Abstract
Purpose
As clinical studies have correlated RANK expression levels with survival in breast cancer, and that RANK signaling is dependent on its cognate ligand RANKL, we hypothesized that dual protein expression further stratifies the poor outcome in TNBC.
Methods
RANK mRNA and protein expression was evaluated in TNBC using genomic databases, cell lines and in a tissue microarray of curated primary tumor samples derived from 87 patients with TNBC. RANK expression was evaluated either by Mann–Whitney U test on log-normalized gene expression data or by Student’s t test on FACS data. Analysis of RANK and RANKL immunostaining was calculated by H-score, and correlations to clinical factors performed using χ 2 or Fisher’s exact test. Associations with RFS and OS were assessed using univariate and multivariate Cox proportional hazard models. Survival estimates were generated using the Kaplan–Meier method.
Results
In three distinct datasets spanning 684 samples, RANK mRNA expression was higher in primary tumors derived from TNBC patients than from those with other molecular subtypes (P < 0.01). Cell surface-localized RANK protein was consistently higher in TNBC cell lines (P = 0.037). In clinical samples, TNBC patients that expressed both RANK and RANKL proteins had significantly worse RFS (P = 0.0032) and OS (P = 0.004) than patients with RANK-positive, RANKL-negative tumors. RANKL was an independent, poor prognostic factor for RFS (P = 0.04) and OS (P = 0.01) in multivariate analysis in samples that expressed both RANK and RANKL.
Conclusions
RANK and RANKL co-expression is associated with poor RFS and OS in patients with TNBC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Triple-negative breast cancer (TNBC), which lacks estrogen receptor (ER) and progesterone receptor (PR) expression and human epidermal growth factor receptor-2 (HER2) amplification, accounts for approximately 15–20% of all breast cancers [1]. Despite its sensitivity to chemotherapy, TNBC remains a clinical challenge because of a high rate of relapse and a propensity to metastasize to visceral organs. Because of this high rate of metastasis and a lack of effective targeted therapies, the 5-year survival rate for patients with TNBC is poorer than that of patients with hormone-receptor positive breast cancer [2–4]. Thus, there is a critical need to identify clinically relevant molecules that are prognostic of patient outcome and that have the potential to provide a rationale to develop as a targeted therapy.
The receptor activator of nuclear factor-κB (RANK) pathway is an emerging clinical target in breast cancer. RANK and its canonical ligand, RANKL, are key molecules in bone metabolism and bone pathophysiology, and in normal mammary gland development [5, 6]. RANKL, which belongs to the tumor necrosis factor (TNF) superfamily, is the only known molecular agonist for RANK that is expressed on the cell surface or secreted into the extracellular milieu [7]. Upon ligation to its cognate receptor, RANKL can induce the recruitment of intracellular adaptor molecules (TNF receptor-associated factors) that transduce downstream signals [8]. Within the developing breast, RANK-RANKL signaling controls cellular growth and ductal branching morphogenesis, which is deregulated during mammary carcinogenesis [9]. Further, stromal RANKL can enhance pro-survival and proliferative signals of RANK-positive epithelial cells during alveologenesis [7, 9, 10]. Preclinical studies have suggested that RANK may enhance tumorigenic potential through the expansion of “stem-like” cell populations that aid cancer cell migration, invasion, and resistance to chemotherapy [5, 11–14]. Moreover, targeted gene ablation of RANK or treatment with RANK-Fc, a fusion protein that can neutralize RANK signaling, did not affect primary tumor growth but did significantly inhibit lung and bone metastasis in preclinical models [5, 11, 15]. Collectively, these reports suggest that activation of RANK-RANKL signaling is involved in tumor development and that targeted inhibition of this pathway may be a viable therapeutic strategy against metastatic breast cancers.
Because of the functional roles of RANK and RANKL in metastatic progression, there has been much interest in determining whether RANK or RANKL can be used as a marker in patients with breast cancer [16–19]. Initial studies have suggested that RANK expression correlates with shorter relapse-free survival (RFS) and is associated with bone-tropic metastasis [18, 19]. In an analysis of primary invasive breast tumors from the neoadjuvant GeparTrio study, RANK expression, but not RANKL expression, was associated with RFS and overall survival (OS) [16]. Moreover, RANK expression was associated with pathological complete response and was detected more frequently in poorly differentiated, highly proliferative, and hormone-receptor negative tumors. From these clinical association studies, it is clear that RANK may play a role in less differentiated breast tumors, such as TNBC.
