Abstract
Alkaptonuria (AKU) is a rare inherited metabolic disorder of tyrosine metabolism that results from a defect in an enzyme called homogentisate 1,2-dioxygenase. The result of this is that homogentisic acid (HGA) accumulates in the body. HGA is central to the pathophysiology of this disease and the consequences observed; these include spondyloarthropathy, rupture of ligaments/muscle/tendons, valvular heart disease including aortic stenosis and renal stones. While AKU is considered to be a chronic progressive disorder, it is clear from published case reports that fatal acute metabolic complications can also occur. These include oxidative haemolysis and methaemoglobinaemia. The exact mechanisms underlying the latter are not clear, but it is proposed that disordered metabolism within the red blood cell is responsible for favouring a pro-oxidant environment that leads to the life threatening complications observed. Herein the role of red blood cell in maintaining the redox state of the body is reviewed in the context of AKU. In addition previously reported therapeutic strategies are discussed, specifically with respect to why reported treatments had little therapeutic effect. The potential use of nitisinone for the management of patients suffering from the acute metabolic decompensation in AKU is proposed as an alternative strategy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Alkaptonuria
Alkaptonuria (AKU, OMIM: 203500) is a rare autosomal recessive disorder of tyrosine metabolism that occurs in one in 250 000 of the general population (Phomphutkul et al 2002). In certain countries it is observed more commonly; for example in Slovakia it is estimated to occur in one in 19 000 of the population (Zatkova 2011; Milch 1960).
AKU results from a defect in the enzyme homogentisate 1,2-dioxygenase (HGD, E.C.1.12.11.5). This results in the accumulation of homogentisic acid (HGA) in the blood. Typically, the kidney clears HGA effectively in AKU leading to the presence of gram quantities in the urine so that the amounts of HGA within the body are minimised. This is achieved both by glomerular filtration and tubular secretion of HGA. Patients with AKU that have preserved renal function demonstrate fractional clearances several hundred times greater than normal (Introne et al 2002). Increased urinary excretion of HGA is diagnostic of AKU (Phomphutkul et al 2002).
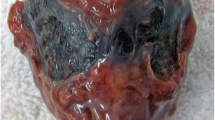
The accumulation of HGA in blood is central to the pathophysiology of the disease. It is proposed that HGA is oxidised to 1,4-benzoquinone-2-acetic acid (BQA) (Zannoni et al 1969). It is thought that BQA polymerises to form a melanin like pigment, which deposits in connective tissues in a process called ochronosis. The consequences of this chronic process are typically observed from the third to fourth decade of life and include spondyloarthropathy, rupture of ligaments/muscle/tendons, valvular heart disease including aortic stenosis and renal and prostate stones (Ranganath et al 2013). Acute metabolic decompensation can occur in AKU presenting with fatal complications, including oxidative haemolysis and or methaemoglobinaemia. It is the latter that will form the basis of this article. Herein the pathophysiology of why these acute complications may occur and the current literature will be reviewed.
Acute metabolic complications associated with alkaptonuria
There are eight cases in the literature reporting the acute fatal metabolic complications that can occur in AKU (Table 1). These include three patients that had oxidative haemolysis and methaemoglobinaemia (Abreo et al 1983; Suehiro et al 2007; Mullan et al 2015); three patients with methaemoglobinaemia (Liu and Prayson 2001; Uchiyama et al 2010; Miyasaka et al 2013) and two patients with oxidative haemolysis (Heng et al 2010; Bataille et al 2014). In all cases the outcome was death.
Common to all of these cases is that all patients had acute kidney injury (AKI), in some cases this was a new presentation and in others it occurred on a background of chronic kidney disease (CKD). Five of eight patients also presented with sepsis (Liu and Prayson 2001; Suehiro et al 2007; Uchiyama et al 2010; Miyasaka et al 2013; Mullan et al 2015). As previously mentioned the kidney plays a critical role in the elimination of HGA from the body, and thus it is reasonable to expect significant increases in the circulating concentration of HGA when kidney function is impaired. In all eight cases reported HGA was not measured, but is presumed to have been increased as kidney function was impaired.
