes in cfDNA showed a decrease of mutated PIK3CA (and not ESR1) ctDNA level after 15 days of palbociclib and fulvestrant treatment, strongly correlated with PFS.
Early identification of a population of mBC harboring persistent cfDNA PIK3CA mutations could allow the future evaluation, in a selected population with an unfavorable prognosis, of anti-PI3K targeted therapies combined with HT and/or CDK4/6 inhibitors, considering the reported synergistic effect of these two classes of drugs [25, 26]. Indeed, focus on relevant biomarker identification on early samples could allow, in the better scenario case, an early adaptation of the treatment, as the aim of a prognostic and/or predictive biomarker is to allow a better identification of a given population early in the therapeutic process. Later time samplings, while of scientific interest, appear less useful considering this tailoring concept.
Although the analysis of early changes in mutation content of cfDNA seems an attractive biomarker [27], there is no consensus on the best technical approach. Digital PCR is an accurate and rapid methodology, easy to implement in the clinical setting and that compares favorably in terms of sensitivity and cost to the next generation sequencing. In addition, compared to standard real-time PCR, digital PCR can achieve a higher sensitivity and an absolute quantification of targeted mutations.
Our study has some limitations, among which the relatively small number of patients, precluding a global statistically valid multivariate analysis as, considering the number of events, it would have violated the 10 events per 1 variable rule [28], inducing greater risks of bias. To circumvent this limitation, we performed four separate multivariate analyses. In these multivariate analyses, of the considered cfDNA variables, persistence of mutated PIK3CA cfDNA at 1 month was associated with the better hazard ratios and appeared the more consistent considering the clinical impact and the published literature on cfDNA value under treatment. Also, only hotspot mutations in the PIK3CA gene were assayed. However, these hotspot mutations are expected to represent 80% of the total PIK3CA gene mutations in HR+/HER2− mBC [29]. These results need to be confirmed in a separated data set including a greater number of patients and events.
Conclusion
Our study provides a proof of concept and attests of the feasibility of cfDNA analysis for patients with ER+ locally advanced or metastatic BC. Early identification of this population with cfDNA PIK3CA mutations allows the identification of a population affected by an unfavorable prognosis. Dedicated and ancillary studies of anti-PI3K targeted therapies are warranted in order to determine the optimal time point to evaluate this new biomarker.
Data availability
The data that support the findings of this study are available from the Department of Biostatistics, Institut Claudius Regaud, IUCT-O Toulouse, France, upon reasonable request.
Abbreviations
- BC:
-
Breast cancer
- cfDNA:
-
Cell-free DNA
- CDK:
-
Cyclin-dependent kinase
- ER+:
-
Estrogen-receptor-positive
- HT:
-
Hormonal therapy
- mBC:
-
Metastatic breast cancer
- mTOR:
-
Mammalian target of rapamycin
- PI3K:
-
Phosphatidylinositol 3-kinase
- PI3KCA:
-
PI3K catalytic subunit alpha
- PFS:
-
Progression-free survival
- RB:
-
Retinoblastoma
- 95% CI:
-
95% confidence interval
References