With Food and Drug Administration-approved RANK-RANKL inhibitors entering the clinic, it is crucial to identify specific subpopulations of breast cancer patients who may benefit from their use. Previous studies have only assessed the relationships between expression of one marker, either RANK or RANKL, and clinical correlates. As activation of canonical RANK signaling requires concomitant expression of RANK and RANKL proteins, we hypothesized that dual expression of these proteins in TNBC would be superior to single marker expression in the stratification of patient outcome. To test this hypothesis, we analyzed the expression of RANK and RANKL in preclinical and clinically derived primary tumor specimens from patients with TNBC.
Methods
Cell culture and reagents
Human TNBC and non-TNBC cell lines were obtained from ATCC and validated by the Characterized Cell Line Core Facility at The University of Texas MD Anderson Cancer Center using a short-term tandem repeat methodology based on a primer extension to detect single base mutations. Cells used for experiments were grown in culture for no longer than 2 months. Prior to use, we screened all cell lines for mycoplasma contamination with the MycoAlert Mycoplasma Detection Kit (catalog #LT07-418; Lonza, Rochester, NY). All cell lines tested negative for mycoplasma. MDA-MB-231, MDA-MB-468, KPL-4, BT-474, and BT-20 cells were cultured in DMEM/F12 medium (catalog #12634-010; Life Technologies, Inc., Grand Island, NY) supplemented with 10% fetal bovine serum (catalog #10438-026; Life Technologies), and 1% antimicrobial-antibiotic (catalog #15240-062; Life Technologies). SUM159 cells were cultured in Ham’s F12 medium supplemented with 5% fetal bovine serum, 5 µg/mL insulin (catalog #I9278; Sigma-Aldrich St. Louis, MO), 1 µg/mL hydrocortisone (catalog #H0888; Sigma-Aldrich), and 1% antimicrobial-antibiotic. HCC1954 cells were cultured in RPMI medium supplemented with 10% fetal bovine serum and 1% antimicrobial-antibiotic. Flow cytometry buffer consisted of 2% fetal bovine serum and 0.005% NaV3 in phosphate-buffered saline (catalog #10010-023; Life Technologies). RANK antibody N2-B10 (7.02 mg/mL) was provided by Amgen, Inc. (Seattle, WA).
cDNA microarray data analysis of three independent public datasets
From the GeneCards website (http://www.genecards.org/), a RANK mRNA probe set (TNFRSF11A:207037_at) for the Affymetrix 133a microarray chip was identified and used to analyze RANK mRNA expression levels. Three independent publicly available datasets were used to test whether RANK mRNA expression level differed between TNBC and non-TNBC. The raw and normalized gene expression data and patients’ characteristics are available on GEO (http://www.ncbi.nlm.nih.gov/geo). Accession numbers are GSE7390, GSE2034, and GSE11121.
Flow cytometry analysis
TNBC and non-TNBC cells (1 × 106 cells per sample) were blocked for 20 min at 4 °C in 0.1 mL of fluorescence-activated cell sorting (FACS) blocking buffer (5% goat serum and 0.005% NaV3 in phosphate-buffered saline), and then immunostained with anti-RANK monoclonal antibody (N2-B10; Amgen) or an IgG isotype control for 30 min. Cells were then washed twice with 1 mL of FACS buffer and incubated with a goat anti-mouse allophycocyanin-conjugated secondary antibody (catalog #115-136-07; Jackson ImmunoResearch Laboratories, Inc., West Grove, PA) at 1:200 in FACS buffer for 20 min. Following this, the cells were washed twice with 0.4 mL of FACS buffer and re-suspended in 0.4 mL of FACS buffer containing 4',6-Diamidino-2-Phenylindole) (5 mg/mL; catalog #D1306; Life Technologies) as a marker for viability. FlowJo V10 software was used to measure RANK expression on individual cells.