Introne et al (2002) reported on a patient with AKU and CKD, where an increased plasma concentration of HGA was observed along with worsening clinically apparent ochronosis. Three months post renal transplantation the concentration of HGA was decreased from 126.3 to 43.7 μmol/L demonstrating the importance of kidney function in the elimination of HGA.
Interestingly, no acute oxidative haemolysis or methaemoglobinaemia was reported despite the very high concentrations of plasma HGA. This is in keeping with others (Venkataseshan et al 1992; Kazancioglu et al 2004; Faria et al 2012) where CKD has been reported in AKU and no fatal metabolic complications have been observed. This highlights that an elevated concentration of HGA alone is not responsible for the fatal metabolic complications that have been observed in other reported cases (Abreo et al 1983; Suehiro et al 2007; Mullan et al 2015; Liu et al 2001; Uchiyama et al 2010; Miyasaka et al 2013; Heng et al 2010; Bataille et al 2014). The authors’ hypothesise that multiple ‘insults’ to anti-oxidant defence mechanisms have a cumulative effect and are responsible for the reported haematological complications.
In all published cases where fatal metabolic complications were observed treatments utilised were unsuccessful. The reasons for this are not entirely clear. Treatments were based around renal replacement therapy (haemodialysis and haemofiltration), blood transfusion and anti-oxidant therapies including; vitamin C, N-acetyl cysteine (NAC) and methylene blue. Some of these therapies can act as pro-oxidant molecules, thus worsening the metabolic complications.
Pathophysiology of acute haematological complications observed in AKU
Mechanisms maintaining the pro- and anti-oxidant balance
Oxidative stress is a disturbance between the pro-oxidant reactions and anti-oxidant defence mechanisms, which favours the former. Under healthy physiological conditions, pro-oxidant reactions do not predominate as red blood cells (RBCs) have greater than 250 times more reducing capacity than oxidizing potential (Burak Cimen 2008). Some of the consequences of a pro-oxidant environment predominating include damage to DNA, membrane ion transport systems, enzymes, proteins and lipid peroxidation (Al-Omar et al 2004; Masella et al 2005).
Oxidative stress can lead to the generation of free radicals. These are chemical entities that possess an unpaired electron and are formed from a one or two electron reduction of oxygen. Reactive oxygen species (ROS) include the non-radical hydrogen peroxide and singlet oxygen, as well as the radicals: superoxide anion, hydroxyl radical and nitric oxide (9) (Fig. 1).
Exogenous and endogenous factors influencing the oxidation of haemoglobin, including the potential role of homogentisic acid and ‘soluble melanins’ and the biological mechanisms responsible for the reduction of methaemoglobin. ROS—reactive oxygen species; H2O2—hydrogen peroxide; O2—singlet oxygen; O2 .−—superoxide anion; HO.—hydroxyl radical; NO—nitric oxide; PPP—pentose phosphate pathway; NADH—nicotinamide adenine dinucleotide; NADPH—nicotinamide adenine dinucleotide phosphate; G6PD—glucose-6-phosphate dehydrogenase; FAD+—flavin adenine dinucleotide; FMN—flavin mononucleotide
Enzymatic systems, principally found within RBCs, act as defence mechanisms against oxidative stress (Figs. 1 and 2). Key enzymes include: glutathione peroxidase, glutathione reductase, catalase, cytochrome b5 reductase, superoxide dismutase, glucose-6-phosphate dehydrogenase (G6PD) and thioredoxin reductase. Non-enzymatic factors that contribute to maintaining the redox state of the body include: (a) vitamins A and E, ubiquinone and melatonin, all of which are lipophilic, and (b) vitamin C, glutathione, uric acid, caeruloplasmin, transferrin and haptoglobin all of which are water soluble.
Enzymatic systems in the red blood cell responsible for maintaining the redox state of the body. The pathways detailed demonstrate the role of the glutathione, thioredoxin and superoxide dismutase in reducing oxidative species generated in the red blood cell. H2O2—hydrogen peroxide; O2—singlet oxygen; O2 .−—superoxide anion; HO.—hydroxyl radical; NO—nitric oxide; PPP—pentose phosphate pathway; NADH—nicotinamide adenine dinucleotide; NADPH—nicotinamide adenine dinucleotide phosphate; G6PD—glucose-6-phosphate dehydrogenase
Disturbance of the pro- and anti-oxidant balance in AKU
HGA is present at very high concentrations in individuals with AKU (serum HGA approximately 30–40 μmol/L, non-AKU reference range <3.1 μmol/L (Davison et al 2015)). HGA alone is unlikely to be directly responsible for promoting a pro-oxidant environment, and the consequent acute oxidative haemolysis or the formation of methaemoglobinaemia that have been observed in AKU due to oxidative stress.
