Abstract
Electromagnetic source localization in electroencephalography (EEG) and magnetoencephalography (MEG) allows finding the generators of transient interictal epileptiform discharges (‘interictal spikes’). In intracerebral EEG (iEEG), oscillatory activity (above 30 Hz) has also been shown to be a marker of neuronal dysfunction. Still, the difference between networks involved in transient and oscillatory activities remains largely unknown. Our goal was thus to extract and compare the networks involved in interictal oscillations and spikes, and to compare the non-invasive results to those obtained directly within the brain. In five patients with both MEG and iEEG recordings, we computed correlation graphs across regions, for (1) interictal spikes and (2) epileptic oscillations around 30 Hz. We show that the corresponding networks can involve a widespread set of regions (average of 10 per patient), with only partial overlap (38 % of the total number of regions in MEG, 50 % in iEEG). The non-invasive results were concordant with intracerebral recordings (79 % for the spikes and 50 % for the oscillations). We compared our interictal results to iEEG ictal data. The regions labeled as seizure onset zone (SOZ) belonged to interictal networks in a large proportion of cases: 75 % (resp. 58 %) for spikes and 58 % (resp. 33 %) for oscillations in iEEG (resp. MEG). A subset of SOZ regions were detected by one type of discharges but not the other (25 % for spikes and 8 % for oscillations). Our study suggests that spike and oscillatory activities involve overlapping but distinct networks, and are complementary for presurgical mapping.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Electrophysiological techniques such as electroencephalography (EEG) and magnetoencephalography (MEG) can be used to characterize brain function and dysfunction in a non-invasive way, with high temporal accuracy. Traditionally, processing was performed at the sensor level, by comparing time courses across regions and experimental conditions. Recent advances now permit to reconstruct temporal dynamics in cortical regions of interest (Mamelak et al. 2002). These reconstructed signals allow, in turn, investigating the dynamics of network activations (David et al. 2002). Thus, interactions between different brain regions can be estimated with measures of connectivity (Horwitz 2003; Darvas et al. 2004), such as correlation (Peled et al. 2001), coherence (Gross et al. 2001), Directed Transfer function (DTF) (Kaminski and Blinowska 1991) or Dynamic Causal Modeling (Kiebel et al. 2009).
In the particular case of epilepsy, non-invasive electromagnetic source localization allows the investigation of the generators of epileptic discharges (Michel et al. 2004). In some cases, it can help guiding placement of intracranial EEG, in the form of grids (electrocorticography) or intracerebral electrodes (intracerebral EEG, iEEG). Several regions can be involved, either as propagation areas or acting together during the generation of epileptic discharges (Bartolomei et al. 2008). The fine characterization of such epileptogenic networks is the goal of presurgical evaluation, where the regions to be resected surgically need to be precisely defined.
Most studies on epileptic networks were performed on intracerebral recordings, during ictal or interictal discharges, or in MEG and EEG on interictal epileptic spikes (Lantz et al. 2003). However, another prominent marker of epilepsy, particularly frequent in cortical malformation (Palmini et al. 1995), consists in epileptic oscillations in the gamma band A major question is whether networks involved in transient epileptic spikes and in epileptic oscillations differ, in terms of neuronal substrates. Our goal here was therefore to investigate the neural networks involved in the genesis of interictal epileptic oscillations (detected in the beta-gamma band) and spikes in two modalities of recordings: (MEG and intracerebral EEG), and to compare the obtained results along two lines: non invasive (MEG) versus invasive (IEEG), and oscillations versus spikes.
Materials and Methods
Patient Selection
We selected 5 drug-resistant patients from the Clinical Neurophysiology Department of the Timone hospital in Marseille, with the following criteria: (1) they had both MEG recordings and intracerebral EEG (Stereotaxic intracerebral EEG, iEEG) recordings (Talairach et al. 1974) for presurgical investigation and (2) MEG recordings were showing stable and frequent interictal activity, including both spikes and oscillations. For the MEG recording, informed consent was obtained from each patient. The study of MEG signals was approved by the institutional Review board of INSERM, the French Institute of Health (IRB0000388, FWA00005831).
Table 1 lists the clinical information for all patients. Doses were given for medication that can influence oscillatory activity.
Signals
Recording of signals is detailed in Sections “MEG Acquisition” and “Intracerebral EEG”; signal processing presented in the subsequent sections was performed with the Matlab software (Mathworks, Natick, MA), with the help of the EEGLab (Delorme and Makeig 2004) and Brainstorm (Tadel et al. 2011) toolboxes.