Provenzano A, Kurian S, Abraham J (2013) Overcoming endocrine resistance in breast cancer: role of the PI3 K and the mTOR pathways. Expert Rev Anticancer Ther 13(2):143–147. https://doi.org/10.1586/era.12.173
Fu X, Osborne CK, Schiff R (2013) Biology and therapeutic potential of PI3 K signaling in ER+/HER2-negative breast cancer. Breast 22(Suppl 2):S12–18. https://doi.org/10.1016/j.breast.2013.08.001
Lopez-Knowles E, Segal CV, Gao Q, Garcia-Murillas I, Turner NC, Smith I, Martin LA, Dowsett M (2014) Relationship of PIK3CA mutation and pathway activity with antiproliferative response to aromatase inhibition. Breast Cancer Res 16(3):R68. https://doi.org/10.1186/bcr3683
Ramirez-Ardila DE, Helmijr JC, Look MP, Lurkin I, Ruigrok-Ritstier K, van Laere S, Dirix L, Sweep FC, Span PN, Linn SC, Foekens JA, Sleijfer S, Berns EM, Jansen MP (2013) Hotspot mutations in PIK3CA associate with first-line treatment outcome for aromatase inhibitors but not for tamoxifen. Breast Cancer Res Treat 139(1):39–49. https://doi.org/10.1007/s10549-013-2529-7
Lai K, Killingsworth MC, Lee CS (2015) Gene of the month: PIK3CA. J Clin Pathol 68(4):253–257. https://doi.org/10.1136/jclinpath-2015-202885
Araki K, Miyoshi Y (2018) Mechanism of resistance to endocrine therapy in breast cancer: the important role of PI3 K/Akt/mTOR in estrogen receptor-positive, HER2-negative breast cancer. Breast Cancer 25(4):392–401. https://doi.org/10.1007/s12282-017-0812-x
Higgins MJ, Jelovac D, Barnathan E, Blair B, Slater S, Powers P, Zorzi J, Jeter SC, Oliver GR, Fetting J, Emens L, Riley C, Stearns V, Diehl F, Angenendt P, Huang P, Cope L, Argani P, Murphy KM, Bachman KE, Greshock J, Wolff AC, Park BH (2012) Detection of tumor PIK3CA status in metastatic breast cancer using peripheral blood. Clin Cancer Res 18(12):3462–3469. https://doi.org/10.1158/1078-0432.CCR-11-2696
Bertucci F, Ng CKY, Patsouris A, Droin N, Piscuoglio S, Carbuccia N, Soria JC, Dien AT, Adnani Y, Kamal M, Garnier S, Meurice G, Jimenez M, Dogan S, Verret B, Chaffanet M, Bachelot T, Campone M, Lefeuvre C, Bonnefoi H, Dalenc F, Jacquet A, De Filippo MR, Babbar N, Birnbaum D, Filleron T, Le Tourneau C, Andre F (2019) Genomic characterization of metastatic breast cancers. Nature 569(7757):560–564. https://doi.org/10.1038/s41586-019-1056-z
Bussolati G, Leonardo E (2008) Technical pitfalls potentially affecting diagnoses in immunohistochemistry. J Clin Pathol 61(11):1184–1192. https://doi.org/10.1136/jcp.2007.047720
Singh VM, Salunga RC, Huang VJ, Tran Y, Erlander M, Plumlee P, Peterson MR (2013) Analysis of the effect of various decalcification agents on the quantity and quality of nucleic acid (DNA and RNA) recovered from bone biopsies. Ann Diagn Pathol 17(4):322–326. https://doi.org/10.1016/j.anndiagpath.2013.02.001
Goto K, Ichinose Y, Ohe Y, Yamamoto N, Negoro S, Nishio K, Itoh Y, Jiang H, Duffield E, McCormack R, Saijo N, Mok T, Fukuoka M (2012) Epidermal growth factor receptor mutation status in circulating free DNA in serum: from IPASS, a phase III study of gefitinib or carboplatin/paclitaxel in non-small cell lung cancer. J Thorac Oncol 7(1):115–121. https://doi.org/10.1097/JTO.0b013e3182307f98
Kim TW, Peeters M, Thomas AL, Gibbs P, Hool K, Zhang J, Ang A, Bach BA, Price T (2018) Impact of emergent circulating tumor DNA RAS mutation in panitumumab-treated chemoresistant metastatic colorectal cancer. Clin Cancer Res. https://doi.org/10.1158/1078-0432.CCR-17-3377
