Abstract
This study investigated local and global changes in the motor network using longitudinal resting-state functional magnetic resonance imaging (rs-fMRI). Motor impairment was measured in 81 stroke patients using Fugl-Meyer assessment on the same day as rs-fMRI acquisition at both 2 weeks and 3 months post-stroke. The relationships between network measures and motor function scores were assessed. With regard to local connectivity, interhemispheric connectivity was noticeably altered at each time point. Interhemispheric connectivity was also related to residual motor function and improvement in motor function. The anterior intraparietal sulcus and other well-known primary and secondary motor-related regions played important roles in motor function. Changes in global connectivity according to stroke type and initial severity were investigated. In global connectivity, interhemispheric connectivity was disrupted at 2 weeks post-stroke regardless of stroke type and initial severity. During the recovery period, interhemispheric connectivity recovered well in patients with hemorrhagic stroke or low severity. In contrast, there were no significant between-group and within-group alterations in intrahemispheric connectivity. Intrahemispheric connectivity of the inferior frontal cortex (IFC) exhibited opposite alterations compared to other connections. There were no differences between groups in IFC connectivity alterations; however, decreasing ipsilesional IFC connectivity and contralesional IFC during recovery were noticeable in patients with mild to moderate impairments and patients with severe impairments, respectively. These results may be helpful in understanding the network changes that occur after stroke and could have important implications for treatment strategy development in future studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Numerous brain functions are associated with specific brain regions, but are also generated by interactions among multiple brain regions. When brain structure is damaged by focal neurological disease, this damage can also influence the function of distant brain regions (Carter et al. 2010; Chen et al. 2015; He et al. 2007a). The physiological influences of neurological disorders are better assessed over an entire network rather than at the local site of damage (Carter et al. 2010; He et al. 2007a; Honey and Sporns 2008). In recent neurologic research, a connectivity-based approach has been widely used to emphasize the fundamental role of distributed neural networks, and to investigate changes in network structure and relationships between network measures and motor functions (Buma et al. 2010; Carter et al. 2010; He et al. 2007b; Rehme and Grefkes 2013; Wang et al. 2010; Westlake et al. 2012). There have been many findings regarding local and global connectivity analysis in previous studies. The most consistent finding was the significant change in interhemispheric connectivity between motor-related regions, with the strength of the connectivity associated with residual motor function. In contrast to interhemispheric connectivity, the role of intrahemispheric connectivity remains controversial, especially with regard to whether contralesional changes are beneficial or non-beneficial for motor recovery (Buetefisch 2015; Dodd et al. 2017; Rehme et al. 2010). Previous connectivity studies used regions of interest (ROIs) obtained from predefined brain structural atlases or a few functional studies. As a result, the ROIs used varied in each connectivity study. Previous studies also had small sample sizes with a heterogeneous patient population with different stroke types and initial severity. Therefore we extracted the motor network using multiple ROIs that showed consistent activation during upper limb movements by stroke patients from 36 neuroimaging studies (Rehme et al. 2012) and investigated alteration and role of local and global connectivity in the network using a substantial amount of longitudinal resting-state fMRI data (81 stroke patients at 2 weeks and 3 months after stroke onset). Investigation of global changes was also performed through stratified analysis according to stroke type and initial severity of patients and the role of connectivity of several ROIs such as the anterior intraparietal sulcus (aIPS) and the inferior frontal cortex (IFC), which has not been established in previous stroke studies, was investigated in the study.
Materials and Methods
Participants
We recruited 81 patients (41 males and 40 females, age 56.40 ± 12.38 years) according to the following inclusion and exclusion criteria (Table 1). We included patients diagnosed with first-onset unilateral stroke (ischemic or hemorrhagic stroke) whose onset was within 2 weeks or less, and who were 19 years or older at stroke onset. Patients were excluded if they exhibited any clinically significant or unstable medical disorders, any neuropsychiatric comorbidity other than stroke, or any contraindication to magnetic resonance imaging (MRI). All patients underwent resting-state functional MRI (fMRI) scans twice. An age-matched control group of 55 healthy subjects (21 males and 34 females, age 54.40 ± 13.73 years) without a history of psychiatric or neurological problems underwent resting-state fMRI scan once. This study was conducted in accordance with the principles of the Declaration of Helsinki. Ethical approval was obtained from the Institutional Review Board of Samsung Medical Center. All participants understood the experimental procedures and signed a consent form.