MEG Acquisition
MEG signal were recorded on two systems: a 151 gradiometers system (CTF Systems Inc., Port Coquitlam, Canada) (patients one, two and three) and a 248 magnetometer system (4D Imaging, San Diego, California) (patients four and five). No activation procedure was used (no sleep deprivation, no reduction in antiepileptic drugs). In order to minimize artifacts, the patient was lying at rest, awake with eyes closed. Spontaneous activity was recorded at a sampling frequency of 1025 Hz for the CTF system and 2035 Hz for the 4D system. Recording sessions were composed of several runs. For the 4D runs, three continuous epochs of 100 s each were acquired (total of 5 min). For the CTF runs, 20 epochs of 5 s each were recorded, triggered visually on spike appearance (from -3 s to +2 s around button press). Before and after each run, head position was digitized with the help of 3 coils placed on the head. For the CTF system, a Fastrak 3SPACE, (Polhemus, Colchester, VT, United Kingdom) was used. For the 4D system, we used the built-in digitizer. This information was used later to match the data from magnetic resonance imaging (MRI) and MEG. A given run was waived if the position of the head before and after the run changed by more than 5 mm (Table 2).
Intracerebral EEG
Intracerebral EEG was performed during presurgical evaluation of the patients, using multi-contact depth electrodes (Alcis, Besançon, France). Electrode characteristics are: diameter 0.8 mm, 10–15 contacts, and each 2 mm long with an inter-contact distance of 1.5 mm. They were implanted intracerebrally according to Talairach’s stereotactic method (Talairach and Bancaud 1973). Precise localization of the target cortical structures was based on surface rendering of the 3D T1 weighted sequence, on 3D MRI reconstruction and on per-operative telemetric angiography. 7–16 electrodes were implanted, providing 70–128 points of measurement in each case and consequently an extended electrophysiological sampling of the brain areas of interest. The cortical targets for the positioning of electrodes were determined by the clinical, neurophysiological and anatomical characteristics of each patient. The exact position of each depth electrode contact was ascertained post-operatively, using the immediate post-operative CT scan and the MRI performed following electrodes removal.
Preprocessing
Detection of patterns
Visual selection of oscillations and spikes in MEG and intracerebral EEG was performed with help from an experienced clinical neurophysiologist (M.G.). Around 30 oscillations and spikes were selected for each of the 5 patients (this number could be achieved either from one or several runs). We selected oscillations that were temporally separated from spikes in order to avoid spurious oscillations by filtering transient signals (Bénar et al. 2010). Sections of 300 ms were created around each spike or oscillation (Jmail et al. 2011). Oscillations in the 15–45 Hz band were marked on MEG and IEEG by visual inspection. We only kept oscillations with at least three cycles in order to avoid filtering artifacts (Bénar et al. 2010).
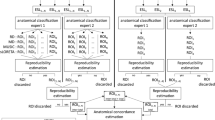
Classification
The k-means algorithm is an unsupervised method of classification (clustering). The goal is to group spikes based on distance metric (Lin et al. 2006). Before clustering, spikes were realigned with respect to their peaks on the global field power; the metric used was the Euclidian distance (Van’t Ent et al. 2003) performed across all time points and channels. We selected the number of classes based on a visual inspection. After clustering, we kept only the group containing the highest number of spike. We retained the same number of spikes for all patients, equal to the minimum number across patients (12).
Band Pass Filtering
We concatenated separately the time windows containing spikes and oscillations and applied FIR filtering on the resulting signals (Jmail et al. 2011). For spikes, a band-pass filter was applied between 10 and 45 Hz in order to eliminate the following slow component. For oscillations a filter was applied between 15 and 45 Hz. For both filters, the ripple amplitude in the pass band was set to Rp = 3 % and the attenuation in the stop band to Rs = 30 dB.
MEG Source Localization
Forward Problem
A multiple-sphere head model was constructed for each subject (Sarvas 1987). We first performed segmentation and meshing of cortex and scalp surfaces, with the BrainVisa software (Grova et al. 2006).
We then imported the surfaces in the Brainstorm Matlab toolbox (Tadel et al. 2011). A registration was performed between the MRI and the sensors based on three fiducial markers: nasion, left and right preauricular points (Grova et al. 2006). A sphere was fitted separately for each sensor, tangent to the brain surface.
Inverse Problem: Identification of Active Regions
In a first step, we identified the active regions as local peaks in a distributed sources solution. We performed the inverse problem on average events (spikes or oscillations). The average was performed across events realigned with respect to the global field power (GFP).
We used a minimum norm estimate (MNE) (Hämäläinen and Ilmoniemi 1994) with dipoles distributed on a reconstruction of the cortex obtained from MRI, constrained to be perpendicular to the cortex. The advantage of a distributed solution is that it does not require specifying a priori the number of sources. The solution was computed with the Brainstorm software, using the following parameters: sources constrained to the normal direction to the cortex, regularization parameter corresponding to a signal to noise ratio equal to three, depth weighting of 0.5. We used an estimate of the noise covariance on a baseline preceding the discharges of the average signal.