HGA undergoes auto-oxidation to form BQA polymers, also referred to as ‘soluble melanins’ (Hegedus and Nayak 1994). The latter are purported to have pro-oxidant properties. It is proposed that the oxidative stress associated with these melanins and their associated metabolites/free radicals (i.e. of oxygen radicals such as superoxide anion, hydroxyl radical and hydrogen peroxide) are a potential ‘trigger’ for oxidative haemolysis. Adding vitamin C and glutathione to cultured cells has been shown to reverse oxidative haemolysis (Hegedus and Nayak 1994).
The role of oxidative stress and its contribution to the mechanisms of the ochronotic process have been studied extensively. This is a progressive chronic disorder and thus an extensive discussion is beyond the scope of this article that is concerned with the acute metabolic complications that can be observed in AKU (see Braconi et al 2015 for a recent review).
CKD has been shown to reduce the anti-oxidant capacity of the body (Stepniewska and Ciechanowski 2005; Stepniewska et al 2006; Olszewska 2004). However when kidney function is stable in CKD, acute complications are not frequently observed. Rapid decline of renal function resulting from an acute insult to the body, for example due to an infection or drug toxicity, can lead to AKI (Table 1). It is thought that this may predispose an individual to the acute oxidative haemolysis.
When AKI occurs in AKU it is proposed that there is a significant retention of HGA, owing to the reduced excretory capacity of the kidney. This in turn may mean that more HGA is oxidised to ‘soluble melanins’, and an excess of ROS are generated. Together these exceed the anti-oxidant capacity of the body by consuming the substrates required for the anti-oxidant defence mechanisms (e.g. NADH, NADPH, vitamin C). This may be exacerbated further by underlying deficiencies in anti-oxidant defence mechanisms; these may have a genetic (e.g. reduced enzyme activity) and or an environmental basis (e.g. poor nutrition). Together these factors are likely to contribute to oxidative haemolysis and or methaemoglobin (MetHb) (Fig. 1), both of which can be fatal as they reduce oxygen carriage to tissues and lead to cyanosis. It is also important to consider that while AKI can occur as a consequence of oxidative stress it can result from massive haemolysis (e.g. G6PD deficiency).
Secondary amyloidosis is another important consideration. It is a serious life threatening complication of AKU and is known to contribute to the decline of renal function in AKU (Millucci et al 2015; Millucci et al 2012). Amyloid A protein is responsible for amyloid A amyloidosis, which occurs in long term inflammatory conditions (Urieli-Shoval et al 2000). The N-terminal fragment of serum amyloid A is an apolipoprotein synthesised by the liver under the transcriptional regulation of inflammatory cytokines (Simons et al 2013). In a minority of patients a sustained inflammatory stimulus and the overproduction of amyloid A protein can lead to protein mis-folding and amyloid deposition (secondary amyloidosis) may occur resulting in kidney damage (Simons et al 2013; Millucci et al 2015).
In considering the impact of CKD on the pro- and anti-oxidant balance we can get an appreciation of why, when AKI occurs, specifically in patients with AKU the outcome can be fatal. It is clear that there appears to be no single factor that is responsible, rather an intricate interplay of several factors.
In CKD (Stepniewska and Ciechanowski 2005; Stepniewska et al 2006; Olszewska 2004) and AKI (Himmelfarb et al 2004) the anti-oxidant capacity of the body is reduced.
Uraemic toxins, observed in CKD have been shown to be associated with enhanced oxidative stress. This occurs indirectly by carbonyl compounds which are generated from the metabolism of carbohydrates and lipids to form advanced glycation and lipid end products, and by the carbonyl modification of proteins (Inagi and Miyata 1999; Miyata et al 2001). The consequences of this are observed in dialysis related amyloidosis.