Experimental Design
This experiment was designed as a longitudinal observational study of repeated fMRI experiments. The participants underwent resting-state fMRI and behavioral assessment at 2 weeks and 3 months after stroke onset. Motor impairments were measured using Fugl-Meyer assessment scores (Fugl-Meyer et al. 1974) on the same day as fMRI data acquisition.
Data Acquisition
All patients participated in the first fMRI session approximately 2 weeks after stroke onset (14.46 ± 6.28 days) and the second session about 3 months (95.69 ± 11.07 days) after onset. Participants were instructed to keep their eyes closed and to remain motionless during the resting-state fMRI scan. fMRI data were acquired using a Philips ACHIEVA® MR scanner (Philips Medical Systems, Best, The Netherlands) operating at 3 T. During each session, 100 whole-brain images were collected using a T2*-weighted gradient echo-planar imaging (EPI) sequence with the following metrics: 35 axial slices, slice thickness = 4 mm, no gap, matrix size = 128 × 128, repetition time = 3000 ms, echo time = 35 ms, flip angle = 90°, and field of view = 220 × 220 mm. T1-weighted MP-RAGE images were also acquired with the following settings: 124 axial slices, slice thickness = 1.6 mm, no gap, matrix size = 512 × 512, and field of view = 240 × 240 for atlas transformation.
Data Pre-processing
Image pre-processing was performed using the SPM8 package (Welcome Trust Centre for Neuroimaging, University College London, London, U.K.). Pre-processing consisted of several steps: slice timing correction, correction for head motion by realigning all consecutive volumes to the first fMRI image using six rigid-body transformation, coregistration of a mean image of the realigned fMRI images and a T1-weighted structural image, spatial normalization into Montreal Neurological Institute (MNI) template space (resampling to a 2-mm isotropic voxel size), and spatial smoothing using a 6-mm full-width half-maximum Gaussian Kernel.
Several nuisance sources were removed using the linear regression of nine nuisance parameters. The parameters were obtained from head motion correction (spatial realignment) and global, white matter, and ventricle signals. Band-pass filtering between 0.009 and 0.08 Hz was performed to remove constant offsets and linear trends. Nuisance regression and band-pass filtering were processed using MATLAB (Mathworks, Inc.).
fMRI Data Analysis
A network consists of a set of nodes and edges between pairs of nodes. In our study, ROIs were obtained from Rehme et al. (2012), who performed meta-analyses on 54 experimental contrasts for movement of the paretic upper limb (472 patients, 452 activation foci) and on 20 experiments comparing activation between patients and healthy controls (177 patients, 113 activation foci) from 36 neuroimaging studies of stroke patients among PubMed search results published up to January 2011. We used “affected upper limb movement vs. rest in stroke patients” results in this study. Regions in these results were not symmetric. To obtain network measurements under the same conditions in bilateral hemispheres, we added the contralesional inferior frontal gyrus (IFG), the inferior frontal sulcus (IFS), the rostral cingulate zone (RCZ), and the ipsilesional aIPS, and constructed a symmetrical network. The 24 ROIs were defined as 10-mm-diameter spheres around the predefined MNI coordinates (Table 2, Supplementary Fig. 1). The lesion area was masked and connections of the motor network were calculated using Pearson’s correlation between the mean time courses of each of the 24 ROIs. The correlation coefficient indicates the strength of connectivity in the study. A one-sample t test (p < 0.01) was conducted to identify significant connections.
To investigate indirect influences on the motor network by stroke onset, motor networks of healthy controls and stroke patients were compared 2 weeks post-stroke. Two-sample t tests were conducted to identify significant differences in motor networks between healthy subjects and stroke patients at 2 weeks post-stroke, and paired t tests were performed to identify significant changes in motor networks of stroke patients between 2 weeks and 3 months after onset (during the recovery period). Relationships between network measures and residual motor functions, and between initial connectivity and improvement in motor function during the recovery period were examined using a linear regression model.
