Abstract
Male breast cancer (MBC) is rare and poorly understood. Like female breast cancer (FBC), MBCs are highly sensitive to hormonal changes, and hyperestrogenism, specifically, represents a major risk factor for MBC. MBC is considered similar to late-onset, post-menopausal estrogen/progesteron receptors positive FBC (ER+/PR+). Sulfotransferase 1A1 (SULT1A1) is an enzyme involved in the metabolism of estrogens. Recently, SULT1A1 common functional polymorphism Arg213His (638G>A) variant has been found to be associated with increased breast cancer (BC) risk, particularly in post-menopausal women. For this reason, we decided to explore whether SULT1A1 Arg213His could exert an effect on MBC development. The primary aim of this study was to evaluate the influence of the SULT1A1 Arg213His polymorphism on MBC risk. The secondary aim was to investigate possible associations with relevant clinical–pathologic features of MBC. A total of 394 MBC cases and 786 healthy male controls were genotyped for SULT1A1 Arg213His polymorphism by PCR–RFLP and high-resolution melting analysis. All MBC cases were characterized for relevant clinical–pathologic features. A significant difference in the distribution of SULT1A1 Arg213His genotypes was found between MBC cases and controls (P < 0.0001). The analysis of genotype-specific risk showed a significant increased MBC risk in individuals with G/A (OR 1.97, 95 % CI 1.50–2.59; P < 0.0001) and A/A (OR 3.09, 95 % CI 1.83–5.23; P < 0.0001) genotypes in comparison to wild-type genotype, under co-dominant model. A significant association between SULT1A1 risk genotypes and HER2 status emerged. Results indicate that SULT1A1 Arg213His may act as a low-penetrance risk allele for developing MBC and could be associated with a specific tumor subtype associated with HER2 overexpression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Male breast cancer (MBC) is a rare disease, representing less than 1 % of all breast cancers (BCs), with incidence rates of approximately 1 per 100,000 men per year [1]. MBC incidence trends are variable, with a minority of countries presenting evidence for an increase. Although outcomes for MBC have improved over time [2], morbidity and mortality in MBC patients are a serious concern.
MBC is likely to be caused by the concurrent effects of various risk factors: hormonal, environmental, and genetic. Like female breast cancer (FBC), MBC appears to be highly sensitive to hormonal changes. MBC is recognized as being primarily a hormone-dependent malignancy [3] and is widely accepted as an estrogen-driven disease specifically related to hyperestrogenism. An increased level of circulating estradiol appears to be an important factor in the etiology of the disease, and the mean total serum estradiol level is significantly increased in MBC patients compared with healthy males [4].
Family history of BC and personal history of cancer are also frequently observed in MBC patients [2], thus pointing to a relevant genetic component in MBC predisposition. Studies to date indicate mutations in the two major high-penetrance BC genes, BRCA1 and, mainly, BRCA2, as having the most impact on MBC susceptibility, though only a small proportion (about 10 %) of MBCs is accounted for by mutations of these genes [5]. Thus, much of the genetic contribution to MBC risk remains to be elucidated. Current data based on age-frequency distribution, age-specific incidence rate patterns, and prognostic factors profiles suggest that MBC is similar to late-onset, post-menopausal estrogen/progesteron receptors positive (ER+/PR+) FBC. However, compared to FBC, MBC occurs later in life, with higher stage, lower grade, and more ER+/PR+ [2, 3].
Sulfotransferase 1A1 (SULT1A1) is one of the members of sulfotransferase (SULT) superfamily, considered to be the predominant type of SULTs because of its extensive tissue distribution and abundance [6]. Within the context, SULT1A1 catalyzes the sulfonation of estrogens to form biologically inactive estrogen sulfates, thus reducing the level of estrogens’ exposure in target tissues, such as mammary tissue. The SULT1A1 Arg213His variant (rs9282861), is a very common functional polymorphism of the SULT1A1 gene [7] and many studies have associated it with BC in women, though with contrasting results [8–13] Recent meta-analysis studies have shown that SULT1A1 Arg213His variant is associated with increased risk of BC, particularly in post-menopausal women [14–18]. SULT1A1 Arg213His variant (rs9282861) consists of a G to A transition at nucleotide 638 and causes an Arginine (Arg) to Histidine (His) substitution at aminoacid 213. Based on crystal structural modeling, it has been proposed that Arg213His aminoacid substitution causes structural alteration in the SULT1A1 protein that affects the binding capacity to substrate [7]. A reduction of enzyme activity was demonstrated for individuals with homozygous 213His allele variant, compared to those with Arg/Arg and Arg/His genotypes, and positive associations with high estrogens blood levels were found to be more pronounced among women carrying the His allele [12].