On the resulting film of activation, we defined the active regions visually as local peaks with high amplitude (secondary local peaks in neighbourings sulci or gyri were ignored). All the MNE peaks were considered as nodes of interest. The number of MNE maxima through the five patients ranged between four and nine. It is to be noted that at a later step statistics are used in order to threshold connectivity graphs: potential spurious peaks are expected not to survive this thresholding.
Inverse problem: reconstruction of time courses
In a second step, we placed a regional dipolar source [3 orthogonal dipoles, i.e. a ‘rotating dipole’ (Scherg 1996)] on each active region as defined by the MNE distributed solution (see previous section). This avoids a potential impact of regularization on the estimation of time series (David et al. 2002),which could result in cross talk across sources. The inversion was performed on the concatenation of all events, separately for spikes and oscillations.
For each active region, data was projected on the three dipoles by linear regression, resulting in one time course per region. We performed a singular value decomposition (SVD) on the three time courses and selected the component with higher energy. This resulted in a single estimated time course for each event (spike or oscillation) within each region, on which connectivity analysis was performed (see next section).
Connectivity
Computation of Graphs
Graphs of connectivity were computed either on MEG data after source reconstruction or directly on the IEEG signals, with one node for each region. The time windows of all events of a given type (spike or oscillation) were concatenated to form a single continuous signal (as in Section “Inverse problem: reconstruction of time courses”).
On the estimated time courses (see Section “Classification”), and for a given type of activity (spike or oscillation), we computed the cross-correlation for a series of lags (from −50 to +50 ms) and kept the lag corresponding to maximum correlation. The sign of the lag determined the directionality of the link. (see next section).
Surrogate Data
In order to threshold the graphs, we used a non-parametric method. Surrogate data were generated by computing the Fourier transforms of the original signals, randomizing the Fourier phases while preserving the modulus, and then performing inverse Fourier transform. This resulted in data with identical spectra but random phases (Prichard and Theiler 1994). We generated n = 1000 surrogate realizations. Correlations were computed for all pairs of regions; we kept at each realization the maximum across pairs (in absolute value), in order to take into account multiple comparisons (Pantazis et al. 2003). We selected the threshold on the resulting histogram corresponding to p = 0.05.
Definition of “Starter” Nodes
We aimed at finding the network nodes from which activity originates before spreading to other regions. We made the hypothesis that these nodes correspond to the more hyper excitable regions, therefore putatively giving information on the regions to be resected surgically. These “starter” nodes were defined as nodes with only outgoing links (i.e. directionality going from starter node to other nodes).
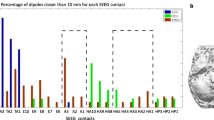
Intracerebral Distribution of Spikes and Oscillations
We measured the intracerebral distribution of oscillations and spikes in order to evaluate the correspondence between the two types of activities at the local level (within each cortical region). We marked visually the contacts involved for spikes and oscillations, with three classes: spikes only, oscillations only and mixed oscillations and spikes.
In order to compare visually the localization of the different results (MEG vs iEEG, and spikes vs oscillations), the cortex was divided into regions by an expert neurologist (MG). These regions were: central (medial, lateral); cingular (posterior); frontal (basal, lateral, pole); hippocampal tail; mesencephalic; occipital (lateral, pole, posterior); occipito-parietal; occipito-temporal (lateral, medial); parietal (inferior, lateral, medial, opercular, superior); prefrontal (medial, lateral); temporal (anterior, basal, lateral, middle, medial, posterior, pole, superior); temporo-parieto-occipital junction.
Results
Data Selection and Source Localization
Figure 1 presents examples of spikes (Fig. 1a) and oscillations (Fig. 1b) detected visually on MEG data for one patient (patient 2).
Figure 2 illustrates the spatial overlap between spikes and oscillations at the level of IEEG contacts for one patient. For all patients, we observed an overlap between the two types of activity within the same electrodes which ranges, between 10 and 50 % for spike contacts and between 15 and 63 % for oscillation contacts. However, in a large proportion of contacts there are only spikes or only oscillations. Also, it is to be noted that there are less contacts involved in oscillations that in spikes.
Figure 3 summarizes the steps involved in the construction of the graph for the spikes corresponding to the patient shown on Fig. 1 (for details, see methods section). First, the movie of source localization on the average signal (MNE method) was reviewed and the peaks of activity marked visually (Fig. 3a). Then the signals at the peaks were extracted at a single event level for spikes and oscillations (Fig. 3b, c). The first component of the SVD captured more than 85 % of the original signal for each region (range 85–88 %). Finally, a connectivity graph across signals from all the peaks was constructed with a statistical threshold obtained non-parametrically (Fig. 3d).