A seed-based approach was used to investigate unobserved connections among specific regions in the whole brain because the motor network constructed using 24 predefined ROIs restricted the number of regions that could be analyzed. The correlation coefficients were calculated between the time course of a specific region and the time course of every voxel in the brain. The correlation coefficient was converted to Gaussian distributed values through Fisher z-transformation defined by \(z=\left( {1/2} \right)\ln \left( {1+r} \right)/ln(1 - r)\).
To examine unobserved connections of the aIPS related to residual motor function in the whole brain (beyond predefined ROIs), voxel-wise connectivity maps (z-statistic maps) of the aIPS for all patients were obtained using a seed-based approach, and relationships between z-values in a voxel for all patients and their residual motor functions was investigated using a linear regression model.
Global changes in interhemispheric and intrahemispheric connectivity in the motor network and changes in intrahemispheric connectivity between the IFC (IFS and IFG) and motor-related regions were investigated. To compare global changes in the motor network according to stroke type (‘Ischemic’ or ‘Hemorrhagic’) and initial severity (‘Mild & Moderate’ or ‘Severe’), two-way repeated-measures analysis of variance (repeated-measures ANOVA) was used. With regard to initial severity, patients were classified into two groups (initial FMA ≤ 55, ‘Severe’; initial FMA > 55, ‘Mild & Moderate’) based on criteria obtained from a severity classification study according to FMA scores (Duncan et al. 1994).
Results
Altered Local Connectivity in the Motor Network
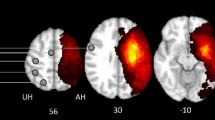
Alterations in connectivity were investigated between healthy controls and stroke patients 2 weeks post-stroke and local changes in connectivity between at 2 weeks and 3 months post-stroke (Fig. 1, Supplementary Tables 1, 2). Most altered connections were weakened 2 weeks post-stroke compared to healthy controls and strengthened for 3 months after the onset. Interhemispheric connections comprised mostly altered connections. In contrast, several intrahemispheric connections of the IFS and IFG were strengthened at 2 weeks post-stroke compared to healthy controls and weakened during the recovery period, the opposite pattern of other connections.
Differences in connectivity between healthy controls and stroke patients at 2 weeks post-stroke (a) and changes in connectivity between 2 weeks and 3 months post-stroke (b). This figure was drawn using BrainNet Viewer software (http://nitrc.org/projects/bnv/). The red edge represents an increase in the strength of the connection, and the blue edge represents a decrease in the strength of the connection (p < 0.05). IL ipsilesional side, CL contralesional side
Functional Connectivity Related to Motor Function
The relationships between network measures and FMA scores were investigated to search for implications related to motor impairments. Table 3 shows significant correlations between connection strength and FMA score. The results show positive correlations: 13 of 15 connections were interhemispheric. Connections among bilateral M1, S1, and premotor areas showed a significant relationship with residual motor function. Connections between these regions composed the majority of connections related to motor function.
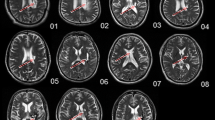
In this study, the aIPS also played a significant role. The interhemispheric connections between the bilateral aIPS and M1 or S1 were correlated with residual function. The bilateral aIPS was additionally analyzed using a seed-based approach to investigate unobserved connections related to residual motor function. The aIPS was mostly connected with the parietal and occipital lobes, and around the central sulcus. Figure 2 is the t-map (uncorrected p < 0.001) constructed by analyzing the correlation between the results from our seed-based approach and motor function scores. Only interhemispheric connections connected with M1 and S1 (ipsilesional aIPS-contralesional M1, peak MNI coordinates [30, − 12, 52], t = 4.46; contralesional aIPS-ipsilesional M1, peak MNI coordinates [− 34, − 10, 54], t = 5.35; contralesional aIPS-ipsilesional S1, peak MNI coordinates [− 40, − 22, 52], t = 5.35) were observed. We verified that the interhemispheric connections between the bilateral aIPS and the primary sensorimotor regions played an important role in motor function.