Given the role of SULT1A1 in the metabolism of estrogens, the relevant role of estrogens in the pathogenesis of MBC, and the suggested similarity of MBC to post-menopausal BC, in which SULT1A1 Arg213His polymorphism has been recently associated with increased risk, we hypothesized that SULT1A1 Arg213His polymorphism might exert some effect on MBC risk. Therefore, the primary aim of our study was to evaluate the influence of the Arg213His polymorphism on MBC risk, in a series of Italian cases and controls. A secondary aim was the investigation of possible associations with relevant clinical–pathologic features of MBC. To our knowledge, this is the first report investigating the association between SULT1A1 polymorphism and MBC risk.
Materials and methods
Study population and data collection
The study was performed comparing a series of 394 MBC patients and 786 healthy male controls residing throughout Italy. Specifically, MBC cases and controls were recruited from ten Italian research hospitals geographically distributed throughout the country, all participating in the ongoing Italian Multicentre Study on MBC [19, 20]. The mean age at BC diagnosis was 61.5 years (SD 11.8) in MBC cases, and the mean age was 53.3 (SD 10.5) in the controls.
Information collected for each MBC case included: age at diagnosis, family and personal history of cancer, recurrence of disease, BRCA1/2 mutational status, tumor histological type, grade, nodal status, ER, PR, MIB1, and HER2 expression.
Control samples were obtained from individuals enrolled under research or clinical protocols and from blood donors. Inclusion criteria: men with BC diagnosis, for MBC cases; and healthy males with residency within the same area as MBC cases, for control samples. All individuals in the control sample were Caucasian, but this was by chance (i.e., not a selection criterion). All participants signed an informed consent for the use of their biological samples for research purposes.
Procedures to maintain confidentiality for all the information collected were developed and strictly adhered to. The study was approved by Local Ethical Committee (“Sapienza” University of Rome, Prot. 264/12).
SNP genotyping
Buffy coat aliquots from MBC cases and controls were anonymously shipped to the research laboratory (Department of Molecular Medicine, Rome) where genomic DNA was extracted using QIAmp DNA Mini Kit (Qiagen Inc., Charlesworth, CA). SULT1A1 Arg213His (G>A) polymorphism was analyzed by PCR–RFLP using the restriction enzyme HaeII (New England BioLabs, Ipswich MA) and by high-resolution melting (HRM) analysis performed with the 7,500 Fast Real-Time PCR (Applied Biosystems, Warrington, UK). Information on primers sequences is available on request. Samples from three individuals carrying the three SULT1A1 Arg213His genotypes, respectively, were used as controls. In order to assess genotyping concordance, 20 % of samples were analyzed by both screening methods and validated by direct sequencing.
Statistical analysis
Genotype frequencies were calculated as the number of participants, with a particular genotype divided by the number of total participants. Tests for Hardy–Weinberg equilibrium among cases and controls were assessed using Pearson’s Chi square test, with one degree of freedom, comparing expected genotype frequencies (based on observed qs) to observed genotype frequencies. Case–control differences on genotype frequencies were also assessed using Pearson’s Chi square test.
The association between MBC risk and SULT1A1 Arg213His (G>A) polymorphism was measured by the odds ratio (OR) and its corresponding 95 % confidence interval, by unconditional logistic regression, adjusted for age and center of enrollment. The analyses were performed with three separate logistic regression models based on dominant, recessive, and co-dominant effects (inheritance model). In the dominant model, the heterozygous variant and rare homozygous variant were combined in a dummy variable. In the recessive model, the variant was defined in a dummy variable as only the rare homozygous genotype. In the co-dominant model, both rare homozygous and heterozygous variant effects were estimated using two dummy variables.
