Abstract
Purpose
Obesity and oversupply of glucose, e.g., due to nutritional factors may shape the tumor microenvironment favorable for tumor progression. O-GlcNAcylation, a reversible modification of intracellular proteins, influences on several cellular functions and is connected to many diseases including cancer. Glycosaminoglycan hyaluronan (HA) enhances tumor progression and in breast cancer HA accumulation associates strongly with poor outcome. In vitro studies have suggested that O-GlcNAcylation may enhance HA synthesis. The aim of this study was to investigate the correlations between O-GlcNAcylation, HA-related parameters, and disease outcome in a clinical breast cancer material consisting of 278 breast cancer cases.
Methods
In microscopic analyses, O-GlcNAc staining of the breast carcinoma cells was evaluated in several randomly picked high-power fields of each section. The extent of cytoplasmic O-GlcNAc staining was graded as either low or high according to the intensity of the staining and the percentage of stained cells. The extent of nuclear O-GlcNAc staining was categorized as either low or high according to the percentage of stained nuclei.
Results
A high extent of both cytoplasmic and nuclear O-GlcNAcylation correlated with an increased relapse rate, development of distant metastases, and poor outcome. A high extent of cytoplasmic O-GlcNAcylation correlated also with the accumulation of all hyaluronan synthase (HAS1-3) proteins and with a large amount of HA in the tumor stroma. In addition, a high extent of nuclear O-GlcNAcylation associated with obesity.
Conclusions
The results suggest a mechanistic association between increased O-GlcNAcylation and HA synthesis, leading to a HA-rich microenvironment favorable for breast cancer progression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It has become evident that the changes in glucose metabolism occurring in cancer cells have an important role in tumor development and progression. Cancer cells take up glucose at a higher rate than normal cells, a property utilized in 18F-fluorodeoxyglucose-positron emission tomography (FDG-PET) for the diagnostics of various tumor types [1]. In addition, even in the presence of oxygen, cancer cells use the energy of glucose from glycolysis, instead of the tricarboxylic acid cycle, a phenomenon called aerobic glycolysis or the Warburg effect [2]. While aerobic glycolysis is an inefficient way to produce energy, it confers an advantage by accumulating many of the building blocks needed for cell proliferation [3].
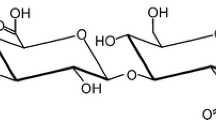
The high glucose uptake and accumulation of glycolysis intermediates in cancer cells also increase the metabolic flux through the hexosamine biosynthetic pathway (HBP). The end product of HBP is uridine diphosphate N-acetylglucosamine (UDP-GlcNAc), a sugar nucleotide used by various glycosyl transferases for the construction of different glycoconjugates like glycoproteins, glycosaminoglycans, and glycolipids [4]. The activation of HBP leads to the accumulation of UDP-GlcNAc particularly in the cytosol, while the uptake of nucleotide sugars in Golgi apparatus is strictly regulated by transporters [5]. Therefore, fluctuations in UDP-GlcNAc supply have the strongest impacts on glycosylations taking place in the cytosol, the most important of these processes being O-GlcNAcylation and hyaluronan (HA) synthesis.
HA is a glycosaminoglycan produced at the plasma membrane by hyaluronan synthases (HAS1-3) which utilize cytosolic UDP-GlcNAc and uridine diphosphate glucuronic acid (UDP-GlcUA) as substrates [6, 7]. HA is an important component of the pericellular and extracellular matrix, participating in many cellular processes like proliferation, survival, migration, and inflammation [8]. HA accumulation enhances tumor progression in several ways [9]. In breast cancer, increased amount of HA and HASs associate with poor prognosis, HER2-positivity, and obesity of the patients [10, 11].
O-GlcNAcylation is the reversible addition of a single N-acetylglucosamine to serine or threonine residues in certain cytosolic, nuclear, and mitochondrial proteins [12, 13]. This dynamic protein modification is controlled by two enzymes, O-GlcNAc transferase (OGT) that adds the O-GlcNAc residue using UDP-GlcNAc as its substrate [14, 15] and O-GlcNAcase (OGA, MGEA5) which removes it [16, 17]. O-GlcNAcylation influences a variety of cellular functions [18, 19] and aberrant O-GlcNAcylation has been connected to many diseases including metabolic diseases and cancer [19–21].