The regions connected with a the contralesional aIPS and b the ipsilesional aIPS are related to motor function. The regions indicate significant connections correlated with residual motor function among all connections of the aIPS in the whole brain. The t-maps (p < 0.001) are axial views (MNI coordinate, z = 52). Interhemispheric connections between primary sensorimotor regions and the aIPS were correlated with residual motor function. IL ipsilesional side, CL contralesional side
Baseline network measures associated with motor functional recovery were also investigated. The relationship between initial local connection strength and change in motor function score during the recovery period was examined (Table 4). Several connections between the M1, S1, pre-SMA, S2, and aIPS were correlated with improvement of motor function scores. The majority of the connections were composed of interhemispheric connections.
Altered Global Connectivity in the Motor Network
Alterations in the average strength of interhemispheric and intrahemispheric connectivity were investigated using stratified analysis according to stroke type and initial severity (Fig. 3; Table 5). Overall and homotopic interhemispheric connectivity at 2 weeks post-stroke was significantly disrupted compared to healthy controls regardless of stroke type and initial severity. However, ipsilesional and contralesional intrahemispheric connectivity did not show any significant differences compared to healthy controls. During the recovery period, changes in interhemispheric connectivity were more distinct than those in intrahemispheric connectivity. Global connectivity showed different alterations according to stroke type and initial severity. There were significant differences of alterations in overall and homotopic interhemispheric connectivity according to stroke type (type × time; overall, F = 4.34, p = 0.0404; homotopic, F = 8.59, p = 0.0044). Interhemispheric connectivity was significantly increased in the Hemorrhagic group (overall, t = − 3.56, p = 0.0018; homotopic, t = − 3.57, p = 0.0018) compared to the Ischemic group. There was no difference between groups according to severity. However, overall interhemispheric connectivity was significantly increased in the Mild and Moderate group (t = − 3.25, p = 0.0036). In contrast to interhemispheric connectivity, ipsilesional and contralesional intrahemispheric connectivity did not exhibit significant differences between groups or within groups. However, contralesional connectivity had a tendency to increase in the Mild & Moderate group and to decrease in the Severe group although differences in contralesional connectivity changes were not significant according to severity (severity × time, F = 2.99, p = 0.0876).
Altered interhemispheric and intrahemispheric connectivity in the motor network. a The strength of overall interhemispheric connectivity. b The strength of interhemispheric connectivity between homotopic regions. c The strength of ipsilesional intrahemispheric connectivity. d The strength of contralesional intrahemispheric connectivity. Error bars represent standard deviation (*p < 0.05; **p < 0.01; ***p < 0.001)
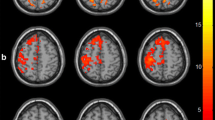
Most connections were weakened at 2 weeks post-stroke compared to healthy controls and strengthened during the recovery period. However, the IFS and IFG connections showed an opposite tendency (Fig. 1, Supplementary Tables 1, 2). The alterations in intrahemispheric connectivity between IFC regions and remaining motor-related regions in the motor network (IFC intrahemispheric connectivity) were investigated (Fig. 4; Table 6). IFC intrahemispheric connectivity was generally strengthened at 2 weeks post-stroke compared to healthy controls and weakened during the recovery period. There were no group differences according to stroke type or initial severity. However, ipsilesional IFC connectivity was significantly decreased during the recovery period in the Hemorrhagic group (t = 2.36, p = 0.0279) and decreases in the connectivity of the Hemorrhagic and Mid & Moderate groups were noticeable. Contralesional IFC connectivity was significantly decreased in the Severe group (t = 2.05, p = 0.0448). Decreased contralesional IFC connectivity in the Hemorrhagic and Severe groups was also noticeable compared to other groups.
Discussion
Changes in the motor networks of stroke patients were investigated by observing local and global measures. Interhemispheric connectivity significantly decreased at 2 weeks post-stroke compared to that of healthy controls, and then increased during the recovery period. Disruptions of interhemispheric interactions are related to an imbalance between bilateral hemispheres after stroke onset and interhemispheric interactions are increased by the rebalancing of bilateral hemispheric networks during the recovery period. Interhemispheric connectivity were also correlated with residual motor function and improvement in motor function during the recovery period. Interhemispheric connectivity was mainly composed of primary and secondary motor-related regions. This implies that more interactive conditions for motor-related brain activity between both hemispheres indicate better motor function and recovery. Interhemispheric connectivity in stroke patients is an important indicator established in previous studies (Carter et al. 2010; Park et al. 2011; Rehme and Grefkes 2013; Wang et al. 2010). This study confirmed the importance of interhemispheric connectivity through analysis of a considerable amount of data.