Steps involved in the construction of the connectivity graph (patient 2). a Movie of source localization by MNE on the average spike. The MNE method was applied at each time point, and the local peaks were identified visually on the movie of activation across the whole event. The step between two snapshots is 25 ms. Black circles indicate the local peaks. b Average spike across all sensors. c Average oscillation over all sensors. d Connectivity graph across regions, with a statistical threshold. Colors represents the connection strength, the number is the lag value for each connection. Black arrows indicate directionality of the link (Color figure online)
Connectivity Graphs
Supplementary Table 1 summarizes the regions involved in spikes and oscillations in MEG and IEEG as well as the concordance between regions presenting network nodes. In Supplementary Table 2, the coordinates of the MEG nodes for which there is a corresponding iEEG node are listed, together with the distance between MEG and iEEG nodes. The median distance between MEG and iEEG nodes is 2.1 cm, and the range is 1.1–3.5 cm.
Figure 4 presents the results of MEG and IEEG networks for interictal spikes and oscillations, as well as the nodes identified as starters, shown as blue circles (for the definition of starters see Section “Forward problem” in Fig. 4a (patient 1), MEG spikes and oscillations share the right lateral occipito-temporal areas. However, the network for oscillations is more extended towards the right fronto-polar regions. In MEG, starters for spikes and oscillations in the right occipito-temporal junction are concordant. Concerning IEEG, we notice that the oscillation network involves more medial regions than the spike network in the parietal lobe, and is more extended towards the posterior temporal medial region. There are IEEG starters in the occipito-parietal region for both spikes and oscillations, with another starter in the medial occipito-temporal region for oscillations. These results are consistent with the lesion in this patient, which is in the lateral occipito-temporal region (focal cortical dysplasia). Starters in IEEG for spikes and oscillations share the right occipito-parietal, which is consistent with the seizure onset zone.
MEG and iEEG networks for interictal spikes and oscillations, a–e patients 1–5. Columns correspond to: MEG spikes, MEG oscillations, iEEG spikes, iEEG oscillations. Blue circles show starters (regions from which arrows originate). Oscillation and spike network bear similarities, but are not identical. In general, non-invasive localization is well confirmed by intracerebral EEG when there is an iEEG electrode in vicinity (Color figure online)
Figure 4b illustrates the results for patient 2. Networks for MEG spikes and oscillations have several regions in common (left occipital and right temporal pole), but differ in several others (in particular L temporal and R occipital). We notice that for MEG spikes networks, there is no starter while for MEG oscillations networks there are four starters. The left temporal lateral posterior region is visible both in IEEG (spikes and oscillations) as a starter (GL, C depth electrodes) and in MEG spikes (L1, L5), and is part of the seizure onset zone. The left occipital region is seen in IEEG (spikes and oscillations) as a starter, and in MEG (spikes and oscillations, starter for oscillations), and is also part of the SOZ.
In Fig. 4c (patient 3), MEG oscillatory network is more widespread than MEG spikes network, in particular with involvement of the right occipital pole and the right prefrontal region. Leading regions are different, bilateral parietal mesial for oscillations and right parietal and temporal pole for spikes. In IEEG, networks are very similar, with more leading regions for spikes than oscillations. The left central medial region is visible in MEG spikes, IEEG spikes and oscillations (starter for oscillations) and is part of the seizure onset zone. The left prefrontal region is visible in all graphs, starter for IEEG spikes, and is part of the SOZ.
Figure 4d illustrates results for patient 4. MEG networks are similar for spikes and oscillations on the right side, involving the occipito-parietal and temporal regions. There are 2 starters identified on MEG, in the right occipito-parietal region for oscillations and in the right temporal posterior region for spikes. In IEEG, spikes network is wider than oscillations network, involving regions consistent with those found in MEG on the right side. There is only one starter for oscillations, in the temporo-parieto-occipital junction. The seizure onset zone is large, involving regions from posterior to anterior temporal lobe (Supplementary Table 1). The temporal posterior SOZ region is visible in IEEG interictal (both spikes and oscillations) and in MEG spikes (as a starter). The temporal anterior medial SOZ region is visible in MEG and IEEG oscillations.
Figure 4e shows results for patients 5. In MEG, spikes and oscillations networks have similar extent, both involving left and right parietal areas. The IEEG network for spikes is involving right parieto-central and the right cingulate posterior regions, but it is to be noted that spatial sampling is limited. For oscillations, only the right precentral region is involved. The right parietal region is visible in MEG (spikes and oscillations) and IEEG spikes, and is part of the seizure onset zone. The parietal inferior SOZ region (Supplementary Table 1) is visible in MEG and IEEG spikes (and is the starter for MEG).
From Supplementary Table 1, one can quantify the level of match between modalities (MEG and IEEG) and across type of activity (spikes and oscillations).
