Abstract
Mitochondrial diseases are clinically, biochemically and genetically heterogeneous disorders of two genomes, for which effective curative therapies are currently lacking. With the exception of a few rare vitamin/cofactor responsive conditions (including ACAD9 deficiency, disorders of coenzyme Q10 biosynthesis, and Leigh syndrome caused by mutations in the SLC19A3 transporter), the mainstay of treatment for the vast majority of patients involves supportive measures. The search for a cure for mitochondrial disease is the subject of intensive research efforts by many investigators across the globe, but the goal remains elusive. The clinical and genetic heterogeneity, multisystemic nature of many of these disorders, unpredictable natural course, relative inaccessibility of the mitochondrion and lack of validated, clinically meaningful outcome measures, have all presented great challenges to the design of rigorous clinical trials. This review discusses barriers to developing effective therapies for mitochondrial disease, models for evaluating the efficacy of novel treatments and summarises the most promising emerging therapies in six key areas: 1) antioxidant approaches; 2) stimulating mitochondrial biogenesis; 3) targeting mitochondrial membrane lipids, dynamics and mitophagy; 4) replacement therapy; 5) cell-based therapies; and 6) gene therapy approaches for both mtDNA and nuclear-encoded defects of mitochondrial metabolism.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mitochondrial diseases are estimated to affect approximately 1 in 5000 of the population (Thorburn 2004) and are defined as disorders directly or indirectly affecting the function of the mitochondrial respiratory chain and oxidative phosphorylation (OXPHOS) system, a series of five multimeric enzyme complexes embedded in the mitochondrial inner membrane. These diseases are characterised by predominantly neuromuscular disease or multisystem disease affecting organs with high energy demands (Rahman and Hanna 2009; Lemonde and Rahman 2015). Despite many efforts, it is still the case that no effective treatments exist for the vast majority of mitochondrial disorders.
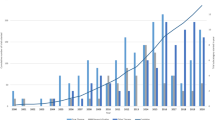
Numerous challenges hamper development of novel treatments for mitochondrial disease, not least the enormous clinical, biochemical and genetic heterogeneity associated with these disorders (Figs. 1 and 2). So far primary mitochondrial diseases have been linked to mutations in more than 200 nuclear genes (Fig. 2), as well as all 37 mitochondrial DNA (mtDNA)-encoded genes. Thus, the term ‘mitochondrial disease’ encompasses several hundred different orphan disease entities, and the reality is that a single sinecure for all of these diseases is unlikely to exist.
Genetic complexity of mitochondrial disease. Nuclear genes linked to mitochondrial disease, grouped according to pathomechanism: oxidative phosphorylation (OXPHOS) enzyme subunits (light green); OXPHOS enzyme assembly factors (dark green); mitochondrial DNA (mtDNA) maintenance (peach); mitochondrial translation (light blue); cofactor biosynthesis (yellow); membrane function and import (dark blue); and miscellaneous (grey)
Another challenge has been targeting drugs and/or nucleic acids into the mitochondrial matrix. Various ingenious strategies have been devised in order to attempt to overcome this, ranging from adding lipophilic cations or mitochondrial targeting sequences to candidate therapeutic molecules, to customised nano-particle delivery methods.
A final historical challenge was the lack of model systems in which to test novel therapies. However recent years have witnessed the development of a plethora of animal models for mitochondrial diseases, including Caenorhabditis elegans, Drosophila melanogaster and murine models (Kanabus et al 2014). Pre-clinical trials that have been performed in these various animal models will be discussed in the relevant sections below.
This review will discuss some treatable disorders that should not be missed, and then focus on five groups of emerging therapies for mitochondrial diseases: 1) antioxidant approaches; 2) stimulating mitochondrial biogenesis; 3) targeting mitochondrial membrane lipids, dynamics and mitophagy; 4) replacement therapy; 5) cell-based therapies; and 6) gene therapy approaches for both mtDNA and nuclear-encoded defects of mitochondrial metabolism.
Treat the treatable
Treatable disorders
In any discussion of developing novel therapies for mitochondrial disease, one must not lose sight of those disorders for which effective treatments already exist. These disorders, which should be actively sought out and treated, include defects of coenzyme Q10 (CoQ10) biosynthesis, which are clinically heterogeneous (Rahman et al 2012); disorders responsive to riboflavin such as ACAD9 deficiency (which may present with hypertrophic cardiomyopathy, lactic acidosis or encephalo/myopathy) and defects of riboflavin transport (Brown-Vialetto-Van Laere syndrome) which may be associated with secondary respiratory chain deficiencies (Gerards et al 2011; Foley et al 2014); and disorders responsive to biotin +/− thiamine (biotinidase deficiency and biotin-thiamine responsive basal ganglia disease) (Fassone et al 2013; Perez-Duenas et al 2013; Haack et al 2014). In this group of ‘treatable’ diseases, I would also include disorders associated with spontaneous recovery, namely ‘benign reversible’ mitochondrial myopathy linked to two homoplasmic mtDNA mutations (T>C or T>G at position m.14674 in the gene encoding tRNA glutamate), and acute liver failure of infancy caused by mutations in TRMU, a gene involved in mitochondrial tRNA modifications essential for normal mitochondrial gene expression (Boczonadi et al 2014).
Supportive therapies
Supportive treatments (Fig. 3) remain the mainstay of management for the vast majority of patients with mitochondrial disease, for whom effective curative therapies are lacking. These will not be discussed in detail here, since the focus of this review is emerging therapies, but important supportive measures include: anticonvulsants; hormone replacement (e.g. thyroxine, growth hormone, insulin); adequate nutrition (enteral feeding via gastrostomy is frequently needed); pancreatic enzyme replacement; electrolyte replacement in patients with severe renal tubulopathy; renal dialysis and/or transplantation; hearing aids; cochlear implants; brow suspension surgery for severe ptosis; cardiac pacing; heart transplantation; blood transfusions for sideroblastic anaemia; psychological support for affected patients and families; and other treatments as indicated (Rahman and Hanna 2009; Kanabus et al 2014).
Supportive therapies available for mitochondrial diseases. The main supportive therapies targeting the clinical problems shown in Fig. 1 are highlighted
Previous clinical trials
The ideal clinical trial should be adequately powered, statistically valid, randomised, double-blinded, placebo controlled and include a large group of homogeneous patients with the same clinical presentation, biochemical findings and genetic defect (at a similar mutation load if mtDNA), and preferably at a similar stage of disease progression. This is clearly impossible for mitochondrial diseases, which are characterised by extreme heterogeneity at every level. These difficulties are highlighted by a recent Cochrane systematic review of clinical trials for mitochondrial disease which found that, of 1335 abstracts reviewed, only 12 fulfilled criteria for rigorous clinical trials (Pfeffer et al 2012). Furthermore, only three of these studies included 30 or more subjects. The agents investigated in these 12 clinical trials included CoQ10, creatine, dimethylglycine, cysteine and lipoic acid. Dramatic effects were not observed in any of these trials (Pfeffer et al 2012; Kanabus et al 2014).
