Abstract
Purpose
There is uncertainty about outcomes differences between partial breast irradiation (PBI) and whole breast irradiation (WBI) for early-stage breast cancer.
Methods
Prospective randomized trials comparing adjuvant PBI to WBI in early-stage invasive breast cancer were identified using PubMed. Odds ratios (OR), 95% confidence intervals and absolute risks were computed for pre-specified efficacy and toxicity outcomes including cosmesis. Subgroup analysis evaluated the effect of PBI modality (external beam radiation treatment [EBRT], intraoperative radiation treatment [IORT] or brachytherapy) on efficacy. Meta-regression analysis explored the influence of median follow-up, patient and tumor characteristics on results.
Results
Nine trials comprising 14514 patients were included. While PBI was associated with increased odds of local recurrence compared to WBI (OR 1.69, P < 0.001), it was associated with reduced odds of death without breast cancer recurrence (OR 0.55, P < 0.001) and with improvement in overall survival (OS) that approached, but did not meet statistical significance (OR 0.84, P = 0.06). Subgroup analysis for PBI modality showed significant differences in the odds of local recurrence, based on method of PBI with EBRT showing the lowest magnitude of inferiority. Nodal involvement was associated with higher local recurrence risk, while larger tumors were associated with lesser improvement in death without breast cancer recurrence and OS. PBI was associated with higher odds of fat necrosis (OR 1.72, P = 0.002). Worse cosmetic outcome with PBI approached statistical significance (OR 1.23, P = 0.06).
Conclusions
Compared to WBI, PBI is associated with higher odds for local recurrence and toxicity, but less death without breast cancer recurrence. The balance between benefit and risk of PBI appears optimal for women with smaller hormone receptor positive tumors, without nodal involvement and treated with EBRT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Whole breast irradiation (WBI) has become a gold standard adjuvant therapy after lumpectomy in women with early-stage breast cancer, substantially reducing the risk of recurrence and improving survival [1]. WBI is associated with a dose-dependent, higher incidence of cardiotoxicity and lung cancer [2, 3], with progressive increase in risk over time after exposure [4]. As most women with early breast cancer are cured of their disease, consideration of long-term toxicity is crucial.
Partial breast irradiation (PBI) is a localized form of radiation, concentrating on the tumor bed, the site for the majority of recurrences [5,6,7]. By delivering radiation to a decreased target volume, PBI lowers exposure of organs at risk, including contralateral breast tissue, heart, lung, skin and ribs, thereby potentially minimizing late adverse effects [8, 9]. Current data on clinical outcomes with PBI are conflicting. While several studies have reported higher risk for local recurrence [10,11,12,13,14,15] and toxicity [16], previous meta-analyses have shown PBI is associated with lower death without breast cancer recurrence [14, 17].
Different modalities can be used to administer PBI, including interstitial and intracavitary brachytherapy, external beam radiation treatment (EBRT) and single fraction intraoperative radiation (IORT). Current treatment guidelines regarding PBI suggest selection criteria based on results from randomized and prospective non-randomized studies, and mainly address brachytherapy and IORT [18, 19]. Recent results from a large randomized phase 3 trial comparing PBI using EBRT to WBI showed non-inferiority in terms of breast cancer outcome and reduced late tissue toxicity with lower than 1% local recurrence at 5 years with PBI, raising the bar for performance of PBI techniques [20].
Here, we report on a meta-analysis evaluating the outcomes of adjuvant radiation with PBI compared to WBI among patients with early-stage breast cancer. As PBI is associated with reduced radiation to organs at risk, we hypothesized that the benefits and risks of PBI may be linked to patient selection and the radiation technique used.
Methods
Literature review and study identification
A literature search utilizing MEDLINE (Host: PubMed) identified randomized clinical trials comparing PBI to WBI for early-stage invasive breast cancer published between January 2007 and January 2018. The terms “partial,” “breast cancer” and “irradiation” and similar terms were cross-searched by using the following search algorithm: (partial OR incomplete) AND (breast neoplasm MeSH OR ((breast OR mammary) AND (carcinoma OR malignant * OR neoplasm OR tumor))). A review of citation lists was performed to improve the sensitivity of the search strategy. All modalities for PBI were included. The search was restricted to the English language reports of prospective clinical trials.