Treatment of uraemic patients with haemofiltration or haemodialysis has also been shown to increase oxidative stress and reduces the concentration of anti-oxidants in the blood (Stepniewska and Ciechanowski 2005; Stepniewska et al 2006; Olszewska 2004). In addition, lack of vitamins A and E, and selenium, blood transfusion and parenteral iron administration have been shown to promote a pro-oxidant environment (Stepniewska and Ciechanowski 2005; Stepniewska et al 2006; Olszewska 2004; Agarwal et al 2004; Karkouti 2012). More specifically it has been shown that in the RBCs of patients with CKD the pentose phosphate pathway (PPP) does not generate adequate supplies of reductive equivalents (i.e. NADPH) necessary to restore reduced glutathione (GSH) (Stepniewska et al 2006), an important free radical scavenger, thus increasing oxidative stress.
Furthermore as haemodialysis causes a significant loss of glucose, which is essential for the PPP, significant changes in the anti-oxidant system of the blood of patients with CKD occurs. It has been demonstrated that the activity of RBC glutathione peroxidase decreases with the duration of dialysis, thus potentiating the effects of oxidative stress (Stepniewska et al 2006). Lower RBC concentrations of selenium in dialysed patients have also been shown to correlate with lower glutathione peroxidase activities (Stepniewska et al 2006).
RBCs in patients with CKD are also exposed to an increased activity of free radicals. The net consequence of this is that peroxidation of lipids and proteins in RBC membrane occurs (Ceballos-Picot et al 1996). This reduces the stability of the RBC and increases the likelihood of haemolysis. Advanced oxidation protein and glycation end products also contribute to this and increase the likelihood of haemolysis (Ceballos-Picot et al 1996).
Disturbances of anti-oxidant enzyme activity in other metabolic pathways can also occur. These include reactions that involve superoxide dismutase, glutathione peroxidase, catalase and glutathione reductase (Fig. 2). The extent to which these pathways are altered is determined by the stage of CKD and efficiency of treatment (Stepniewska and Ciechanowski 2005).
Of particular note is that the energy production in RBCs depends largely on glycolysis, with glucose as the principal substrate. Both glycolysis and the PPP generate NADH and NADPH, respectively to reduce MetHb, which is being continuously produced. If aberrations occur in these systems a pro-oxidant environment will dominate and MetHb will be present at higher concentrations (normal reference range <1.5 %, fatal >70 %).
In health there are two main mechanisms to minimise the formation of MetHb (Skold et al 2011). The first is to minimise the formation of ROS and the second to reduce ferric (Fe3+) iron back to its ferrous (Fe2+) state. The main enzyme in RBCs that does this is cytochrome b5 reductase, which utilises NADH to reduce cytochrome b5 which in turn reduces MetHb (Skold et al 2011).
A second enzyme called flavin reductase also contributes to maintaining haemoglobin in the ferrous state through its utilisation of NADPH and the co-factor methylene blue, to form leukomethylene blue (Fig. 1). Riboflavin, flavin adenine dinucleotide and flavin mononucleotide also act as electron acceptors to reduce MetHb back to its ferrous state.
A very important consideration in RBC oxidative stress is the activity of the enzyme G6PD. This enzyme is central to the formation of the reducing equivalents NADH and NADPH. A deficiency in G6PD can lead to inadequate formation of NADPH and NADH, the consequence of which is that the demands of anti-oxidant regulatory pathways are not met. This predisposes an individual to an increased risk of haemolytic anaemia and or methaemoglobinaemia (Cappellini and Fiorelli 2008). In all cases reported (Table 1) the activity of G6PD was not documented, and may have been an independent risk factor for the development of the fatal metabolic complications observed.
Altered activities of other enzymes responsible for maintaining the balance between anti- and pro-oxidants are also important to consider. It has been suggested that cytochrome b5 reductase, catalase and glutathione synthetase deficiency may put individuals at risk of drug induced methaemoglobinaemia or haemolytic anaemia (Cappellini and Fiorelli 2008; Beutler and Baluda 1963).
Treatment options currently employed in haemolysis in AKU
All therapeutic strategies employed in the eight cases reported (see Table 1) failed to demonstrate therapeutic benefit, as all patients died. It is important to consider why this is the case. Treatments included vitamin C, NAC, methylene blue, blood transfusion and renal replacement therapy (i.e. haemodialysis and or haemofiltration).