Previous studies have shown that in breast cancer, O-GlcNAcylation and OGT expression are increased in comparison to normal breast tissue [22–24], whereas OGA expression is decreased [23]. In vitro experiments have shown that increased O-GlcNAcylation due to OGA inhibition induces an invasion of breast cancer cells [22], whereas decreased O-GlcNAcylation as a consequence of OGT silencing inhibits tumor cell growth and invasion [22, 25]. In mice, decreased O-GlcNAcylation mediated by OGT silencing reduced the development of lung metastases [22]. In human breast cancer, there is some evidence that higher levels of O-GlcNAcylation and OGT expression may correlate with higher histological grade of the tumor [23, 24]. Also, it has been shown that O-GlcNAcylation is increased in lymph node metastases as compared to primary breast cancer tissue [22], a finding in line with a correlation found between down-regulated OGA expression and lymph node metastases [23]. On the contrary, one study has shown that reduction of OGT expression and O-GlcNAcylation correlate with lymph node metastases in breast cancer [26].
O-GlcNAcylation has been shown to exert profound effects on many cellular functions considered as hallmarks of cancer [4], and interestingly, it also influences HA synthesis. In cultured vascular smooth muscle cells, O-GlcNAcylation was shown to increase HAS2 stability [27]. Likewise, in a melanoma cell line, O-GlcNAcylation of HAS3 prevented its lysosomal degradation, increasing its transport to plasma membrane and elevating enzymatic activity [28]. Taken together, these in vitro experiments suggest that increased O-GlcNAcylation may contribute to the increased HA levels found in breast cancer.
Previous studies have indicated that O-GlcNAcylation may enhance breast cancer progression and HA synthesis, but to our knowledge there are no studies showing whether there is a connection between general O-GlcNAcylation and patient outcome, nor an association between O-GlcNAcylation and HA accumulation in human breast cancer. The aim of this study was to evaluate the extent of O-GlcNAcylation in 278 human breast cancer cases and to investigate the correlations between O-GlcNAcylation, HA-related parameters, clinicopathological characteristics, and outcome of the patients.
Materials and methods
Patient material
The patient material of this study includes 278 primary breast cancer cases operated at Kuopio University Hospital during 2002–2008. As reported previously [10], at first all HER2-positive operated cases (n = 163) were collected retrospectively. Cases with inadequate tissue blocks at the time of diagnosis (n = 24) were excluded, resulting in a total of 139 HER2-positive cases. Then 139 HER2-negative cases were selected by matching for patient’s age and time of operation. HER2 status was the only clinicopathological characteristic available at the time of patient selection. Other clinicopathological data, e.g., tumor size, nodal status, hormone receptor status, and adjuvant treatments, were collected during the year 2010 from the patient records of Kuopio University Hospital. The follow-up data were updated on October 8, 2014. Ethical approval for this study was provided by the Ethics Committee of the University of Eastern Finland (February 24, 2009, 19//2009), and by the National Supervisory Authority for Welfare and Health (VALVIRA, April 8, 2009, 1928/05.01.00.06/2009). The reporting of this study is in accordance with the REMARK criteria [29].
Immunohistochemistry and in situ hybridization
Immunohistochemical staining for O-GlcNAc was performed using 5-µm formalin-fixed, paraffin-embedded sections of surgical tumor specimens. The sections were heated at 58 °C for 30 min, dewaxed, and rehydrated. The deparaffinized sections were subjected to antigen retrieval by incubation in 0.1 mM citrate buffer, pH 6.0, for 10 min in a pressure cooker at 120 °C. Endogenous peroxidase was blocked with a 5-min treatment in 1 % hydrogen peroxide. After washing with H2O for 2 × 3 min and with 0.1 M phosphate buffer, pH 7.4 (PB) for 2 × 5 min, the sections were incubated in 3 % bovine serum albumin (BSA) in PB for 30 min at 37 °C to block unspecific staining. Mouse monoclonal antibody HGAC85 (1:200; Abcam, Cambridge, UK) was used to detect O-GlcNAc. Incubation with the primary antibody was performed at 4 °C overnight, followed by washing with PB for 3 × 10 min. Then, the sections were incubated for 1 h with a biotinylated antimouse secondary antibody (1:300; Vector Laboratories, Irvine, CA, USA), washed with PB for 3 × 10 min and stained with the avidin–biotin peroxidase method (1:200; Vectastain ABC kit, Vector Laboratories). After washing with PB for 3 × 10 min, the signal was visualized using the chromogen 3,3′-diaminobenzidine (Sigma-Aldrich, St Louis, MO, USA). Nuclei were stained with Mayer’s hematoxylin, followed by dehydration, clearance, and mounting. Sections with primary antibody replaced by Control Ascites Fluid from murine myeloma (1:2500, Sigma-Aldrich, St Louis, MO, USA) were used as negative controls.