Data extraction
Data were collected independently by two reviewers (Y.K. and H.G.). Discrepancies were resolved by a third reviewer (E.A.). All data were extracted from primary publications and their associated online appendices. Collected data included year of publication, number of patients, median age, proportion of pre-menopausal patients, median duration of follow-up and information about the radiation treatment. We also collected trial-level tumor characteristics including the proportion of patients with small tumor size (defined as maximal diameter of ≤ 1.0 cm or T1a or T1b staging), nodal involvement, high-grade tumors, histology subtype (ductal carcinoma versus other), estrogen receptor (ER) expression and human epidermal growth factor receptor 2 (HER2) over-expression or amplification (as determined by individual studies).
Local recurrence was defined as any recurrence in the ipsilateral breast. Where available, the total number of events at 5 years were collected for the following outcomes: local recurrence, regional recurrence, contralateral breast cancer, disease free survival (DFS), death without breast cancer recurrence and OS. Data on hazard ratio (HR) and 95% confidence intervals (CI) for local recurrence were also collected. We collected data on potential radiation-related morbidities, including secondary malignancies (excluding breast cancer), pulmonary fibrosis and cardiac mortality. Additionally, data on cosmetic outcome and on local toxicities were extracted including arm symptoms, breast pain, fat necrosis, telangiectasia, hyperpigmentation and induration or fibrosis. When outcomes were not reported explicitly, they were estimated either from figures or from survival curves where possible.
Data synthesis and statistical analysis
The primary analysis compared the odds of events between patients who were randomized to PBI and those randomized to WBI. The odds ratio (OR) and associated 95% CI were computed for each outcome and were then pooled in a meta-analysis using RevMan 5.3 (The Cochrane Collaboration, Copenhagen, Denmark). Pooled estimates of OR were computed using Peto one-step OR [21] when the absolute event rates in the experimental and control groups were less than 1% in at least one study; otherwise, the Mantel–Haenszel OR method was used [22]. Statistical heterogeneity was reported using Cochran Q and I2 statistics. Statistically significant heterogeneity was defined as Cochran Q P < 0.10 or I2 > 50%. In analyses where statistically significant heterogeneity was observed, random-effects modelling was utilized. Otherwise, fixed-effect modelling was performed. Subgroup analyses by PBI modality (brachytherapy, IORT and EBRT) were performed to explore the effect of the modality used on outcomes. Differences between the subgroups were assessed using methods described by Deeks et al. [23]. Efficacy outcomes were assessed at the 5-year time point. For studies where such data were not available, outcome at later time points was included, but a sensitivity analysis was performed to explore the effect of these studies on the pooled estimate. Multiple sensitivity analyses were performed including: repeating all analyses using random effects irrespective of statistical heterogeneity (due to the presence of clinical heterogeneity such as differences in radiation techniques), excluding studies that used data that were estimated from figures or survival curves rather than extracted directly, and excluding studies in which there was contamination reported in > 10% of the study population. Finally, for variables reported as a range rather than an absolute number, different estimates within the range were explored (e.g., if median age was not reported explicitly, but the median fell within a 10-year range age estimates using the lower, middle and upper estimates of the range were used). Meta-regression analyses explored the influence of duration of follow-up, median age and proportion of patients with small tumor size, nodal involvement, high grade, ductal subtype, ER expression and HER2 overexpression or amplification on the OR for each outcome. Meta-regression was performed using SPSS version 25 (IBM Corp, Armonk, NY, USA) using the weighted least squares (mixed effect) function. Statistical significance was defined as P < 0.05. No corrections were made for multiple significance testing.
Results
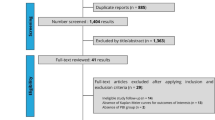
The search identified 840 studies. After exclusions (see Fig. 1), 11 publications reporting on outcomes from nine studies were included in the analysis (the GEC-ESTRO study reported on efficacy in one publication [24] and on toxicity and cosmetic outcomes in a second publication [10] while updated efficacy data for the RAPID study were presented at the 2018 San Antonio Breast Cancer Symposium [28]) [10,11,12,13, 20, 24,25,26,27,28,29]. Included studies comprised 14,514 patients. Individual study characteristics are shown in Table 1. Two studies used IORT [12, 13] and 2 studies used brachytherapy [10, 11, 24]. In one of the brachytherapy studies, the protocol allowed 50 Gy limited-field external beam irradiation for patients who were technically unsuitable for brachytherapy and 31% of the study cohort received this intervention [11]. Four studies used EBRT for PBI, of these two studies used Accelerated PBI (APBI) using three-dimensional conformal external beam radiation therapy (3D-CRT) [26, 27], one study used APBI with intensity modulated radiotherapy (IMRT) [25] and one study used standard fractionation with IMRT [20]. In one study [20], there was also a reduced-dose group (36 Gy whole-breast radiotherapy and 40 Gy to the partial breast) that were excluded, and only data from the PBI and standard WBI groups were utilized. In one study, all PBI modalities were allowed [29]; therefore, this study was not included in the subgroup analysis. The methods used to assess local recurrence, local toxicity and cosmetics in each study are reported in Appendix A in Electronic Supplementary Material.