In MEG, nodes corresponding to spikes were matched to regions detected for oscillations in 28 out of 52 cases (54 %). Conversely, nodes corresponding to oscillations were matched to regions detected for spikes for 28 cases out of 50 (56 %). Considering regions detected in both types of activities (spikes and oscillations), there was a total of 74 regions with 28 (38 %) in common. In IEEG, spike nodes were matched to oscillation nodes for 11 cases out of 22 (50 %), and the reverse for 11 nodes out of 18 (61 %). In total, there were 11 regions in common out of 29 (38 %).
In the cases where an IEEG contact was in the region detected in MEG, MEG nodes were confirmed by IEEG in 15/19 cases (79 %) for the spikes, and in 6/12 cases (50 %) for the oscillations. Conversely, when a node was detected in IEEG, it was seen in MEG in 15 cases out of 23 (65 %) for the spikes, whereas this was true only in 6 cases out of 17 (35 %) for the oscillations.
In term of network starters, the match in MEG between spikes and oscillations starters is very low (only one case out of 16). In IEEG, the match in network starters is higher: 4 out of 10 regions are matching. Only one MEG starter was confirmed as starting region by IEEG (this concerns only the 5 starters for which there was an IEEG electrode in the same region).
However, if one checks for each starter in each type (spikes or oscillations) whether the same region was detected in the other type, independently of being a starter or not, then the level of match is high. In MEG, nodes corresponding to spike starters were matched to regions detected for oscillations in 7 out of 9 cases (78 %). Conversely, nodes corresponding to oscillation starters were matched to regions detected for spikes for 5 cases out of 8 (63 %). In IEEG, nodes corresponding to spike starters were matched to regions detected for oscillations in 5 out of 6 cases (83 %). Conversely, nodes corresponding to oscillation starters were matched to regions detected for spikes for 7 cases out of 8 (88 %).
In each patient we obtained the seizure onset zone (SOZ) from the clinical report. For each region labeled as SOZ, we verified the concordance with the regions detected on spikes and interictal oscillations, for MEG and IEEG.
In terms of sensitivity, we verified for each SOZ region if there was a corresponding network node. We obtained a 67 % match for MEG spikes, 25 % for MEG oscillations, 75 % for IEEG spikes and 46 % for IEEG oscillations. If one considers starters only, the match with SOZ was 18 % for MEG spikes, 20 % for MEG oscillations, 25 % for IEEG spikes and 33 % for IEEG oscillations.
For the specificity, we tested for each leader node in MEG or IEEG if it corresponded to a region labeled as SOZ. This was the case for 22 % for MEG spikes, 25 for MEG oscillations, 50 % for IEEG spikes, 50 % for IEEG oscillations.
It is to be noted that for all patients except patient 1, at least one region of the SOZ was detected by either spikes or oscillations in MEG.
Discussion
Retrieving Networks in MEG and IEEG
MEG and IEEG are both characterized by a high temporal resolution, and a large frequency content which permits to characterize transient events such as spikes and oscillations. However, in non invasive electrophysiology (EEG and MEG), the activity of a given source is spread across several sensors, which can induce spurious synchronization when measured at the sensor level. We have used measures performed at the level of sources which provide a way to infer connectivity directly across regions (David et al. 2002).
We have confirmed that interictal spikes can involve widespread networks, in line with previous studies showing that interictal epileptic activities can propagate rapidly in IEEG (Alarcon et al. 1994) or in non-invasive electrophysiology (Larsson et al. 2010; Tanaka et al. 2010). Furthermore, we have shown that this is also the case for epileptic oscillations in the beta/low gamma band. We observed only partial overlap between the networks involved in spikes and oscillations. This suggests that the two types of activity may have different mechanisms of generation and propagation, both locally and at a large scale.
It is interesting to note that, when there was an IEEG contact in the vicinity of a node detected by MEG, we obtained confirmation of the non-invasive results by the recordings performed directly within the brain in a majority of cases, however less in oscillations that for spikes. Conversely, when a region is detected in IEEG, the proportion of times when it is detected on MEG also depends on the type of activity, higher for spikes than for oscillations. This is consistent with our other finding that oscillations involve less IEEG contacts than spikes. Indeed, detect ability at the sensor level depend on the amount of cortex involved in the discharges, which has been demonstrated for epileptic spikes (Ebersole et al. 1995; Cosandier-Rimélé et al. 2008).
We found less consistency in terms of network starters. Even though leading regions of a given type/modality corresponded to regions that were generally detected in other types/modality, only few regions were labeled as starter in more than one type or modality. This could be further indication of different mechanisms for spikes and oscillations.
Comparison with SOZ
Our results obtained on interictal activity were compared to the seizure onset zone (SOZ) as defined during IEEG presurgical evaluation. For 4 patients out of 5, there was always at least one region of the SOZ that was detected in MEG by spikes or oscillations; in one case this was in a complementary way (one region detected based on spikes and the other on oscillations).