Patients
Our tissue microarray was constructed from archived primary breast tumor samples from 109 patients who were diagnosed with triple-negative breast cancer between March 1993 and April 2009 and who had pathological evaluation of ER, PR, and HER2 expression [20]. TNBC samples were histologically defined based on American Society of Clinical Oncology guidelines [21]. ER-negative and PR-negative status was defined as <1% of cells having positive immunohistochemical staining for the protein. HER2-negative status was defined as a HER2/CEP17 (centromeric probe for chromosome 17) ratio of <2.0 by fluorescent in situ hybridization and/or an intensity scored as 0, 1+ , or 2+ on immunohistochemical staining [21, 22]. Patient characteristics were tabulated, including age, menopausal status, histology, pathological stage, nuclear grade, lymphovascular invasion, and RANKL expression. We excluded 14 of the 109 patients from this study as they did not have adequate tissue to be evaluated. Of the remaining 95 patients, we excluded a further 8 patients in whom ER and/or PR was not measured as a continuous variable or evaluation of ER and/or PR status was inconsistent with American Society of Clinical Oncology guidelines [21]. The final number of patients in this study was 87. The median age of patients in our cohort was 53 years (range 22–74 years), and we used age 50 years as the cut-off for dichotomizing age. All samples were collected under a protocol approved by the Institutional Review Board at MD Anderson Cancer Center (LAB05-0530).
Immunohistochemical staining and scoring
The tissue microarray was stained with anti-human RANK (N-1H8; Amgen) or RANKL (M366; Amgen) mouse monoclonal antibodies or isotype-matched control mouse IgG as previously described [23]. The specificities of the RANK and RANKL antibodies were previously reported [24]. RANKL and RANK expression within the primary tumors were scored individually according to the semi-quantitative histochemical score (H-score) [25] and interpreted by a pathologist (D.B.) blinded to any sample identification. The percentage of RANKL-positive tumor cells and RANK-positive tumor cells was multiplied by staining intensity: 0 (absent), 1 (weak intensity), 2 (moderate intensity), or 3 (strong intensity). The H-score, the sum of all products, ranged from 0 to 300. Patients with TNBC were stratified according to RANK H-scores as having RANK-positive (H-score > 0) or RANK-negative (H-score = 0) TNBC. For RANKL expression, tumors were stratified as being RANKL-positive (H-score > 0) or RANKL-negative (H-score = 0).
Statistical analyses
For cDNA microarray analysis, cases were normalized with the MAS5 algorithm, and RANK mRNA gene expression was log-normalized and significance calculated by the Mann–Whitney U Test. Dot-plots were constructed using GraphPad Prism 6 software, with horizontal bars representing the mean of the data ± SEM. Student’s t test was used to calculate the mean (SEM). P < 0.05 was considered to be significant. The χ 2 test and Fisher’s exact test were used to evaluate the association between two categorical variables of patient characteristics. Overall survival (OS) was defined from the date of surgery to that of death, and relapse-free survival (RFS) was defined from the date of surgery to that of first local or distant metastasis or loss to follow-up, whichever came earlier. Patients who died before detection of a recurrence event were right censored at the date of death. Kaplan–Meier survival curves were used to estimate the survival of patients with RANK-positive primary tumors and patients with RANK-negative primary tumors. To assess the effects of RANK-RANKL dual expression, survival curves were generated separately for patients with RANK-positive primary tumors and patients with RANK-negative primary tumors. P values were generated using the log-rank test. Univariate and multivariate Cox proportional hazard models were used to evaluate the association of covariates with survival. Independent covariates included in the analysis were age, menopausal status, histology, nuclear grade, pathological stage, lymphovascular invasion, and RANKL expression. Variables with P ≤ 0.25 in the univariate analysis were included in the full multivariable model. We obtained the reduced multivariable model using a backward selection approach, removing the least significant covariates from the full model one at a time, using P < 0.05 as the limit for inclusion in the analysis [26]. For all other analyses, P < 0.05 was considered statistically significant. Statistical analyses were performed with SPSS statistics version 21 (IBM Corporation, Armonk, NY) and STATA version 13 (STATA Corp, College Station, TX).
Results
RANK mRNA expression is elevated in primary TNBC tumors and is localized to the cell surface of epithelial TNBC cells
Prior to assessing RANK and RANKL protein levels in TNBC, we first evaluated these markers in three publicly available and independent cDNA microarray datasets. Out of 684 distinct breast tumor samples, we found RANK mRNA expression was elevated in tumors that were classified as TNBC (P < 0.0005) (Fig. 1a).
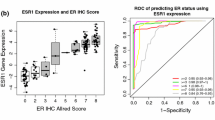
RANK expression is elevated in TNBC. a Log-normalized RANK mRNA expression was analyzed in three distinct breast cancer datasets. b Surface expression of RANK (relative median peak height) was assessed by flow cytometry in a panel of non-TNBC and TNBC cell lines. c Representative images of RANK-positive, RANKL-negative (RANK+RANKL−) and RANK-positive, RANKL-positive (RANK+RANKL+) TNBC tumor samples stained with IgG isotype control, RANK, or RANKL antibody
As RANK expression was elevated in TNBC, we next sought to identify whether RANK protein was expressed and localized to the cell surface of epithelial TNBC cells. Using FACS analysis, we determined that cell surface-localized RANK protein levels were greater on TNBC cells compared to other cell lines that were not triple-negative (P < 0.037) (Fig. 1b). Collectively, our findings suggest that RANK expression is higher in TNBC tumor samples, which is likely due to elevated cell surface levels within the epithelial compartment.