The histopathological evaluation of the standard parameters was performed at the time of diagnosis in Kuopio University Hospital, Department of Pathology, using surgical tumor specimens and core needle biopsy samples. HER2 expression was determined by the chromogenic in situ hybridization test (Zymed 84-0146, San Francisco, CA, USA), and considered as positive when six or more gene copies were found. Immunohistochemistry was used to assess estrogen (ER) and progesterone (PR) receptor status; the limit for hormone receptor positivity was 10 %.
The staining for HA and HAS1-3, and their evaluation have been described previously [10, 11]. For this study, HA expression in breast carcinoma cells was graded as either weak (0–50 %) or strong (51–100 %) according to the percentage of HA-positive breast carcinoma cells, and the intensity of stromal HA staining was graded as weak (including the original groups weak and moderate) or strong (including the original groups intense and very intense). The expressions of HAS1-3 were categorized as weak (0–25 %), moderate (26–75 %), or strong (76–100 %) according to the percentage of HAS1-3 positive breast carcinoma cells, and as weak (0–25 %) or strong (26–100 %) according to the percentage of HAS1-3 positive stromal cells.
Microscopic evaluation of O-GlcNAc immunostaining
In each section, several randomly picked high-power fields (×40 magnification) in the invasive area were evaluated in order to determine the extent of O-GlcNAc staining. A total of 24 sections had to be excluded since there was not enough invasive component left in the tumor tissue, resulting in a total of 254 evaluated sections. Since OGT is expressed in splice variants with partly different subcellular distributions and therefore different target proteins [30], we scored the O-GlcNAc staining of cytoplasm and nucleus separately. The intensity of O-GlcNAc staining in the cytoplasm was graded as weak, moderate, or strong. The percentage of stained cells was scored as negative (0–5 %), low (6–25 %), moderate (26–50 %), or high (51–100 %). In the subsequent evaluations, the extent of cytoplasmic O-GlcNAc staining was graded as either low or high by combining the data of intensity and the percentage of stained cells as follows: weak intensity 1 point, moderate intensity 2 points, strong intensity 3 points, and the percentage of stained cells 0–5 % 0 points, 6–25 % 1 point, 26–50 % 2 points, and 51–100 % 3 points. The final scores were calculated by adding up the intensity score to the percentage score. The resulting total scores 1–3 represented low extent of cytoplasmic O-GlcNAc staining and scores 4–6 represented high extent of cytoplasmic O-GlcNAc staining.
Nuclear staining was considered as positive when the staining in the nucleus was strong. The extent of nuclear O-GlcNAc staining was graded as either low (0–50 %) or high (51–100 %) according to the percentage of stained nuclei. The microscopic assessment was performed by three investigators (KH, ST, PA). The investigators had no information on the patient’s clinicopathological data at the time of the evaluation.
Statistical analyses
The data were analyzed using IBM SPSS Statistics 22 for Windows (IBM Corporation, Armonk, NY, USA). The correlations between the extent of O-GlcNAc staining, clinicopathological characteristics, and HA-related parameters were calculated with the Chi-Square test. Kaplan–Meier survival curves were plotted for disease-free survival and for overall survival. Univariate and multivariate survival analyses were performed with the Cox’s model. P value < 0.05 was regarded statistically significant.