Overall, in both MEG and IEEG, we obtained better performance for spikes than for oscillations in detection of SOZ. This is surprising in patients with focal cortical dysplasia, as oscillations in such patients are usually tightly linked with spikes (Palmini et al. 1994). This could be due to the fact that we considered oscillations away from spikes, in order to avoid mixture of the two types of activity (Bénar et al. 2010), and such oscillations are more difficult to label as purely epileptiform. Further work is needed that will be based on techniques for disentangling spikes and oscillations overlapping in time (Jmail et al. 2011).
Limitations
One of the limitations of the present study arises from the fact that two different systems have been used, one based on gradiometers (CTF) and the other on magnetometers (4D). The two systems may have different sensitivity profiles, and could require different depth weightings in the MNE solution. Still, we believe that this would not change the general pattern of our findings are solutions are compared in a regional way (i.e. at a relatively coarse resolution), and are compared within the same subject.
Moreover, limitations exist in the sampling of events. Firstly, due to a technical issue: in the CTF system, the temporal sampling is triggered on visual detection of spikes. This may limit the amount of data available for characterizing discharges, as well as set a constraint on the brain state in which oscillations are sampled. Secondly, due to the choice we made of selecting only the most representative spike and oscillation events, which do not rule out that better correspondence could arise for less frequent events. These points would deserve further investigation.
In order to produce our graph, some technical choices were made. Peaks in results of source localization were marked visually. Despite careful marking, this could lead to some errors in location, or to missing some peaks. In future work, this procedure should be automatized. Automatic registration to an atlas is alsi under development based on the work of Brovelli and colleagues (Auzias et al. 2016). Also, we computed the correlation measure on a concatenation of events of interests instead of each event separately. This makes the computation more robust by incorporating a larger amount of data, but does not take into account variability of spikes. Methods for single-trial graph analysis (Brovelli 2012) should be investigated in further studies.
Part of the discrepancy between MEG and IEEG networks can arise from the fact that some regions were not explored in iEEG. Thus, the fact that patients are not completely seizure free after surgery may indicate that parts of the SOZ were not sufficiently sampled with iEEG. The MEG nodes that are outside the iEEG implantation Sheme may indicate important regions involved in the generation of the epileptic discharges. This highlights the potential benefits of MEG in planning the iEEG implantation (Schwartz et al. 2003).
Implication for Clinical Practice
A better understanding of epileptic networks involved in spikes and oscillation, based on non-invasive characterization, could lead to better definition of the zone to be resected (Van Mierlo et al. 2014). In particular, it is expected that the identification of starters for both spikes and oscillations will contribute to the planning of SEEG implantation, pointing to areas that may have been missed by conventional evaluation. Moreover, accumulation of evidence over a large population of the adequacy of MEG network measures in finding the epileptogenic zone could lead in the future to a reduction of patients that will need invasive SEEG recordings.
Future Directions
Several types of epileptic oscillations can be detected on MEG, which may correspond to completely different mechanisms. Thus, recent studies suggest that epileptic oscillations can be detected in the beta/gamma band (Guggisberg et al. 2008; Rampp et al. 2010) as in our study, and even in the fast ripple band (Xiang et al. 2009).As high frequency activity (HFOs > 80 Hz) has been shown to be a good indicator of the seizure onset zone on intracerebral EEG (Worrell et al. 2008; Bagshaw et al. 2009; Zijlmans et al. 2011), a promising venue would be to combine network localization on beta/low gamma oscillations with localization of HFOs (Van Klink et al. 2014). This could provide a better specificity for delineating the epileptogenic zone within the distributed networks involved in epileptic discharges. In that case, development of tools for localizing specifically oscillations will be of great interest (Lina et al. 2011).
A better understanding of epileptic networks could lead to better preoperative planning and more focused interventions. Resection or gamma knife radio surgery (Régis et al. 2000) of selected parts of the network could stop seizure activity (Wilke et al. 2011). An interesting pathway resides in neurocomputational modeling of the networks (Deco et al. 2008; Wendling 2008), which could help testing hypothesis on the effect of selective surgery.