Efficacy
Results of the main analysis for all included efficacy outcomes and for subgroups based on type of PBI are shown in Table 2. Compared to WBI, PBI was associated with increased odds of 5-year local recurrence (Fig. 2a). In contrast, PBI was also associated with reduced odds of death without breast cancer recurrence and with improvement in OS that approached, but did not reach statistical significance (Fig. 2b, c). Similar odds of 5-year regional recurrence, contralateral breast cancer and DFS were observed between WBI and PBI (Fig. 2e, f).
Forest plots for outcomes. a Local recurrence, b death without breast cancer recurrence, c overall survival, d regional recurrence, e contralateral breast cancer, f disease free survival. Odds ratios for each trial are represented by the squares, the size of the square represents the weight of the trial in the meta-analysis, and the horizontal line crossing the square represents the 95% confidence interval. The diamonds represent the estimated pooled effect. All P values are two-sided
Subgroup analysis showed a significant difference between PBI modality and local recurrence with lower magnitude of inferiority when PBI delivered as EBRT (OR 1.08), compared to PBI delivered as IORT or brachytherapy (OR 3.10 and OR 1.44, respectively), subgroup difference P = 0.003. Otherwise, subgroup analyses based on type of PBI showed generally similar results (Table 2; Fig. 2a–f), and although the benefit in 5 year death without breast cancer recurrence seemed to be driven by IORT, PBI modality did not have statistically significant impact on the results. Sensitivity analyses did not show significant effect on the results (Appendices B and C in Electronic Supplementary Material).
Results of meta-regression for efficacy endpoints are shown in Appendix D in Electronic Supplementary Material. Nodal involvement was associated with significantly greater magnitude of effect on the odds of local recurrence (P = 0.027), while protection from death without breast cancer recurrence and OS was reduced with larger tumor size (P = 0.011 and P = 0.019, respectively). Invasive ductal carcinoma was associated with reduced magnitude of effect on regional recurrence compared to other morphologic subtypes; however, this approached, but did not meet statistical significance (P = 0.062). Protection from contralateral breast cancer with PBI was greater in studies with older median age. Finally, while larger and high-grade tumors were associated with a greater magnitude of effect on local recurrence, these associations approached, but did not meet statistical significance (P = 0.075 and P = 0.105, respectively). No other significant associations were observed.
Toxicity
Results of the main analysis for all included toxicity outcomes are shown in Table 3. Compared to WBI, PBI was associated with increased odds of fat necrosis. PBI was also associated with increased odds of breast pain, which approached, but did not reach significance (OR 1.17, 95% CI 0.98–1.40, P = 0.07). There was no association between PBI and secondary malignancy (excluding breast cancer). PBI and WBI also had similar odds for telangiectasia and breast induration and fibrosis. Data on cardiac mortality were available in two studies [13, 20]; therefore, data were not pooled. Overall, cardiac mortality was low, but in both studies there were numerically more cardiac deaths with WBI compared to PBI (absolute difference between 0.34–0.44%). Data on lung fibrosis were limited. In one study, a subgroup of volunteers agreed to undergo follow-up spiral CT imaging [12]. Pulmonary fibrosis was seen in 4.2% (4/95) of the patients treated with PBI compared to 45.8% (38/83) in the control group. One study reported symptomatic lung fibrosis and showed comparable incidence (0.6% in both groups) [20]. Data were available from only 2 studies for hyperpigmentation [10, 12] and arm lymphedema [10, 20]; therefore, data were not pooled. However, compared to WBI, women treated with PBI had fewer events of hyperpigmentation (absolute difference range between 4.6–13.7%) and arm lymphedema (absolute difference range between 1.3–1.8%).
The results of the meta-regression for late adverse events are shown in Appendix E in Electronic Supplementary Material. Studies with higher proportion of ER positive disease had a lower magnitude of effect on the odds of fibrosis or induration (P = 0.042). Studies with longer duration of follow-up had significantly lower increases in the relative odds for breast pain. There were no other significant associations between the evaluated variables and late adverse events.