Board RE, Wardley AM, Dixon JM, Armstrong AC, Howell S, Renshaw L, Donald E, Greystoke A, Ranson M, Hughes A, Dive C (2010) Detection of PIK3CA mutations in circulating free DNA in patients with breast cancer. Breast Cancer Res Treat 120(2):461–467. https://doi.org/10.1007/s10549-010-0747-9
Baselga J, Im SA, Iwata H, Cortes J, De Laurentiis M, Jiang Z, Arteaga CL, Jonat W, Clemons M, Ito Y, Awada A, Chia S, Jagiello-Gruszfeld A, Pistilli B, Tseng LM, Hurvitz S, Masuda N, Takahashi M, Vuylsteke P, Hachemi S, Dharan B, Di Tomaso E, Urban P, Massacesi C, Campone M (2017) Buparlisib plus fulvestrant versus placebo plus fulvestrant in postmenopausal, hormone receptor-positive, HER2-negative, advanced breast cancer (BELLE-2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol 18(7):904–916. https://doi.org/10.1016/S1470-2045(17)30376-5
Alix-Panabieres C, Pantel K (2016) Clinical applications of circulating tumor cells and circulating tumor DNA as liquid biopsy. Cancer Discov 6(5):479–491. https://doi.org/10.1158/2159-8290.CD-15-1483
Hayes DF, Ethier S, Lippman ME (2006) New guidelines for reporting of tumor marker studies in breast cancer research and treatment: REMARK. Breast Cancer Res Treat 100(2):237–238. https://doi.org/10.1007/s10549-006-9253-5
McShane LM, Altman DG, Sauerbrei W, Taube SE, Gion M, Clark GM, Statistics Subcommittee of the NCIEWGoCD (2005) REporting recommendations for tumour MARKer prognostic studies (REMARK). Eur J Cancer 41(12):1690–1696. https://doi.org/10.1016/j.ejca.2005.03.032
Lamy PJ, Castan F, Lozano N, Montelion C, Audran P, Bibeau F, Roques S, Montels F, Laberenne AC (2015) Next-generation genotyping by digital PCR to detect and quantify the BRAF V600E Mutation in melanoma biopsies. J Mol Diagn 17(4):366–373. https://doi.org/10.1016/j.jmoldx.2015.02.004
Hu ZY, Xie N, Tian C, Yang X, Liu L, Li J, Xiao H, Wu H, Lu J, Gao J, Hu X, Cao M, Shui Z, Xiao M, Tang Y, He Q, Chang L, Xia X, Yi X, Liao Q, Ouyang Q (2018) Identifying circulating tumor DNA mutation profiles in metastatic breast cancer patients with multiline resistance. EBioMedicine 32:111–118. https://doi.org/10.1016/j.ebiom.2018.05.015
Rothe F, Laes JF, Lambrechts D, Smeets D, Vincent D, Maetens M, Fumagalli D, Michiels S, Drisis S, Moerman C, Detiffe JP, Larsimont D, Awada A, Piccart M, Sotiriou C, Ignatiadis M (2014) Plasma circulating tumor DNA as an alternative to metastatic biopsies for mutational analysis in breast cancer. Ann Oncol 25(10):1959–1965. https://doi.org/10.1093/annonc/mdu288
Liu YR, Jiang YZ, Zuo WJ, Yu KD, Shao ZM (2014) PIK3CA mutations define favorable prognostic biomarkers in operable breast cancer: a systematic review and meta-analysis. OncoTargets Ther 7:543–552. https://doi.org/10.2147/OTT.S60115
Hortobagyi GN, Stemmer SM, Burris HA, Yap YS, Sonke GS, Paluch-Shimon S, Campone M, Petrakova K, Blackwell KL, Winer EP, Janni W, Verma S, Conte P, Arteaga CL, Cameron DA, Mondal S, Su F, Miller M, Elmeliegy M, Germa C, O’Shaughnessy J (2018) Updated results from MONALEESA-2, a phase III trial of first-line ribociclib plus letrozole versus placebo plus letrozole in hormone receptor-positive, HER2-negative advanced breast cancer. Ann Oncol 29(7):1541–1547. https://doi.org/10.1093/annonc/mdy155
Andre F, Ciruelos E, Rubovszky G, Campone M, Loibl S, Rugo HS, Iwata H, Conte P, Mayer IA, Kaufman B, Yamashita T, Lu YS, Inoue K, Takahashi M, Papai Z, Longin AS, Mills D, Wilke C, Hirawat S, Juric D, Group S-S, the S-SG (2019) Alpelisib for PIK3CA-mutated, hormone receptor-positive advanced breast cancer. N Engl J Med 380(20):1929–1940. https://doi.org/10.1056/NEJMoa1813904