RANK and RANKL are expressed in triple-negative breast tumors
We next utilized two previously established, immunohistochemically appropriate antibodies to evaluate RANK and RANKL protein staining as markers for prognosis in a cohort of TNBC patients. Detection of these proteins in a pre-constructed TMA of 87 TNBC patient tissues demonstrated that when present, both RANK and RANKL were observed within the epithelial compartment of the primary tumor (Fig. 1c). Both proteins were identified in the cytoplasm and on the surface membrane of epithelial cancer cells. In our study cohort of 87 TNBC patient tissues, which consisted of patients with a higher percentage of RANK-positive primary tumors (72%) and RANKL-negative primary tumors (82%), there were slightly more patients older than the median age of 50 (56%) and with a majority of patients that reached post-menopausal status (70%). Most patients had early stage (I and II) tumors (94%), nuclear grade III tumors (84%), and were negative for lymphovascular invasion (LVI) (68%). As a result of our correlative analysis of TNBC stratified by RANK (Table 1) and RANKL (Table 2), we did not observe a significant correlation between these two proteins (Table 1: P = 0.36; Table 2: P = 0.36), nor did we observe a correlation between RANK or RANKL with other patient characteristics (Tables 1, 2). However, we did observe a significant correlation between RANKL-stratified TNBC and nuclear grade (Table 2: P = 0.004), which indicates that RANKL-negative TNBC patients are more likely to have a nuclear grade III tumor.
Patients with TNBC that express both RANK and RANKL within their primary tumor are associated with poor survival
We did not observe clinical associations with RFS and OS in TNBC patients when RANK or RANKL were used as independent markers. Thus, we next sought to evaluate the potential of combined RANK and RANKL expression with clinical correlates in this cohort in which we first performed a univariate analysis. From these results, we found RANK-positive TNBC patients (n = 63) with RANKL-positive primary tumors to have a significant association with poor OS (HR 6.11; 95% CI 1.52–24.62, P = 0.01) and a borderline significant association with RFS (HR 45; 95% CI 1.00–20.37; P = 0.05) (Table 3). From our multivariate analysis, RANKL was found to be an independent predictor of shorter RFS (HR 4.96; 95% CI 1.07–22.99; P = 0.04) and OS (HR 18.25; 95% CI 2.01–165.48; P = 0.01) (Table 3). Univariate analysis of patients with RANK-negative TNBC (n = 24) failed to show any significant association between RANKL and RFS or OS (Supplementary Table S1). Among TNBC patients with RANK-negative tumors (n = 24), we did not observe associations in RFS (P = 0.730) or OS (P = 0.709) when patients were stratified into RANKL-negative or RANKL-positive sub-groups (Fig. 2a). However, among TNBC patients with RANK-positive primary tumors (n = 63), patients with RANKL-positive primary tumors had significantly shorter RFS and OS than patients with RANKL-negative primary tumors (RFS, P = 0.0032; OS, P = 0.004) (Fig. 2b). Collectively, our data suggest that TNBC patients with tumors that express both RANK and RANKL have poorer survival outcomes.
Discussion
This is the first study that has specifically evaluated the relationship between the co-expression of RANK and RANKL in the prognosis of TNBC. Analyzing multiple gene expression databases, we found that RANK mRNA was consistently elevated in primary tumors with a triple-negative molecular subtype. Supporting this finding, we observed increased cell surface-localized expression of RANK on TNBC cell lines in vitro, which suggests that elevated RANK expression in TNBC tumors may be due to increased expression in cancer cells.
We utilized two highly specific antibodies to interrogate the specific localization of RANK and RANKL in a large panel of TNBC primary tumors. Moreover, we employed a scoring method that specifically assessed the localization of RANK and RANKL to the cell membrane of cancer cells, which provides a stringent evaluation of the molecular targets based on molecular function. While neither marker was able to independently predict clinical outcome, when patients were stratified by both RANK and RANKL, we observed striking correlations with RFS and OS in TNBC patients. Additionally, we observed a significant correlation between nuclear grade III and lack of RANKL expression. Based on these findings, we infer that expression of both RANK and RANKL proteins within the primary tumor is predictive of poor prognosis in TNBC patients and is suggests that canonical RANK-RANKL signaling may be involved in the aggressiveness of TNBC.