The reasons for the dearth of clinical trials for mitochondrial disease are manifold. There are hundreds of different genetic causes of mitochondrial disease (Fig. 2), each individually rare, which creates difficulties in collecting large homogeneous cohorts of patients. Furthermore, an individual patient may have many different clinical problems, and different treatment approaches may be needed for each of these. The unpredictable natural course of mitochondrial disease, with episodic deterioration, transient recovery and long periods of stability, together with lack of good natural history data, also present difficulties in interpreting the results of clinical trials. Identification of validated, clinically meaningful outcome measures is also challenging. Despite all of these obstacles, progress is being made, as evidenced by the following broad review of the emerging pharmacological, cell-based and gene therapy strategies for mitochondrial disease.
Emerging approaches 1: antioxidant approaches
It is generally accepted that accumulation of reactive oxygen species (ROS) is a major cause of mitochondrial disease pathogenesis, and leads to depletion of glutathione (GSH), the main mitochondrial antioxidant. Decreased GSH levels have been documented in skeletal muscle and plasma of patients with primary mitochondrial disorders (Hargreaves et al 2005; Salmi et al 2012). Furthermore, partial respiratory chain inhibition was shown to increase formation of superoxide before cellular metabolism was impaired in an astrocyte model, suggesting that oxidative stress may be more important than ATP depletion in the pathophysiology of mitochondrial disease (Jacobson et al 2005). It is therefore not surprising that many therapeutic strategies have attempted to treat mitochondrial disease by using antioxidants to ameliorate the effects of ROS, as follows.
Coenzyme Q10 and analogues
The most frequently used mitochondrial antioxidant is CoQ10, also known as ubiquinone. Although CoQ10 is of proven value in treating disorders of CoQ10 biosynthesis (Montini et al 2008; Rahman et al 2012), its role in other mitochondrial disorders is less certain. CoQ10 has been investigated in a number of randomised clinical trials for mitochondrial disease, but the results have been inconclusive (Pfeffer et al 2012; Kanabus et al 2014). A phase 3 randomised, double blind, crossover trial of CoQ10 was completed in May 2013 (Table 1), but the findings have not yet been reported. Idebenone, a synthetic CoQ10 analogue with shorter isoprenyl chain length and reputedly better blood brain barrier penetration, has been investigated in clinical trials as a potential treatment for Leber’s hereditary optic neuropathy and Friedreich’s ataxia, with suggestions of improvement (Klopstock et al 2011; Kerr 2013). A phase IIa randomised, double blind, placebo controlled, dose-finding study of idebenone is ongoing in MELAS syndrome (Table 1). EPI-743 is another synthetic structurally modified analogue of CoQ10, in which the bis-methoxy groups of the quinone have been replaced with bis-methyl groups, and the tail has three rather than ten isoprenyl units. EPI-743 has been investigated in a number of open label studies (Enns et al 2012; Martinelli et al 2012; Sadun et al 2012) with some potentially encouraging results, but the unpredictable natural course of Leigh syndrome, in particular, means that the results of such studies should be interpreted with caution. Double blind, placebo controlled, randomised clinical trials of EPI-743 are currently in progress for Leigh syndrome, Kearns-Sayre syndrome and Friedreich’s ataxia (Table 1).
N-acetylcysteine
Combined treatment with metronidazole and N-acetyl cysteine has been suggested to be beneficial in ethylmalonic encephalopathy (Viscomi et al 2010), but use of N-acetyl cysteine has not been explored in formal clinical trials for other mitochondrial disorders.
Vitamins C and E and analogues
Other antioxidants suggested to be of benefit in mitochondrial disease include vitamins E and C. Trolox (6-hydroxy-2,5,7,8-tetramethylchromane-2-carboxylic acid), an analogue of vitamin E, has been shown to ameliorate cellular phenotypes of mitochondrial complex I deficiency. For example, it has been reported to reduce ROS production, mitochondrial membrane potential and Ca2+−stimulated ATP production in complex I deficient fibroblasts (Distelmaier et al 2009; Blanchet et al 2015), but again has not been formally investigated in clinical trials.
Emerging approaches 2: stimulating mitochondrial biogenesis
For several years, a great hope for treating mitochondrial disease has been the development of strategies to stimulate mitochondrial ‘biogenesis’, i.e. the formation of new mitochondria. The biological processes underlying mitochondrial biogenesis are extremely complex and under tight transcriptional control, orchestrated by the master translational co-activator PGC1α (reviewed by (Kanabus et al 2014)). Strategies to increase mitochondrial biogenesis can be broadly divided into three groups: pharmacological, dietary and exercise. The role of exercise will not be reviewed in detail here since no new data are available about efficacy of exercise in mitochondrial disease, and this approach has been discussed extensively elsewhere (Taivassalo and Haller 2005; Taivassalo et al 2006; Murphy et al 2008). Although these approaches do not correct the underlying defect, it is thought that simply increasing mitochondrial numbers (whether ‘good’ or ‘bad’ mitochondria) will result in a net increase in energy production. Various agents have been used to attempt to stimulate mitochondrial biogenesis. Positive effects observed in these studies have varied between different models, even when using the same agent, as discussed below.
Pharmacological approaches
Bezafibrate is a synthetic ligand of the PPARα transcription factor, and has been used to treat several mouse models of mitochondrial disease. Oral bezafibrate therapy slowed onset of mitochondrial myopathy and prolonged survival in a muscle-specific Cox10−/− mouse model (Wenz et al 2008). However a subsequent study investigating two other mouse models of cytochrome c oxidase (COX) deficiency, Surf1 and COX15 knockout mice, did not replicate these findings (Viscomi et al 2011). Furthermore, although bezafibrate improved muscle histological findings and reduced the accumulation of mtDNA deletions in the muscle of the ‘Deletor’ mouse harbouring a dominant mutation in the Twinkle helicase, these effects did not appear to be mediated by inducing mitochondrial biogenesis (Yatsuga and Suomalainen 2012). It should be noted that the use of bezafibrate in rodent models is complicated by severe adverse effects on hepatic metabolism, and may not reflect efficacy in the treatment of human mitochondrial disease (Yatsuga and Suomalainen 2012). However, a randomised clinical trial of bezafibrate did not improve clinical symptoms in two mitochondrial fatty acid oxidation disorders, CPTII deficiency and VLCAD deficiency (Orngreen et al 2014). No clinical trials of bezafibrate have been reported in patients with OXPHOS defects.