Chi square test and logistic regression models were also performed in a case–case analysis, in order to evaluate the potential associations between SULT1A1 Arg213His genotypes and specific MBC clinical–pathologic characteristics.
A P value < 0.05 was considered statistically significant. All the analyses were performed using SAS (SAS/STAT version 9.1) statistical program.
Results
All 1,180 samples, including 394 MBC cases and 786 male controls were genotyped for SULT1A1 Arg213His (G>A) polymorphism. Genotype distribution was consistent with Hardy–Weinberg equilibrium (P > 0.05) among controls.
The distribution of genotype frequencies of the SULT1A1 Arg213His polymorphism in MBC cases and controls, and the risk estimate, calculated by separate multivariate regression analyses, based on different transmission models (co-dominant, dominant, and recessive) are summarized in Table 1. Significant differences emerged in the distribution of genotypes between MBC cases and controls (P < 0.0001). The analysis of the genotype-specific risks by co-dominant model showed that individuals with A/A homozygous genotype (OR 3.09, 95 % CI 1.83–5.23; P < 0.0001) and individuals with G/A heterozygous genotype (OR 1.97, 95 % CI 1.50–2.59; P < 0.0001) were at increased MBC risk. These results were confirmed by dominant and recessive models (Table 1).
The associations of A/A and G/A genotypes with increased MBC risk persisted also, when 52 MBC carriers of germ-line BRCA1/2 mutations were excluded from the analyses (Table 2).
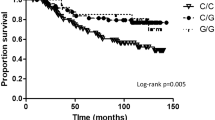
Statistically significant association between SULT1A1 risk genotypes and HER2 status emerged. No other significant associations were found (Table 3). In a case–case multivariate analysis adjusted for center of enrollment and age of patients, a statistically significant association between SULT1A1 A/A risk genotype and HER2-positive tumors emerged (OR 4.70; 95 % CI 1.50–14.71; P = 0.008).
Discussion
The primary aim of our study was to evaluate the possible influence of SULT1A1 Arg213His functional polymorphism on MBC risk by genotyping 394 MBC cases and 786 healthy male controls. Genotype frequencies of SULT1A1 Arg213His polymorphism were different between MBC cases and healthy male controls. The analyses of the genotype and allele-specific risks showed that in our series, males carrying the 213His allele were at increased risk of MBC. At present, there are no published data on the role of SULT1A1 Arg213His polymorphism in MBC; thus, our data are the first to demonstrate a possible association between a SULT1A1 common functional polymorphism and BC susceptibility in men.
From an epidemiological point of view, MBC resembles post-menopausal ER-positive FBC with which it shares some major risk factors such as high estrogen levels [2, 3]. Association between the SULT1A1 Arg213His variant and BC risk has been investigated in women, but with inconclusive results [8–13]. The contrasting data in the literature concerning SULT1A1 Arg213His variant and FBC risk may reflect the heterogeneity of BC in women as well as the confounding factors related to the high disease frequency and high variability of hormone history found in women. Within this context, we propose that increased knowledge of the underlying mechanisms of MBC, unencumbered by these confounding factors, might be instrumental to a better understanding of the complex interrelationship between genetic, hormonal, and environmental factors involved in the pathogenesis of BC in both genders.
Recently, SULT1A1 Arg213His variant has been associated with increased risk of post-menopausal BC [17, 18]. Though more studies need to be conducted on this particular subgroup, our data seem to support these conclusions. Thus, results from our study may point to a common pathogenic mechanism involving alteration in the estrogen metabolic pathways that are present in both males and females.