References
Alarcon G, Guy CN, Binnie CD et al (1994) Intracerebral propagation of interictal activity in partial epilepsy: implications for source localisation. J Neurol Neurosurg Psychiatry 57:435–449
Auzias G, Coulon O, Brovelli A (2016) MarsAtlas: a cortical parcellation atlas for functional mapping. Hum Brain Mapp 37:1573–1592
Bagshaw AP, Jacobs J, Levan P et al (2009) Effect of sleep stage on interictal high-frequency oscillations recorded from depth macroelectrodes in patients with focal epilepsy. Epilepsia 50:617–628
Baillet S, Mosher JC, Leahy RM (2001) Electromagnetic brain mapping. Networks 18:14–30. doi:10.1109/79.962275
Bartolomei F, Chauvel P, Wendling F (2008) Epileptogenicity of brain structures in human temporal lobe epilepsy: a quantified study from intracerebral EEG. Brain 131:1818–1830
Bénar CG, Chauvière L, Bartolomei F, Wendling F (2010) Pitfalls of high-pass filtering for detecting epileptic oscillations: a technical note on “false” ripples. Clin Neurophysiol 121:301–310
Brovelli A (2012) Statistical analysis of single-trial Granger causality spectra. Comput Math Methods Med 3:10
Cosandier-Rimélé D, Merlet I, Badier JM et al (2008) The neuronal sources of EEG: modeling of simultaneous scalp and intracerebral recordings in epilepsy. Neuroimage 42:135–146
Darvas F, Pantazis D, Kucukaltun-Yildirim E, Leahy RM (2004) Mapping human brain function with MEG and EEG: methods and validation. Neuroimage 23(Suppl 1):S289–S299. doi:10.1016/j.neuroimage.2004.07.014
David O, Garnero L, Cosmelli D, Varela FJ (2002) Estimation of neural dynamics from MEG/EEG cortical current density maps: application to the reconstruction of large-scale cortical synchrony. IEEE Trans Biomed Eng 49:975–987
Deco G, Jirsa VK, Robinson PA et al (2008) The dynamic brain: from spiking neurons to neural masses and cortical fields. PLoS Comput Biol 4(8):e1000092
Delorme A, Makeig S (2004) EEGLAB: an open source toolbox for analysis of single-trial EEG dynamics including independent component analysis. J Neurosci Methods 134:9–21
Ebersole JS, Squires KC, Eliashiv SD, Smith JR (1995) Applications of magnetic source imaging in evaluation of candidates for epilepsy surgery. Neuroimaging Clin N Am 5:267–288
Gross J, Kujala J, Hamalainen M et al (2001) Dynamic imaging of coherent sources: studying neural interactions in the human brain. Proc Natl Acad Sci USA 98:694–699
Grova C, Daunizea J, Lina JM et al (2006) Evaluation of EEG localization methods using realistic simulations of interictal spikes. Neuroimage 29:734–753
Guggisberg AG, Kirsch HE, Mantle MM et al (2008) Fast oscillations associated with interictal spikes localize the epileptogenic zone in patients with partial epilepsy. Neuroimage 39:661–668
Hämäläinen MS, Ilmoniemi RJ (1994) Interpreting magnetic fields of the brain: minimum norm estimates. Med Biol Eng Comput 32:35–42
Hirai N, Uchida S, Maehara T et al (1999) Enhanced gamma (30–150 Hz) frequency in the human medial temporal lobe. Neuroscience 90:1149–1155
Horwitz B (2003) The elusive concept of brain connectivity. Neuroimage 19:466–470
Jmail N, Gavaret M, Wendling F et al (2011) A comparison of methods for separation of transient and oscillatory signals in EEG. J Neurosci Methods 199:273–289
Kaminski MJ, Blinowska KJ (1991) A new method of the description of the information flow in the brain structures. Biol Cybern 65:203–210
Kiebel SJ, Garrido MI, Moran R et al (2009) Dynamic causal modeling for EEG and MEG. Hum Brain Mapp 30:1866–1876
Lantz G, Spinelli L, Seeck M et al (2003) Propagation of interictal epileptiform activity can lead to erroneous source localizations: a 128-channel EEG mapping study. J Clin Neurophysiol 20:311–319
Larsson PG, Eeg-Olofsson O, Michel CM et al (2010) Decrease in propagation of interictal epileptiform activity after introduction of levetiracetam visualized with electric source imaging. Brain Topogr 23:269–278
Lin R, Lee RG, Tseng CL et al (2006) Multi-channel EEG recording system and study of EEG clustring method. System 18:276–283
Lina JM, Chowdhury R, Lemay E, Kobayashi E, Grova C (2011) Wavelet-based localization of oscillatory sources from magnetoencephalography data. IEEE Trans Biomed Eng 61(8):2350–2364
Mamelak AN, Lopez N, Akhtari M, Sutherling WW (2002) Magnetoencephalography-directed surgery in patients with neocortical epilepsy. J Neurosurg 97:865–873
Michel CM, Lantz G, Spinelli L et al (2004) 128-channel EEG source imaging in epilepsy: clinical yield and localization precision. J Clin Neurophysiol 21(2):71–83
Palmini A, Gambardella A, Andermann F et al (1994) Operative strategies for patients with cortical dysplastic lesions and intractable epilepsy. Epilepsia 35(Suppl 6):S57–S71