Cosmetic results
Data on cosmetic results were reported explicitly in 4 studies [10, 11, 25, 27] and were estimated from a figure in one study [26]. PBI was associated with higher odds of fair to poor cosmetic results (rather than good to excellent) which approached but did not meet statistical significance (OR 1.23, 95% CI 0.99–1.52, P = 0.06). In absolute terms, 15.5% of patients in the PBI group had fair to poor cosmesis compared to 13.1% in the WBI group. The weighted pool absolute difference was 2.3%. Sensitivity analysis is shown in Appendix B in Electronic Supplementary Material.
Discussion
Adjuvant radiation after lumpectomy has shown to improve local control and improve survival compared to lumpectomy alone [32]. However, radiation results in increased adverse events including cardiac toxicity and secondary malignancies [4, 5, 33]. As PBI targets only the volume of breast tissue at highest risk of recurrence, reduction in radiation doses to organs at risk can be achieved, thereby potentially reducing the risk of long-term complications [8, 9].
The majority of the included patients in this meta-analysis had ER positive, small tumors (≤ 3 cm), without nodal involvement. We found PBI was associated with significantly higher odds for local recurrence compared to WBI; however, subgroup analysis by PBI modality showed significant difference. The highest risk of local recurrence was observed with IORT, whereas when EBRT was used the odds for local recurrence were equivalent to WBI. This is consistent with a previous meta-analysis that showed comparable local recurrence in studies that used PBI with imaging based planning (EBRT and brachytherapy) as opposed to studies that did not, suggesting that selection of treatment technique could attenuate the inferior local recurrence risk with PBI [14]. In contrast to IORT, PBI given with EBRT utilizes imaging based planning to better define the target volume, and compared to brachytherapy, EBRT-based PBI provides more generous margins, which may explain this observation. Of note, the IORT studies included more patients with high-grade disease and with nodal involvement (26.6% in the ELIOT study and 16.1% in TARGIT-A), including even patients with more than 3 lymph nodes involved [12, 13]. The worse prognostic features of the patients included in these studies could account for at least part of the high local recurrence rate. This explanation is supported by the meta-regression results showing significantly higher magnitude of effect in patients with nodal involvement and a borderline significantly greater magnitude of effect on local recurrence with high-grade disease. These data suggest that PBI utilizing EBRT may be the optimal method of achieving adequate local control while the optimal method of limiting toxicity remains uncertain.
This literature-based meta-analysis has also shown PBI is associated with significantly reduced odds for death without breast cancer recurrence compared to WBI. While data from prior meta-analyses already reported similar results [14, 17], our meta-analysis is much larger, comprising 14,514 patients and included only modern studies. Additionally, the results of recently presented data from NSABP B39 [29] trial and updated efficacy results from the RAPID trial [28] are also included in this meta-analysis.
The increased risk of major coronary events with breast irradiation is well established, is evident within the first 5 years after radiation exposure and persists for at least 20 years [2]. The association between radiation and coronary events is influenced by the mean heart dose. With changes in field design, utilization of advanced planning techniques and breathing manipulation, radiation exposure to the heart has been reduced over the last few decades [34]. However, despite this, the mean radiation dose to the heart and left anterior descending (LAD) coronary artery with left-tangential irradiation remains clinically significant [35]. All modalities of PBI have shown to be heart sparing, with lower volumes and heart doses compared to WBI, especially in left sided tumors [8, 9, 36]. In our study, data on cardiac mortality were available in only two studies [13, 20]; therefore, meta-analysis was not performed. Cardiac mortality was uncommon and seen in fewer than 1% of patients; however, there was numerically lower cardiac mortality in patients treated with PBI.
An increase in secondary malignancies has also been reported in breast cancer survivors with an excess risk attributed to radiation [37]. In our analysis, fewer secondary malignancies were noted in the PBI group, with a weighted absolute difference of 0.4%, without reaching statistical significance. This might be attributed to relatively short follow-up time in our study, as the risk is more evident with longer follow-up [38]. Additionally, caution is urged when interpreting these results, as the number of events for both cardiac mortality and secondary malignancies was very small.
The magnitude of improved OS and reduced death without breast cancer recurrence was significantly lower in patients with larger tumors. These results can be partly explained by the worse prognosis associated with larger tumors. This finding may also be explained by differences in radiation volume. Larger tumor requires more extensive radiation fields even when PBI is delivered; therefore, the advantage of reduced radiation to organs at risks compared to WBI is expected to be lower for larger tumor.