Our results suggest that the role of SULT1A1 Arg213His as a genetic risk factor for MBC may be related to its function in estrogens metabolism. Men carrying the SULT1A1 213His allele may be more susceptible to estrogen-induced carcinogenesis in mammary tissue due to the presence of high levels of bioactive estrogens. A high level of bioactive estrogens may provide a growth advantage for ER-positive tumors. Consistently, a high proportion of MBCs expresses hormone receptors. However, it cannot be excluded that the association between SULT1A1 genotypes and BC risk could be even more complicated, considering the dual effect of SULT1A1 on both inactivation of estrogens and activation of environmental mammary carcinogens.
It is known that SULT1A1 participates in the elimination of 4-hydroxy-tamoxifen (4-OH-TAM), which is one of the major active metabolites of tamoxifen (TAM), and that functional genetic polymorphisms of SULT1A1 may modify the pharmacokinetics of TAM therapy potentially influencing the activity of TAM [21]. TAM is generally considered the standard adjuvant treatment for hormone-dependent MBC [22]. Interestingly, several findings suggest that the possible reduction of SULT1A1 enzymatic activity could contribute to a minor elimination of estrogens on one hand, and an accumulation of active metabolites of TAM on the other [21, 23–25]. This paradoxical effect could increase estrogens’ exposure through a competitive mechanism. In this context, MBC patients with SULT1A1 His213His genotype may benefit from hormone therapy that is different from TAM, such as aromatase inhibitors. However, prospective studies are needed to elucidate this speculation.
In this study, we also evaluated a possible association between SULT1A1 Arg213His genotypes and clinical–pathologic characteristics of MBCs. Results were statistically significant for an over-represented SULT1A1 213His genotype in HER2-positive cases. Recently, we have shown that BRCA2-associated MBCs represent a subgroup of tumors with a peculiar phenotype characterized by HER2-positive status and aggressive behavior [19] and that SULT1A1 gene deletion is significantly associated with BRCA2-related tumors [26]. Taken together, all these findings may suggest that the possible reduction of SULT1A1 enzymatic activity, due to either the presence of 213His allele or of SULT1A1 gene deletion, may contribute to an aggressive phenotype in MBC. This is consistent with the higher prevalence of lymph node metastases, which has been found in FBC patients with the SULT1A1 Arg213His polymorphism [10], again suggesting a possible common pathogenic mechanism in BC of both genders.
Although we studied a large sample size, a potential limitation of our study is that it is based on a series collected in a single country. Given the ethnic differences in the impact of SULT1A1 Arg213His polymorphism reported in BC risks among women from different populations [13, 14, 16, 17], further studies are needed to better define the role of SULT1A1 Arg213His polymorphism in MBC risk in additional populations.
In conclusion, our results indicate that SULT1A1 Arg213His variant could represent a low-penetrance risk factor for developing BC in men. Our study is the first to explore and demonstrate a possible association between this genetic polymorphism and MBC risk. Although further studies are needed to confirm these data, the national scope of our research may provide useful information for identifying males at increased risk of BC in Italy, and may serve to encourage additional MBC-related research nationally and internationally.