The majority of connections related to motor function were interhemispheric connections including M1, S1, premotor areas and aIPS. Several connections with M1, S1, and premotor areas were found to play important roles in previous stroke studies (Carter et al. 2010; Park et al. 2011; Wang et al. 2010). However, the connections in the aIPS were not primarily investigated in other stroke studies. In healthy subject studies, the aIPS contributed to hand grip function (Davare et al. 2011; Ehrsson et al. 2001). The aIPS also provides motor-related regions with visual information about objects, as well as influencing grasp-related and muscle-specific M1-premotor cortex interactions (Davare et al. 2009; Olivier et al. 2007; Reichenbach et al. 2010; Tunik et al. 2005). Recently, connections between M1 and the aIPS have been described in humans (Koch et al. 2010), and the proportional fractional anisotropy values of the ipsilesional and contralesional tracts between the premotor cortex and the aIPS have been shown to contribute to motor function using structural connectivity data in chronic stroke patients (Schulz et al. 2015). In our functional connectivity study, the bilateral aIPS also played an important role; interhemispheric connections between the aIPS and primary sensorimotor areas contributed to motor function in stroke patients.
Changes in the several intrahemispheric connections of the IFC in both hemispheres contrasted with those of other connections in the study. Compared to healthy controls, intrahemispheric connections in the IFC were strengthened at 2 weeks post-stroke and weakened during the recovery period. In a meta-analysis (Rehme et al. 2012), the IFC was activated during upper limb movements by stroke patients. Interestingly, this region was activated during affected and unaffected upper limb movements by stroke patients, but was not activated during movement by healthy subjects in the meta-analysis. Such inverse alterations in IFC connectivity may be related to disruption and recovery of network segregation. In this sense, disruption and recovery of interhemispheric connectivity in the motor network can be also related to disruption and recovery of interhemispheric integration. Functional networks of healthy subjects exhibit segregation and integration properties (Bullmore and Sporns 2012; Sporns 2013; Tononi et al. 1994). However, the properties are disrupted by stroke onset (Deco et al. 2015; Gratton et al. 2012). The IFC is a part of the ventral attention system and is included in the attention network (Bledowski et al. 2004; Corbetta et al. 2008; Corbetta and Shulman 2002; Linden et al. 1999). Because of the blurry within-hemisphere boundaries between the attention and motor networks related to disruption of network segregation, the intrahemispheric connections between the IFC and motor-related regions can be abnormally increased compared to healthy controls. After the recovery period, these connections can be somewhat decreased. Recently, an increase of ipsilesional connectivity between the default mode network and the dorsal attention network caused by disruption of network segregation was reported in subacute stroke patients compared to healthy controls (Siegel et al. 2016). The IFC region can be co-activated during movements in stroke patients because of abnormally strong connectivity with motor-related regions related to disruption of network segregation.
In functional terms, enrollment of the IFC during movement in stroke patients can also be considered to be related to their attention. This region is an important part of the ventral attention system, which is associated with response to detection of a behaviorally relevant target (Bledowski et al. 2004; Corbetta et al. 2008; Corbetta and Shulman 2002; Linden et al. 1999). Patients have difficulty moving their limbs due to motor impairments caused by stroke and must pay much more attention during movements in comparison with healthy subjects. Therefore, connections between the IFC and motor-related regions may become stronger in the subacute stage due to co-activation between the IFC and motor-related regions. Compared to the subacute stage, less attention is required during chronic stage because motor impairment is typically reduced and due to patient adaptation. As a result, these connections between the IFC and motor-related regions may weaken.
Alterations in global connectivity were investigated according to stroke type and initial severity. Changes in interhemispheric connectivity were prominently observed compared to intrahemispheric connectivity. This result was consistently reported in previous studies (Carey et al. 2013; Rehme and Grefkes 2013; Siegel et al. 2016). These changes in global connectivity differed slightly according to stroke type and initial severity in our study. Disruptions of interhemispheric connectivity caused by stroke onset were observed regardless of stroke type and initial severity. However, recovery of connectivity over the course of 3 months was noticeable in patients with hemorrhagic stroke or low severity. The changes in contralesional connectivity tended to differ according to severity, although there were no significant differences between groups. Connectivity showed a tendency to increase in mild to moderate patients. Alterations of IFC intrahemispheric connectivity also varied according to stroke type and initial severity. Reduced connectivity over 3 months was apparent in patients with hemorrhagic stroke. Ipsilesional intrahemispheric connectivity was decreased in patients with mild to moderate impairments, while a decrease in contralesional intrahemispheric connectivity were noticeable in patients with severe impairments.