A better understanding of breast cancer biology during the last decades has allowed tailoring of adjuvant systemic treatment, with safe omission of chemotherapy for many patients [39]. Breast tumor subtypes have prognostic and predictive values which can be utilized to guide systemic decision making [40, 41]. Implications of genomic risk and tumor subtypes on adjuvant radiation treatment are emerging [42, 43]. Given the low rates of recurrence in early-stage ER positive breast cancer in the era of effective systemic treatment [44], reducing radiation treatment has become the subject of many investigations and there are several ongoing studies evaluating omission of adjuvant radiation based on risk of recurrence in multi-gene assays [45,46,47]. A recent meta-analysis showed that compared to omission of radiation, WBI in elderly patients (≥ 70) with early breast cancer who were treated with adjuvant endocrine treatment resulted in reduced local recurrence, but had no effect on distant recurrence or overall survival [48]. As these results are limited to a subgroup of older women with low risk tumors, further studies comparing PBI and omission of radiation in younger women are desired. A Surveillance, Epidemiology, and End Results Program (SEER) analysis found that the proportion of women with node negative early breast cancer eligible for WBI alternatives is high, with 75% of women estimated to be eligible for treatment with PBI and up to 20% eligible for endocrine therapy without radiation [49]. In light of this and our findings of decreased mortality with PBI compared to WBI, tailoring radiation including the use of PBI should be considered more often. Individual decisions should be based on patient age, comorbidities, tumor characteristics and personal preferences, as alternatives to WBI would probably be endorsed by many women.
Our study has several limitations. First, this is a literature-based rather than an individual patient-based meta-analysis. Consequently, it is subject to publication bias. Additionally, the lack of individual patient data necessitated the use of meta-regression on trial summary data which is less informative. Second, there was heterogeneity in the included studies especially in the utilization of different modalities and techniques for PBI. A subgroup analysis according to method of radiation delivery was performed in order to understand better the results; however, the potential for residual heterogeneity related to treatment delivery results in uncertainty about the precision of the reported results. Additionally, while analyses utilizing fixed-effect were subjected to a sensitivity analysis using random-effects, this may not fully address heterogeneity. Also, contrary to several previous meta-analyses [14, 17], we planned to include only studies published in the last decade, in an attempt to focus on studies using modern radiation techniques and contemporary systemic treatment, thus reducing heterogeneity. Third, in the TARGIT-A study there was substantial contamination with approximately 15% of the women allocated to receive PBI, receiving both WBI and IORT [13]. However, sensitivity analysis excluding this study did not affect the results. Fourth, there was variability in the duration of follow-up between the included studies although meta-regression showed that except for chronic breast pain, duration of follow-up did not influence the results. Additionally, meta-regression for adjuvant trastuzumab was not applicable as data were scarce. Finally, the overall number of deaths was low and longer duration of follow-up is required to determine survival-based outcomes, especially in patients with ER positive disease who represented the majority of patients in included studies. Additionally, the ongoing improvement in radiation techniques is expected to further reduce the risk of cardiotoxicity; therefore, the difference in death without breast cancer recurrence between WBI and PBI might be even smaller. In light of the relatively short duration of follow-up and the reduced doses to organs at risk when utilizing modern WBI techniques, caution is recommended in the conclusions that PBI is associated with improved survival compared to WBI. Additionally, while our meta-analysis includes studies with well-established techniques for PBI [11, 20, 24, 25], studies utilizing IORT were also included; however, uncertainty exists regarding the latter mainly due to immature data in the TARGIT trial [13, 30] and inferior outcomes in the ELIOT trial [12].
Conclusions
Despite higher odds of local recurrence and increased toxicity, compared to WBI, PBI is associated with significantly reduced 5-year risk of death without breast cancer recurrence and a borderline significant improvement in 5-year OS. Improved outcomes are likely explained by the observation that local recurrence has a limited effect on long-term breast-cancer outcomes, and PBI is associated with reduced non-breast cancer death compared with WBI. However, further follow-up is desired to better understand of the impact of PBI on survival. The balance between benefit and risk of PBI appears optimal in women with smaller ER positive tumors and without nodal involvement.