Resveratrol activates the sirtuin SIRT1, which in turn is responsible for NAD+-dependent deacetylation of multiple proteins, including PGC1α and the mitochondrial transcription factor TFAM. Resveratrol has been shown to increase mitochondrial biogenesis in cell models (Lopes et al 2014) but did not appear to increase OXPHOS enzyme activities in patient fibroblasts in another study (De Paepe et al 2014). A phase 1/2 open label clinical trial has recently been completed in Friedreich ataxia (NCT01339884), but the findings have yet to be reported. A novel SIRT1 activator SRT2104 has also been suggested to improve mitochondrial function (Libri et al 2012).
5-Aminoimidazole-4-carboxamide ribonucleotide (AICAR) is a pharmacological activator of the adenosine monophosphate kinase (AMPK)-PGC1α axis. Increased mitochondrial biogenesis and ATP production and decreased ROS were observed in complex I deficient fibroblasts treated with AICAR (Golubitzky et al 2011). AICAR has also been reported to increase mitochondrial biogenesis and partially correct COX deficiency in three mouse models (Viscomi et al 2011).
Nicotinamide riboside is a newly reported form of vitamin B3 that is able to stimulate mitochondrial biogenesis by increasing NAD+ availability via a salvage/recycling pathway for NAD+ biosynthesis, leading to NAD+-dependent activation of SIRT1 and thus increasing mitochondrial biogenesis (Lightowlers and Chrzanowska-Lightowlers 2014). Early studies have demonstrated improvements following nicotinamide riboside therapy of two mouse models of mitochondrial disease. Nicotinamide riboside delayed disease progression, induced mitochondrial biogenesis in muscle and prevented the formation of mtDNA deletions in Deletor mice (Khan et al 2014), and improved respiratory chain activities and exercise intolerance in the Sco2 knockout/knockin mouse (Cerutti et al 2014). Human clinical trials are currently being planned.
Dietary approaches
Much has been written about the ketogenic diet as a potential treatment for mitochondrial disease, but at present the evidence in patients remains anecdotal and sparse (Rahman 2012). Evidence in favour of this treatment is derived from studies in cell and animal models of mitochondrial disease. Ketones reduced mtDNA mutation load in a cybrid model (Santra et al 2004), and slowed progression of mitochondrial myopathy in the Deletor mouse (Ahola-Erkkila et al 2010). Recently decanoic acid (C10), a fatty acid that is known to increase in the plasma of individuals on a ketogenic diet, was shown to stimulate mitochondrial biogenesis in both neuronal cells and cultured skin fibroblasts via a PPAR-γ mediated mechanism (Hughes et al 2014). It will be interesting to investigate whether C10 can also stimulate mitochondrial biogenesis in cell and/or animal models of mitochondrial disease.
Emerging approaches 3: targeting mitochondrial dynamics and mitophagy
Recently described approaches aim to target other aspects of mitochondrial biology. The importance of mitochondrial quality control is increasingly recognised, and includes the processes of mitochondrial fission and fusion, mitophagy (autophagy of damaged mitochondria, triggered by loss of mitochondrial membrane potential), mitochondrial biogenesis and repair (Green and Van 2011). Manipulating mitochondrial dynamics is potentially an attractive approach to treat mitochondrial diseases, since altering the balance of fission and fusion may allow damaged mitochondria (or damaged segments of mitochondria) to be rescued by complementation or else be selectively eliminated by mitophagy. Mitochondrial fragmentation is observed in some mitochondrial disorders, both primary and secondary neurodegenerative disorders. Inhibitors of the mitochondrial fission protein DRP1 such as the selective peptide inhibitor P110 could theoretically decrease aberrant mitochondrial fission in these disorders (Qi et al 2013).
One method of targeting mitophagy may be via mTOR (target of rapamycin) inhibition, and a recent study investigating rapamycin in the Ndufs4−/− Leigh syndrome conditional knockout mouse model yielded promising results (Johnson et al 2013). There appeared to be delayed onset and progression of neurological symptoms in the treated mice, with lower brain lactate and histological evidence of reduced brain inflammation and prevention of the brain lesions characteristic of Leigh syndrome (Johnson et al 2013). However, there was no change in OXPHOS capacity in these mice following treatment, leading the authors to conclude that the observed benefits may have resulted from an immunosuppressive effect of the rapamycin rather than a direct effect on mitochondrial function.
Emerging approaches 4: replacement therapy
Nucleoside therapy
Several of the mitochondrial DNA depletion syndromes (MDDS) are caused by defects of enzymes involved in nucleoside metabolism (Rahman and Poulton 2009). It has been postulated that nucleoside therapy may rescue these disorders, but achieving the right balance of nucleosides to correct the defects without toxic side effects has proved challenging (Camara et al 2013). A recent study treated mice with thymidine kinase deficiency, a form of MDDS, with a combination of the nucleosides deoxycytidine monophosphate (dCMP) and deoxythymidine monophosphate (dTMP), and reported biochemical (increased respiratory chain activities) and genetic (increased mtDNA levels) improvements in the treated mice, accompanied by increased survival. Another study showed that either supplementation with deoxycytidine or inhibition of deoxyribonucleoside metabolism with tetrahydrouridine could modulate mitochondrial deoxyribonucleoside triphosphate levels in a mouse model of mitochondrial neurogastrointestinal encephalomyopathy (MNGIE) (Camara et al 2014). It remains uncertain whether it will be possible to translate these approaches to treat human MDDS.
Enzyme replacement
Enzyme replacement therapy (ERT) is not a feasible option for primary OXPHOS deficiencies (for example, disorders caused by OXPHOS enzyme subunit or assembly factor mutations), since these are large multimeric enzyme complexes embedded in the inner mitochondrial membrane, with consequent difficulties in targeting recombinant proteins to the correct subcellular compartment. However ERT would theoretically be effective in MNGIE, since the defect is in the cytosolic enzyme thymidine phosphorylase (TP). A proof of principle study in which recombinant TP was administered encapsulated in the patient’s own red cells to a patient with advanced disease was associated with biochemical improvement, but the patient died 21 days after receiving ERT (Moran et al 2008). More recently clinical and biochemical improvements have been reported in a patient who received almost 2 years of ERT, leading the authors to suggest that a clinical trial of ERT for MNGIE is indicated (Bax et al 2013).