Interhemispheric connectivity and IFC intrahemispheric connectivity during the recovery period were markedly altered in the motor network of hemorrhagic stroke patients. In this study, marked alteration of connectivity in hemorrhagic stroke implies better recovery compared to ischemic stroke patients, and this needs to be considered in terms of proportional recovery. Proportional recovery rule means that improvement of motor function in stroke patients during recovery period is approximately 70% of the available improvement in their impairment. In other words, the greater initial functional deficit, the higher potential for recovery. The potential for recovery may be greater in hemorrhagic stroke because of greater disruption of connectivity at the subacute stage compared to ischemic stroke. In previous clinical studies, hemorrhagic stroke typically leads to more severe neurological impairments compared to ischemic stroke during the acute phase and the mortality rate is also higher. However, hemorrhagic stroke survivors have better functional prognoses and more rapid recovery (Paolucci et al. 2003; Perna and Temple 2015; Schepers et al. 2008). Although the brain network is seriously damaged by hemorrhagic stroke onset, network reorganization during the recovery period appears to result in better recovery in survivors.
Interhemispheric connectivity and contralesional intrahemispheric connectivity showed an increasing tendency in patients with mild to moderate impairments. Disruptions of interhemispheric interactions in severely impaired patients were reported and the lower the severity of stroke, the greater the recovery of interhemispheric connectivity during the recovery period in previous studies (Carter et al. 2010; Lee et al. 2017; Park et al. 2011; Rehme and Grefkes 2013; Siegel et al. 2016; van Meer et al. 2012; Wang et al. 2010). Although alterations in the contralesional hemisphere and their role in stroke are still under debate, in one animal study, intraregional signal coherence in the contralesional hemisphere improved more in low severity stroke than in high severity stroke in rats (van Meer et al. 2012).
With regard to IFC intrahemispheric connectivity, decreasing ipsilesional connectivity was noticeable in patients with mild to moderate impairments while changes in contralesional intrahemispheric connectivity were noticeable in patients with severe impairments. In this study, ipsilesional IFC connectivity was increased at 2 weeks post-stroke in patients with mild to moderate impairments compared to healthy controls and greater contralesional IFC connectivity was observed at 2 weeks post-stroke in patients with severe impairments. Differences in IFC intrahemispheric connectivity during the recovery period may be caused by differences in connectivity at the subacute stage. In terms of proportional recovery, the bigger the differences in connectivity between healthy controls and stroke patients at the subacute stage, the higher the potential for alterations during the recovery period. An increase of ipsilesional hemispheric connectivity between the different networks was reported in subacute stroke patients compared to healthy controls in the previous study (Siegel et al. 2016). Participants of the previous study were mainly patients with mild to moderate impairments. In our study, apparent alterations in IFC connectivity were also observed in ipsilesional hemispheric connectivity in patients with mild to moderate impairments. Intracortical activity in the contralesional hemisphere is predominantly enhanced, along with involvement of contralesional motor-related regions, in severely impaired patients (Schaechter et al. 2008; Stinear et al. 2007; Ward et al. 2006). There were noticeable increases in contralesional hemispheric connectivity and the connectivity during the recovery period was significantly decreased in patients with severe impairments in our study.
The alterations in connectivity between predefined ROIs during recovery period were investigated and the correlation analyses between the motor functions and the strengths of the connectivity were performed. Statistical significance was determined by the uncorrected p value because the significance level might be conservative by multiple comparisons between many observed connectivity values obtained from 24 ROIs. However, this should be described as a limitation of our study that multiple comparisons were not performed to control type I errors.
In conclusion, we investigated alterations in interhemispheric and intrahemispheric connectivity and their role in the motor network through local and global analyses. Alterations in global connectivity according to stroke type and initial severity were also investigated. This study may be helpful in understanding the network changes that occur after stroke and may provide insight into neurorehabilitation strategies for stroke patients in terms of therapeutic planning.