References
Darby S, McGale P, Correa C, Taylor C, Arriagada R, Clarke M et al (2011) Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet 378(9804):1707–1716
Darby SC, Ewertz M, McGale P, Bennet AM, Blom-Goldman U, Brønnum D et al (2013) Risk of ischemic heart disease in women after radiotherapy for breast cancer. N Engl J Med 368(11):987–998
Taylor C, Correa C, Duane FK, Aznar MC, Anderson SJ, Bergh J et al (2017) Estimating the risks for lung cancer radiotherapy: evidence from modern radiation doses to the lungs and heart and from previous randomized trials. J Clin Oncol 35(15):1641–1649
Henson KE, McGale P, Taylor C, Darby SC (2013) Radiation-related mortality from heart disease and lung cancer more than 20 years after radiotherapy for breast cancer. Br J Cancer 108(1):179–182
Veronesi U, Marubini E, Mariani L, Galimberti V, Luini A, Veronesi P et al (2001) Radiotherapy after breast-conserving surgery in small breast carcinoma: long-term results of a randomized trial. Ann Oncol 12(7):997–1003
Liljegren G, Holmberg L, Bergh J, Lindgren A, Tabár L, Nordgren H et al (1999) 10-year results after sector resection with or without post-operative radiotherapy for stage I breast cancer: a randomized trial. J Clin Oncol 17(8):2326–2333
Smith TE, Lee D, Turner BC, Carter D, Haffty BG (2000) True recurrence vs. new primary ipsilateral breast tumor relapse: an analysis of clinical and pathologic differences and their implications in natural history, prognoses, and therapeutic management. Int J Radiat Oncol Biol Phys 48(5):1281–1289
Stewart AJ, O’Farrell DA, Cormack RA, Hansen JL, Khan AJ, Mutyala S et al (2008) Dose volume histogram analysis of normal structures associated with accelerated partial breast irradiation delivered by high dose rate brachytherapy and comparison with whole breast external beam radiotherapy fields. Radiat Oncol 3:39
Gale AA, Jain AK, Vallow LA, Serago CF, Buskirk SJ, Heckman MG (2009) Cardiac dose evaluation for 3-dimensional conformal partial breast irradiation compared with whole breast irradiation. J Appl Clin Med Phys 10(1):2868
Polgár C, Ott OJ, Hildebrandt G, Kauer-Dorner D, Knauerhase H, Major T et al (2017) Late side-effects and cosmetic results of accelerated partial breast irradiation with interstitial brachytherapy versus whole- breast irradiation after breast-conserving surgery for low-risk invasive and in-situ carcinoma of the female breast: 5-year results of a randomised, controlled, phase 3 trial. Lancet Oncol 18(2):259–268
Polgár C, Fodor J, Major T, Sulyok Z, Kásler M (2013) Breast-conserving therapy with partial or whole breast irradiation: ten-year results of the Budapest randomized trial. Radiother Oncol 108(2):197–202
Veronesi U, Orecchia R, Maisonneuve P, Viale G, Rotmensz N, Sangalli C et al (2013) Intraoperative radiotherapy versus external radiotherapy for early breast cancer (ELIOT): a randomised controlled equivalence trial. Lancet Oncol 14(13):1269–1277
Vaidya JS, Wenz F, Bulsara M, Tobias JS, Joseph DJ, Keshtgar M et al (2014) Risk-adapted targeted intraoperative radiotherapy versus whole-breast radiotherapy for breast cancer: 5-year results for local control and overall survival from the TARGIT-A randomised trial. Lancet 383(9917):603–613
Liu G, Dong Z, Huang B, Liu Y, Tang Y, Li Q et al (2017) Efficacy and safety of accelerated partial breast irradiation: a meta-analysis of published randomized studies. Oncotarget 8(35):59581–59591
Hickey BE, Lehman M, Francis DP, See AM (2016) Partial breast irradiation for early breast cancer (review). Cochrane Database Syst Rev 7:CD007077
Huo J, Giordano SH, Smith BD et al (2016) Contemporary toxicity profile of breast brachytherapy versus external beam radiation after lumpectomy for breast cancer. Int J Radiat Oncol Biol Phys 94:709–718
Vaidya JS, Bulsara M, Wenz F, Coombs N, Singer J, Ebbs S et al (2016) Reduced mortality with partial-breast irradiation for early breast cancer: a meta-analysis of randomized trials. Int J Radiat Oncol Biol Phys 96(2):259–265
Correa C, Harris EE, Leonardi MC. Smith BD, Taghian AG, Thompson AM et al (2017) Accelerated partial breast irradiation: executive summary for the update of an ASTRO evidence-based consensus statement. Pract Radiat Oncol 7(2):73–79