Elevated RANK expression within tumor cells has been observed in both triple-negative and “luminal-A” (ER-positive, HER2-negative) breast cancers [10, 14, 16]. Relevant to our study, Azim et al., demonstrated that RANK expression was higher in poorly differentiated, Ki67-high, and triple-negative breast tumors than in ER-positive, HER2-negative breast tumors [10]. Moreover, RANK-positive tumors were correlated with gene expression profiles that were associated with activation of the immune response and proliferation, which are two clinically actionable pathways that are emerging in distinct subsets of TNBC.
In preclinical studies, the RANK-RANKL pathway has been functionally linked to the growth and dissemination of breast tumors in vivo [5, 12, 14, 15]. Common signaling pathways activated through RANK include nuclear factor κB (NFκB), Src, and MAPKs, which are critical regulators of cell fate, survival, local inflammation, and cellular invasion [11, 29]. Thus, there has been much interest in targeting of this pathway as a potential therapeutic approach for invasive breast cancer. Indeed, recombinant Fc-tagged RANK or osteoprotegerin proteins, designed to inhibit the activation of RANKL, have been produced and can block osteoclastogenesis [30] and metastasis in preclinical models [31, 32]. A study by Yoldi et al. found that tumor-specific RANK expression, in an orthotopic model of breast adenocarcinoma, promotes survival of tumor cells [33]. This may indicate that RANKL in the tumor microenvironment, such as in tumor-infiltrating leukocytes, contributes to tumor survival. In addition, they found that systemic delivery of a RANK/RANKL antagonist (RANK-Fc) can induce tumor cell differentiation by reducing the population of cancer stem-like cells (CSCs), suggesting that inhibition of RANKL can reduce breast adenocarcinoma tumor invasion and metastasis [33].
Our analysis is limited due to the retrospective nature of the study and through potential confounding variables, such as menopausal status and nuclear grade. Of future interest would be to assess a larger cohort of TNBC patients to validate our findings and investigate the association of RANK and RANKL expression with bone metastases and the distribution of RANK and RANKL among the six proposed subtypes of TNBC [27]. It is thought that the more aggressive or stem-like nature of TNBC is derived from the immunomodulatory (IM), mesenchymal-like (M), and mesenchymal stem-like (MSL) expression profiles, which include up-regulation of cytokine pathways that are regulated by RANK and/or RANKL activity [27]. For instance, one particular study demonstrated that RANK-RANKL signaling can induce interleukin-6 production in breast cancer cells, which could in turn elevate RANK expression, creating a positive feedback loop [28].
Our study highlights the heterogeneity of RANK and RANKL expression in primary tumors from TNBC patients. Of importance, those tumors that were ‘double-positive’ occurred in a specific fraction (~20%) of TNBC patients that had poor RFS and OS. This is an extremely important clinical finding as it has major implications for the translation of RANK/RANKL as a marker and potential therapeutic target in TNBC. With the development of a Food and Drug Administration-approved, fully humanized monoclonal antibody which specifically targets RANKL (denosumab), there is increased clinical interest in characterizing the RANK-RANKL pathway in breast cancer. Future translational drug studies should consider stratifying patients based on RANK and RANKL expression as a marker for patients that may have enhanced clinical benefit.
Conclusion
This is the first study to link dual expression of RANK and RANKL with poor clinical outcomes in TNBC. The findings from this retrospective study underscore the importance of performing a more comprehensive investigation to assess serum levels of RANK, RANKL, osteoprotegerin, and activated downstream signaling molecules in patients with TNBC and their prognosis. Denosumab (Xgeva, Amgen), a humanized monoclonal antibody that inhibits RANKL, has Food and Drug Administration approval for the treatment of osteoporosis and the prevention of skeletal-related events in patients with solid tumors with bone metastases. Multiple clinical trials have been initiated to assess its anti-resorptive effects to control or prevent bone metastatic disease (NCT02366130, NCT02051218, and NCT01920568). We are conducting a phase II, prospective clinical study involving the detection of RANK and RANKL expression along with other invasive markers in circulating tumor cells from patients with advanced breast cancer treated with denosumab (NCT01952054). The clinical impact of denosumab in the prospective clinical study may offer novel insights into how we can reduce mortality associated with TNBC.