Regardless of treatment it is clear that the supply of reducing equivalents were inadequate to meet the cellular demands to minimise oxidative stress, thus oxidative haemolysis and or the formation of MetHb occurred.
Increased oxidative stress from the generation of ‘soluble melanins’ (pro-oxidants) may have saturated anti-oxidant mechanisms causing depletion of NADPH and thus when these treatments were given they were ineffective.
Both vitamin C and NAC (Fig. 2) are key co-factors in the recycling of thioredoxin and glutathione, respectively. Vitamin C is a self-limiting anti-oxidant mechanism as humans cannot synthesise vitamin C. Moreover, vitamin C when given at high concentrations has been shown to induce haemolysis in patients with G6PD deficiency (Cappellini and Fiorelli 2008). No patients were reported to have G6PD deficiency; however this may have been a contributing factor in the lack of therapeutic response to anti-oxidant therapy.
The use of NAC is entrenched in the medical literature for the treatment of oxidative liver damage, observed in paracetamol overdose. This is because of its role in the recycling of glutathione. While its use in AKU has not been assessed for clinical efficacy, it has been used (Heng et al 2010; Mullan et al 2015) based on its purported benefits as an anti-oxidant. It is likely that therapeutic benefit has not been demonstrated in patients with AKU due to the magnitude of pro-oxidant species present.
Methylene blue has a number of clinical uses but at first glance seems counter intuitive as therapy for the treatment of oxidative stress in AKU as it can behave as a pro-oxidant at higher concentrations, thus potentially exacerbating oxidative stress. In addition there are concerns over its use in patients that have G6PD deficiency as it can lead to life threatening haemolytic anaemia (Beutler and Baluda 1963). It is proposed that leukomethylene blue can diffuse into G6PD deficient RBCs resulting in haemolysis (Beutler et al 1963).
Haemodialysis and or haemofiltration were used as treatments in five of the eight cases reported (Suehiro et al 2007; Mullan et al 2015; Miyasaka et al 2013; Heng et al 2010; Bataille et al 2014). While this in principle may have facilitated the removal of HGA, thus potentially reducing the formation of ‘soluble melanins’ and oxidative stress. It is known that haemodialysis increases oxidative stress as anti-oxidant defences are reduced by pro-oxidant haemodialysis factors, which is more profound in patients with renal anaemia (Stepniewska and Ciechanowski 2005; Stepniewska et al 2006; Olszewska 2004). Therefore this treatment is not without its limitations.
As a consequence of haemolysis the majority of patients (Table 1) were given blood transfusions. This is a lifesaving treatment during haemolysis; however it is known that transfusions can harm the kidney. The exact mechanism of how this occurs is not fully understood. It is know that RBCs during storage undergo biochemical and morphological change and it is thought that after transfusion these changes promote a pro-inflammatory state impairing oxygen delivery to tissues and promoting oxidative stress (Karkouti 2012).
In all it can be seen that there were limitations to all medical therapies given in the cases reported. In principle renal transplantation could serve to reduce the circulating concentration of HGA (Introne et al 2002) and thus reduce the risk of oxidative haemolysis and or the formation of MetHb, however this is not a treatment that could be implemented rapidly and has its own challenges (i.e. risk of graft rejection). A potentially lifesaving therapy could be the utilisation of a therapy that decreases the production of HGA and this can be achieved by a drug, namely nitisinone.
The need for more effective therapy in AKU complicated by acute haemolysis—the case for nitisinone
Nitisinone is a reversible competitive inhibitor of HGD (McKiernan 2013). It is used off licence for the treatment of AKU in Liverpool at the National Centre for AKU and is now being evaluated in a long term (5-years) multi-centre trial (SONIA-2) comparing a 10 mg daily dose to no treatment. Nitisinone is not yet licenced to treat children with AKU.
Nitisinone has been demonstrated to significantly reduce the serum concentration of HGA (Phomphutkul et al 2002; Introne et al 2011; Suwannarat et al 2005; Ranganath et al 2014). This has also been shown in a mouse model of AKU (Preston et al 2014). If the additional ‘insult’ for the haematological complications in AKU is the formation of pro-oxidants as a consequence of HGA accumulating and being metabolised to ‘soluble melanins’ then the inhibition of the formation of HGA would be a highly suitable treatment. Moreover, the drop in HGA concentrations is rapid, with approximately 60 % decrease in circulating HGA within 48 h on 2 mg dose (unpublished data) and thus is an efficacious treatment. Published trials have demonstrated a significant dose response decrease in urinary HGA in AKU with 8 mg daily dose reducing urinary HGA to 98.8 % of baseline concentrations (Ranganath et al 2014).