Palmini A, Gambardella A, Andermann F et al (1995) Intrinsic epileptogenicity of human dysplastic cortex as suggested by corticography and surgical results. Ann Neurol 37:476–487
Pantazis D, Nichols TE, Baillet S, Leahy RM (2003) Spatiotemporal localization of significant activation in MEG using permutation tests. Inf Process Med Imaging 18:512–523
Peled A, Geva AB, Kremen WS et al (2001) Functional connectivity and working memory in schizophrenia: an EEG study. Int J Neurosci 106:47–61. doi:10.3109/00207450109149737
Prichard D, Theiler J (1994) Generating surrogate data for time series with several simultaneously measured variables. Phys Rev Lett 73:4
Rampp S, Kaltenhäuser M, Weigel D et al (2010) MEG correlates of epileptic high gamma oscillations in invasive EEG. Epilepsia 51:1638–1642
Régis J, Bartolomei F, De Toffol B et al (2000) Gamma knife surgery for epilepsy related to hypothalamic hamartomas. Acta Neurochir Suppl 47:1343–1351
Sarvas J (1987) Basic mathematical and electromagnetic concepts of the biomagnetic inverse problem. Phys Med Biol 32:11–22
Scherg MBP (1996) New concepts of brain source imaging and localization. Electroencephalogr Clin Neurophysiol Suppl 46:127–137
Schwartz DP, Badier JM, Vignal JP et al (2003) Non-supervised spatio-temporal analysis of interictal magnetic spikes: comparison with intracerebral recordings. Clin Neurophysiol 114:438–449
Tadel F, Baillet S, Mosher JC et al (2011) Brainstorm: a user-friendly application for MEG/EEG analysis. Comput Intell Neurosci 2011:879716. doi:10.1155/2011/879716
Talairach J, Bancaud J (1973) Stereotaxic approach to epilepsy. Methodology of anatomo-functional stereotaxic investigations. Prog Neurol Surg 5:297–354
Talairach J, Bancaud J, Szikla G, Bonis A, Geier S, Vedrenne C (1974) New approach to the neurosurgery of epilepsy. Stereotaxic methodology and therapeutic results. 1. Introduction and history. Neuro-Chirurgie 20:1
Tanaka N, Hämäläinen MS, Ahlfors SP et al (2010) Propagation of epileptic spikes reconstructed from spatiotemporal magnetoencephalographic and electroencephalographic source analysis. Neuroimage 50:217–222
van Klink NE, Van’t Klooster ΜΑ, Zelmann R et al (2014) High frequency oscillations in intra-operative electrocorticography before and after epilepsy surgery. Clin Neurophysiol 125:2212–2219
Van Mierlo P, Papadopoulou M, Carrette E et al (2014) Functional brain connectivity from EEG in epilepsy: seizure prediction and epileptogenic focus localization. Neurobiology 121:19–35
Van’t Ent D, Manshanden I, Ossenblok P et al (2003) Spike cluster analysis in neocortical localization related epilepsy yields clinically significant equivalent source localization results in magnetoencephalogram (MEG). Clin Neurophysiol 114:1948–1962
Wendling F (2008) Computational models of epileptic activity: a bridge between observation and pathophysiological interpretation. Expert Rev Neurother 8:889–896
Wilke C, Worrell G, He B (2011) Graph analysis of epileptogenic networks in human partial epilepsy. Epilepsia 52:84–93
Worrell GA, Gardner AB, Stead SM et al (2008) High-frequency oscillations in human temporal lobe: simultaneous microwire and clinical macroelectrode recordings. Brain 131:928–937
Xiang J, Liu Y, Wang Y et al (2009) Frequency and spatial characteristics of high-frequency neuromagnetic signals in childhood epilepsy. Epileptic Disord 11:113–125
Zijlmans M, Jacobs J, Kahn YU et al (2011) Ictal and interictal high frequency oscillations in patients with focal epilepsy. Clin Neurophysiol 122:664–671
Acknowledgments
The authors thank Jean Marc Lina, Olivier David, Michael Scherg and Catherine Liegeois-Chauvel for useful discussions. N. Jmail was supported by an Averroes grant from the European Community and a Campus France travelling grant. The authors also wish to thank the anonymous reviewers for their useful comments. Part of this work was funded by a joint Agence Nationale de la Recherche (ANR) and Direction Génerale de l’Offre de Santé (DGOS) under grant ‘VIBRATIONS’ ANR 13 PRTS 0011 01.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
10548_2016_501_MOESM1_ESM.docx
Supplementary Table 1 Regions involved in spikes and oscillations in MEG and iEEG and concordance between regions presenting network nodes
10548_2016_501_MOESM2_ESM.docx
Supplementary Table 2 List of sensor coordinates that are concordant between MEG and iEEG for spikes and oscillations in the 5 patients (when several IEEG contacts were present, only closest matches are shown).
Rights and permissions
About this article
Cite this article
Jmail, N., Gavaret, M., Bartolomei, F. et al. Comparison of Brain Networks During Interictal Oscillations and Spikes on Magnetoencephalography and Intracerebral EEG. Brain Topogr 29, 752–765 (2016). https://doi.org/10.1007/s10548-016-0501-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10548-016-0501-7