Results
Among the 254 cases, the median age of the patients was 58.5 years (range 32–86 years) at the time of diagnosis. Clinicopathological data of the cases are presented in Table 1. The adjuvant treatments were carried out according to treatment guidelines, and the majority of the patients received some form of adjuvant treatment; 190 (75 %) were treated with chemotherapy, 155 (61 %) with hormonal treatment, and 229 (90 %) with radiotherapy. In all, 59 (45 %) of the HER2-positive patients received adjuvant trastuzumab. The median follow-up time was 7.91 years (range 0.53–13.22 years). During the follow-up, 62 (24 %) patients died, 70 (28 %) patients suffered a relapse, and 63 (25 %) patients developed distant metastases.
O-GlcNAc immunostaining
O-GlcNAc immunostaining was detected both in the cytoplasm and nucleus of breast carcinoma cells (Fig. 1). Very faint O-GlcNAc staining was observed in the stromal cells (Fig. 1) which were not analyzed further. The intensity of cytoplasmic staining in breast carcinoma cells was weak in 69 (27 %) sections, moderate in 137 (54 %) sections, and strong in 48 (19 %) sections. Cytoplasmic O-GlcNAc staining was found in all of the samples and in the majority of the cases (n = 211, 83 %) over half of the breast carcinoma cells exhibited some O-GlcNAc staining. In subsequent analyses, the cytoplasmic O-GlcNAc staining was graded as either low or high by combining the data of intensity and the percentage of stained cells as described in “Materials and methods” section, resulting in 33 (13 %) cases included in the group with low extent of cytoplasmic O-GlcNAcylation, while the majority of cases (221 = 87 %) displayed a high extent of O-GlcNAcylation. A strong correlation was found between the intensity of cytoplasmic staining and the percentage of stained cells (p < 0.001). Nuclear staining was less frequent; only 27 (11 %) sections exhibited over 50 % of stained nuclei. The extent of nuclear O-GlcNAc staining correlated with the extent of cytoplasmic staining (p = 0.034).
Breast carcinoma sections stained with an O-GlcNAc antibody. Panel a shows an overview of a section with a high extent of cytoplasmic O-GlcNAc staining and panel b provides an example of nuclear O-GlcNAc staining. In panel c an overview of a section with both cytoplasmic and nuclear O-GlcNAc staining is shown. Panel d displays an example of a section with a low extent of cytoplasmic and nuclear O-GlcNAc staining
High extent of O-GlcNAcylation correlates with an increased relapse rate and distant metastases
During the follow-up, 30 % (n = 67) of the patients with a high extent of cytoplasmic O-GlcNAcylation suffered a relapse, compared to only 9 % (n = 3) of the patients with a low extent of cytoplasmic O-GlcNAcylation (p = 0.011) (Table 2). There was also a strong correlation between a high extent of nuclear O-GlcNAcylation and increased relapse rate, i.e., 48 % (n = 13) of the patients with high and only 25 % (n = 57) of the patients with a low extent of nuclear O-GlcNAcylation had a relapse (p = 0.011) (Table 2). A high extent of both cytoplasmic and nuclear O-GlcNAcylation also correlated with the development of distant metastases (p = 0.008 and p = 0.012, respectively) (Table 2). No correlation was found between the extent of O-GlcNAcylation and standard prognostic factors like tumor size, nodal status, HER2 status, ER status, PR status, or histological grade (data not shown).
High extent of O-GlcNAcylation correlates with poor outcome
As the follow-up ended, only 70 % (n = 154) of the patients with a high extent of cytoplasmic O-GlcNAcylation were disease free in comparison to 91 % (n = 30) of the patients with a low extent of cytoplasmic O-GlcNAcylation (p = 0.021, HR 3.901, 95 % CI 1.225–12.419) (Fig. 2a). Similarly, 52 % (n = 14) of the patients with high and 75 % (n = 170) of the patients with a low extent of nuclear O-GlcNAcylation were disease free (p = 0.006, HR 2.352, 95 % CI 1.274–4.340) (Fig. 2b).