Polgár C, Van Limbergen E, Pötter R, Kovács G, Polo A, Lyczek J et al (2010) Patient selection for accelerated partial-breast irradiation (APBI) after breast-conserving surgery: recommendations of the Groupe Européen de Curiethérapie-European Society for Therapeutic Radiology and oncology (GEC-ESTRO) breast cancer working group based on clinical evidence (2009). Radiother Oncol 94(3):264–273
Coles CE, Griffin CL, Kirby AM, Titley J, Agrawal RK, Alhasso A et al (2017) Partial-breast radiotherapy after breast conservation surgery for patients with early breast cancer (UK IMPORT LOW trial): 5-year results from a multicentre, randomised, controlled, phase 3, non-inferiority trial. Lancet 390(10099):1048–1060
Sweeting MJ, Sutton AJ, Lambert PC (2004) What to add to nothing? Use and avoidance of continuity corrections in meta-analysis of sparse data. Stat Med 23(9):1351–1375
Higgins JPT, Deeks JJ, Altman DG (2011) Meta-analysis of rare events. In: Higgins JPT, Green S (eds) Cochrane handbook for systematic reviews of interventions (version 5.1.0). The Cochrane Collaboration, London
Deeks JJ (2001) Systematic reviews in health care: Systematic reviews of evaluations of diagnostic and screening tests. Br Med J 323(7305):157–162
Strnad V, Ott OJ, Hildebrandt G, Kauer-Dorner D, Knauerhase H, Major T et al (2016) 5-year results of accelerated partial breast irradiation using sole interstitial multicatheter brachytherapy versus whole-breast irradiation with boost after breast-conserving surgery for low-risk invasive and in-situ carcinoma of the female breast: a randomised, phase 3, non-inferiority trial. Lancet 387(10015):229–238
Livi L, Meattini I, Marrazzo L, Simontacchi G, Pallotta S, Saieva C et al (2015) Accelerated partial breast irradiation using intensity-modulated radiotherapy versus whole breast irradiation: 5-year survival analysis of a phase 3 randomised controlled trial. Eur J Cancer 51(4):451–463
Rodriguez N, Sanz X, Dengra J, Foro P, Membrive I, Reig A et al (2013) Five-year outcomes, cosmesis, and toxicity with 3-dimensional conformal external beam radiation therapy to deliver accelerated partial breast irradiation. Int J Radiat Oncol Biol Phys 87(5):1051–1057
Olivotto IA, Whelan TJ, Parpia S, Kim DH, Berrang T, Truong PT et al (2013) Interim cosmetic and toxicity results from RAPID: a randomized trial of accelerated partial breast irradiation using three-dimensional conformal external beam radiation therapy. J Clin Oncol 31(32):4038–4045
Whelan T, Julian J, Levine M, Berrang T, Kim D-H, Gu CS et al (2018) RAPID: a randomized trial of accelerated partial breast irradiation using 3-dimensional conformal radiotherapy (3D-CRT). In: San Antonio Breast cancer symposium, GS4-03
Vicini FA, Cecchini RS, White JR, Julian TB, Arthur DW, Rabinovitch RA et al (2018) Primary results of NSABP B-39/RTOG 0413 (NRG Oncology): a randomized phase III study of conventional whole breast irradiation (WBI) versus partial breast irradiation (PBI) for women with stage 0, I, or II breast cancer. In: San Antonio breast cancer symposium, GS4-04
Vaidya JS, Wenz F, Bulsara M, Tobias JS, Joseph DJ, Saunders C et al (2016) An international randomized controlled trial to compare TARGeted Intraoperative radioTherapy (TARGIT) with conventional postoperative radiotherapy after breast-conserving surgery for women with early-stage breast cancer (the TARGIT-A trial). Health Technol Assess 20:1–188
Peterson D, Truong PT, Parpia S, Olivotto IA, Berrang T, Kim DH et al (2015) Predictors of adverse cosmetic outcome in the RAPID trial: an exploratory analysis. Int J Radiat Oncol Biol Phys 91(5):968–976
Clarke M, Collins R, Darby S, Davies C, Elphinstone P, Evans V et al (2005) Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet 366(9503):2087–2106
Cuzick J, Stewart H, Rutqvist L, Houghton J, Edwards R, Redmond C et al (1994) Cause-specific mortality in long-term survivors of breast cancer who participated in trials of radiotherapy. J Clin Oncol 12(3):447–453
Drost L, Yee C, Lam H, Zhang L, Wronski M, McCann C et al (2018) A systematic review of heart dose in breast radiotherapy. Clin Breast Cancer 18:e819–e824