References
Bledowski C, Prvulovic D, Goebel R, Zanella FE, Linden DE (2004) Attentional systems in target and distractor processing: a combined ERP and fMRI study. Neuroimage 22:530–540
Buetefisch CM (2015) Role of the contralesional hemisphere in post-stroke recovery of upper extremity motor function. Front Neurol 6:214
Bullmore E, Sporns O (2012) The economy of brain network organization. Nat Rev Neurosci 13:336–349
Buma FE, Lindeman E, Ramsey NF, Kwakkel G (2010) Functional neuroimaging studies of early upper limb recovery after stroke: a systematic review of the literature. Neurorehabilit Neural Repair 24:589–608
Carey LM et al (2013) Beyond the lesion: neuroimaging foundations for post-stroke recovery. Future Neurol 8:507–527
Carter AR et al (2010) Resting interhemispheric functional magnetic resonance imaging connectivity predicts performance after stroke. Ann Neurol 67:365–375. https://doi.org/10.1002/ana.21905
Chen X et al (2015) An ischemic stroke model of nonhuman primates for remote lesion studies: a behavioral and neuroimaging investigation. Restor Neurol Neurosci 33:131–142
Corbetta M, Shulman GL (2002) Control of goal-directed and stimulus-driven attention in the brain. Nat Rev Neurosci 3:201–215
Corbetta M, Patel G, Shulman GL (2008) The reorienting system of the human brain: from environment to theory of mind. Neuron 58:306–324
Davare M, Montague K, Olivier E, Rothwell JC, Lemon RN (2009) Ventral premotor to primary motor cortical interactions during object-driven grasp in humans. Cortex 45:1050–1057
Davare M, Kraskov A, Rothwell JC, Lemon RN (2011) Interactions between areas of the cortical grasping network. Curr Opin Neurobiol 21:565–570
Deco G, Tononi G, Boly M, Kringelbach ML (2015) Rethinking segregation and integration: contributions of whole-brain modelling. Nat Rev Neurosci 16:430–439
Dodd KC, Nair VA, Prabhakaran V (2017) Role of the contralesional vs. Ipsilesional hemisphere in stroke recovery. Front Hum Neurosci 11:469
Duncan PW, Goldstein LB, Horner RD, Landsman PB, Samsa GP, Matchar DB (1994) Similar motor recovery of upper and lower extremities after stroke. Stroke 25:1181–1188
Ehrsson HH, Fagergren A, Forssberg H (2001) Differential fronto-parietal activation depending on force used in a precision grip task: an fMRI study. J Neurophysiol 85:2613–2623
Fugl-Meyer AR, Jääskö L, Leyman I, Olsson S, Steglind S (1974) The post-stroke hemiplegic patient. 1. a method for evaluation of physical performance. Scand J Rehabil Med 7:13–31
Gratton C, Nomura EM, Pérez F, D’Esposito M (2012) Focal brain lesions to critical locations cause widespread disruption of the modular organization of the brain. J Cogn Neurosci 24:1275–1285
He BJ, Shulman GL, Snyder AZ, Corbetta M (2007a) The role of impaired neuronal communication in neurological disorders. Curr Opin Neurol 20:655–660
He BJ, Snyder AZ, Vincent JL, Epstein A, Shulman GL, Corbetta M (2007b) Breakdown of functional connectivity in frontoparietal networks underlies behavioral deficits in spatial neglect. Neuron 53:905–918
Honey CJ, Sporns O (2008) Dynamical consequences of lesions in cortical networks. Hum Brain Mapp 29:802–809. https://doi.org/10.1002/hbm.20579
Koch G et al (2010) In vivo definition of parieto-motor connections involved in planning of grasping movements. Neuroimage 51:300–312
Lee J, Park E, Lee A, Chang WH, Kim DS, Kim YH (2017) Recovery-related indicators of motor network plasticity according to impairment severity after stroke. Eur J Neurol 24:1290–1299. https://doi.org/10.1111/ene.13377
Linden DE, Prvulovic D, Formisano E, Völlinger M, Zanella FE, Goebel R, Dierks T (1999) The functional neuroanatomy of target detection: an fMRI study of visual and auditory oddball tasks. Cereb Cortex 9:815–823
Olivier E, Davare M, Andres M, Fadiga L (2007) Precision grasping in humans: from motor control to cognition. Curr Opin Neurobiol 17:644–648