Kaplan–Meier curves representing disease-free survival (DFS) and overall survival (OS) according to the extent of O-GlcNAc staining. Panels a and b present DFS according to the extent of cytoplasmic (a) and nuclear (b) O-GlcNAcylation, and in panels c and d OS according to the extent of cytoplasmic (c) and nuclear (d) O-GlcNAcylation are shown. Low cytoplasmic/nuclear O-GlcNAcylation representing a low extent of O-GlcNAcylation in the cytoplasm or in the nuclei, and high cytoplasmic/nuclear O-GlcNAcylation representing a high extent of O-GlcNAcylation in the cytoplasm or in the nuclei. DFS disease-free survival, OS overall survival
At the end of the follow-up, 74 % (n = 163) of the patients with high and 88 % (n = 29) of the patients with a low extent of cytoplasmic O-GlcNAcylation were alive, suggesting lower survival among patients with high extent of cytoplasmic O-GlcNAcylation but this difference did not reach statistical significance (p = 0.07, HR 2.553, 95 % CI 0.926–7.040) (Fig. 2c). A high extent of nuclear O-GlcNAcylation correlated with short overall survival of the patients, since as the follow-up ended, 63 % (n = 17) of the patients with high and 77 % (n = 175) of the patients with a low extent of nuclear O-GlcNAcylation were alive (p = 0.038, HR 2.053, 95 % CI 1.041–4.048) (Fig. 2d).
The Cox multivariate analyses for overall survival were performed separately for the extents of cytoplasmic and nuclear O-GlcNAcylation. The other variables included in the analyses were tumor size, nodal status, ER status, PR status, HER2 status, and histological grade. In both multivariate analyses, the significant prognostic factors for overall survival were nodal status (p < 0.001,) and tumor size (p ≤ 0.019).
Cytoplasmic O-GlcNAcylation correlates with the levels of HAS1-3 proteins and stromal HA
Studies on cultured cells have indicated that O-GlcNAcylation of HAS2 and 3 proteins blocks their degradation and increases the synthesis of HA [27, 28]. The present findings in breast cancer patients are in line with those in vitro data, since a significant positive correlation was found between the extent of cytoplasmic O-GlcNAcylation and the amount of all three HAS proteins in breast carcinoma cells (p ≤ 0.029) (Table 3). Accordingly, a high extent of cytoplasmic O-GlcNAcylation correlated with a strong intensity of stromal HA staining (p = 0.033) (Table 3). Interestingly, a significant correlation also existed between carcinoma cell O-GlcNAcylation and stromal cell HASs (p ≤ 0.033), but the extent of O-GlcNAcylation in breast carcinoma cells was not correlated with their HA content (Table 3).
High extent of nuclear O-GlcNAcylation correlates with obesity
Obesity increases the risk for breast cancer and also impairs the outcome in an established breast cancer [31–33], while O-GlcNAcylation is considered to be a metabolic sensor. We therefore checked if there was any link between obesity and the extent of O-GlcNAcylation among breast cancer patients. A significant positive correlation between obesity (body mass index ≥30) and the extent of O-GlcNAcylation was indeed found, but it was only present in the premenopausal patients and was confined to the nuclear O-GlcNAcylation (p = 0.025) (Table 4).
Discussion
This study demonstrates for the first time that a high extent of O-GlcNAcylation in the breast cancer cells at the time of breast cancer surgery correlates with an increased relapse rate, distant metastases, and poor outcome during the follow-up. In addition, a high extent of cytoplasmic O-GlcNAcylation correlates with the accumulation of all HAS proteins both in the breast carcinoma cells and in the stromal cells, and with the accumulation of HA in the tumor stroma. Moreover, nuclear O-GlcNAcylation associates with obesity.
There are previous data supporting the present finding that excessive O-GlcNAcylation is associated with an unfavorable prognosis in breast cancer. It has been reported that increased O-GlcNAcylation enhances invasion and migration of breast carcinoma cells in vitro [22], whereas a reduction of O-GlcNAcylation inhibits breast carcinoma cell growth and invasion [22, 25]. In mice, a reduction of O-GlcNAcylation through OGT silencing reduced the development of lung metastases but did not have an impact on the size of the primary tumor [22]. These findings are in agreement with our results showing a significant correlation between a high extent of O-GlcNAcylation, increased relapse rate, and development of distant metastases, as well as with the lack of any correlations between the extent of O-GlcNAcylation and known prognostic factors such as histological grade, hormone receptor status, and lymph node metastases at the time of operation. However, there are also studies pointing to an association between O-GlcNAcylation and lymph node metastases [22, 23] and histological grade of the tumor [23, 24]. Since over 1000 proteins can be O-GlcNAcylated [34], it would be important to determine the entire set of O-GlcNAcylated proteins involved, as in addition to HASs there is most likely a panel of proteins contributing to unfavorable prognosis.