Emerging approaches 5: cell-based therapies
Allogeneic haematopoietic stem cell therapy
Allogeneic haematopoietic stem cell therapy (AHSCT) has shown potential in MNGIE, as a means of replacing TP enzyme activity (Hirano et al 2006), but has been associated with a high mortality, probably reflecting the degree of ill health of the affected patients prior to transplantation. A clinical trial is planned using an internationally agreed protocol (Halter et al 2011). So far AHSCT has not been shown to be of benefit for any other mitochondrial disorders. AHSCT has been reported to improve haematological function and metabolic acidosis in Pearson marrow pancreas syndrome, but the only three published cases were associated with poor outcomes following AHSCT, including progressive neurological decline and early death in all three cases (Tumino et al 2011; Gagne et al 2014). This is presumably because mtDNA deletions continue to accumulate in nondividing tissues, particularly the brain.
Mesenchymal stem cell therapy
Co-culture of adult stem cells and somatic cells showed that mitochondria can move between cells and rescue aerobic respiration in cells with non-functional mitochondria (Spees et al 2006). Based on these observations, it was suggested that damaged cells can be ‘rejuvenated’ by transfer of mitochondria from stem cells. In support of this, intra-tracheal administration of mesenchymal stem cells (MSCs) was associated with mitochondrial transfer to alveolar epithelial cells, and consequent improvement of cellular bioenergetics and alveolar function in a mouse model of acute lung injury (Islam et al 2012). A recent study showed that the mitochondrial Rho-GTPase Miro1 facilitates mitochondrial movement from MSCs to epithelial cells, with greater transfer efficiency following Miro1 overexpression in the MSCs (Ahmad et al 2014). Thus, mitochondrial transfer from MSCs may be an interesting avenue to pursue in treating primary mitochondrial diseases.
Direct delivery of mitochondria
An approach that would bypass the need to penetrate the mitochondrion to target therapies would be to deliver intact mitochondria instead. Recently, direct mitochondrial transfer using the cell-penetrating peptide Pep-1 (KETWWETWWTEWSQPKKKRKV-cysteamine) was reported to rescue mitochondrial function and cell viability of m.8344A>G cybrids (Chang et al 2013; Liu et al 2014). This is an intriguing concept, although it is difficult to envisage how this could be scaled up to the whole organismal level.
Emerging approaches 6: gene therapy
Although mitochondrial gene therapy was for a long time thought to be a fantastical notion, several methods have shown some promise at the cellular level and these will be described below.
Restriction endonucleases
Since most mtDNA mutations are heteroplasmic (i.e. coexisting with wild-type mtDNA in variable ratios) and have a threshold level above which mitochondrial function is compromised, theoretically manoeuvres to reduce the heteroplasmy level below the threshold could correct the biochemical defect in cells. One method that has been used to alter the balance between mutant and wild-type mtDNA is to use restriction endonucleases with mitochondrial targeting sequences. An initial study showed that intramitochondrial delivery of the SmaI nuclease reduced m.8993T>G mutant load (Tanaka et al 2002).
Zinc finger nucleases
Subsequently mitochondrially-targeted zinc finger nucleases (ZFNs) were developed to selectively degrade mtDNA mutations (Minczuk et al 2008). These engineered ZFNs are chimeric enzymes in which a modular Cys2His2 zinc finger DNA-binding domain is conjugated to the C-terminal catalytic subunit of the restriction enzyme FokI. Although the requirement for an additional nuclear exclusion sequence (to avoid inadvertent nuclear localisation of the ZFN) make these a cumbersome tool, recently they were successfully used to selectively eliminate the m.8993A>G point mutation and the ‘common’ ~5 kb deletion from heteroplasmic cybrid models of mitochondrial disease (Gammage et al 2014).
Mitochondrially-targeted TALENs and CRISPR/Cas9
Transcription activator-like effector (TALE) nucleases (TALENs) are synthetic enzymes created by fusing a nuclease (e.g. FokI) with a bacterial TALE sequence — a 34 amino acid repeat sequence that includes two amino acids that confer DNA binding specificity (Mak et al 2012). A mitochondrial TALEN with a mitochondrial localisation signal was recently shown to successfully cleave mutant mtDNA harbouring the common 5 kb deletion (Bacman et al 2013). Preliminary studies have also shown that this system can be used to selectively destroy mtDNA harbouring specific point mutations. Further studies are required to test this system in mouse models of mtDNA mutations, to determine whether TALENs are effective at the whole organismal level.
Another possible approach is to use a second endonuclease-based genome editing system known as CRISPR (clustered regularly interspaced palindromic repeat)/Cas9 (Doudna and Charpentier 2014) to modify mtDNA. The CRISPR associated protein Cas9 is an endonuclease that uses a guide sequence within an RNA duplex to form base pairs with target DNA sequences, and then Cas9 introduces a site-specific double-strand break in the DNA. Although CRISPR/Cas9 genome editing is reported to be more effective than TALENs (Doudna and Charpentier 2014), the requirement of an RNA component in the CRISPR/Cas9 system is a problem since it is not yet possible to import RNA reliably into mitochondria.
Allotopic gene expression
In allotopic gene expression, genes normally encoded by the mtDNA are recoded using the universal nuclear genetic code, so that they can be inserted into and expressed from the nucleus. A proof of principle study performed more than a decade ago showed that it was possible to rescue the ATP synthesis defect caused by the m.8993A>G mutation (associated with maternally inherited Leigh syndrome and neuropathy, ataxia and retinitis pigmentosa) using a recoded MTATP6 gene (Manfredi et al 2002). Subsequently allotopic expression of MTND4 (encoding a complex I subunit) in a rat model of LHON (induced by in vivo electroporation of a mutant MTND4 gene containing the m.11778G>A mutation into rat eyes) prevented retinal ganglion cell (RGC) loss and impairment of visual function (Ellouze et al 2008). Further studies assessed the efficiency and safety of AAV-mediated human ND4 gene delivery into mouse and rabbit eyes (Guy et al 2009; Shi et al 2012). Three human clinical trials of allotopic gene therapy in LHON are currently in progress: a randomised open-label safety and efficacy study of rAAV2-ND4 (NCT01267422), a phase 1/2 open-label safety of rAAV2/2-ND4 (NCT02064569) and an open-label dose escalation study of AAV gene therapy for m.11778G>A (NCT02161380) (www.clinicaltrials.gov; Table 1).