Abbreviations
- ER:
-
Estrogen receptor
- FACS:
-
Fluorescence-activated cell sorting
- HER2:
-
Human epidermal growth factor receptor 2
- OS:
-
Overall survival
- PR:
-
Progesterone receptor
- RANK:
-
Receptor activator of nuclear factor kappa B
- RANKL:
-
RANK ligand
- RFS:
-
Relapse-free survival
- TNBC:
-
Triple-negative breast cancer
- TMA:
-
Tissue microarray
References
Gluz O, Liedtke C, Gottschalk N, Pusztai L, Nitz U, Harbeck N (2009) Triple-negative breast cancer–current status and future directions. Ann Oncol 20(12):1913–1927. doi:10.1093/annonc/mdp492
Gelmon K, Dent R, Mackey JR, Laing K, McLeod D, Verma S (2012) Targeting triple-negative breast cancer: optimising therapeutic outcomes. Ann Oncol 23(9):2223–2234. doi:10.1093/annonc/mds067
Dent R, Trudeau M, Pritchard KI, Hanna WM, Kahn HK, Sawka CA, Lickley LA, Rawlinson E, Sun P, Narod SA (2007) Triple-negative breast cancer: clinical features and patterns of recurrence. Clin Cancer Res 13(15 Pt 1):4429–4434. doi:10.1158/1078-0432.CCR-06-3045
Dent R, Hanna WM, Trudeau M, Rawlinson E, Sun P, Narod SA (2009) Pattern of metastatic spread in triple-negative breast cancer. Breast Cancer Res Treat 115(2):423–428. doi:10.1007/s10549-008-0086-2
Gonzalez-Suarez E, Jacob AP, Jones J, Miller R, Roudier-Meyer MP, Erwert R, Pinkas J, Branstetter D, Dougall WC (2010) RANK ligand mediates progestin-induced mammary epithelial proliferation and carcinogenesis. Nature 468(7320):103–107. doi:10.1038/nature09495
Dougall WC (2012) Molecular pathways: osteoclast-dependent and osteoclast-independent roles of the RANKL/RANK/OPG pathway in tumorigenesis and metastasis. Clin Cancer Res 18(2):326–335. doi:10.1158/1078-0432.CCR-10-2507
Walsh MC, Choi Y (2014) Biology of the RANKL-RANK-OPG System in immunity, bone, and beyond. Front Immunol 5:511. doi:10.3389/fimmu.2014.00511
Inoue J (1997) The TRAF family protein-mediated B cell proliferation signal and the mechanism of LMP1-induced B cell transformation. Nihon Rinsho 55(2):299–304
Asselin-Labat ML, Vaillant F, Sheridan JM, Pal B, Wu D, Simpson ER, Yasuda H, Smyth GK, Martin TJ, Lindeman GJ, Visvader JE (2010) Control of mammary stem cell function by steroid hormone signalling. Nature 465(7299):798–802. doi:10.1038/nature09027
Azim HA Jr, Peccatori FA, Brohee S, Branstetter D, Loi S, Viale G, Piccart M, Dougall WC, Pruneri G, Sotiriou C (2015) RANK-ligand (RANKL) expression in young breast cancer patients and during pregnancy. Breast Cancer Res 17:24. doi:10.1186/s13058-015-0538-7
Tang ZN, Zhang F, Tang P, Qi XW, Jiang J (2011) RANKL-induced migration of MDA-MB-231 human breast cancer cells via Src and MAPK activation. Oncol Rep 26(5):1243–1250. doi:10.3892/or.2011.1368
Joshi PA, Jackson HW, Beristain AG, Di Grappa MA, Mote PA, Clarke CL, Stingl J, Waterhouse PD, Khokha R (2010) Progesterone induces adult mammary stem cell expansion. Nature 465(7299):803–807. doi:10.1038/nature09091
Schramek D, Leibbrandt A, Sigl V, Kenner L, Pospisilik JA, Lee HJ, Hanada R, Joshi PA, Aliprantis A, Glimcher L, Pasparakis M, Khokha R, Ormandy CJ, Widschwendter M, Schett G, Penninger JM (2010) Osteoclast differentiation factor RANKL controls development of progestin-driven mammary cancer. Nature 468(7320):98–102. doi:10.1038/nature09387
Palafox M, Ferrer I, Pellegrini P, Vila S, Hernandez-Ortega S, Urruticoechea A, Climent F, Soler MT, Munoz P, Vinals F, Tometsko M, Branstetter D, Dougall WC, Gonzalez-Suarez E (2012) RANK induces epithelial-mesenchymal transition and stemness in human mammary epithelial cells and promotes tumorigenesis and metastasis. Cancer Res 72(11):2879–2888. doi:10.1158/0008-5472.CAN-12-0044