Increased O-GlcNAcylation of HAS2 [27] and HAS3 [28] proteins have been shown to increase their stability and activity in vitro. HAS1 activity is also highly dependent on the supply of UDP-GlcNAc [35], the same substrate that increases O-GlcNAcylation in general. The strong positive correlations between the extent of O-GlcNAcylation and HAS contents that we found suggest that the increase in the amounts of HAS proteins is due to their stabilization by O-GlcNAcylation. The correlation occurred especially with the cytoplasmic O-GlcNAcylation, which fits well with the cytoplasmic location of the HAS targets. Since high levels of HAS1-3 and HA are strong indicators of poor prognosis in breast cancer [10, 11], the present findings suggest that the unfavorable outcome related to the high extent of O-GlcNAcylation is at least in part due to HAS activation and HA accumulation which enhances tumor progression. We hypothesize that the Warburg effect causing increased glucose uptake results in an enlarged pool of UDP-GlcNAc in tumor cells and contributes to the accumulation of HA via increased O-GlcNAcylation.
Interestingly, breast carcinoma cell O-GlcNAcylation also correlated with the HAS contents within the stromal cells, raising the question of whether the Warburg effect takes place also in the surrounding stromal cells. However, no sign of increased O-GlcNAcylation was found in the stromal cells. On the other hand, cancer cells are known to control the phenotype of the stromal cells in multiple ways, including induction of genetic defects [36] and shedding of microvesicles targeted at the stromal cells [37]. The latter possibility is particularly attractive since elevated O-GlcNAcylation can enhance melanoma cell secretion of HAS-enriched microvesicles [28]. Further analyses will be needed to clarify whether metabolic features corresponding to aerobic glycolysis are a part of these control mechanisms.
Obesity and type 2 diabetes, which is usually associated with obesity, increase breast cancer risk and also impair the outcome of breast cancer patients [31–33, 38]. The connection between obesity and increased breast cancer risk, as well as the effect of obesity on prognosis, has been established especially among postmenopausal women. More recently, it has been revealed that obesity also impairs the outcome of premenopausal breast cancer patients [32, 33]. Obesity correlates with high levels of HA and HASs in breast cancer [10, 11]. In the present study, we showed that high extent O-GlcNAcylation correlates with stromal HA accumulation and with high levels of HASs and also with obesity among premenopausal breast cancer patients. The present results together with the previous data suggest that an oversupply of glucose due to nutritional factors does not only provide building blocks for rapid cell proliferation but also induces O-GlcNAcylation and HA synthesis leading to a microenvironment suitable for cancer progression.
In summary, this study reveals that a high extent of O-GlcNAcylation in the primary tumor correlates with the development of distant metastases and poor outcome in human breast cancer, apparently conferring on cancer cells a survival advantage and allowing them to metastasize. O-GlcNAcylation seems to activate the HAS enzymes and HA synthesis, leading to a HA-rich microenvironment favorable for breast cancer progression.