Transkingdom gene therapy
Transkingdom gene therapy aims to use a heterologous gene, encoding an exogenous oxidase otherwise absent from mammals, to bypass a defective respiratory chain enzyme. In theory Ndi, a rotenone-resistant NADH dehydrogenase single subunit complex I equivalent encoded by the nuclear yeast gene NDI1, could bypass complex I whilst the AOX alternative oxidase could bypass complexes III+IV (El-Khoury et al 2014). In an initial proof of principle study the AOX gene from the chordate Ciona intestinalis was allotopically expressed in cultured human cells (Hakkaart et al 2006), and later was shown to rescue biochemical phenotypes in human cells with COX10 or COX15 deficiency (Dassa et al 2009). Recently the C. intestinalis AOX gene was successfully expressed in early mouse embryos using germ line lentiviral transduction, to generate the MitAOX mouse model, which will be useful to study the effects of AOX in other murine models of complex IV deficiency (El-Khoury et al 2013). Another recent study used intraocular (intravitreal) injection of recombinant adeno-associated virus (AAV) serotype 2 expressing yeast NDI1 to treat a rotenone-induced murine model of LHON (Chadderton et al 2013). AAV-NDI1 reduced RGC death and optic nerve atrophy in this LHON model, and improved retinal function as assessed by optokinetic responses (Chadderton et al 2013).
Rescue by overexpression of aminoacyl tRNA synthetases
Targeting mitochondrial transfer RNAs (tRNAs) is an attractive therapeutic strategy, since more than 250 putatively pathogenic mutations have been reported in the mitochondrial tRNA genes, making these the most frequently occurring mtDNA mutations (www.mitomap.org). Furthermore, since it remains extremely difficult to manipulate human mtDNA directly, targeting the tRNAs may be a more feasible option for gene therapy approaches. Aminoacyl tRNA synthetases (aaRSs) are responsible for charging tRNAs with their cognate amino acids in the first step of protein synthesis. The observation that a yeast mitochondrial aaRS acted as a nuclear repressor for mutations in its cognate tRNA (Rinaldi et al 1997) was followed by reports that overexpression of LARS2 could partially rescue the m.3243A>G mutation in mt-tRNAleu(UUR) mutation (Park et al 2008) and that IARS2 expression levels modulated penetrance of a homoplasmic mt-tRNAile mutation associated with hypertrophic cardiomyopathy (Perli et al 2012). Subsequently it was shown that yeast LARS2 could suppress non cognate mt-tRNA mutations (Francisci et al 2011), and recently this was confirmed in human cells harbouring pathogenic tRNA mutations, supporting the hypothesis that the C-terminal domain of LARS2 has a noncanonical function in stabilising mitochondrial tRNA structures to promote translational efficiency (Perli et al 2014; Hornig-Do et al 2014).
Novel strategies for mitochondrial gene delivery
A Japanese group has developed MITO-porter, a novel membrane-based nano device for non-viral gene delivery. In this system functional nucleic acid is packaged as a nano particle covered with a lipid envelope, and a mitochondrial targeting signal peptide is added to increase efficiency of uptake of the carriers (Kawamura et al 2013).
Pronuclear and metaphase cell spindle transfer
An option to prevent transmission of mtDNA diseases is transfer of nuclear genetic material between oocytes (metaphase II spindle transfer) or embryos (pronuclear transfer). These techniques have been successfully performed in rhesus macaque monkeys (Tachibana et al 2009) and human embryos and oocytes (Craven et al 2010; Tachibana et al 2013), but have generated a great deal of controversy and debate about related ethical issues (Bredenoord et al 2011). It has been argued that these techniques constitute germline gene therapy but, after extended debate, both the House of Commons and the House of Lords of the UK government recently granted permission for these two mitochondrial donation techniques to be used under licence as part of in vitro fertilisation treatment with the aim of preventing the transmission of serious mitochondrial disease from a mother to her child (http://www.parliament.uk/business/news/2015/february/lords-mitochondrial-donation-si/). Concerns remain about the long-term efficacy and safety of these techniques in humans, which will hopefully be addressed by further research (Reinhardt et al 2013; Amato et al 2014). It should be noted, however, that currently there is no evidence that these novel techniques will offer any advantage over preimplantation genetic diagnosis for the vast majority of women carrying a mtDNA mutation (Treff et al 2012; Sallevelt et al 2013).
Gene therapy for nuclear-encoded mitochondrial disorders
In comparison to mtDNA-encoded defects, gene therapy for nuclear-encoded mitochondrial disorders is relatively straightforward. So far, AAV-mediated gene therapy has been reported in mouse models of MNGIE and ethylmalonic encephalopathy. Lentiviral-mediated haematopoietic gene therapy was used to treat Tymp/Upp1 double knockout mice, which were partially myeloblated prior to treatment (Torres-Torronteras et al 2011). Biochemical correction was observed, with high levels of TP activity in blood and reduced nucleoside concentrations following gene therapy. For ethylmalonic encephalopathy, intracardiac AAV2/8-mediated ETHE1 gene transfer has been administered to 20 Ethe1−/− mice, with evidence of restoration of enzyme activity, normalisation of plasma thiosulphate levels and increased survival, to >6–8 months compared to 1 month in untreated mice (Di Meo et al 2012).
Conclusions: closing the translational gap
Whilst it remains true that there are still no curative therapies for the vast majority of patients with mitochondrial disease, this review has demonstrated that numerous innovative treatments (pharmacological, cell-based and genetic) are currently at various stages of development (summarised in Fig. 4). The most promising pharmacological therapies target mitochondrial biogenesis, ROS and mitophagy, and a diverse range of gene therapy approaches are being developed. It seems unlikely that any single agent will be able to cure all mitochondrial diseases; strategies aimed at individualised genomic medicine are more likely to be successful. The unmet medical need for patients with mitochondrial disorders is uncontroversial, yet translating the exciting emerging therapies described in this review to the bedside remains challenging because of the lack of large cohorts of clinically, biochemically and genetically homogeneous individuals, natural history data, and validated meaningful outcome measures for use in clinical trials of novel therapeutic agents. However, the recent development of national and international mitochondrial disease consortia (Nesbitt et al 2013; Falk et al 2015), and the reports of several large natural history studies (Kaufmann et al 2011; Wedatilake et al 2013; Sofou et al 2014; Broomfield et al 2014) yield hope that progress is being made. Despite the many barriers, one can now be cautiously optimistic that effective therapies for mitochondrial disease will be found.