References
Ly D, Forman D, Ferlay J, Brinton LA, Cook MB (2013) An international comparison of male and female breast cancer incidence rates. Int J Cancer 132(8):1918–1926
Korde LA, Zujewski JA, Kamin L, Giordano S, Domchek S, Anderson WF, Bartlett JM, Gelmon K, Nahleh Z, Bergh J, Cutuli B, Pruneri G, McCaskill-Stevens W, Gralow J, Hortobagyi G, Cardoso F (2010) Multidisciplinary meeting on male breast cancer: summary and research recommendations. J Clin Oncol 28:2114–2122
Brinton LA, Cook MB, McCormack V, Johnson KC, Olsson H, Casagrande JT, Cooke R, Falk RT, Gapstur SM, Gaudet MM, Gaziano JM, Gkiokas G, Guénel P, Henderson BE, Hollenbeck A, Hsing AW, Kolonel LN, Isaacs C, Lubin JH, Michels KB, Negri E, Parisi D, Petridou ET, Pike MC, Riboli E, Sesso HD, Snyder K, Swerdlow AJ, European Rare Cancer Study Group, Trichopoulos D, Ursin G, van Den Brandt PA, Van Den Eeden SK, Weiderpass E, Willett WC, Ewertz M, Thomas DB (2014) Anthropometric and hormonal risk factors for male breast cancer: male breast cancer pooling project results. J Natl Cancer Inst 106(3):djt465. doi:10.1093/jnci/djt465
Nirmul D, Pegoraro RJ, Jialal I, Naidoo C, Joubert SM (1983) The sex hormone profile of male patients with breast cancer. Br J Cancer 48(3):423–427
Rizzolo P, Silvestri V, Tommasi S, Pinto R, Danza K, Falchetti M, Gulino M, Frati P, Ottini, Ottini L (2013) Male breast cancer: genetics, epigenetics, and ethical aspects. Ann Oncol 24(Suppl 8):viii75–viii82
Hempel N, Gamage N, Martin JL, McManus ME (2007) Human cytosolic sulfotransferase SULT1A1. Int J Biochem Cell Biol 39(4):685–689
Nagar S, Walther S, Blanchard RL (2006) Sulfotransferase (SULT) 1A1 polymorphic variants *1, *2, and *3 are associated with altered enzymatic activity, cellular phenotype, and protein degradation. Mol Pharmacol 69(6):2084–2092
Zheng W, Xie D, Cerhan JR, Sellers TA, Wen W, Folsom AR (2001) Sulfotransferase 1A1 polymorphism, endogenous estrogen exposure, well-done meat intake, and breast cancer risk. Cancer Epidemiol Biomark Prev 10:89–94
Tang D, Rundle A, Mooney L, Cho S, Schnabel F, Estabrook A, Kelly A, Levine R, Hibshoosh H, Perera F (2003) Sulfotransferase 1A1 (SULT1A1) polymorphisms PAH-DNA adduct levels in breast tissue and breast cancer risk in a case–control study. Breast Cancer Res Treat 78(2):217–222
Langsenlehner U, Krippl P, Renner W, Yazdani-Biuki B, Eder T, Wolf G, Wascher TC, Paulweber B, Weitzer W, Samonigg H (2004) Genetic variants of the sulfotransferase 1A1 and breast cancer risk. Breast Cancer Res Treat 87:19–22
Han DF, Zhou X, Hu MB, Wang CH, Xie W, Tan XD, Zheng F, Liu F (2004) Sulfotransferase 1A1 (SULT1A1) polymorphism and breast cancer risk in Chinese women. Toxicol Lett 150(2):167–177
Yang G, Gao YT, Cai QY, Shu XO, Cheng JR, Zheng W (2005) Modifying effects of sulfotransferase 1A1 gene polymorphism on the association of breast cancer risk with body mass index or endogenous steroid hormones. Breast Cancer Res Treat 94(1):63–70
Xiao J, Zheng Y, Zhou Y, Zhang P, Wang J, Shen F, Fan L, Kolluri VK, Wang W, Yan X, Wang M (2014) Sulfotransferase SULT1A1 Arg213His polymorphism with cancer risk: a meta-analysis of 53 case–control studies. PLoS One 9(9):e106774
Kotnis A, Kannan S, Sarin R, Mulherkar R (2008) Case–control study and meta-analysis of SULT1A1 Arg213His polymorphism for gene, ethnicity and environment interaction for cancer risk. Br J Cancer 99(8):1340–1347
Sun Y, Zang Z, Xu X, Zhang Z, Zhong L, Zan W, Zhao Y, Sun L (2010) The association of SULT1A1 codon 213 polymorphism and breast cancer susceptibility: meta-analysis from 16 studies involving 23,445 subjects. Breast Cancer Res Treat 125(1):215–219