Blake ML, Tometsko M, Miller R, Jones JC, Dougall WC (2014) RANK expression on breast cancer cells promotes skeletal metastasis. Clin Exp Metas 31(2):233–245. doi:10.1007/s10585-013-9624-3
Pfitzner BM, Branstetter D, Loibl S, Denkert C, Lederer B, Schmitt WD, Dombrowski F, Werner M, Rudiger T, Dougall WC, von Minckwitz G (2014) RANK expression as a prognostic and predictive marker in breast cancer. Breast Cancer Res Treat 145(2):307–315. doi:10.1007/s10549-014-2955-1
Hein A, Bayer CM, Schrauder MG, Haberle L, Heusinger K, Strick R, Ruebner M, Lux MP, Renner SP, Schulz-Wendtland R, Ekici AB, Hartmann A, Beckmann MW, Fasching PA (2014) Polymorphisms in the RANK/RANKL genes and their effect on bone specific prognosis in breast cancer patients. Biomed Res Int 2014:842452. doi:10.1155/2014/842452
Park HS, Lee A, Chae BJ, Bae JS, Song BJ, Jung SS (2014) Expression of receptor activator of nuclear factor kappa-B as a poor prognostic marker in breast cancer. J Surg Oncol 110(7):807–812. doi:10.1002/jso.23737
Zhang L, Teng Y, Zhang Y, Liu J, Xu L, Qu J, Hou K, Yang X, Liu Y, Qu X (2012) Receptor activator for nuclear factor kappa B expression predicts poor prognosis in breast cancer patients with bone metastasis but not in patients with visceral metastasis. J Clin Pathol 65(1):36–40. doi:10.1136/jclinpath-2011-200312
Parinyanitikul N, Blumenschein GR, Wu Y, Lei X, Chavez-Macgregor M, Smart M, Gonzalez-Angulo AM (2013) Mesothelin expression and survival outcomes in triple receptor negative breast cancer. Clin Breast Cancer 13(5):378–384. doi:10.1016/j.clbc.2013.05.001
Hammond ME, Hayes DF, Dowsett M, Allred DC, Hagerty KL, Badve S, Fitzgibbons PL, Francis G, Goldstein NS, Hayes M, Hicks DG, Lester S, Love R, Mangu PB, McShane L, Miller K, Osborne CK, Paik S, Perlmutter J, Rhodes A, Sasano H, Schwartz JN, Sweep FC, Taube S, Torlakovic EE, Valenstein P, Viale G, Visscher D, Wheeler T, Williams RB, Wittliff JL, Wolff AC (2010) American Society of Clinical Oncology/College Of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J Clin Oncol 28(16):2784–2795. doi:10.1200/JCO.2009.25.6529
Wolff AC, Hammond ME, Hicks DG, Dowsett M, McShane LM, Allison KH, Allred DC, Bartlett JM, Bilous M, Fitzgibbons P, Hanna W, Jenkins RB, Mangu PB, Paik S, Perez EA, Press MF, Spears PA, Vance GH, Viale G, Hayes DF, American Society of Clinical O, College of American P (2013) Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update. J Clin Oncol 31(31):3997–4013. doi:10.1200/JCO.2013.50.9984
Wood CE, Branstetter D, Jacob AP, Cline JM, Register TC, Rohrbach K, Huang LY, Borgerink H, Dougall WC (2013) Progestin effects on cell proliferation pathways in the postmenopausal mammary gland. Breast Cancer Res 15(4):62. doi:10.1186/bcr3456
Branstetter DG, Nelson SD, Manivel JC, Blay JY, Chawla S, Thomas DM, Jun S, Jacobs I (2012) Denosumab induces tumor reduction and bone formation in patients with giant-cell tumor of bone. Clin Cancer Res 18(16):4415–4424. doi:10.1158/1078-0432.CCR-12-0578
McCarty KS Jr, Miller LS, Cox EB, Konrath J, McCarty KS Sr (1985) Estrogen receptor analyses. Correlation of biochemical and immunohistochemical methods using monoclonal antireceptor antibodies. Arch Pathol Lab Med 109(8):716–721
Hosmer DW Jr, Lemeshow S (2008) Applied survival analysis: regression modeling of time to event data, 2nd edn. Wiley, New York
Lehmann BD, Bauer JA, Chen X, Sanders ME, Chakravarthy AB, Shyr Y, Pietenpol JA (2011) Identification of human triple-negative breast cancer subtypes and preclinical models for selection of targeted therapies. J Clin Invest 121(7):2750–2767. doi:10.1172/JCI45014