References
Ahmad T, Mukherjee S, Pattnaik B et al (2014) Miro1 regulates intercellular mitochondrial transport & enhances mesenchymal stem cell rescue efficacy. EMBO J 33:994–1010
Ahola-Erkkila S, Carroll CJ, Peltola-Mjosund K et al (2010) Ketogenic diet slows down mitochondrial myopathy progression in mice. Hum Mol Genet 19:1974–1984
Amato P, Tachibana M, Sparman M, Mitalipov S (2014) Three-parent in vitro fertilization: gene replacement for the prevention of inherited mitochondrial diseases. Fertil Steril 101:31–35
Bacman SR, Williams SL, Pinto M, Peralta S, Moraes CT (2013) Specific elimination of mutant mitochondrial genomes in patient-derived cells by mitoTALENs. Nat Med 19:1111–1113
Bax BE, Bain MD, Scarpelli M, Filosto M, Tonin P, Moran N (2013) Clinical and biochemical improvements in a patient with MNGIE following enzyme replacement. Neurology 81:1269–1271
Blanchet L, Smeitink JA, van Emst-de Vries SE et al (2015) Quantifying small molecule phenotypic effects using mitochondrial morpho-functional fingerprinting and machine learning. Sci Rep 5:8035. doi:10.1038/srep08035
Boczonadi V, Bansagi B, Horvath R (2014) Reversible infantile mitochondrial diseases. J Inherit Metab Dis
Bredenoord AL, Dondorp W, Pennings G, de Wert G (2011) Ethics of modifying the mitochondrial genome. J Med Ethics 37:97–100
Broomfield A, Sweeney MG, Woodward CE et al (2014) Paediatric single mitochondrial DNA deletion disorders: an overlapping spectrum of disease. J Inherit Metab Dis. doi:10.1007/s10545-014-9778-4
Camara Y, Gonzalez-Vioque E, Scarpelli M, Torres-Torronteras J, Marti R (2013) Feeding the deoxyribonucleoside salvage pathway to rescue mitochondrial DNA. Drug Discov Today 18:950–957
Camara Y, Gonzalez-Vioque E, Scarpelli M et al (2014) Administration of deoxyribonucleosides or inhibition of their catabolism as a pharmacological approach for mitochondrial DNA depletion syndrome. Hum Mol Genet 23:2459–2467
Cerutti R, Pirinen E, Lamperti C et al (2014) NAD(+)-dependent activation of Sirt1 corrects the phenotype in a mouse model of mitochondrial disease. Cell Metab 19:1042–1049
Chadderton N, Palfi A, Millington-Ward S et al (2013) Intravitreal delivery of AAV-NDI1 provides functional benefit in a murine model of Leber hereditary optic neuropathy. Eur J Hum Genet 21:62–68
Chang JC, Liu KH, Li YC et al (2013) Functional recovery of human cells harbouring the mitochondrial DNA mutation MERRF A8344G via peptide-mediated mitochondrial delivery. Neurosignals 21:160–173
Craven L, Tuppen HA, Greggains GD et al (2010) Pronuclear transfer in human embryos to prevent transmission of mitochondrial DNA disease. Nature 465:82–85
Dassa EP, Dufour E, Goncalves S et al (2009) Expression of the alternative oxidase complements cytochrome c oxidase deficiency in human cells. EMBO Mol Med 1:30–36
De Paepe B, Vandemeulebroecke K, Smet J et al (2014) Effect of resveratrol on cultured skin fibroblasts from patients with oxidative phosphorylation defects. Phytother Res 28:312–316
Di Meo I, Auricchio A, Lamperti C, Burlina A, Viscomi C, Zeviani M (2012) Effective AAV-mediated gene therapy in a mouse model of ethylmalonic encephalopathy. EMBO Mol Med 4:1008–1014
Distelmaier F, Visch HJ, Smeitink JA, Mayatepek E, Koopman WJ, Willems PH (2009) The antioxidant Trolox restores mitochondrial membrane potential and Ca2+ −stimulated ATP production in human complex I deficiency. J Mol Med (Berl) 87:515–522
Doudna JA, Charpentier E (2014) Genome editing. The new frontier of genome engineering with CRISPR-Cas9. Science 346:1258096. doi:10.1126/science.1258096
El-Khoury R, Dufour E, Rak M et al (2013) Alternative oxidase expression in the mouse enables bypassing cytochrome c oxidase blockade and limits mitochondrial ROS overproduction. PLoS Genet 9:e1003182. doi:10.1371/journal.pgen.1003182
El-Khoury R, Kemppainen KK, Dufour E, Szibor M, Jacobs HT, Rustin P (2014) Engineering the alternative oxidase gene to better understand and counteract mitochondrial defects: state of the art and perspectives. Br J Pharmacol 171:2243–2249
Ellouze S, Augustin S, Bouaita A et al (2008) Optimized allotopic expression of the human mitochondrial ND4 prevents blindness in a rat model of mitochondrial dysfunction. Am J Hum Genet 83:373–387
Enns GM, Kinsman SL, Perlman SL et al (2012) Initial experience in the treatment of inherited mitochondrial disease with EPI-743. Mol Genet Metab 105:91–102
Falk MJ, Shen L, Gonzalez M et al (2015) Mitochondrial Disease Sequence Data Resource (MSeqDR): a global grass-roots consortium to facilitate deposition, curation, annotation, and integrated analysis of genomic data for the mitochondrial disease clinical and research communities. Mol Genet Metab 114:388–396
Fassone E, Wedatilake Y, Devile CJ, Chong WK, Carr LJ, Rahman S (2013) Treatable Leigh-like encephalopathy presenting in adolescence. BMJ Case Rep 2013:200838. doi:10.1136/bcr-2013-200838
Foley AR, Menezes MP, Pandraud A et al (2014) Treatable childhood neuronopathy caused by mutations in riboflavin transporter RFVT2. Brain 137:44–56
Francisci S, Montanari A, De LC, Frontali L (2011) Peptides from aminoacyl-tRNA synthetases can cure the defects due to mutations in mt tRNA genes. Mitochondrion 11:919–923
Gagne KE, Ghazvinian R, Yuan D et al (2014) Pearson marrow pancreas syndrome in patients suspected to have Diamond-Blackfan anemia. Blood 124:437–440
Gammage PA, Rorbach J, Vincent AI, Rebar EJ, Minczuk M (2014) Mitochondrially targeted ZFNs for selective degradation of pathogenic mitochondrial genomes bearing large-scale deletions or point mutations. EMBO Mol Med 6:458–466
Gerards M, van den Bosch BJ, Danhauser K et al (2011) Riboflavin-responsive oxidative phosphorylation complex I deficiency caused by defective ACAD9: new function for an old gene. Brain 134:210–219
Golubitzky A, Dan P, Weissman S, Link G, Wikstrom JD, Saada A (2011) Screening for active small molecules in mitochondrial complex I deficient patient’s fibroblasts, reveals AICAR as the most beneficial compound. PLoS One 6:e26883. doi:10.1371/journal.pone.0026883