One of the major biochemical consequences of nitisinone therapy is that serum tyrosine concentrations can increase tenfold (Phomphutkul et al 2002; Introne et al 2011; Suwannarat et al 2005; Thimm et al 2011; De Laet et al 2011; Ranganath et al 2014). The metabolic fate of this is largely unknown in AKU, apart from reports of tyrosine keratopathy (Stewart et al 2014).
Elevated serum tyrosine concentrations are also a documented consequence of nitisinone therapy in hereditary tyrosinaemia-1 (HT-1). It is proposed that the supra-physiological concentrations of tyrosine may be responsible for the cognitive impairment observed in HT-1 (Thimm et al 2011; De Laet et al 2011). Other reported side effects in HT-1 include thrombocytopenia, leukopenia and ocular symptoms (Mayorandan et al 2014).
Natural protein restriction is recommended with essential amino acid supplementation in patients treated with nitisinone that have HT-1. The overall aim is to ensure serum tyrosine concentrations are <400 μmol/L (Mayorandan et al 2014).
The authors’ postulate that treatment with nitisinone should be made available earlier even if renal function is normal rather than waiting for decline in renal function and the presentation of haematological complications. This approach is also recommended as there may be delays in obtaining nitisinone quickly, in what could be a rapidly fatal event. The importance of the above is demonstrated by the recent report by Mullan et al (2015) where the patient died within a week of hospitalisation.
Conclusions
The acute haematological complications associated with AKU are complex and can be fatal. Astute recognition of these complications and appropriate medical management present significant challenges. It is however the view of the authors’ that nitisinone may provide a suitable lifesaving treatment especially in the context of deterioration in renal function and suboptimal anti-oxidant defence mechanisms. Moreover it is recommended that G6PD should be measured following the diagnosis of AKU so patients at risk can have appropriate dietary and drug modifications made to minimise depletion of NADPH and NADH, thus limiting oxidative stress.
Abbreviations
- AKU:
-
Alkaptonuria
- HGA:
-
Homogentisic acid
- HGD:
-
Homogentisate-1,2-dioxygenase
- BQA:
-
1,4-benzoquinone-2-acetic acid
- AKI:
-
Acute kidney injury
- CKD:
-
Chronic kidney disease
- NAC:
-
N-acetyl cysteine
- RBCs:
-
Red blood cells
- MetHb:
-
Methaemoglobin
- PPP:
-
Pentose phosphate pathway
- NADH:
-
Nicotinamide adenine dinucleotide
- NADPH:
-
Nicotinamide adenine dinucleotide phosphate
- ROS:
-
Reactive oxygen species
- G6PD:
-
Glucose-6-phosphate dehydrogenase
References
Abreo K, Abreo F, Zimmerman SW et al (1983) A fifty-year-old man with skin pigmentation, arthritis, chronic renal failure and methemoglobinemia. Am J Med Genet 14:97–114
Agarwal R, Vasavada N, Sachs NG et al (2004) Oxidative stress and renal injury with intravenous iron in patients with chronic kidney disease. Kid Inter 65:2279–2289
Al-Omar MA, Beedham C, Alsarra IA (2004) Pathological roles of reactive oxygen species and their defence mechanisms. Saudi Pharm J 12:1–18
Bataille S, Moal V, Aquaron RR et al (2014) Hemolysis: a fatal complication of alkaptonuria in a severe renal failure patient. Clin Nephrol 81(5):374–376
Beutler E, Baluda MC (1963) Methemoglobin reduction. Studies of the interaction between cell populations and of the role of methylene blue. Blood 22:323–333
Braconi D, Millucci L, Bernardini G et al (2015) Oxidative stress and mechanisms of ochronosis in alkaptonuria. Free Radic Biol Med. doi:10.1016/j.freeradbiomed.2015.02.021i
Burak Cimen MY (2008) Free radical metabolism in human erthyrocytes. Clin Chim Acta 390:1–11