Zheng Y, Chow SO, Boernert K, Basel D, Mikuscheva A, Kim S, Fong-Yee C, Trivedi T, Buttgereit F, Sutherland RL, Dunstan CR, Zhou H, Seibel MJ (2014) Direct crosstalk between cancer and osteoblast lineage cells fuels metastatic growth in bone via auto-amplification of IL-6 and RANKL signaling pathways. J Bone Miner Res 29(9):1938–1949. doi:10.1002/jbmr.2231
Lacey DL, Boyle WJ, Simonet WS, Kostenuik PJ, Dougall WC, Sullivan JK, San Martin J, Dansey R (2012) Bench to bedside: elucidation of the OPG-RANK–RANKL pathway and the development of denosumab. Nat Rev Drug Discov 11(5):401–419. doi:10.1038/nrd3705
Boyle WJ, Simonet WS, Lacey DL (2003) Osteoclast differentiation and activation. Nature 423(6937):337–342. doi:10.1038/nature01658
Canon JR, Roudier M, Bryant R, Morony S, Stolina M, Kostenuik PJ, Dougall WC (2008) Inhibition of RANKL blocks skeletal tumor progression and improves survival in a mouse model of breast cancer bone metastasis. Clin Exp Metas 25(2):119–129. doi:10.1007/s10585-007-9127-1
Holland PM, Miller R, Jones J, Douangpanya H, Piasecki J, Roudier M, Dougall WC (2010) Combined therapy with the RANKL inhibitor RANK-Fc and rhApo2L/TRAIL/dulanermin reduces bone lesions and skeletal tumor burden in a model of breast cancer skeletal metastasis. Cancer Biol Ther 9(7):539–550
Yoldi G, Pellegrini P, Trinidad EM, Cordero A, Gomez-Miragaya J, Serra-Musach J, Dougall WC, Munoz P, Pujana MA, Planelles L, Gonzalez-Suarez E (2016) RANK signaling blockade reduces breast cancer recurrence by inducing tumor cell differentiation. Cancer Res 76(19):5857–5869. doi:10.1158/0008-5472.CAN-15-2745
Acknowledgements
We thank Stephanie Deming for providing editorial support on behalf of Scientific Publications at MD Anderson Cancer Center, and Albert Rhee for providing medical writing support on behalf of Amgen, Inc.
Author’s contribution
Amgen, Inc. funded the study and supported the authors in the development of the study design, and in the collection, analysis, and interpretation of data. MER, TF, DB, HM, BLE, WCD, and NU contributed to the study conception and design; MER, TF, DB, BLE, SK, XW, JR, WW, GH, DT, WCD, and NU contributed to the collection, and analysis of data; MER, TF, DB, BLE, HM, BJE, SK, XW, JMR, WAW, GNH, DT, WCD, and NTU contributed to the interpretation of the data and development of the manuscript. Medical writing support was provided by Amgen, Inc. The decision to submit was taken jointly by all authors and Amgen, Inc. All authors read and approved the final manuscript. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding
Funding support for this study was provided by Amgen, Inc. Technical support for generation of flow cytometry data was provided by The University of Texas MD Anderson Cancer Center Flow Cytometry and Cellular Imaging Core Facility, funded by the National Cancer Institute Cancer Support Grant P30CA16672.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
Author NU is principal investigator of the above-mentioned study of denosumab (NCT01952054), which is supported by Amgen, Inc. Authors WCD and DB are former employees and shareholders of Amgen, Inc. Authors MER, TF, SK, HM, XW, JMR, WAW, BJE, GNH, DT, BLE declare no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
This study adhered to ethical guidelines at MD Anderson Cancer Center and the IRB study protocol (LAB05-0530).
Rights and permissions
About this article
Cite this article
Reyes, M.E., Fujii, T., Branstetter, D. et al. Poor prognosis of patients with triple-negative breast cancer can be stratified by RANK and RANKL dual expression. Breast Cancer Res Treat 164, 57–67 (2017). https://doi.org/10.1007/s10549-017-4233-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-017-4233-5