Green DR, Van Houten B (2011) SnapShot: mitochondrial quality control. Cell 147(950):950. doi:10.1016/j.cell.2011.10.036
Guy J, Qi X, Koilkonda RD et al (2009) Efficiency and safety of AAV-mediated gene delivery of the human ND4 complex I subunit in the mouse visual system. Invest Ophthalmol Vis Sci 50:4205–4214
Haack TB, Klee D, Strom TM et al (2014) Infantile Leigh-like syndrome caused by SLC19A3 mutations is a treatable disease. Brain 137, e295. doi:10.1093/brain/awu128
Hakkaart GA, Dassa EP, Jacobs HT, Rustin P (2006) Allotopic expression of a mitochondrial alternative oxidase confers cyanide resistance to human cell respiration. EMBO Rep 7:341–345
Halter J, Schupbach WM, Casali C et al (2011) Allogeneic hematopoietic SCT as treatment option for patients with mitochondrial neurogastrointestinal encephalomyopathy (MNGIE): a consensus conference proposal for a standardized approach. Bone Marrow Transplant 46:330–337
Hargreaves IP, Sheena Y, Land JM, Heales SJ (2005) Glutathione deficiency in patients with mitochondrial disease: implications for pathogenesis and treatment. J Inherit Metab Dis 28:81–88
Hirano M, Marti R, Casali C et al (2006) Allogeneic stem cell transplantation corrects biochemical derangements in MNGIE. Neurology 67:1458–1460
Hornig-Do HT, Montanari A, Rozanska A et al (2014) Human mitochondrial leucyl tRNA synthetase can suppress non cognate pathogenic mt-tRNA mutations. EMBO Mol Med 6:183–193
Hughes SD, Kanabus M, Anderson G et al (2014) The ketogenic diet component decanoic acid increases mitochondrial citrate synthase and complex I activity in neuronal cells. J Neurochem 129:426–433
Islam MN, Das SR, Emin MT et al (2012) Mitochondrial transfer from bone-marrow-derived stromal cells to pulmonary alveoli protects against acute lung injury. Nat Med 18:759–765
Jacobson J, Duchen MR, Hothersall J, Clark JB, Heales SJ (2005) Induction of mitochondrial oxidative stress in astrocytes by nitric oxide precedes disruption of energy metabolism. J Neurochem 95:388–395
Johnson SC, Yanos ME, Kayser EB et al (2013) mTOR inhibition alleviates mitochondrial disease in a mouse model of Leigh syndrome. Science 342:1524–1528
Kanabus M, Heales SJ, Rahman S (2014) Development of pharmacological strategies for mitochondrial disorders. Br J Pharmacol 171:1798–1817
Kaufmann P, Engelstad K, Wei Y et al (2011) Natural history of MELAS associated with mitochondrial DNA m.3243A>G genotype. Neurology 77:1965–1971
Kawamura E, Yamada Y, Harashima H (2013) Mitochondrial targeting functional peptides as potential devices for the mitochondrial delivery of a DF-MITO-porter. Mitochondrion 13:610–614
Kerr DS (2013) Review of clinical trials for mitochondrial disorders: 1997–2012. Neurotherapeutics 10:307–319
Khan NA, Auranen M, Paetau I et al (2014) Effective treatment of mitochondrial myopathy by nicotinamide riboside, a vitamin B3. EMBO Mol Med 6:721–731
Klopstock T, Yu-Wai-Man P, Dimitriadis K et al (2011) A randomized placebo-controlled trial of idebenone in Leber’s hereditary optic neuropathy. Brain 134:2677–2686
Lemonde H, Rahman S (2015) Inherited mitochondrial disease. Paediatr Child Health 25(3):133–138. doi:10.1016/j.paed.2014.11.002
Libri V, Brown AP, Gambarota G et al (2012) A pilot randomized, placebo controlled, double blind phase I trial of the novel SIRT1 activator SRT2104 in elderly volunteers. PLoS One 7:e51395. doi:10.1371/journal.pone.0051395
Lightowlers RN, Chrzanowska-Lightowlers ZM (2014) Salvaging hope: is increasing NAD(+) a key to treating mitochondrial myopathy? EMBO Mol Med 6:705–707
Liu CS, Chang JC, Kuo SJ et al (2014) Delivering healthy mitochondria for the therapy of mitochondrial diseases and beyond. Int J Biochem Cell Biol 53:141–146
Lopes CA, Le BC, Mathieu L et al (2014) Beneficial effects of resveratrol on respiratory chain defects in patients’ fibroblasts involve estrogen receptor and estrogen-related receptor alpha signaling. Hum Mol Genet 23:2106–2119
Mak AN, Bradley P, Cernadas RA, Bogdanove AJ, Stoddard BL (2012) The crystal structure of TAL effector PthXo1 bound to its DNA target. Science 335:716–719
Manfredi G, Fu J, Ojaimi J et al (2002) Rescue of a deficiency in ATP synthesis by transfer of MTATP6, a mitochondrial DNA-encoded gene, to the nucleus. Nat Genet 30:394–399
Martinelli D, Catteruccia M, Piemonte F et al (2012) EPI-743 reverses the progression of the pediatric mitochondrial disease–genetically defined Leigh Syndrome. Mol Genet Metab 107:383–388
Minczuk M, Papworth MA, Miller JC, Murphy MP, Klug A (2008) Development of a single-chain, quasi-dimeric zinc-finger nuclease for the selective degradation of mutated human mitochondrial DNA. Nucleic Acids Res 36:3926–3938
Montini G, Malaventura C, Salviati L (2008) Early coenzyme Q10 supplementation in primary coenzyme Q10 deficiency. N Engl J Med 358:2849–2850
Moran NF, Bain MD, Muqit MM, Bax BE (2008) Carrier erythrocyte entrapped thymidine phosphorylase therapy for MNGIE. Neurology 71:686–688
Murphy JL, Blakely EL, Schaefer AM et al (2008) Resistance training in patients with single, large-scale deletions of mitochondrial DNA. Brain 131:2832–2840
Nesbitt V, Pitceathly RD, Turnbull DM et al (2013) The UK MRC mitochondrial disease patient cohort study: clinical phenotypes associated with the m.3243A>G mutation-implications for diagnosis and management. J Neurol Neurosurg Psychiatry 84:936–938
Orngreen MC, Madsen KL, Preisler N, Andersen G, Vissing J, Laforet P (2014) Bezafibrate in skeletal muscle fatty acid oxidation disorders: a randomized clinical trial. Neurology 82:607–613
Park H, Davidson E, King MP (2008) Overexpressed mitochondrial leucyl-tRNA synthetase suppresses the A3243G mutation in the mitochondrial tRNA(Leu(UUR)) gene. RNA 14:2407–2416
Perez-Duenas B, Serrano M, Rebollo M et al (2013) Reversible lactic acidosis in a newborn with thiamine transporter-2 deficiency. Pediatrics 131:e1670–e1675