O’Leary B, Hrebien S, Morden JP, Beaney M, Fribbens C, Huang X, Liu Y, Bartlett CH, Koehler M, Cristofanilli M, Garcia-Murillas I, Bliss JM, Turner NC (2018) Early circulating tumor DNA dynamics and clonal selection with palbociclib and fulvestrant for breast cancer. Nat Commun 9(1):896. https://doi.org/10.1038/s41467-018-03215-x
Vora SR, Juric D, Kim N, Mino-Kenudson M, Huynh T, Costa C, Lockerman EL, Pollack SF, Liu M, Li X, Lehar J, Wiesmann M, Wartmann M, Chen Y, Cao ZA, Pinzon-Ortiz M, Kim S, Schlegel R, Huang A, Engelman JA (2014) CDK 4/6 inhibitors sensitize PIK3CA mutant breast cancer to PI3 K inhibitors. Cancer Cell 26(1):136–149. https://doi.org/10.1016/j.ccr.2014.05.020
Herrera-Abreu MT, Palafox M, Asghar U, Rivas MA, Cutts RJ, Garcia-Murillas I, Pearson A, Guzman M, Rodriguez O, Grueso J, Bellet M, Cortes J, Elliott R, Pancholi S, Baselga J, Dowsett M, Martin LA, Turner NC, Serra V (2016) Early adaptation and acquired resistance to CDK4/6 inhibition in estrogen receptor-positive breast cancer. Cancer Res 76(8):2301–2313. https://doi.org/10.1158/0008-5472.CAN-15-0728
Ma F, Zhu W, Guan Y, Yang L, Xia X, Chen S, Li Q, Guan X, Yi Z, Qian H, Yi X, Xu B (2016) ctDNA dynamics: a novel indicator to track resistance in metastatic breast cancer treated with anti-HER2 therapy. Oncotarget 7(40):66020–66031. https://doi.org/10.18632/oncotarget.11791
Peduzzi P, Concato J, Feinstein AR, Holford TR (1995) Importance of events per independent variable in proportional hazards regression analysis. II. Accuracy and precision of regression estimates. J Clin Epidemiol 48(12):1503–1510
Dirican E, Akkiprik M, Ozer A (2016) Mutation distributions and clinical correlations of PIK3CA gene mutations in breast cancer. Tumour Biol 37(6):7033–7045. https://doi.org/10.1007/s13277-016-4924-2
Acknowledgements
The authors want to thank Dr. Hélène de Forges for her substantive writing and editing assistance.
Funding
This ancillary study was supported by the “Fond pour la Recherche Val d’Aurelle” grant. This research was supported by the SIRIC Montpellier Cancer Grant INCa_Inserm_DGOS_12553.
Author information
Authors and Affiliations
Contributions
Study concept/design/funding: WJ, P-JL, EL-C, FD, and AD. Reagents/materials/analysis tools contribution: NG, P-JL, NL, and EL-C. Patients’ inclusion and follow-up: WJ, FD, AD, J-LL, SP, LG, GR, and HR. Acquisition of data: NG, WJ, P-JL, and EL-C. Statistical analysis: LC and TF. Analysis and interpretation of data: WJ, P-JL, and EL-C. Drafting of the manuscript: NG, WJ, P-JL, EL-C, FD, LC, and TF. All the authors participated to the critical revision and validation of the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
This study was approved by the CPP (Ethics Committee) Sud-Ouest et Outre-Mer III and registered under the reference No. 2012/25. This study was performed in accordance with the Declaration of Helsinki.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Jacot, W., Dalenc, F., Lopez-Crapez, E. et al. PIK3CA mutations early persistence in cell-free tumor DNA as a negative prognostic factor in metastatic breast cancer patients treated with hormonal therapy. Breast Cancer Res Treat 177, 659–667 (2019). https://doi.org/10.1007/s10549-019-05349-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-019-05349-y