Taylor CW, Wang Z, Macaulay E, Jagsi R, Duane F, Darby SC (2015) Exposure of the heart in breast cancer radiation therapy: a systematic review of heart doses published during 2003–2013. Int J Radiat Oncol Biol Phys 93(4):845–853
Kirby AM, Evans PM, Donovan EM, Convery HM, Haviland JS, Yarnold JR (2010) Prone versus supine positioning for whole and partial-breast radiotherapy: a comparison of non-target tissue dosimetry. Radiother Oncol 96(2):178–184
Burt LM, Ying J, Poppe MM, Suneja G, Gaffney DK (2017) Risk of secondary malignancies after radiation therapy for breast cancer: comprehensive results. Breast 35:122–129
De bruin ML, Sparidans J, van’t Veer MB, Noordijk EM, Louwman MW, Zijlstra JM et al (2009) Breast cancer risk in female survivors of Hodgkin’s lymphoma: lower risk after smaller radiation volumes. J Clin Oncol 27(26):4239–4246
Cardoso F, van’t Veer LJ, Bogaerts J, Slaets L, Viale G, Delaloge S et al (2016) 70-gene signature as an aid to treatment decisions in early-stage breast cancer. N Engl J Med 375(8):717–729
Park YH, Lee SJ, Cho EY, Choi YL, Lee JE, Nam SJ et al (2011) Clinical relevance of TNM staging system according to breast cancer subtypes. Ann Oncol 22(7):1554–1560
Harris LN, Ismalla N, McShane LM, Andre F, Collyar DE, Gonzalez-Angulo AM et al (2016) Use of biomarkers to guide decisions on adjuvant systemic therapy for women with early-stage invasive breast cancer: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol 34(10):1134–1150
Horton JK, Jagsi R, Woodward WA, Ho A (2018) Breast cancer biology: clinical implications for breast radiation therapy. Int J Radiat Oncol Biol Phys 100(1):23–37
Mamounas EP, Liu Q, Paik S, Baehner FL, Tang G, Jeong JH et al (2017) 21 Gene recurrence score and locoregional recurrence in node-positive/ER-positive breast cancer treated with chemo-endocrine therapy.J Natl Cancer Inst 109(4)
Bouganim N, Tsvetkova E, Clemons M, Amir E (2013) Evolution of sites of recurrence after early breast cancer over the last 20 years: implications for patient care and future research. Breast Cancer Res Treat 139(2):603–606
Prospective cohort study evaluating risk of local recurrence following breast conserving surgery and endocrine therapy in Low Risk Luminal A Breast Cancer (LUMINA). https://clinicaltrials.gov/ct2/show/NCT01791829. Accessed 15 May 2018
The IDEA Study (Individualized Decisions for Endocrine Therapy Alone). https://clinicaltrials.gov/ct2/show/NCT02400190. Accessed 15 May 2018
The PRECISION Trial (Profiling Early Breast Cancer for Radiotherapy Omission): a phase II study of breast-conserving surgery without adjuvant radiotherapy for favorable-risk breast cancer. https://clinicaltrials.gov/ct2/show/NCT02653755. Accessed 15 May 2018
Chesney TR, Yin JX, Rajaee N, Tricco AC, Fyles AW, Acuna SA et al (2017) Tamoxifen with radiotherapy compared with Tamoxifen alone in elderly women with early-stage breast cancer treated with breast conserving surgery: a systematic review and meta-analysis. Radiother Oncol 123(1):1–9
Manyam BV, Tendulkar R, Cherian S, Vicini F, Badiyan SN, Shah C (2018) Evaluating candidacy for hypofractionated radiation therapy, accelerated partial breast irradiation, and endocrine therapy after breast conserving surgery: a Surveillance Epidemiology and End Results (SEER) analysis. Am J Clin Oncol 41(6):526–531
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Yasmin Korzets, Anthony Fyles, and Daniel Shepshelovich declare that they have no conflict of interest. Eitan Amir declares that he has received fees from Genentech/Roche for Expert Testimony and from Apobiologix for Advisory Boards. These fees were outside of the submitted work. Hadar Goldvaser declares honorarium payment from Roche for invited speaker. These fees were outside of the submitted work.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Korzets, Y., Fyles, A., Shepshelovich, D. et al. Toxicity and clinical outcomes of partial breast irradiation compared to whole breast irradiation for early-stage breast cancer: a systematic review and meta-analysis. Breast Cancer Res Treat 175, 531–545 (2019). https://doi.org/10.1007/s10549-019-05209-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-019-05209-9