Wang Z, Fu Y, Tang C, Lu S, Chu WM (2010) SULT1A1 R213H polymorphism and breast cancer risk: a meta-analysis based on 8,454 cases and 11,800 controls. Breast Cancer Res Treat 122(1):193–198
Jiang Y, Zhou L, Yan T, Shen Z, Shao Z, Lu J (2010) Association of sulfotransferase SULT1A1 with breast cancer risk: a meta-analysis of case–control studies with subgroups of ethnic and menopausal statue. J Exp Clin Cancer Res 29:101
Lee H, Wang Q, Yang F, Tao P, Li H, Huang Y, Li JY (2012) SULT1A1 Arg213His polymorphism, smoked meat, and breast cancer risk: a case–control study and meta-analysis. DNA Cell Biol 31(5):688–699
Ottini L, Silvestri V, Rizzolo P, Falchetti M, Zanna I, Saieva C, Masala G, Bianchi S, Manoukian S, Barile M, Peterlongo P, Varesco L, Tommasi S, Russo A, Giannini G, Cortesi L, Viel A, Montagna M, Radice P, Palli D (2012) Clinical and pathologic characteristics of BRCA-positive and BRCA-negative male breast cancer patients: results from a collaborative multicentre study in Italy. Breast Cancer Res Treat 134(1):411–418
Ottini L, Silvestri V, Saieva C, Rizzolo P, Zanna I, Falchetti M, Masala G, Navazio AS, Graziano V, Bianchi S, Manoukian S, Barile M, Peterlongo P, D’Amico C, Varesco L, Tommasi S, Russo A, Giannini G, Cortesi L, Viel A, Montagna M, Radice P, Palli D (2013) Association of low-penetrance alleles with male breast cancer risk and clinicopathological characteristics: results from a multicenter study in Italy. Breast Cancer Res Treat 138(3):861–868
Grabinski JL, Smith LS, Chisholm GB, Drengler R, Rodriguez GI, Lang AS, Kalter SP, Garner AM, Fichtel LM, Hollsten J, Pollock BH, Kuhn JG (2006) Genotypic and allelic frequencies of SULT1A1 polymorphisms in women receiving adjuvant tamoxifen therapy. Breast Cancer Res Treat 95(1):13–16
Bradley KL, Tyldesley S, Speers CH, Woods R, Villa D (2014) Contemporary systemic therapy for male breast cancer. Clin Breast Cancer 14(1):31–39
Nowell S, Sweeney C, Winters M, Stone A, Lang NP, Hutchins LF, Kadlubar FF, Ambrosone CB (2002) Association between sulfotransferase 1A1 genotype and survival of breast cancer patients receiving tamoxifen therapy. J Natl Cancer Inst 94(21):1635–1640
Jin Y, Desta Z, Stearns V, Ward B, Ho H, Lee KH, Skaar T, Storniolo AM, Li L, Araba A, Blanchard R, Nguyen A (2005) CYP2D6 genotype, antidepressant use, and tamoxifen metabolism during adjuvant breast cancer treatment. J Natl Cancer Inst 97(1):30–39
Wegman P, Elingarami S, Carstensen J, Stål O, Nordenskjöld B, Wingren S (2007) Genetic variants of CYP3A5, CYP2D6, SULT1A1, UGT2B15 and tamoxifen response in postmenopausal patients with breast cancer. Breast Cancer Res 9(1):R7
Palli D, Rizzolo P, Zanna I, Silvestri V, Saieva C, Falchetti M, Navazio AS, Graziano V, Masala G, Bianchi S, Russo A, Tommasi S, Ottini L (2013) SULT1A1 gene deletion in BRCA2-associated male breast cancer: a link between genes and environmental exposures? J Cell Mol Med 17(5):605–607
Acknowledgments
The authors wish to thank Lesley Pritikin for her assistance with preparation of the manuscript.
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
This work was supported by AIRC (Associazione Italiana Ricerca Cancro, Grant No. IG12780) to L.O., FIRC (Fondazione Italiana Ricerca Cancro triennial fellowship “Mario e Valeria Rindi”) to V.S., and ITT (Istituto Tumori Toscano, triennial Grant 2010, Grant No. 6204) to D.P.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ottini, L., Rizzolo, P., Zanna, I. et al. Association of SULT1A1 Arg213His polymorphism with male breast cancer risk: results from a multicenter study in Italy. Breast Cancer Res Treat 148, 623–628 (2014). https://doi.org/10.1007/s10549-014-3193-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-014-3193-2