Abbreviations
- FDG-PET:
-
18F-fluorodeoxyglucose-positron emission tomography
- HBP:
-
Hexosamine biosynthetic pathway
- UDP-GlcNAc:
-
Uridine diphosphate N-acetylglucosamine
- HA:
-
Hyaluronan
- HAS:
-
Hyaluronan synthase
- UDP-GlcUA:
-
Uridine diphosphate glucuronic acid
- HER2:
-
Human epidermal growth factor receptor 2
- OGT:
-
O-GlcNAc transferase
- OGA, MGEA5:
-
O-GlcNAcase
- PB:
-
Phosphate buffer
- BSA:
-
Bovine serum albumin
- ER:
-
Estrogen receptor
- PR:
-
Progesterone receptor
- BMI:
-
Body mass index
- DFS:
-
Disease-free survival
- OS:
-
Overall survival
References
Gambhir SS (2002) Molecular imaging of cancer with positron emission tomography. Nat Rev Cancer 2:683–693
Warburg O (1956) On the origin of cancer cells. Science 123:309–314
Vander Heiden MG, Cantley LC, Thompson CB (2009) Understanding the Warburg effect: the metabolic requirements of cell proliferation. Science 324:1029–1033
Ma Z, Vosseller K (2013) O-GlcNAc in cancer biology. Amino Acids 45:719–733
Vigetti D, Viola M, Karousou E et al (2014) Metabolic control of hyaluronan synthases. Matrix Biol 35:8–13
Tammi RH, Passi AG, Rilla K et al (2011) Transcriptional and post-translational regulation of hyaluronan synthesis. FEBS J 278:1419–1428
Weigel PH, DeAngelis PL (2007) Hyaluronan synthases: a decade-plus of novel glycosyltransferases. J Biol Chem 282:36777–36781
Sironen RK, Tammi M, Tammi R et al (2011) Hyaluronan in human malignancies. Exp Cell Res 317:383–391
Toole BP (2004) Hyaluronan: from extracellular glue to pericellular cue. Nat Rev Cancer 4:528–539
Auvinen P, Tammi R, Kosma VM et al (2013) Increased hyaluronan content and stromal cell CD44 associate with HER2 positivity and poor prognosis in human breast cancer. Int J Cancer 132:531–539
Auvinen P, Rilla K, Tumelius R et al (2014) Hyaluronan synthases (HAS1-3) in stromal and malignant cells correlate with breast cancer grade and predict patient survival. Breast Cancer Res Treat 143:277–286
Torres CR, Hart GW (1984) Topography and polypeptide distribution of terminal N-acetylglucosamine residues on the surfaces of intact lymphocytes. Evidence for O-linked GlcNAc. J Biol Chem 259:3308–3317
Fardini Y, Dehennaut V, Lefebvre T et al (2013) O-GlcNAcylation: a new cancer hallmark? Front Endocrinol (Lausanne) 4:99
Haltiwanger RS, Holt GD, Hart GW (1990) Enzymatic addition of O-GlcNAc to nuclear and cytoplasmic proteins. Identification of a uridine diphospho-N-acetylglucosamine: peptide beta-N-acetylglucosaminyltransferase. J Biol Chem 265:2563–2568
Haltiwanger RS, Blomberg MA, Hart GW (1992) Glycosylation of nuclear and cytoplasmic proteins. Purification and characterization of a uridine diphospho-N-acetylglucosamine: polypeptide beta-N-acetylglucosaminyltransferase. J Biol Chem 267:9005–9013
Dong DL, Hart GW (1994) Purification and characterization of an O-GlcNAc selective N-acetyl-beta-d-glucosaminidase from rat spleen cytosol. J Biol Chem 269:19321–19330
Gao Y, Wells L, Comer FI et al (2001) Dynamic O-glycosylation of nuclear and cytosolic proteins: cloning and characterization of a neutral, cytosolic beta-N-acetylglucosaminidase from human brain. J Biol Chem 276:9838–9845
Zachara NE, Hart GW (2004) O-GlcNAc a sensor of cellular state: the role of nucleocytoplasmic glycosylation in modulating cellular function in response to nutrition and stress. Biochim Biophys Acta 1673:13–28
Hart GW, Slawson C, Ramirez-Correa G et al (2011) Cross talk between O-GlcNAcylation and phosphorylation: roles in signaling, transcription, and chronic disease. Annu Rev Biochem 80:825–858
Hart GW, Housley MP, Slawson C (2007) Cycling of O-linked beta-N-acetylglucosamine on nucleocytoplasmic proteins. Nature 446:1017–1022
Slawson C, Hart GW (2011) O-GlcNAc signalling: implications for cancer cell biology. Nat Rev Cancer 11:678–684
Gu Y, Mi W, Ge Y et al (2010) GlcNAcylation plays an essential role in breast cancer metastasis. Cancer Res 70:6344–6351
Krzeslak A, Forma E, Bernaciak M et al (2012) Gene expression of O-GlcNAc cycling enzymes in human breast cancers. Clin Exp Med 12:61–65