Paolucci S et al (2003) Functional outcome of ischemic and hemorrhagic stroke patients after inpatient rehabilitation: a matched comparison. Stroke 34:2861–2865
Park C-h, Chang WH, Ohn SH, Kim ST, Bang OY, Pascual-Leone A, Kim Y-H (2011) Longitudinal changes of resting-state functional connectivity during motor recovery after stroke. Stroke 42:1357–1362
Perna R, Temple J (2015) Rehabilitation outcomes: ischemic versus hemorrhagic strokes. Behav Neurol 2015:1–6
Rehme AK, Grefkes C (2013) Cerebral network disorders after stroke: evidence from imaging-based connectivity analyses of active and resting brain states in humans. J Physiol 591:17–31
Rehme AK, Fink GR, von Cramon DY, Grefkes C (2010) The role of the contralesional motor cortex for motor recovery in the early days after stroke assessed with longitudinal FMRI. Cereb Cortex 21:756–768
Rehme AK, Eickhoff SB, Rottschy C, Fink GR, Grefkes C (2012) Activation likelihood estimation meta-analysis of motor-related neural activity after stroke. Neuroimage 59:2771–2782
Reichenbach A, Bresciani J-P, Peer A, Bülthoff HH, Thielscher A (2010) Contributions of the PPC to online control of visually guided reaching movements assessed with fMRI-guided TMS. Cereb Cortex 21:1602–1612
Schaechter JD, Perdue KL, Wang R (2008) Structural damage to the corticospinal tract correlates with bilateral sensorimotor cortex reorganization in stroke patients. Neuroimage 39:1370–1382
Schepers VP, Ketelaar M, Visser-Meily AJ, de Groot V, Twisk JW, Lindeman E (2008) Functional recovery differs between ischaemic and haemorrhagic stroke patients. J Rehabil Med 40:487–489
Schulz R et al (2015) Parietofrontal motor pathways and their association with motor function after stroke. Brain 138:1949–1960
Siegel JS et al (2016) Disruptions of network connectivity predict impairment in multiple behavioral domains after stroke. Proc Natl Acad Sci USA 113:E4367–E4376
Sporns O (2013) Network attributes for segregation and integration in the human brain. Curr Opin Neurobiol 23:162–171
Stinear CM, Barber PA, Smale PR, Coxon JP, Fleming MK, Byblow WD (2007) Functional potential in chronic stroke patients depends on corticospinal tract integrity. Brain 130:170–180
Tononi G, Sporns O, Edelman GM (1994) A measure for brain complexity: relating functional segregation and integration in the nervous system. Proc Natl Acad Sci USA 91:5033–5037
Tunik E, Frey SH, Grafton ST (2005) Virtual lesions of the anterior intraparietal area disrupt goal-dependent on-line adjustments of grasp. Nat Neurosci 8:505–511
van Meer MP et al (2012) Extent of bilateral neuronal network reorganization and functional recovery in relation to stroke severity. J Neurosci 32:4495–4507
Wang L et al (2010) Dynamic functional reorganization of the motor execution network after stroke. Brain 133:1224–1238. https://doi.org/10.1093/brain/awq043
Ward NS et al (2006) Motor system activation after subcortical stroke depends on corticospinal system integrity. Brain 129:809–819
Westlake KP et al (2012) Resting state alpha-band functional connectivity and recovery after stroke. Exp Neurol 237:160–169
Acknowledgements
This study was supported by a National Research Foundation of Korea (NRF) Grant funded by the Korean government (MSIP, NRF-2017R1A2A1A05000730; MSIT, NRF-2017M3A9G5083690; NRF-2017R1D1A1B03034109).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that this research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Handling Editor: Christoph M. Michel.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lee, J., Park, E., Lee, A. et al. Alteration and Role of Interhemispheric and Intrahemispheric Connectivity in Motor Network After Stroke. Brain Topogr 31, 708–719 (2018). https://doi.org/10.1007/s10548-018-0644-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10548-018-0644-9