Cappellini MD, Fiorelli G (2008) Glucose-6-phosphate dehydrogenase deficiency. Lancet 371:64–74
Ceballos-Picot I, Witko-Sarsat V, Merad-Boudia M et al (1996) Glutathione antioxidant system as a marker of oxidative stress in chronic renal failure. Free Radic Biol Med 21:845–853
Davison AS, Milan AM, Hughes AT et al (2015) Serum concentrations and urinary excretion of tyrosine and homogentisic acid in normal subjects. Clin Chem Lab Med 53:e81–e83
De Laet C, Munoz VT, Jaeken J, FranÅois B et al (2011) Neuropsychological outcome of NTBC-treated patients with tyrosinaemia type 1. Develop Med Child Neurol 53:962–964
Faria B, Vidinha J, Pêgo C et al (2012) Impact of chronic kidney disease on the natural history of alkaptonuria. Clin Kidney J 5:352–355
Hegedus ZL, Nayak U (1994) Homogentesic acid and structurally related compounds as intermediates in plasma soluble melanin formation and soft tissue toxicities. Arch Int Physiol Biochim Biophys 102:175–181
Heng AE, Courbebaisse M, Kemeny JL et al (2010) Hemolysis in a patient with alkaptonuria and chronic kidney failure. Am J Kidney Dis 56:e1–e4
Himmelfarb J, McMonagle E, Freedman S et al The PICARD Group (2004) Oxidative stress is increased in critically ill patients with acute renal failure. J Am Soc Nephrol 15:2449–2456
Inagi R, Miyata T (1999) Oxidative protein damage with carbohydrates and lipids in uremia: ‘carbonyl stress’. Blood Purif 17:95–98
Introne WJ, Phornphutkul C, Bernardini I et al (2002) Exacerbation of the ochronosis of alkaptonuria due to renal insufficiency and improvement after renal transplantation. Mol Genet Metab 77:136–142
Introne WJ, Perry MB, Troendle J et al (2011) A 3-year randomized therapeutic trial of nitisinone in alkaptonuria. Mol Genet Metab 103:307–314
Karkouti K (2012) Transfusion and risk of acute kidney injury in cardiac surgery. Br J Anaesth 109:i29–i38
Kazancioglu R, Taylan I, Aksak F et al (2004) Alkaptonuria and renal failure: a case report. J Nephrol 17:441–445
Liu W, Prayson RA (2001) Dura mater involvement in ochronosis (alkaptonuria). Arch Pathol Lab Med 125:961–963
Masella R, Benedetto R, Vary R et al (2005) Novel mechanisms of natural antioxidant compounds in biological systems: involvement of glutathione and glutathione-related enzymes. J Nutr Biochem 16:577–586
Mayorandan S, Meyer U, Gokcay G et al (2014) Cross-sectional study of 168 patients with hepatorenal tyrosinaemia and implications for clinical practice. Orphanet J Rare Dis 9:107
McKiernan PJ (2013) Nitisinone for the treatment of hereditary tyrosinemia type I. Exp Opin Orphan Drug 1:491–497
Milch RA (1960) Studies of alcaptonuria: inheritance of 47 cases in eight highly inter-related Dominican kindreds. Am J Hum Genet 12:76–85
Millucci L, Spreafico A, Tinti L, Braconi D et al (2012) Alkaptonuria is a novel human secondary amyloidogenic disease. Biochim Biophys Acta 1822:1682–1691
Millucci L, Braconi D, Bernardini G, Lupetti P et al (2015) Amyloidosis in alkaptonuria. J Inherit Metab Dis 38:797–805
Miyasaka C, Ohe C, Takahashi H et al (2013) An autopsy case of methemoglobinemia with ochronosis. Shindan Byori. Jpn J Diagn Pathol 30:112–117 (in Japanese)
Miyata T, Saito A, Kurokawa K, van Persele Y, de Strihou C (2001) Advance glycation and lipoxidation end products: reactive carbonyl compounds-related uraemic toxicity. Nephrol Dial Transplant 16(4):8–11
Mullan A, Cocker D, Taylor G et al (2015) Fatal oxidative haemolysis and methaemoglobinaemia in a patient with alkaptonuria and acute kidney injury. Clin Kidney J 8:109–112
Olszewska M (2004) The effect of hemodialysis on some parameters of the antioxidant system in the blood of patients with chronic renal failure. Ann Acad Med Stetin 50:41–52