Champattanachai V, Netsirisawan P, Chaiyawat P et al (2013) Proteomic analysis and abrogated expression of O-GlcNAcylated proteins associated with primary breast cancer. Proteomics 13:2088–2099
Caldwell SA, Jackson SR, Shahriari KS et al (2010) Nutrient sensor O-GlcNAc transferase regulates breast cancer tumorigenesis through targeting of the oncogenic transcription factor FoxM1. Oncogene 29:2831–2842
Jiang K, Gao Y, Hou W et al (2016) Proteomic analysis of O-GlcNAcylated proteins in invasive ductal breast carcinomas with and without lymph node metastasis. Amino Acids 48:365–374
Vigetti D, Deleonibus S, Moretto P et al (2012) Role of UDP-N-acetylglucosamine (GlcNAc) and O-GlcNAcylation of hyaluronan synthase 2 in the control of chondroitin sulfate and hyaluronan synthesis. J Biol Chem 287:35544–35555
Deen AJ, Arasu UT, Pasonen-Seppanen S et al (2016) UDP-sugar substrates of HAS3 regulate its O-GlcNAcylation, intracellular traffic, extracellular shedding and correlate with melanoma progression. Cell Mol Life Sci 73(16):3183–3204
McShane LM, Altman DG, Sauerbrei W et al (2006) REporting recommendations for tumor MARKer prognostic studies (REMARK). Breast Cancer Res Treat 100:229–235
Janetzko J, Walker S (2014) The making of a sweet modification: structure and function of O-GlcNAc transferase. J Biol Chem 289:34424–34432
van den Brandt PA, Spiegelman D, Yaun SS et al (2000) Pooled analysis of prospective cohort studies on height, weight, and breast cancer risk. Am J Epidemiol 152:514–527
Protani M, Coory M, Martin JH (2010) Effect of obesity on survival of women with breast cancer: systematic review and meta-analysis. Breast Cancer Res Treat 123:627–635
Chan DS, Vieira AR, Aune D et al (2014) Body mass index and survival in women with breast cancer-systematic literature review and meta-analysis of 82 follow-up studies. Ann Oncol 25:1901–1914
Ostrowski A, van Aalten DM (2013) Chemical tools to probe cellular O-GlcNAc signalling. Biochem J 456:1–12
Rilla K, Oikari S, Jokela TA et al (2013) Hyaluronan synthase 1 (HAS1) requires higher cellular UDP-GlcNAc concentration than HAS2 and HAS3. J Biol Chem 288:5973–5983
Tuhkanen H, Anttila M, Kosma VM et al (2004) Genetic alterations in the peritumoral stromal cells of malignant and borderline epithelial ovarian tumors as indicated by allelic imbalance on chromosome 3p. Int J Cancer 109:247–252
Green TM, Alpaugh ML, Barsky SH et al (2015) Breast cancer-derived extracellular vesicles: characterization and contribution to the metastatic phenotype. Biomed Res Int 2015:634865
Coughlin SS, Calle EE, Teras LR et al (2004) Diabetes mellitus as a predictor of cancer mortality in a large cohort of US adults. Am J Epidemiol 159:1160–1167
Acknowledgments
We thank Kari Kotikumpu and Eija Rahunen (Institute of Biomedicine, Anatomy, University of Eastern Finland, Finland) for technical help with O-GlcNAc immunostaining, Tuomas Selander (Science Service Center, Kuopio University Hospital, Finland) for assistance with the statistical analyses, and Ewen MacDonald for English language editing.
Funding
This study was supported by the Special Government Funding (EVO/VTR) of Kuopio University Hospital (Grant Nos. 5654132 and 5053101) and a Grant from Cancer Society of North Savo. The funders were not involved in the collection, management, or analysis of the data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Ethical approval for this study was provided by the Ethics Committee of the University of Eastern Finland and by the National Supervisory Authority for Welfare and Health. The execution of this study complies with the current laws of Finland.
Rights and permissions
About this article
Cite this article
Tiainen, S., Oikari, S., Tammi, M. et al. High extent of O-GlcNAcylation in breast cancer cells correlates with the levels of HAS enzymes, accumulation of hyaluronan, and poor outcome. Breast Cancer Res Treat 160, 237–247 (2016). https://doi.org/10.1007/s10549-016-3996-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-016-3996-4