Perli E, Giordano C, Tuppen HA et al (2012) Isoleucyl-tRNA synthetase levels modulate the penetrance of a homoplasmic m.4277T>C mitochondrial tRNA(Ile) mutation causing hypertrophic cardiomyopathy. Hum Mol Genet 21:85–100
Perli E, Giordano C, Pisano A et al (2014) The isolated carboxy-terminal domain of human mitochondrial leucyl-tRNA synthetase rescues the pathological phenotype of mitochondrial tRNA mutations in human cells. EMBO Mol Med 6:169–182
Pfeffer G, Majamaa K, Turnbull DM, Thorburn D, Chinnery PF (2012) Treatment for mitochondrial disorders. Cochrane Database Syst Rev 4, CD004426. doi:10.1002/14651858
Qi X, Qvit N, Su YC, Mochly-Rosen D (2013) A novel Drp1 inhibitor diminishes aberrant mitochondrial fission and neurotoxicity. J Cell Sci 126:789–802
Rahman S (2012) Mitochondrial disease and epilepsy. Dev Med Child Neurol 54:397–406
Rahman S, Hanna MG (2009) Diagnosis and therapy in neuromuscular disorders: diagnosis and new treatments in mitochondrial diseases. J Neurol Neurosurg Psychiatry 80:943–953
Rahman S, Poulton J (2009) Diagnosis of mitochondrial DNA depletion syndromes. Arch Dis Child 94:3–5
Rahman S, Clarke CF, Hirano M (2012) 176th ENMC international workshop: diagnosis and treatment of coenzyme Q(10) deficiency. Neuromuscul Disord 22:76–86
Reinhardt K, Dowling DK, Morrow EH (2013) Medicine. Mitochondrial replacement, evolution, and the clinic. Science 341:1345–1346
Rinaldi T, Lande R, Bolotin-Fukuhara M, Frontali L (1997) Additional copies of the mitochondrial Ef-Tu and aspartyl-tRNA synthetase genes can compensate for a mutation affecting the maturation of the mitochondrial tRNAAsp. Curr Genet 31:494–496
Sadun AA, Chicani CF, Ross-Cisneros FN et al (2012) Effect of EPI-743 on the clinical course of the mitochondrial disease Leber hereditary optic neuropathy. Arch Neurol 69:331–338
Sallevelt SC, Dreesen JC, Drusedau M et al (2013) Preimplantation genetic diagnosis in mitochondrial DNA disorders: challenge and success. J Med Genet 50:125–132
Salmi H, Leonard JV, Rahman S, Lapatto R (2012) Plasma thiol status is altered in children with mitochondrial diseases. Scand J Clin Lab Invest 72(2):152–157. doi:10.3109/00365513.2011.646299
Santra S, Gilkerson RW, Davidson M, Schon EA (2004) Ketogenic treatment reduces deleted mitochondrial DNAs in cultured human cells. Ann Neurol 56:662–669
Shi H, Gao J, Pei H et al (2012) Adeno-associated virus-mediated gene delivery of the human ND4 complex I subunit in rabbit eyes. Clin Experiment Ophthalmol 40:888–894
Sofou K, de Coo IF, Isohanni P et al (2014) A multicenter study on Leigh syndrome: disease course and predictors of survival. Orphanet J Rare Dis 9:52. doi:10.1186/1750-1172-9-52
Spees JL, Olson SD, Whitney MJ, Prockop DJ (2006) Mitochondrial transfer between cells can rescue aerobic respiration. Proc Natl Acad Sci U S A 103:1283–1288
Tachibana M, Sparman M, Sritanaudomchai H et al (2009) Mitochondrial gene replacement in primate offspring and embryonic stem cells. Nature 461:367–372
Tachibana M, Amato P, Sparman M et al (2013) Towards germline gene therapy of inherited mitochondrial diseases. Nature 493:627–631
Taivassalo T, Haller RG (2005) Exercise and training in mitochondrial myopathies. Med Sci Sports Exerc 37:2094–2101
Taivassalo T, Gardner JL, Taylor RW et al (2006) Endurance training and detraining in mitochondrial myopathies due to single large-scale mtDNA deletions. Brain 129:3391–3401
Tanaka M, Borgeld HJ, Zhang J et al (2002) Gene therapy for mitochondrial disease by delivering restriction endonuclease SmaI into mitochondria. J Biomed Sci 9:534–541
Thorburn DR (2004) Mitochondrial disorders: prevalence, myths and advances. J Inherit Metab Dis 27:349–362
Torres-Torronteras J, Gomez A, Eixarch H et al (2011) Hematopoietic gene therapy restores thymidine phosphorylase activity in a cell culture and a murine model of MNGIE. Gene Ther 18:795–806
Treff NR, Campos J, Tao X, Levy B, Ferry KM, Scott RT Jr (2012) Blastocyst preimplantation genetic diagnosis (PGD) of a mitochondrial DNA disorder. Fertil Steril 98:1236–1240
Tumino M, Meli C, Farruggia P et al (2011) Clinical manifestations and management of four children with Pearson syndrome. Am J Med Genet A 155A:3063–3066
Viscomi C, Burlina AB, Dweikat I et al (2010) Combined treatment with oral metronidazole and N-acetylcysteine is effective in ethylmalonic encephalopathy. Nat Med 16:869–871
Viscomi C, Bottani E, Civiletto G et al (2011) In vivo correction of COX deficiency by activation of the AMPK/PGC-1alpha axis. Cell Metab 14:80–90
Wedatilake Y, Brown R, McFarland R et al (2013) SURF1 deficiency: a multi-centre natural history study. Orphanet J Rare Dis 8:96. doi:10.1186/1750-1172-8-96
Wenz T, Diaz F, Spiegelman BM, Moraes CT (2008) Activation of the PPAR/PGC-1alpha pathway prevents a bioenergetic deficit and effectively improves a mitochondrial myopathy phenotype. Cell Metab 8:249–256
Yatsuga S, Suomalainen A (2012) Effect of bezafibrate treatment on late-onset mitochondrial myopathy in mice. Hum Mol Genet 21:526–535
Acknowledgments
SR is supported by Great Ormond Street Hospital Children’s Charity and currently receives research grant funding from The Wellcome Trust, The Lily Foundation, and Vitaflo International Ltd.
Compliance with Ethics Guidelines
ᅟ
Conflict of interest
Professor Rahman declares that she has received grant support from Vitaflo International Ltd, but the funder played no role in the preparation of this manuscript.
Animal rights
This article is a review, and does not contain any studies with human or animal subjects performed by the author.
Author contribution
Professor Rahman is the sole author of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by: Eva Morava
Rights and permissions
About this article
Cite this article
Rahman, S. Emerging aspects of treatment in mitochondrial disorders. J Inherit Metab Dis 38, 641–653 (2015). https://doi.org/10.1007/s10545-015-9855-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10545-015-9855-3