Phomphutkul C, Introne WJ, Perry MB et al (2002) Natural history of alkaptonuria. N Eng J Med 347:2111–2121
Preston AJ, Keenan CM, Sutherland H et al (2014) Ochronotic osteoarthropathy in a mouse model of alkaptonuria, and its inhibition by nitisinone. Ann Rheum Dis 73:284–289
Ranganath LR, Jarvis JC, Gallagher JA (2013) Recent advances in management of alkaptonuria. J Clin Pathol 66:367–373
Ranganath LR, Milan AM, Hughes AT et al (2014) Suitability of nitisinone in Alkaptonuria 1 (SONIA 1): an international, multicentre, randomised, open-label, no-treatment controlled, parallel-group, dose–response study to investigate the effect of once daily nitisinone on 24-h urinary homogentisic acid excretion in patients with alkaptonuria after 4 weeks of treatment. Ann Rheum Dis [Epub ahead of print]. doi:10.1136/annrheumdis-2014-206033
Simons JP, Al-Shawi R, Ellmerich S et al (2013) Pathogenetic mechanisms of amyloid A amyloidosis. P Natl Acad Sci USA 110:16115–16120
Skold A, Cosco DL, Klein R (2011) Methemoglobinemia: pathogenesis, diagnosis, and management. South Med J 104:757–761
Stepniewska J, Ciechanowski K (2005) Oxidative stress as a reason of treatment difficulties in chronic renal failure. Pol Merkur Lekarski 19:697–700
Stepniewska J, Dolegowska B, Ciechanowski K et al (2006) Erythrocyte antioxidant defense system in patients with chronic renal failure according to the hemodialysis conditions. Arch Med Res 37:353–359
Stewart RMK, Briggs MC, Jarvis JC et al (2014) Reversible keratopathy due to hypertyrosinaemia following intermittent low-dose nitisinone in alkaptonuria: a case report. JIMD Rep 17:1–6
Suehiro K, Rinka H, Matsuura K et al (2007) A case of alkaptonuria with severe methemoglobinemia. Nihon Rinsho Kyukyu Igakukai Zasshi. J Jpn Soc Emer Med 10:71–75 (in Japanese)
Suwannarat P, O’Brien K, Perry MB et al (2005) Use of nitisinone in patients with alkaptonuria. Metab Clin Exp 54:719–728
Thimm E, Herebian D, Assmann B, Klee D, Mayatepek E, Spiekerkoetter U (2011) Increase of CSF tyrosine and impaired serotonin turnover in tyrosinemia type I. Mol Genet Metab 102:122–125
Uchiyama C, Kondoh H, Shintani H (2010) Acute methemoglobinemia associated with ochronotic valvular heart disease: report of a case. Thorac Cardiov Surg 58:113–119
Urieli-Shoval S, Linke RP, Matzner Y (2000) Expression and function of serum amyloid A, a major acute-phase protein, in normal and disease states. Curr Opin Hematol 7:64–69
Venkataseshan VS, Chandra B, Graziano V et al (1992) Alkaptonuria and renal failure: a case report and review of the literature. Mod Pathol 5:464–471
Zannoni VG, Lomtevas N, Goldfiner S (1969) Oxidation of homogentisic acid to ochronotic pigment in connective tissue. Biochim Biophys Acta 177:94
Zatkova A (2011) An update on molecular genetics of alkaptonuria (AKU). J Inherit Metab Dis 34:1127–1136
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Standards
All procedures reported in this review were in accordance with the ethical standards of the local Hospital ethics committee and with the Helsinki Declaration of 1975, as revised in 2000.
Informed Consent
Informed consent was obtained from patient(s) wherever included in this review.
Ethical Approval
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Conflict of interest
None.
Additional information
Communicated by: Daniela Karall
Rights and permissions
About this article
Cite this article
Davison, A.S., Milan, A.M., Gallagher, J.A. et al. Acute fatal metabolic complications in alkaptonuria. J Inherit Metab Dis 39, 203–210 (2016). https://doi.org/10.1007/s10545-015-9902-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10545-015-9902-0